SIBO, FODMAP & The Alphabet Soup of Your Gut

join Dr. Taz to explain SIBO, FODMAPs, and how to improve your health by aiding your gut.
- Get help using this
information to become healthier.
- Get your personalized plan for optimizing your gut health with my new
book. - Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional
Medicine Review Clinical Newsletter.
*Thank you to Dr. Taz for sharing this interview with us. To learn more, visit the Dr. Taz MD Show*
Dr. Taz Bhatia: Welcome back to the show where every episode we’re trying to help you write your own personal
prescription for power. That’s right. This is Power Rx. And joining me today is Dr. Ruscio. Dr. Ruscio gives smart,
busy people suffering from symptoms like bloating, fatigue, and unexplained weight gain simple steps to start living
a healthy and enjoyable life again, no matter how long you’ve been suffering.
So many of you suffer with gut issues. Dr. Ruscio has spoken at the SIBO Symposium summit, the Paleo f(x), the
Ancestral Health Symposium, Sean Croxton’s Digestion Sessions, as well as many other international conferences and
top health podcasts. Welcome to the show, Dr. Ruscio.
Dr. Michael Ruscio: Hi, thank you for having me.
DrTB: Well, we’re thrilled to have you. I’ve got to admit this is a question that comes up over and over again
in practice. And when I speak to people, everybody’s really, first of all, concerned about gut health. And they’re
super confused about SIBO which is small intestinal bacterial overgrowth, really confused about what that is. Do
they have it? How do they treat it? Tell us a little bit about how you jumped into the world of gut health and how
you became so specific in dealing with SIBO.
DrMR: Well, I would love to. And I’m sure many listening have probably heard before in various interviews, I
had my own personal health experience which diverted me down the path into more integrative medicine with a focus on
gut health. Long story short, when I was in college, I went from feeling really good overall to having insomnia,
brain fog, fatigue, mood dips.
And this led me on a journey to discover what the answer was. It ended up actually being an intestinal infection that
was causing all those symptoms. But I didn’t realize that right out of the gate. I was pursuing what I thought was
hypothyroidism or low testosterone or heavy metal toxicity or adrenal fatigue.
So I did what wouldn’t be unexpected to do. I went on the internet. I started searching my symptoms. And of course,
you pull up various articles and videos and what have you. And that’s all fine and good, but I didn’t have the
greater context of understanding how important it is to start your journey with a gut evaluation in case you have
something in your gut that’s contributing to your symptoms.
So I spent several months spinning my wheels. Eventually, I determined that I had an intestinal infection that was
the underlying cause of all my symptoms, even though I didn’t really have much in the way of digestive symptoms
specifically. And it was addressing that underlying cause in the gut that finally allowed me to have long-lasting
improvement in my symptoms.
And then, as I got into clinical practice, it turns out that my experience was fairly common. And there were many
other people who were pursuing what they thought was the cause of their symptoms: thyroid, adrenal. And not to say
that sometimes those aren’t the cause, but in many cases, there’s an underlying gut problem that’s really at the
root cause of someone’s symptoms.
And this can go all the way to something like brain fog or insomnia even. And by addressing that, they can see very
profound improvement. So that’s become a progressive area of focus for me in practice because it just delivers so
much in the way of symptomatic improvement.
DrTB: It’s so funny how so many of us have entered the field after our own personal issues, really searching
for answers on our own. So you started this right out of college. So you would’ve been pretty young when your
symptoms began. Is that correct?

an amoebic infection which is a fairly pathogenic infection. He said, “This is going to be an unpleasant process,
but it’s also going to be one of your biggest gifts because it’s going to teach you firsthand what patients go
through and what happens in your body when you have an imbalance in the gut.” And he was absolutely right.
It was not pleasant in the moment, but I learned so much from it. And it gave me such a valuable grounding experience
that has been like the set of the sail to help me stay focused on this very important area for people’s health.
DrTB: I think it’s such an important area. Some of my background is in Chinese and ayurvedic medicine. They
recognized the importance of the gut thousands of years ago. This was not a new or novel idea or concept for them,
so much so that they believed if you didn’t have good gut health, you really didn’t have health. That’s really how
they defined everything.
I think it’s taken us in Western medicine a really long time to catch up to that idea and to that philosophy. Why in
your opinion, just thinking about your practice and what you deal with day-in and day-out, why do you think gut
health is so important? I have my own opinion just based on my experience. I’m curious to know what you think.
DrMR: Well, we know that the small intestine is responsible for over 90% of caloric absorption. So there is
one huge aspect. If you don’t absorb your food well and your nutrients well, it’s almost akin to eating an unhealthy
diet because you’re absorbing an unhealthy amount of nutrients. So that’s one foundational factor.
And there’s also the observation that the small intestine contains the largest density of immune cells in the entire
body. And so, we have this very immune-rich organ which is our small intestine, and if things there are not in
harmony, if the immune system is reacting, then that’s a source of chronic inflammation in the body. And that
inflammation, as we know, can cause a litany of symptoms and correlates with a number of conditions.
So those may be two of the more important aspects. The way you impact your nutrient absorption and the way you can
affect the status of the immune system and inflammation which are very tightly linked. There are others, but I think
those would probably be two of the most profound mechanisms through which the gut health leads to such an impact on
one’s overall health more broadly.
DrTB: And for those of you listening, I really hope you caught that. That is a central tenet as to why gut
health is so important. So much of our immune system is centered there. So much of the whole process of inflammation
begins there. And honestly, I’m sure Dr. Ruscio would agree, most of what we deal with today in terms of medical
practice are diseases of the immune system or are diseases of inflammation.
So this is a really, really important topic, and I hope everyone’s taking notes and just trying to get whatever you
can get out of this particular episode. What are some of the reasons—what causes some of these problems in the gut.
I don’t think anyone sets out thinking about gut health and certainly wanting to cause issues. I’m sure you’ve
experienced this as well. This is kind of the why of why someone who eats perfectly healthy and really is meticulous
about their diet is still unhealthy when this particular aspect of their health is not taken care of.
What do you think causes a lot of these gut problems?
eating healthy and they’re still not feeling much better, then it’s very important to not try to necessarily force a
dietary solution to what may be a non-dietary problem. And that’s one mistake I see people make quite often, which
is they go on progressively more restrictive diets.
And yes, sometimes we may need a more restrictive diet in the short term, but it’s very important not to go on a diet
that’s highly, highly restricted at the same time missing the fact that you have an active issue in the gut that’s
the cause of all your symptoms. I just want to echo that because that’s such an important concept.
But regarding underlying problems in the gut that can be the causative factor, food intolerances—and I’m using that
term loosely—but eating foods that don’t agree with you probably the most foundational because that’s going to be
the easiest to fix and the most cause-based.
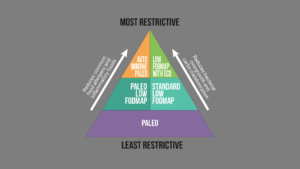
And there are a few different diets, and we can go more into detail about them in a moment. But the way I look at the
food aspect is there are really two main factors to control for. And this is once you get over the basic dietary
hurdle of no processed foods and added sugars…
DrTB: Sugar.
DrMR: And once you’re eating a healthy, whole food-based diet, then the two chief items to concern oneself
with, in my opinion, would be foods that your body does not react well to because you’re a bit food intolerant,
meaning you have this, for lack of a better term, inflammatory reaction.
So some people will have some inflammation if they eat gluten or dairy or soy. So cutting out the common—again, I’m
using the term loosely—allergens that may not agree with the gut and cause this inflammatory immune reaction. And
then, the other underneath the food umbrella would be not consuming foods that don’t work well for your microbiota
or the world of bacteria and fungus in your gut specifically.
And these are known as foods that are rich in FODMAPs which are seemingly healthy foods on the surface. And this can
throw people sometimes because a food such as broccoli or asparagus, for some people, especially for people with
digestive symptoms, may actually be contributing to your symptoms.
That’s not to say you never eat those again, but you may have to go through a short phase where you curtail the
amount of FODMAP or prebiotic-rich foods that you’re consuming. And just briefly, why that’s relevant is because
these foods that are rich in FODMAPs or prebiotics are very good at feeding bacteria. And that can be a good or a
bad thing depending on what’s going on underneath the hood of your digestive tract.
If you have a bacterial overgrowth known as small intestinal bacterial overgrowth, as you alluded to earlier, if you
eat a diet rich in these FODMAPs, in these prebiotics, then you’re feeding an overgrowth. And of course, that can
exacerbate the problem. So those are two places to start: an elimination diet and/or a low FODMAP diet.
DrTB: Ok. I’m going to stop you because you’ve said two things that I know everyone starts—their eyes start to
swim a bit when they hear these words. And I can see the flush and the panic the minute they hear them as well. So
let’s unwind them just a bit.

those any better, unfortunately. I wish we could. But processed foods, sugars, diets high in food additives,
preservatives, all of those type of things are going to be bad for the gut. So some of this is our Western
lifestyle, convenience foods, packaged foods, and what they’ve done.
But once you accomplish or sort of hit that layer one of removing that stuff from your diet, the next conversation to
have is getting into what is SIBO, or small intestinal bacterial overgrowth, and what is the FODMAP diet? And, Dr.
Ruscio, I will tell you patients try really hard with this diet, but get super frustrated with it.
In your opinion, how would you best describe the symptoms and signs of SIBO and how would somebody know that they
have it? And then, from there, let’s help them with that FODMAP diet. What are the top five things you would tell
them because they have SIBO, and it’s confirmed either through their history or testing or things like that, this is
what they probably need to do next? Help us bridge that because I just see the struggle when I’m working with
patients or even speaking on this topic where people get super, super confused about this.
DrMR: Sure. And it’s very understandable, and I agree with you completely which is why I think it’s important
people obtain information on this issue that’s well thought out and not overzealous. Because you’re absolutely
right. Sometimes people are obtaining the information perhaps from a well-intentioned but an overzealous source, and
that may cause them to have more fear around small intestinal bacterial overgrowth and it’s justifiable.
So I just want to make sure to say that most of what I’ve seen my patients read on the internet regarding SIBO makes
SIBO look far worse than it actually is.
DrTB: Thank you for saying that.
DrMR: If you’re obtaining competent advice that’s evidence-based, it’s not something to be overly concerned
about. It’s very treatable, and so I just want to preface my comment by saying that. I think from a mental
perspective this may provide some psychological ease.
Small intestinal bacterial overgrowth, essentially as the name alludes, is a condition of excessive bacterial growth
in the small intestine. And you can test this with a breath test, although I don’t think that is as necessary as
it’s often portrayed to be. It can be helpful, but you don’t necessarily need to have the testing.
Now, the symptoms, you have your classical box of symptoms which would be your IBS-like symptoms, abdominal pain,
bloating, and altered bowel function, meaning you have constipation, diarrhea, or sometimes you oscillate between
the two. And then there are some other similar digestive symptoms that we’re seeing small intestinal bacterial
overgrowth correlated with: reflux, indigestion, heartburn probably the most common.
Here’s where it gets a little bit more complicated, though. Because there are other non-digestive symptoms that can
be associated to SIBO or, more broadly, to impaired digestive health. And this is where it can make it difficult to
say if I have X, Y, Z symptoms, I may have SIBO or a similar gut imbalance.
We know, for example, that you can have a gut problem or SIBO that can manifest as digestive symptoms. That’s kind of
an easy one to piece together. But we’ve also seen SIBO highly correlated with small intestinal bacterial
overgrowth. We’ve seen certain gut imbalances when treated improve thyroid autoimmunity.

with mood problems like anxiety, depression, and brain fog. We see some trials showing the treatment we go to
improve metabolism via cholesterol markers and blood sugar markers. We see the treatment of SIBO able to improve
rosacea and certain dietary changes able to improve skin conditions. And we see gut treatments at large able to
improve rheumatoid arthritis and inflammatory bowel disease.
So since the symptoms can be so broad, I think it’s helpful to provide people with a hierarchy, meaning start with
the basics like we mentioned a few moments ago. And then if the basics don’t get you to a point where you feel fully
improved, the next thing to do would be to go through a gut evaluation. And that may include SIBO.
Although, I don’t necessarily think you have to do a SIBO test, but whether you use something like a self-help plan
provided in a book or you work with a provider, the next thing I would do is do a gut health check-up. And then,
regarding the low FODMAP diet, the nice thing about the low FODMAP diet and many diets, if you use them
pragmatically, is you only require two to three weeks on the diet to be able to ascertain whether or not that diet
will help you.
DrTB: That’s encouraging. That’s good news.
DrMR: So if you find a low FODMAP food list on the internet, you only need about two weeks, maybe three weeks
tops. And if you’re not clearly noticing you’re improved at the end of that two to three weeks, then that may not be
the diet for you. And there’s more that we can outline there, but I’ll pause there in case you want to add anything
to that.
DrTB: No, I just think that should be encouraging for everybody listening. I think people think that this is
going to be a change forever. They’re never going to be able to eat anything they ever want to again.
DrMR: Right.
DrTB: If you’re out there suffering from some of these symptoms Dr. Ruscio was talking about, just thinking
like for two to three weeks this is something that you’re going to focus on, I think that’s manageable. And tell us
a little bit more about what that involves.
DrMR: Right. And you’re absolutely right. It is manageable and it’s important to know that this doesn’t mean
forever because oftentimes that’s where people go. If you say, you need X, Y, or Z, people will immediately go to,
“Ugh, I can never have broccoli or asparagus again or onions or garlic.” No. Most diets follow a similar trajectory
of, first, be a little bit strict, yes. Eliminate the foods not on the diet.
But on the tail end of that, then you reintroduce the foods that you cut out to find out where your personal boundary
for the diet is. And that’s a key aspect. So that would be how you implement the FODMAP diet amongst many others.
You start with a more strict application of the diet, and then you don’t necessarily have to perform the
reintroduction after two to three weeks. You just need to get to the two to three-week mark and then reassess and
say, yes, I’m clearly feeling better or, eh, I don’t really feel any different.
And if you’re saying, eh, then you move onto other diets or other therapeutic options.
DrTB: Got it.
DrMR: But if you’re saying to yourself, yes, I clearly feel improved, then I would ride that diet until you
see a plateau in your improvement. Then wait a couple weeks to make sure that you’re stable in your new peak of
health, and then you can perform a reintroduction from there.
And those FODMAP foods that you’re referring to, you’ve mentioned them a couple of times. You mentioned broccoli,
garlic, onions. What else would be in the family of FODMAP foods that somebody would be consciously trying to
remove?
DrMR: What’s funny is you are looking at a lot of seemingly healthy foods that you cut out on the low FODMAP
diet which is why this is so counterintuitive. So there’s many vegetables that we would label as healthy: artichoke,
asparagus, broccoli, Brussel sprouts, eggplant, onion, apples, mango, pear. It’s a list that it would do one well to
look at because, again, many of these we would stereotype as healthy foods.
And it’s not to say that they’re unhealthy foods, but they’re very rich in those prebiotics. This also includes a
number of dairy products because dairy has the lactose that, for some people, can function very highly as a
prebiotic. And a number of grains like wheat and rye. In fact, some of the research is suggesting that the reason
why some people are benefiting from a gluten-free diet is because a gluten-free diet also restricts these FODMAPs.
And also, cauliflower is included in this and other vegetables. So there are a number of vegetables here that would
seem healthy. And this can be the real curveball and you alluded to this a moment ago which is someone improves
their diet but they’re not feeling any better. Sometimes what happens is someone goes on a whole foods diet, but
it’s also a high FODMAP diet. And so they say, “Ugh, I’m improving my diet, but I my even feel worse. I feel more
bloated or more gassy.”
And it may be because, while they cut out all the processed foods, now they’re eating a very FODMAP-rich diet. It can
be very frustrating.
DrTB: Interesting. So what can you eat on the FODMAP diet? What are things that people usually when they cut
all these, like you said, healthy foods that many of us love, what can you eat on this particular diet?
DrMR: And that’s the good news. There’s a lot of foods that you can eat. It’s just needing that map, that diet
list to guide you. So you can use bok choy, carrots, beans—green beans, that is—squash, potato, taro, zucchini,
gluten-free bread products can work, blueberries, boysenberries, cranberries, kiwis, lemons, oranges, lactose-free
milk, oats, hard cheeses.
DrTB: Lots of options.
DrMR: So there’s a lot you can do.
DrTB: Yeah.
DrMR: But it’s just having that little bit of a guide to help you go through your shopping cart and say, “Ok,
these are the foods I’m going to focus on, and these are the foods that I’m going to avoid.” And I should also
mention, it’s not to say you can’t have one bite of the high FODMAP foods during that two to three-week diet
experiment.
You just want to reduce them as much as you can. If you go out for a work event one night and you have some broccoli,
it’s not going to be the end of the world. You just want to attempt for an 80-90% compliance during your dietary
experiment.
DrTB: And Dr. Ruscio, you have a book that was just released in February called Healthy Gut, Healthy
You. Are a lot of these lists and resources in that particular book?
DrMR: Yes. This book comes with a number of handouts, not actually in the book but as part of the online
compendium to the book. So you’ll have a handout for an elimination diet that cuts out those inflammatory foods like
we mentioned a moment ago. You have a handout for a low FODMAP diet also with some resources for cookbooks and
essentially a number of handouts to help you along your journey.
terms of, ok, here’s all the stuff you’ve heard regarding your gut: paleo diet, low carb, low fat, low FODMAP,
probiotics, enzymes, antimicrobial herbs. What do we do when? How do we sequence this? And how can we apply this
information in such a way that we will be practical? We won’t go on crazy diets for too long and we’ll use dietary
supplements but not overly use them and try to make this as efficient and as empowering of a process as we can.
DrTB: Well, actually, that was going to be my next question because I am curious as to your opinion on—I know
you talk about this in the book, but I’m curious as to your opinion on the role of probiotics, on the role of
digestive enzymes, other supplements that we see that are gut-based, bitters. There’s a whole litany in the gut
nutraceutical toolbox.
What do you think works for somebody who’s—they understand the importance of diet. I always say if you don’t master
the diet component, then it’s really hard for any supplement to do much for you. But they’ve mastered the diet part.
They’ve bought into the idea of SIBO. What are some of the supplements that you’ve seen work in the most efficient
way when somebody is struggling with some of these different symptoms?
DrMR: Sure. That’s a great question. The first thing, again, definitely diet. And that’s why, step one, in the
healing protocol in the book is a series of short, mini experiments to help you find the best diet for you and for
your gut. Because it’s not going to be the same for everyone. So we want to do a little bit of tinkering to see if
we can fix this with diet because, again, you’re absolutely right. That’s where we want to start.
It’s very important because we don’t want to be going on fancy supplements when the diet may be the cause of the
problem. So definitely start there. But then, step two, we introduce and we outline enzyme therapy and also
hydrochloric acid. Some people may have heard of hydrochloric acid or betaine hydrochloride which is a supplemental
way to take the acid that your stomach produces as part of the digestive process.
So we talk about enzymes and acid and then also probiotics. And that’s really our step two. And probiotics can be
very effective. Out of all those I just mentioned, we have by far and away the best evidence supporting the
beneficial role of probiotics. And probiotics have been shown to help with everything from bloating and constipation
through anxiety and depression.
And that’s the far-reaching impact of the gut. It can even reach all the way to your brain and influence things like
anxiety and depression. Probiotics can be very confusing for people because there are hundreds of products out
there. And it seems like every few weeks there’s a new product out.
And of course, every time a product is released, the company wants to market that product, so you get all these bits
and bites. And it’s very hard to know why is this probiotic better or is it not any better, is it the same as the
other one I heard about previously. And in the book, I introduce a category system that’s based on the research that
helps people really simplify this.
And we can supply probiotics down to three main categories. Category one is a mixture of Lactobacillus and
Bifidobacterium strains and there are many probiotics that fit this bill.
DrTB: Right.
DrMR: This is what most people will see in health food stores or may have tried previously and that can be a
very helpful type of probiotic or category one Lactobacillus and Bifidobacterium strain mixture. So when you look on
the label, you’ll see mostly Lactobacillus X or Bifidobacterium Y or what have you.
Category two is a healthy fungus known as Saccharomyces boulardii. And on the label, there you’ll see, predominantly,
Saccharomyces boulardii. And then, category three are soil-based or spore-forming probiotics. And you typically see
different strains of Bacillus in this type of formula.
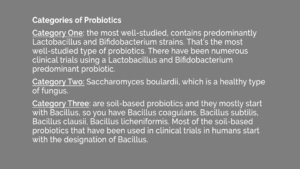
you don’t have to try all the hundreds of different products out there, but say, “Ok, I’m going to try one probiotic
from category one, one probiotic from category two, and one probiotic from category three.”
And figure out which one or maybe all three of those works well for me because what happens sometimes is, let’s say,
someone goes on a category two probiotic, the Saccharomyces boulardii, and they notice nothing. But then a few
months later, they go on another probiotic that has a different name, but they didn’t read the label to realize this
is essentially the same thing I was using before. It just has a different name on the label.
So when you understand that, you can greatly simplify the probiotic process and figure out what of this very helpful
therapeutic line you should use and then move on.
DrTB: Wow. What great information. I have so many more questions. I’m sure all of you out there listening are
as well. But hopefully, this episode has cleared up a little bit about SIBO, FODMAP, probiotics. I’m sure there’s
much more.
Dr. Ruscio’s book is Healthy
Gut, Healthy You which you can find on Amazon and anywhere that books are available. Dr. Ruscio, any
parting thoughts before we say goodbye to you? This has been, I know, tremendously helpful to everybody out there
listening.
DrMR: Well, thank you. And what I would leave people with is remember that improving your gut health should be
a journey that makes you feel empowered, and it should not make you feel fearful or afraid of food or depend upon
supplements. So if you’re getting that feeling with whatever you’re reading or listening to, I would urge you to
take some steps to try to find some information that seems a bit more empowering and a bit less fear-mongering.
Because unfortunately, there is a fair amount out there on the internet. And I see more patients than I’d like to
admit come in who are very distraught around this issue. And that’s why I wrote Healthy Gut, Healthy
You is to give people a guide that would not make them fearful, would help them feel empowered,
because that feeling of fear is not healthy for you. So it’s important that you’re not afraid, and there’s really no
need for you to be afraid. So that’s what I would leave people with.
DrTB: I love that. I couldn’t agree more. And for everybody out there listening, grab a copy of Dr. Ruscio’s
book. It’s Healthy Gut,
Healthy You. It’s on Amazon. And remember, we want you empowered, and every day is an opportunity
for you to find your power and write your own personal prescription for power. Thanks for joining us. Thank you, Dr.
Ruscio.
DrMR: Thank you.
What do you think? I would like to hear your thoughts or experience with this.
- Get help using this
information to become healthier.
- Get your personalized plan for optimizing your gut health with my new
book. - Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional
Medicine Review Clinical Newsletter.
Dr. Ruscio is your leading functional and integrative doctor specializing in gut related
disorders such as SIBO, leaky gut, Celiac, IBS and in thyroid disorders such as hypothyroid and hyperthyroid. For
more information on how to become a patient, please contact our office. Serving the San Francisco bay
area and distance patients via phone and Skype.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!