Listener Questions – What the Health, Low FODMAP Diets, Gene Tailored Diets, MegaSpore Probiotic, Probios & Constipation, and More…
Another listener Questions podcast! Today we will discuss
- What the Health
- Low FODMAP Diets
- Gene Tailored Diets
- MegaSpore Probiotic
- Probios & Constipation
- Alternative prescription antibiotics and antifungals
- And more…
Dr. R’s Fast Facts
Is a Low FODMAP diet harmful because it “starves” my gut bacteria?
Studies have shown conflicting results on the impact of Low FODMAP diet to the microbiota. Two recent studies suggest good results for Low FODMAP diet in clinical conditions like IBS and IBD.
- Causes normalization of serotonin cell density in the small intestine and in the colon
- Reduces overactive immune system by modulating histamine
- Reduces leaky gut
Do gene testing guided diets offer additional benefit to people with the APOE genotype?
- More studies are needed but try diet and see if it works for you.
- Full write up of the study is in the November edition of the Functional Medicine Review.
Is Megaspore probiotic good for SIBO patients?
- Open to it but not a lot of evidence out there yet.
- There is better evidence on other probiotics at this time. A good rule of thumb, try it and see if it works for you.
Probiotics & Constipation
- Probiotics can be helpful but they’re not helpful for everyone.
- Experiment with different probiotics and see if they work for you.
- Different classes, you can try individually or together
- Lactobacillus Bifidobacterium blend
- S Boulardii
- Soil-based probiotic
- Coli nissle 1917
What the health – Is meat consumption bad?
Studies show that Paleo and Mediterranean diets actually have a slight edge on no meat diets. Meat consumption suggestions:
- Eat non-processed meat
- Add in some fasting
- Try a no or low protein day
- Continue to buy high-quality meats
Any recommendations for replacing Fluconazole while on Imodium (for someone with IBSD)?
- Try any of the herbal antifungals while you’re taking Imodium.
- If you can manage, maybe discontinue Imodium until you have finished the round of antifungal.
My new book Healthy Gut, Healthy You will be for sale in February. There is a comprehensive protocol in there for folks who want help healing their gut.
- Get help using this information to become healthier.
- Get my free gut health eBook.

Does A Low FODMAP Diet Starve Gut Bacteria? … 00:00:47
Amoeba Histolytica Infection … 00:04:52
Treating SIBO and other Dysbiosis … 00:06:13
Dieting for Your Genetics … 00:07:31
Using MegaSpore Biotic for SIBO … 00:09:26
Dr. Ruscio’s Book Update … 00:14:37
Probiotics and Constipation … 00:17:11
“What the Health” … 00:21:43
(click gray Topics bar above to expand and see full outline/time stamp)
Replacing Fluconazole for IBS-D when Taking Imodium … 00:30:11
Will Prokinetics Address My Gut Issues? … 00:36:13
Episode Wrap-up … 00:37:52
Download Episode (Right click on link and ‘Save As’)
Listener Questions – What the Health, Low FODMAP Diets, Gene Tailored Diets, MegaSpore Probiotic, Probios & Constipation, and More…
Episode Intro
Dr. Michael Ruscio: Hey, everyone. Welcome to Dr. Ruscio Radio. This is Dr. Ruscio and let’s jump in to another edition of Listener Questions.
Does A Low FODMAP Diet Starve Gut Bacteria?
The first is not necessarily one person’s individual question, but it is a question that often comes up, which is, “Is a low FODMAP diet harmful because it ‘starves my gut bacteria?’” And there’s potentially a very long answer to this question.
But firstly, the opinion or the thought that it universally starves your gut bacteria or does so in a significant way has not fully been bore out. Some studies have shown refuting results in terms of the impact on the microbiota. The others, which are far more important in my mind, are really threefold. One, maybe most important—nah, maybe not important. I can’t say any one of these is more important than the others. But this is important.
Two studies to date have shown that by adherence to a low FODMAP diet, both the cells in the colon and the cells in the small intestines can actually increase the density of serotonin cells and become more like that of healthy controls by going on a low FODMAP diet.
Again, the key takeaway there is a low FODMAP diet causes a normalization of serotonin cell density in the small intestine and in the colon. And this is looking at samples in IBS patients before going on a low FODMAP diet, resampling the intestinal tissue after going on a low FODMAP diet, and showing that the density of serotonin cells and other, what’s known as enteroendocrine cells, actually becomes more like that of healthy controls.
Now, again, notably, serotonin cell density increases. Why is serotonin important? Amongst other things, it helps alleviate pain or dampen nociception. And, oh, my God, it helps with motility. And I know everyone loves to freak out over motility. And I do think that the importance of motility is there, but is definitely overstated. However, this is an argument for potentially helping with motility, because what do prokinetics do? Many prokinetics actually help to facilitate the action of serotonin in the gut. Hence, their ability to have a pro-motility effect.
So if a low FODMAP diet can increase the density of serotonin cells, it would stand very reasonably to the inference that it could help restore intestinal motility. Now, this may be part of the reason why we see a reduction of leaky gut in other studies that have examined a low FODMAP diet, and a reduction of immune activation in other studies that have looked at the low FODMAP diet. And when I say immune activation, I am referring to a lowering of histamine.
So when we look at all these things together and we see that a low FODMAP diet may—and I don’t think we can even say that confidently—may have a significant impact in diminishing the amount of bacteria in your gut, which may not be a bad thing. But when we weigh that against the fact that it can normalize serotonin cells, reduce immune over-activation by modulating histamine and reduce leaky gut, we start seeing that if we sync two bacterial centrically, microbiota, microbiota, microbiota, and not more broadly about what’s happening in someone’s physiology, we could be very easily misled.
Now, this is all trumped in my opinion by the clinical evidence. We see very good results in clinical conditions like IBS and IBD from a low FODMAP diet. I’m not making the argument that everyone needs to be on a low FODMAP diet all the time and forever. I think we’re on the same page with starting with a low FODMAP diet, giving that time to realize full effects. It may be one month, it may be two months, it may be three months, what have you, and then reintroducing to try to find the broadest diet possible.
But it is important, I think, to be aware of those three things. I did share that at this year’s Ancestral Health Symposium. And I think some lightbulbs are finally starting to click with not looking at everything in the gut via the context of the microbiota, but thinking a little bit more broadly. So hopefully that was helpful to the audience there. We will be sharing that video—they did a video, the lectures, and we should have that coming out in a few weeks.
Amoeba Histolytica Infection
I also wanted to share a couple reflections from the clinic. We talked so much about all this science and, whatever, all this health and medical stuff. Sometimes it’s nice to think just to share some simple things. One patient came in and, gosh, this poor guy came in with either his wife or his girlfriend. And this poor guy was really in dire straits, not feeling well. I can’t recall his exact symptom profile off the top of my head, but fatigue, depression, brain fog, food reactivity, and to a point where it was becoming somewhat debilitating. And we found in this young man Entamoeba histolytica infection, which is a very pathogenic amoeba. And that’s one that’s near and dear to my heart because it’s what I had and is what profoundly taught me the impact of the gut. And it’s nice sometimes just to be sitting there holding the answers to this person’s ailment and having an answer for them.
And by the way, this wasn’t something that required me to map out every pathway in their body like sometimes functional medicine advocates, we just had to get to a core issue and identify that fairly simply. He’s just starting treatment but I’m very hopeful for him, and I’m sure we’ll probably have a patient conversation video published on the website at some point with him.
Treating SIBO and other Dysbiosis
And another patient came in, and this was kind of cool. When this patient first came in, now, I’m thinking probably about two years ago, we found SIBO and I think other dysbiosis and treated him, and he responded really well. When he came in, he looked a bit sickly. I mean, I don’t know how to say this, very thin, very pale, made very poor eye contact, kind of shifty and timid. And the gentleman that came back in just a couple weeks ago was like a totally different person.
He had much more vibrant look to his face. His cheekbones and eyes didn’t look sunken in. He had vibrance to him. He made good eye contact. He had this vitality to him. And he was just coming in because he felt like he was regressing just slightly and he wanted to do some tweaking. But sometimes when someone responds really well and then they don’t follow up and they just kind of keep working the plan on their own and they heal and heal and heal and heal and improve and improve, and then they come in a year and a half later and you can really see that. It’s quite remarkable. And so just two cases that were, I guess, kind of wind in my sails, to really see the good work that functional medicine can do for people, and especially gut-focused functional medicine.
Dieting for Your Genetics: The ApoE Genotype
Okay, so moving on, there was a question that I did answer a few months ago. It was about gene type diets or gene-testing guided diet. And a study was published recently that speaks to this entitled, “The Effect of Apolipoprotein E Genotyping on Response to Personalized Dietary Advice Intervention: Findings from the Food4Me Randomized Controlled Trial.” Essentially, what this study found was that the gene tailoring of the diet offered no additional benefit in terms of just trying the diet irrespective of if you have the genes or not.
So they essentially took groups of people, two different groups of people, those that had the APOE genotype and those that did not have the APOE genotype. They put them, both groups, on a diet that was lower in saturated fat essentially, a little bit lower on protein, saturated fat, and higher in carbs. And they saw equivalent improvements in both groups, meaning that the people with the genes didn’t respond any better to the diet than the people without the genes, which comes back to my answer to this question from a few months ago, which is I’m open to it but I haven’t really been impressed with what I’ve seen.
So, essentially, what this means is you can just try a diet and see how you respond. And if it doesn’t give you the results you’re ideally looking for, try a different diet or potentially start running off the hierarchy that we’re always painting in this podcast, which is start with diet and lifestyle. And if that doesn’t work, then consider starting with the gut and hopefully under the guidance of a well-studied gut clinician.
Now, if you want the details on this, a full write-up of this study along with some images from the study, graphs and charts and such, will appear in the November Edition of The Future of Functional Medicine Review clinical newsletter. So you can definitely sign up and check that out if you wanted to get the deeper dive.
Using MegaSpore Biotic for SIBO
All right. So the next question is actually an audio question. So let me get my super high tech setup here where I play it from my phone into my microphone, and we will get rolling.
Speaker: Hi, Dr. Ruscio. I have a question regarding a probiotic that I have heard is supposed to be helpful with patients that have SIBO. I was diagnosed with SIBO about three years ago. I went through one round of Xifaxan, but it quickly came back, and I sort of gave up. But now I’m looking at retesting myself next week and starting looking at taking the antibiotics again. And the name of this probiotic that’s supposed to be good is called MegaSporeBiotic. And I just wanted to know your opinion about this, if you’ve heard of it, and if it really is a good one or is it just marketing. Thank you so much. Bye-bye.
DrMR: All right, so good question, definitely a question I get in the clinic here and there from patients. And so what’s my answer?
Well, I’m certainly open to MegaSporeBiotic. I’ve used it with a few patients. I’ve experimented with them myself. And I really have no reason to believe it’s any better than any other probiotic. However, we have better evidence for other probiotics, hence my leaning towards those.
So that’s really my answer, open to it. But there’s something really important that I think is helpful for all of us to understand—it took me a little while to learn this but I’m so glad that I did—is that new does not mean better. It really doesn’t. And that’s why I try to be open minded but also disciplined in looking to where we have good evidence, because oftentimes we do have good evidence.
And so I understand that in the name of progress, sometimes you have to perceive the things that don’t have as much evidence but you have to weigh that against the other understanding, which is new does not mean better. Now, someone may say, but I’ve heard about a study with MegaSpore or I watched a really compelling video or what have you. And that’s all fine and good, right? But really, the less you know I think the more amenable you are to information marketing. Now, when I were to see a study on MegaSpore which, by the way, doesn’t have impressive clinical evidence in my opinion. It’s got some but nothing I would consider very impressive.
You can look at multiple antibiotic studies that show successful outcomes for SIBO using different antibiotics. Yes, this goes beyond the standard antibiotic of Rifaximin and neomycin. There are others that work very well also. The downside of some of these other antibiotics is they have a higher chance of side effects because they have a more broad action. But many antibiotics have been shown to be successful.
Alternatively, many herbal antimicrobials have shown to be successful too. You have the Gerry Mullin’s protocol, which is similar but has completely different products than the protocol that I use. And many in the SIBO community like Allison Siebecker’s type protocol, which is more one or two ingredients at a time and that also works.
So, there are multiple different herbal antimicrobials that all work. Regarding probiotics specifically, there had been quite a few, I think now maybe eight or more studies, showing successful outcomes in SIBO, either SIBO symptoms, SIBO gas levels, or both using different probiotics in almost every study. Even with elemental diets, different elemental formulas have been used.
Even semi-elemental formulas have shown equivalent results. I should say more so with symptoms and with SIBO gas levels. We don’t have that scientific data. But I’ve used some elemental formulas in the clinic alongside traditional elemental diets and seen absolutely equivalent results. And we do have side-by-side trials in Crohn’s disease with elemental versus semi-elemental and they both show equivalent outcomes.
So what does this mean? It means all of these things work and this means that there is not a magic product. And really the magic is in the process, right? And so, it’s less sexy. It’s easier to sell someone a magic product like a magic probiotic. But when you’re a clinician, you see that all of these things can work but rarely does one thing work for everyone. So it’s figuring out how to orchestrate the use of different treatments in the most efficient process possible. That’s why I say that the magic is in the process, not in the product. And I talked about this in my book quite a bit, and I expand upon this.
So you could start again with just working with a competent SIBO clinician who will likely run you through a SIBO algorithm, I shouldn’t say ‘the’ because there’s not one universal. But there’s a tentative outline that emerges in how to best treat SIBO.
So you can start there. And if you can’t find a good doctor, you can always reach out to my clinic or pick up a copy of my book, which will be available in February, and go to that protocol. And I should update on the book.
Dr. Ruscio’s Book Update
So, gosh, we’re getting close. It’s been a long time, longer than I’d like to admit. But we’re rounding the final few corners here. And the book will go on pre-sale in January. And then it will be for sale and officially published in February. And I’m exceedingly, exceedingly excited about this. I just got some feedback from our developmental editor and these are people who are—they’re editors for a living. They’re not necessarily health geeks like we are. So I was curious to get an opinion as to whether the deep scope of this book would be something that might turn people off because I want to strike that balance between making it clinically advanced but also not overwhelming a beginner.
And I was very, very happy to hear her say something along the lines of despite this book having such a breadth of information, it’s very accessible, and it keeps the reader engaged, and the protocol to run through is clear and concise. So I have been saying for a while, I’m excited about it. I’m even more excited after getting that feedback and the book is almost here.
Sponsored Resources


So I don’t always have the time to make a home crockpot of food and of broth. So these are easy, convenient, healthy and shelf-stable, so I don’t have to worry about potentially having to throw them out. So thank you again to Kettle & Fire, and also Equip Foods and Perfect Keto. Definitely check them out. Okay, back to the show.
Probiotics and Constipation
Another audio question about probiotics and constipation.
Speaker: Hi, Dr. Ruscio. I’ve been trying to improve general gut health by introducing probiotics. But I had found most of them seemed to make my main digestive complaint, constipation, even worse. I’m wondering if there’s merit to taking probiotics intermittently, maybe once or twice a week rather than daily. Is it possible that doing so would still allow me to experience some of the benefits with less of the downside? I love your podcast and appreciate everything you do. Thanks.
DrMR: Okay. So, a good question. Now, probiotics can be very helpful and we’ve talked about multiple ways in which probiotics can be helpful mechanistically and multiple conditions for which probiotics can be helpful. But it does not mean that a probiotic will be helpful for everyone. So, what’s funny here, right, is the real world and what you see in published studies may not look, at a surface glance, like it always matches. And so here’s what I mean; we’ve talked about a few studies that have shown a couple different probiotic formulas have been shown to be helpful for constipation. So it would seem quite counterintuitive that someone would have a negative reaction of constipation from a probiotic.
But this is because science or clinical trials will not tell you exactly what will happen to someone. But it gives you information that tells you what you have a higher probability of happening. So when we see trials showing successful outcomes with irritable bowel syndrome and with constipation, for example, it doesn’t mean that everyone with IBS and with constipation will improve from that probiotic or from probiotics as a general class. What it does mean is that you have a much higher incidence of successful outcomes than you do adverse outcomes. But the adverse outcomes are still there. So it’s important to keep that in mind, and this is why we want to use science to guide our decision-making. But again, if it were as simple as one study showed this and that’s all you had to do, we really wouldn’t need doctors to think through this.
So what I’d recommend you do is experiment with some different probiotics and find what works for you. You can try a Lactobacillus-Bifidobacterium blend. You can try S. boulardii. You can try a soil-based probiotic. And you can try an E. coli Nissle 1917, trade name is Mutaflor probiotic. You can try each one of those, maybe even experiment with using those together and see if those work for you, if one or any combination of those seems to work for you.
If you’re always reacting negatively, then it’s most likely that probiotics are not going to be a good fit for you, and then you can just focus on food. And if fermented foods don’t work well for you, then you may just want to avoid probiotics altogether. I would not continue to try to force yourself to use probiotics if you’re not noticing that they help you. Because again, while the majority do tend to either be neutral or benefit from probiotics, there are some people with almost any treatment that are going to be what’s known as paradoxical responders, meaning they have the opposite of the intended effect.
So do some experimentation. Try those categories of probiotics: lactobifido blend, S. boulardii, a soil-based organism, and an E. coli. And if none of those works, then I would move on. Now, someone may argue that and there may be a small probability that some other unique strain—because there are a few exceptions to those four general categories that I outlined.
So a strain that’s outside of those four categories or a mixture of strains may work for you. But in my estimation, if someone reacts negatively to all four of these different classes, the probability of a different “super special” mixture or strain helping them is pretty dismal. So hopefully that helps.
“What the Health”
Now, Jessica Goodlife asks, “I recently watched a video titled, ‘What the Health,’ that basically makes the statement that eating meat will lead to a number of health problems like diabetes and heart attack. I can see then point made in the film showing the way that grocery store meat is raised, given drugs, and processed. I always pay the big bucks for grass-fed, free range, organic, wild caught, etcetera, and even buy from local farmers. As a person who counts macros and lifts weights, I’ve been told you must eat actually a rather high amount of protein, one gram per pound of body weight, to build muscle appropriately. Those diets tend to also be on the low end of carbs as well. Can you weigh on meat consumption? It seems that from the beginning we were meant to eat meat. I get that the way grocery store meat is now, it can be very bad for you. But all meats? Am I wasting my money? Am I putting my health at risk eating grass-fed, etcetera?”
Okay. So there are a number of points here. And I’ve spoken to this many a time before, but a few thoughts. First, processed meat does not equal all meat. And I think that was one conflation that was made in that documentary. I did not watch that documentary. Quite simply, I don’t have the time to watch a spin piece that’s not very well scientifically validated. So I didn’t bother to watch it, but I’ve caught a few snippets. And I think one of the things they’ve done in that documentary is conflated all meat in with processed meat, which of course is just hellaciously poor science.
Now, moving on to things that are actually real world science that measures real world outcome, comparative trials looking at vegetarian or similar type diets to Paleo diets or lower carb diets have shown a slight edge favoring lower carb or Paleo for obesity, metabolic syndrome, diabetes, cardiovascular disease risk marker assessments like total cholesterol and HDL cholesterol, triglycerides, and blood sugar when you look at the whole panel together and quantify risks.
And there have been two studies that have shown that a Paleo or a Mediterranean diet both reduce risk of colorectal cancer. So it’s important to keep these comparative trials in mind because these are conveniently left out of the vegetarian argument.
And it’s frustrating that people have so much dogma regarding nutrition. You would think that nutrition is religion, and we actually talked about this a while back with Alan Levinovitz in his book. I think it’s called The Gluten Lie. He was on, gosh, now maybe two years ago. And he made the statement that diet and nutrition is often treated more like religion than it is science. Because in this documentary, from one of the snippets that I did catch, there was this very official doctor in the white coat, the expert comes down from the mountain to offer us his opinion, and his opinion was a load of garbage. Because it was incredibly biased and there was a nice and neat iteration of one side of the argument.
And there’s, gosh, there’s nothing—well, there may be a few things, but there are very few things that irritate me more than when someone hides behind the perceived expert credential and gives you a biased opinion. It drives me nuts because what it does is it violates your trust. It doesn’t matter to me because I know better. But for the consumer, it violates your trust and it is absolutely maddening. People could very easily say, what I can tell you is I used this diet, it works well for patients, it’s been shown to have a lot of health benefits.
But when you start making these claims and we’ve talked about this before, the evidence shows, these studies have clearly shown, they start making these definitive statements as if you have gone through a weighing of all the evidence on both sides of the argument. When you make claims like that, but you clearly haven’t done it, you are lying to people. You are innocuously and covertly lying to people. And it absolutely drives me nuts.
Now, we have gone through a comprehensive review of the literature of both sides of the evidence. And in my book, I present you both sides of the evidence. And guess what, almost any diet can work compared to no diet at all. Some diets have a slight edge like I just outlined. So don’t think because they interview official-looking people in this documentary that they are not amenable to bias, because of course, they are.
And to the evolutionary piece, I’ve also spoken about this, there was a key point in time. It was Homo habilis versus Paranthropus boisei. We think, anyway, to the best knowledge according to the archaeology data, there was a shift where the more omnivorous Homo habilis, because of their omnivorous diet, actually had a, guess what, a shortening of the colon and a shift away from a highly fermentative, highly plant-based digestive tract like a cow and more towards the omnivorous GI tract that we now have.
This is why in part we have a shorter colon when we look at ruminants like cows or other mammals that are predominantly vegetarian in their diet because we haven’t allocated as much room in the colon for fermenting and breaking down these hard-to-digest food stuff, because we can procure things like ripe fruits, starches, and meats, all what are known in the archaeology literature as high-quality foods. High-quality meaning how much calories do you have in a unit of food, not is it grass-fed or what have you. High-quality food means you’re smart enough or you have the dexterity to access foods that deliver more calories per gram essentially, which gives you more energy.
And then the more easily you can access energy, the more you can stop using all your time in a day to procure food. And now you can focus on tool-making communication, community building, and then the culture advances. So certainly, there are some evidence showing that we are not meant to be strictly vegetarian and that we are omnivorous. I have to say everyone has to be eating protein in their diet, but to say that we’re not meant to eat protein is an absolute scientific farce in my opinion.
So eating processed meat, again, you don’t have to eat meat, but I think it’s generally healthier. You may want to pepper in some fasting or intermittent fasting. And you may want to add in a no or low protein day like we’ve talked about previously with some different guests. But I think the first person to introduce me to that was Sal from Mind Pump. And yes, I would continue buying the high quality, definitely. And I think you’re doing yourself a great service by doing that.
Dr. Ruscio Resources
Hey, everyone, in case you’re someone who is in need of help or would like to learn more, I just wanted to take a moment to let you know what resources are available. For those who would like to become a patient, you can find all that information at drruscio.com/gethelp.
For those who are looking for more of a self-help approach and/or to learn more about the gut and the microbiota, you can request to be notified when my print book becomes available at drruscio.com/gutbook. You can also get a copy of my free 25-page gut health eBook there.
And finally, if you’re a healthcare practitioner looking to learn more about my functional medicine approach, you can visit drruscio.com/review. All of these pages are at the drruscio.com URL, which is D-R-R-U-S-C-I-O dot com, then slash either ‘gethelp,’ ‘gutbook,’ or ‘review.’ Okay, back to the show.
Replacing Fluconazole for IBS-D when Taking Imodium
Next question, this is from Shallah. “Dr. Rao and Dr. Ruscio, what do you recommend to replace fluconazole for someone with IBSD”—so diarrheal-type IBS—“and is unable to give up Imodium? My doctor does not dare give me fluconazole while I’m on Imodium.” So that’s first part of the question.
You could try an herbal medicine or any number of other antifungals and you can simply check to see what antifungals has the least risk of a negative reaction with Imodium. Or you can just stop Imodium for a couple of weeks. I’m not sure how needed that is to keep your symptoms at bay. But usually antifungal medications are two, maybe three weeks. Herbals you could get away with while you’re taking the Imodium. So those are some options for you there.
And he continues with a question. “Dr. Rao, you co-wrote a paper on people whose digestive problems worsened after using probiotics.” And he provides a link. “How do you treat these patients?”
Well, in the August edition on The Future of Functional Medicine Review clinical newsletter, we did a full write-up on this, and I will give you a little sneak peek 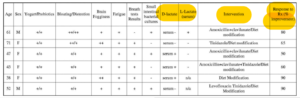
And predominantly, there was essentially an antibiotic and an antiparasitic agent. Tinidazole, I believe, is predominantly antiprotozoal. So yeah, I mean, nothing here incredibly sexy and many may have anticipated that something like fluconazole and Rifaximin were used, but it comes back to my earlier posit, which is many different treatments within the same treatment class tend to work.
So I keep harping on this to prevent US healthcare consumer or US clinician or doctor from thinking that someone has the magic protocol, right? And every time a new product pops up, everyone is up in arms about this being the next big thing, I just watch and wait as the anticipation builds. And then you see what happens in the real world and excitement dies and it gets leveled out. There are rarely things that are blockbusters in terms of they work far better than anything else in the same treatment class. I’m certainly excitedly awaiting those, but again it comes back to knowing how to use these things as part of a more broad toolkit – the when and the how rather than having the magical what.
And the final aspect of this gentleman’s question, “My IBSD”—diarrheal—“worsened using after bacterial probiotics after a course of Xifaxan or Rifaximin. Additional courses of Xifaxan did not relieve any of the symptoms – brain fog, horribly increased gas pain, bloating, and physical collapse. The only way to control it is greatly restricting my carb intake to small amounts of millet. I have tried other low FODMAPs without relief. Potato and buckwheat both flattened me immediately. A gruel of millet flour does the same while whole millet does not but then whole passes through me hardly digested.”
All right. So I will consider some other treatment approaches. An elemental diet may work very well for you. Herbal antimicrobials may work very well for you. You may have both bacteria and fungus, so you may need more than just Xifaxan. Now, the herbals would cover this because most herbals will be both antibacterial and antifungal. Or you could try, per Dr. Rao’s recommendation, a pairing of Rifaximin with fluconazole. But remember, just because Dr. Rao said that, I’m sure if we had him here on the line right now, he wouldn’t say that’s the only protocol that you can use. Because right here in the study, an assortment of a few different antibiotics and antiprotozoals were used and showed favorable outcome.
So again, please don’t think because you’ve heard one thing, one place, one time, that that’s the only way to do it. This is where you should work with your doctor a little bit and don’t go into your doctor demanding he do the exact same treatment that you heard in my podcast. If they’re going to use something similar, that’s of the same treatment class, so if we recommended Rifaximin with fluconazole in the Rao podcast, and your doctor wanted to use let’s say, Rifaximin with Tinidazole instead or different antifungal agent, I’d be open to trying that. And if all of this fails for you, you can go through the protocol in my book or find yourself a good doc because you may just need a little additional attention. And you may need to have someone just kind of work with you to work through what treatment approach will work best for you.
And just a quick reminder guys, I have been so thankful for the iTunes reviews. It has given us such a nice jump, so a thousand thank yous for that. And if you’re someone that hasn’t left an iTunes review yet, if you wouldn’t mind just taking two seconds, you can write a quick one, anything. It really helps us climb in iTunes. And then when Mary Sue is looking for some information on her health and she types in health podcast, we have a higher probability of reaching her, which I think is so important, because I’m trying to protect people from some of the unscrupulous functional medicine out there that’s well-intentioned but just misguided and pulls people into this fear-mongering, elaborate testing, restrictive dieting, and may not give them the ideal solution to their problems. So thank you if you can do that.
Will Prokinetics Address My Gut Issues?
All right, another question here. Vicky says hi. Hi, Vicky. “I found that herbal antibiotics, Candida enzymes, low FODMAP diet, and enemas keep things at bay. But when consuming prebiotic foods, like in a green super food powder aggravate my digestive system. What am I missing? Digestive enzymes, HCl, DAO”—DAO is a diamine oxidase enzyme that helps with the breakdown of histamine—“oh and staying away from histamine foods too, any suggestions? What prokinetics would you suggest besides ginger? I found that laxative teas relieve discomfort within an hour, which makes me suspect SIBO-SIFO but clearly not something I consider as a solution. Also, since daily enemas, there has been no need for such tea. Thank you.”
Okay, so there’s a lot there. I think you would really benefit from the protocol in my book because it takes you through from foundation to I guess fruition, a very solid protocol for the gut. And I don’t mean to be overly referring to my book, but I can give you way more either treating you as a patient or in my book than I can give you here because guess what? In the book, there’s a step-by-step protocol where we’re going to go through all this together, check in on how you’re doing. And then depending on how you answer, I’ve built in the response to how you’re doing and what the next step should be because, again, I wish I could tell you, “Hey, do this and that, and it’s going to fix it,” but the likelihood of that happening is extremely small.
Now, you may simply not do well on prebiotics and this is a fair number of people. You may just not be reacting to prebiotics. This is why, in part, I am passionate about sharing the message that a low FODMAP diet shouldn’t be something to be shun as being damaging for your microbiota. Certainly, I think we have a little more to learn about the long-term implications of a low FODMAP diet. However, no one’s recommending a strict adherence to a low FODMAP diet in perpetuity but rather avoiding low FODMAP foods to your tolerance. So go strict for four to eight weeks, reintroduce the tolerance, most people will have some high FODMAP foods that they don’t tolerate and that’s okay. So the answer here may be simple where you just have to simply avoid the foods that are irritating you.
And I don’t know that you would need a prokinetic. We discussed others that you can try in the podcast before, herbal, Iberogast, or MotilPro, pharmaceutical low-dose erythromycin, low-dose naltrexone, low-dose Resolor, but if you have a semi-immediate type reaction to these foods, which it sounds to me like you do, I’m not sure on this. But it doesn’t sound to me like you’re slowly getting worse month after month and then two to three months later, you’ve kind of regressed. It sounds you have a fairly immediate response. And I’m not sure that a prokinetic is a solution to that. Because remember, prokinetics prevent SIBO relapses which are usually gradual. They’re not instantaneous. So again, just because you’ve heard that probiotics can be helpful for SIBO, there’s a lot of assumptions that you’re drawing, I’m thinking anyway, that would lead one to conclude that you actually need a prokinetic.
So you may but if you’re presentation is a sudden reaction to foods, it may be that your SIBO a) is not cleared or b) that it’s not SIBO entirely. If you’ve cleared SIBO or if you don’t have SIBO and you’re having these immediate reactions to foods, then it’s not a SIBO problem, which means that lack of motility is not the issue, because a lack of motility will eventually cause SIBO to slowly creep back. So I would find a clinician or use my book. And again, what’s probably happening here is if it’s not SIBO, you may just have not struck the right balance in your microbiota and with your gut immune system. And that may be underlying where these reactions are coming from. So it can be sorted out. It’s just you have to work through some of the stuff and figure out what your specific gut and your gut ecosystem needs to be more harmonious.
Episode Wrap-up
All right, well, that takes us to the end of my list. Thank you guys for your support of the podcast. Keep your questions coming. Sorry, I got a little bit behind on these trying to get the book out the door here, and that’s on its way. And, yeah, I will talk to you guys next time. All right, thanks. Bye.
What do you think? I would like to hear your thoughts or experience with this.
- Get help using this information to become healthier.
- Get my free gut health eBook.
Dr. Ruscio is your leading functional and integrative doctor specializing in gut related disorders such as SIBO, leaky gut, Celiac, IBS and in thyroid disorders such as hypothyroid and hyperthyroid. For more information on how to become a patient, please contact our office. Serving the San Francisco bay area and distance patients via phone and Skype.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!