Tips for Recurring SIBO
Today I answer a listener question regarding what causes recurring SIBO and tips for if this is you. The good news here is if you understand some key fundamentals you can overcome recurring SIBO and digestive symptoms.
Dr. R’s Fast Facts
Identify if This is Actually SIBO
- A flare of digestive symptoms does not mean that you have SIBO.
- A flare of digestive symptoms doesn’t necessarily mean anything’s wrong or broken.
- Even if you have a flare of digestive symptoms that correlates with a SIBO breath test being positive, that doesn’t necessarily mean anything is wrong or broken but rather there’s an imbalance that can be rectified.
If You See Positive Lab Work and Your Symptoms are Flaring
- Level one – check in on your diet and lifestyle
- If you have become too liberal with foods and are not getting enough sleep, you may want to revisit a Low FODMAP diet and make sure you are resting well and keeping stress at bay.
- Level two – Probiotics are probably the best support, both for initial kind of foundational support, both for cleaning SIBO out of the small intestine and for helping one to get to a point where they have less symptoms.
- Level three – You may want to consider antimicrobials
- herbal therapy or antibiotics
- Level four – what can be used preventatively to prevent SIBO from recurring?
- herbal or pharmaceutical prokinetic therapy can be helpful
Underlying Cause of SIBO
- These therapies have been shown to loosely increase one’s risk for SIBO recurrence
- Use of acid-lowering medications like Prevacid, Nexium
- Immunosuppressive drugs
- Certain types of intestinal surgery
- The condition known as impaired motility—this is where things slow down in the intestines and this may allow SIBO to recur
Keep in Mind
- Remember that you could be having a regression of your symptoms, an IBS-like regression of symptoms, not regression of SIBO
- It’s important to not think about your gut health exclusively through the lens of SIBO
- My book Healthy Gut, Healthy You can help walk you through these steps
- Get help with recurring SIBO.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Dr. Michael Ruscio: Hey, everyone. This is Dr. Ruscio. Let’s today discuss a question regarding recurring SIBO. And I’d like to play you this question from one of our audience members.
Mike: Hey, Dr. Ruscio. It’s Mike in NYC. Just a quick question on SIBO. Do you find that SIBO is usually recurrent in your patients? And if so, does this suggest a deeper root issue than just treating the SIBO alone? In other words, if SIBO is recurrent, can you speculate on some possible root issues like what could be at the center of recurrent SIBO? Thank you very much.
DrMR: Ok. Good question. Understandable question. And there’s a couple factors to address even before answering that question which is, is this actually SIBO. Because I think we’ve come to a point now where people are blaming SIBO for more than SIBO is actually causing.
And I think we’ve gotten to a point in the healthcare culture where SIBO has generated too much momentum. I’ve been very thankful for the awareness about SIBO, but now I think people are blaming SIBO for everything, even when they don’t have SIBO. And it’s almost become this mystical or somewhat mythical figure in healthcare. And it’s important to have an accurate understanding of what SIBO is, what SIBO is not and not just be attributing any flare of symptoms that you’re having to SIBO.
So let me put a few bullet-points up here on the screen. First, identify is this actually SIBO. A flare of digestive symptoms does not mean that you have SIBO. And a flare of digestive symptoms doesn’t necessarily mean anything’s wrong or broken. Or even if you have a flare of digestive symptoms that correlates with a SIBO breath test being positive, that doesn’t necessarily mean anything is wrong or broken but rather there’s an imbalance that can be rectified. And that’s important to keep in mind because sometimes people have a fear of SIBO.
So I want to make sure to clarify that if you do actually have documented SIBO as a cause of your symptoms, don’t get overly concerned about that. It’s something that’s very treatable and manageable. Yes, there are some severe cases, but for the most part, what I notice in the clinic is people have a far more fearful reaction to being diagnosed with SIBO than they likely should. So don’t be afraid of SIBO.
So if you do have a flare of symptoms or show a regression of SIBO lab work plus symptoms—again, sometimes it’s just your symptoms flaring and it’s not SIBO. Or sometimes you may see lab work positive and your symptoms flaring. If that does happen, there’s a few things that you can consider in terms of what you can do, and then I’ll come back to what the underlying cause or causes may be.
Level one would be to check in on your diet and lifestyle. And this is important because what happens sometimes is people have become too liberal with their diet or with their lifestyle. So if someone got themselves to a point where they were feeling well, they may have been eating a cleaner diet, getting more sleep, exercising, managing stress. And now that they’re feeling good, they’re doing more, sleeping less, exercising less, eating out more, eating less healthy foods, which I think is a good thing. Don’t get me wrong. I think that’s a good thing to move in that direction.
However, sometimes if you go too far for too long, you regress your gut because you’ve done too much. And I use this example often. It’s like if you had a knee injury and you did rehab and you got yourself back to exercise or back to sports but you overdid it, your knee may start to ache again. And what you’d have to do there is go back to some of your rehab exercises, perform a little less activity. And in a little while, you’d be right back to normal.
So sometimes, all you have to do is tend to your diet. That may mean that you’re eating too much sugar, too much processed food. If you had done a paleo diet or a low FODMAP diet, you may be consuming too much non-paleo-compliant foods or high FODMAP foods. And just simple adjustments there of reducing some of those things can be helpful in some cases.
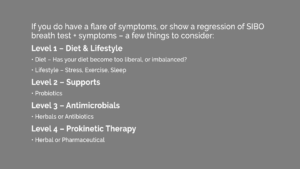
If that still doesn’t work, then level three of therapy could be antimicrobials. And this could be herbal therapy or antibiotics. And then level four, what can be used preventatively to prevent SIBO from recurring, if it is in fact SIBO, which it’s important that you quantify that it actually is, then herbal or pharmaceutical prokinetic therapy can be helpful.
So those are some things can be helpful. And if you’ve already had SIBO and you’re wondering about recurrence, then sometimes, to put it quite simply, what can be helpful to prevent that recurrence is just a short re-visitation of the therapy that got you to a healthy position in the first place. So if a paleo diet plus probiotics got you healthy, you may just need to revisit paleo plus probiotics.
If you had to do low FODMAP plus herbal antimicrobials, you might need to revisit a low FODMAP diet plus a small-dose, short-course of antimicrobials. So sometimes the solution is one that you have already discovered and just needs a re-visitation, just like doing some of the rehab exercises for your knee if you were to have a flare.
Regarding underlying cause of SIBO, use of acid-lowering medications like Prevacid, Nexium, have been shown at least loosely to increase one’s risk for SIBO, as have immunosuppressive drugs, as have certain types of intestinal surgery, and as has the condition known as impaired motility—this is where things slow down in the intestines and this may allow SIBO to recur. I think that mechanism is actually over-popular compared to how much utility it can actually serve for people. But those are some of the underlying causes. What you do about that is really codified into that steps one through four that we just went through.
Now, also remember that you could be having a regression of your symptoms, an IBS-like regression of symptoms, not regression of SIBO. And for symptomatic regression, diet, lifestyle, stress can all be factors that can lead to symptomatic regressions. And also, for the symptoms specifically, pain-signaling may be one factor that’s an underlying cause of people who have sensitive guts. So sometimes its easy to blame SIBO—and I think that gives us an overly narrow perspective on gut health. There are multiple factors that can lead to one’s gut health.
Someone who’s hypersensitive to pain, it may lead them to have periodic regressions. And there’s a couple of solutions for that. Probiotics is one. Low FODMAP is another. Again, another reason why it’s important to not think about your gut health exclusively through the lens of SIBO.
So my advice would be to listen to your gut and work to provide the optimum environmental support to allow a healthy gut and a healthy gut ecosystem to exist. This is much broader and less reductionistic than thinking about just one underlying factor such as SIBO or such as SIBO being caused by a motility impairment. And this is a mistake in thinking, trying to reduce the gut down to one thing that might be in vogue at the moment, right now it’s definitely SIBO. And SIBO certainly can be important, but we can’t reduce everything in your gut: the highest density of immune cells that you have in your entire body, the multitude of bacteria, the thousands of bacteria species plus fungal species plus how they get along with your gut plus how you digest foods plus how certain foods jive with your immune system plus your genetic pain signaling propensity.
We cannot reduce all that down to one thing. So while it can seem scientific and seem like a good idea to try to focus on SIBO and get really deep into one factor, I think the best success comes when you look at your gut broadly. So, again, I’d recommend that you do not focus on just one thing but rather what combination of environmental factors will present the best stimulus to your gut to have a healthy gut, healthy gut immune system, and keep you devoid of symptoms.
And if you focus on a broad, holistic approach to your gut health, then you should be able to come out on top, meaning you have a minimal, if no, symptoms. And if you do have an occasional regression, that’s actually ok. It’s not a big deal, and sometimes we just have to revisit a therapy for a bit of a touch-up. And it doesn’t mean anything is wrong or broken.
So hopefully that helps, Mike, and hopefully this helps you get healthy and get back to your life.
What do you think? I would like to hear your thoughts or experience with this.
- Get help with recurring SIBO.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Dr. Ruscio is your leading functional and integrative doctor specializing in gut related disorders such as SIBO, leaky gut, Celiac, IBS and in thyroid disorders such as hypothyroid and hyperthyroid. For more information on how to become a patient, please contact our office. Serving the San Francisco bay area and distance patients via phone and Skype.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!