Listener Questions – Rotating Prokinetics for SIBO, Finding Your Ideal Carb-Fat Ratio, Tips for Healthy Skin & The F/B Ratio for Weight Loss
Today I will answer more listener questions regarding;
- Rotating Prokinetics for SIBO
- Finding Your Ideal Carb-Fat Ratio
- Tips for Healthy Skin
- The F/B Ratio for Weight Loss
I’ve heard that the problem with prokinetics is that they stop working after a while. I’m wondering if rotating prokinetics would alleviate the problem?
- Open to rotating prokinetics. Prefer the idea of retreatment with low dose therapies, but either or both can work.
- There is no data to support if the natural agents work, although they likely do.
Efficacy of Bioidentical Hormone Replacement Therapy for traumatic brain injury (TBI)
- Here are a couple of studies that show that growth hormone has helped with TBI
- Recommend working with a well-trained chiropractic neurologist and a growth hormone specialist
- Also, take a look at or try to work with Cavin Balaster who was recently on our podcast
My heritage involves over 8 different nationalities and 4 different continents, how do I apply the discussion you had on the podcast about carb intake as it relates to geographic location from the equator?
This question is referencing the study about latitudinal discrepancy in macronutrient consumption, showing the closer to the equator you live, the higher carb/lower fat diet indigenous populations would eat and the farther away from the equator, north or south toward the poles, the lower carb/higher fat diet is consumed when there is no ability to intervene with stores or modern food preservation methods.
- This illustrates a point, not a rule, that there is not one best diet for all.
- Different populations can do better on different diets
- Experiment to find what works best for you.
Any insight on how to treat Dermatitis Herpetiformis? Is it a form of celiac disease I’ve seen some studies that indicate it may not be. Avoiding wheat and beta glucan seems to help. Any other guidance that I can take back to my doctor?
- Try a gluten free or gluten reduced diet to see if that works for you. If you do not derive benefit then you can continue eating gluten.
- Take a look at this study and a full write up here
- Overall a good starting point is improving your gut
- Consider a low FODMAP diet
- Investigate possible dysbiosis in the gut
- A low histamine diet may be something to consider too
- Consider a modified fast or Elemental Heal
- Sun Exposure
- Try a few minutes (15 min) of sun exposure daily (between 11:00-2:00 PM)
- If it helps – continue, if it irritates – discontinue but try to get some sun.
- Try a few minutes (15 min) of sun exposure daily (between 11:00-2:00 PM)
We are trying to figure out an issue with our daughter, her Firmicutes/Bacteroidetes (F/B) ratio from a Genova GI stool test. She has Hashimoto’s and is starting to struggle with weight even though she’s an athlete and eats the Autoimmune Paleo diet (AIP).
Her functional doctor has her taking a “very good” probiotic and we think it may be causing weight issues for her because when she ran out for three weeks, she was finally losing inflammation, and when she re-started it without any other med/supplement changes, her weight has started to go up.
Her F/B ratio is 4 (very low) in the range of 12-620. We are also considering that she may have histamine issues with the probiotic. Any insight with the ratio and if you think this is a possibility would be so wonderful! Is a low ratio just as telling for weight issues as a high ratio or do you think that is totally outdated?
- See an earlier podcast episode on Microbiota and Obesity; What You Haven’t Been Told – Episode 40
- The AIP diet might be too restrictive for a young girl, this could put her at risk for eating disorders
- If removing one or two ingredients from the diet shows great benefit, then it is ok to continue but to remove several foods without deriving benefit can be too restrictive.
- Though there is a known connection between Thyroid AI and gluten sensitivity, it affects a small percentage of people. She may not need to remove gluten.
- Here is an earlier podcast with more details on the subject of Gluten Sensitivity – Prevalence & Association with Thyroid Autoimmunity
- Treat the patient not the labs.
- Consider stopping that category of probiotics and try a different one. Continue to have her thyroid monitored.
Experiment with diets, macros and other gut healing interventions. Test less. See the protocol in my book Healthy Gut Healthy You for a step-by-step guide.
In This Episode
Episode Intro … 00:00:39
Rotating Prokinetics … 00:00:50
Bioidentical Hormone Replacement Therapy … 00:09:05
Latitudinal Carb Intake … 00:12:30
Dermatitis Herpetiformis … 00:16:18
Firmicutes/Bacteroidetes Ratio … 00:24:42
Episode Wrap-up … 00:40:00
Download this Episode (right click link and ‘Save As’)
Episode Intro
Dr. Michael Ruscio, DC: Hey, everyone. Welcome to another episode of Dr. Ruscio Radio. This is Dr. Ruscio. And let’s fire into some more listener questions.
Rotating Prokinetics
I’ll start with one from Chris C.
“Good book. Very precise. I noticed you don’t say anything about rotating prokinetics.”
Prokinetics are just agents that can help keep food moving through the intestines at an appropriate pace, for our audience.
“Those of us with stubborn cases will be on prokinetics for some time. I have heard both Dr. Pimentel and Dr. Allison Siebecker state that the problem with prokinetics is that they stop working after a while. Dr. Pimentel is clearly knowledgeable in this area as he has followed patients with MMC problems for ten years or more.”
So for the audience and for the person asking this question, I’m already getting suspicious, from the way this question is phrased, that this person is a bit too involved in their healthcare. And I listen to how people talk and the way they write questions if it’s written very attentively because in here this person could be biasing themselves into thinking that their condition is worse than it is because they’re studying people who are studying some of the sickest people in this condition.
So already I will remain open that this patient could be one of the most severe cases. But already I’m suspicious this person has dove too deeply into the pool of research on this and may be actually detracting from their health with the information that they’re reading. And let me finish the question now.
“I’m wondering if rotating prokinetics would alleviate this problem. After a year and three months of dealing with SIBO much in the manner laid out in your book, I’m trying to be clear of bacteria long enough to tackle the autoimmunity that underlies my particular problem. I need to keep moving to breathe through my intestinal tract while my MMC is not functioning properly and am concerned about relying on prokinetics that don’t really work. Any thoughts on rotating them?”
So again for Chris, I understand how frustrating it can be not to feel well. The biggest thing here I want to make sure what does not happen is that we create a worse problem in our minds than it actually is. And that’s not to take anything away from the suffering that someone may encounter. I suffered for quite awhile. And I thought I had a lot more wrong with me than I actually did.
So to the question of rotating prokinetics, I am totally open with that. Will rotating prokinetics be the difference between success and failure? In my mind, absolutely not. It’s usually not that complex. Can it help? Yeah, I think we have one, maybe two to three studies supporting that. We don’t have unbelievable evidence. And I think that’s also important to mention.
I very much, though, appreciate the work that Dr. Pimentel has done in advancing the bacterial component of IBS. However, we also have to be careful that we don’t take a motility researcher and project the hypothesis they’re working on. In this case, of course, Dr. Pimentel is very interested in motility. And so you’ll get a lot of motility-centric information from Dr. Pimentel. Again, this is not a criticism. It’s just a statement of fact.
We want to be careful that we don’t paint all of IBS to be a motility problem, nor all of SIBO. Yes, it can be a problem. But you would think that prokinetic treatments are the most important treatment for SIBO, based upon the narrative that you receive from Pimentel and also potentially from Dr. Siebecker. But in my opinion, that’s not the case.
Again, from an evidence-based perspective, we have one good study that extended the time before a relapse but did not cure these patients of IBS, from using prokinetics, one of which is no longer available on the United States market. The other two, I believe you could make a case for, not as good of data because the study population—they were unique cohorts of patients that were being studied.
Now, also regarding natural agents, there is not one study that has shown that a natural agent can prolong time in remission of SIBO. In fact, we were trying to do that study, and we hit some major roadblocks. And we are still trying to do that study to answer the question because I really would like to know. I’m inclined to think if or when we can complete that study we will show that the natural prokinetics also work.
But rotating the prokinetics—no problem. But what I found is that many patients require finding what factors work for their gut and then occasionally repeating what works. So you may do very well on antimicrobials. And you may occasionally need a low dose of antimicrobials in the future on a periodic basis. Or if you’re uncomfortable with antimicrobials, you can periodically use a two-to-four day, or even one day, exclusive elemental diet as a reset. Or you can use the elemental diet in a hybrid application.
Now, also don’t forget the aspect of friends, family, relationship, purpose, stress management. I get the sense that—again, given the detailed level of this question and the assumptions that are being made—that we have to be on prokinetics long term, we have to rotate them. I have to fix my autoimmunity.
Has that autoimmunity even been tested? Or is it presumed? It seems there are a lot of presumptions in this question that make me suspicious that the person is essentially reading the information at a doctor-training level without the other contextual information that doctors have, which is the incidence and prevalence. And that can very easily mislead someone into thinking that there in a worse position than they actually are.
So yes, you can rotate prokinetics. I would also make sure to keep in mind all of the other things that I mentioned because sometimes the difference between success and failure is not a better treatment per se. But it’s better utilizing the available treatments in combination with a little bit of a head check. And I don’t say that in a flippant way. For some people, this shifting of paradigm or focus can be a hugely cathartic endeavor.
So yes, you can rotate natural prokinetics. I have no problem with that. You can rotate natural and pharmaceutical. Just keep whatever doctor you’re working with in the loop. If you’re not working with a doctor, I would definitely work with a doctor or go through the protocol in my book.
But also remember that there may be other things at play here that have eluded your gaze, especially if your gaze is very SIBO-centric and narrow in focus. So this is where, if you haven’t brought in a good clinician, that may be a good idea to do so.
So I hope that helps, Chris. And again, I want to be very careful in saying that none of my remarks are meant to be criticisms. But they’re meant to be hopefully guiding lines I’m throwing you to help you not get too deeply focused on one area, potentially missing another. And ironically, that would be an example of us being too reductionistic and not being holistic enough. So any case, hopefully, that helps.
Sponsored Resources
Hey, guys. We’ve discussed at length the benefits of probiotics. But it can be hard to know which specific probiotic products to use. One probiotic that I endorse is Just Thrive Probiotic. Just Thrive is one of the few category three (aka soil-based) probiotics I recommend. In fact, one exciting study has found that the strains in Just Thrive Probiotic can begin healing leaky gut.
They also have some very exciting research coming in the future. If you haven’t listened to our podcast with Kiran Krishnan who is performing some of this research, you should definitely check it out.
And good news! If you’d like to try Just Thrive, they’re offering 25% off your first purchase when you use the code RUSCIO at checkout (R-U-S-C-I-O). They’re available at ThriveProbiotic.com or on Amazon. Check them out.
Bioidentical Hormone Replacement Therapy
DrMR: Okay. The second question is regarding bioidentical hormone replacement therapy for traumatic brain injuries. And let me play this one now.
Listener: Hey, Dr. Ruscio. Recently, I became aware of bioidentical hormone replacement therapy for traumatic brain injury. I know that you are very science-based and are rigorous about your research and what works. So I’d like your input on this interesting new therapy. Or maybe it’s been around for awhile. I don’t know. Just to get your input on what the efficacy is and whether it’s safe. Thank you.
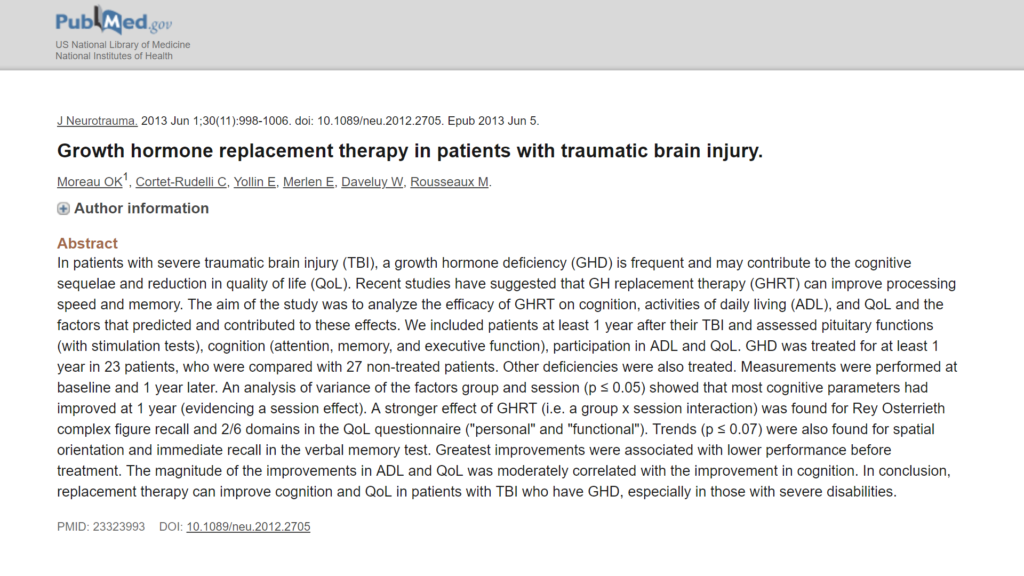
DrMR: All right. So there is our next question. Now, I don’t know the nuances of this argument. I don’t deal much with brain health directly per se. The gut-brain connection, absolutely. But I was able to find two papers that did find that growth hormone replacement therapy was able to assist healing in TBI (or traumatic brain injury).
Now, usually the term “bioidentical hormone replacement” refers to potentially growth hormone but oftentimes some of the steroid hormones, like your testosterones, estrogens, progesterones. But there is some evidence showing growth hormone.

I would potentially consider working with some type of neurologist. I think a well-trained chiropractic neurologist can be worth his weight in gold with helping with TBIs. And so you may want to look into the Carrick Institute.
I would also be a little bit careful. Sometimes the Carrick training seems to make things a little bit overly complicated. And that can trickle down into providers making their care recommendations a little bit overcomplicated also. So you’d want to look for someone, just like in functional medicine, who is going to be a bit of a bottom line, get-to-the-point kind of person and is not going to pull you into all this academic rigmarole.
Talk with your doctor. Or find potentially an anti-aging doctor who may have some degree of familiarity with this, with the growth hormone that is, and bounce it off them and see what they think. And also consider a chiropractic neurologist in addition to just following up if you’re working with your PCP or your neurologist to have both your traditional, conventional scope covered and then also some items that are a little bit more integrative. And hopefully, that will help you get there.
Also, one final thing I should mention is Cavin Balaster who was on the podcast recently himself suffered from a TBI and wrote a book on it. And he may be a good person to reach out to because he may have some clinicians or associates or doctors who are fairly well plugged into this. So hopefully a few things there that can help get you on your way.
Latitudinal Carb Intake
Next question is submitted by Richmond. And he asks,
“Hi. I would be remiss if I didn’t make a comment somewhere. This is my second ever public statement ever. Partly listened to your podcast tonight. And thinking about the conversation discussing carbohydrate as it pertains to percentages as you move from the equator and how this influences your diet based upon the position on the planet you evolved from. What about us souls that have over eight different nationalities and four different continents going on? That may create complexity in your bio-rules. I’m sure you’ve already gone on this road, but far and few between fall into the perfect plain vanilla anymore. It would be wonderful if you gave me a response. Would love to keep the dialogue going.”
Okay. So great question. Yeah, it’s a question you get a lot. And there’s a simple answer. The latitudinal discrepancy in macronutrient consumption that was laid out by Cordain and others essentially showing that the closer to the equator you live, the higher-carb, lower-fat diet indigenous populations would typically eat. And then the farther away from the equator you go north or south toward the poles, the lower the carb and the higher the fat diet tends to be when eaten by indigenous populations, when there’s no ability to intervene with grocery stores and modern food preservation methods.
So this is a point. It’s not a rule. And the point is hopefully meant to illustrate that there is no one best diet for everyone. But rather, different populations can do better on different diets. And this should hopefully shoot a big hole in the argument of, “We should all be vegetarian. We should all be Atkins. We should all be Pritikin. We should all be Mediterranean. We should all be paleo. Or we should all be low carb or high carb.” The basic macronutrient is what this may boil down to. And there are differences depending on someone’s genetics.
Now, if your genetics are mixed and even if your genetics are not mixed, you want to go through the same process of just understanding that people are different and do some self-experimentation to figure out what works well for you. That’s been one of the most consistent recommendations I have made across almost everything, which is listen to your body. Experiment, observe and adjust.
So experiment to find what works well for you, just like I lay out in Healthy Gut, Healthy You. There is some important background that you need to get to a certain level of health before you’re well able to listen to your body. But once you clean out some of the imbalances and de-inflame and address any dysbiosis if it’s present, then you get a much better ability to tune into the signals that your body is sending you.
And then that’s when you can run a good experiment with your macronutrients to see if you do better higher carb, lower carb. Or if you’re someone who has a healthy metabolism, you can probably get away with either. Or you may even oscillate as the seasons progress, as some people recommend, eating higher carb in the summer and essentially lower carb in the winter.
So yes, there is no right answer here. It’s not to say if you’re of Venezuelan descent and you feel terrible on a high carb diet you should eat a high carb diet because of this observation.
And to your point, many people will have a mixing. So let your body tell you what to do. Listen to your body. But perhaps run through a little bit of maintenance before you do that so that you can get a clearer signal from your body that’s not confounded from the noise of eating inflammatory foods or having an inflamed gut or what have you. So Richmond, hopefully, that helps.
Dermatitis Herpetiformis
Okay, next question is about dermatitis herpetiformis. And this is essentially, for lack of a better term, when people have lesions on their skin—pimples and rashes. And here is the question from Jay.
Jay: Hey, Dr. Ruscio. This is Jay. I really appreciate the show and your science-based approach. Really great. I have dermatitis herpetiformis.
And I’m wondering if you have any insight as to any things that can be done with that or things I could take to my doctor to try, as in the research I’ve noticed that a lot of people say it’s a form of celiac disease. But there’s at least one study showing that the presence of gluten doesn’t actually make that big of a difference in terms of whether or not it heals.
So I’ve also noticed in myself avoiding wheat does help but also it flares when I use something that contains beta glucan. So I get those blisters on my body. So just wondering if you had any other insight besides just avoiding things with beta glucan and wheat and things like that. Thanks a lot.
DrMR: So another good question. And you’ve already hit two major things which are you’ve noticed in your own experience that gluten seems to flare it as do certain prebiotics, the beta-glucuronidase (or beta glucan). So I would start there.
Now, I have not done an exhaustive review of the literature to see what the relationship between gluten and dermatitis herpetiformis is. I’m assuming what you would find, if there has been a systematic review and/or meta-analysis published, would be, yes, there is mixed data. There is rarely ever 100% uniformity in a body of data. But we would see that there is suggestion that people do better avoiding gluten who have dermatitis herpetiformis.
Now, I want to be careful in saying that there’s a difference between reducing gluten and being 100% gluten free. You may be okay with a gluten-reduced diet where you can have gluten but you make it only on occasion. And maybe you suffer a little bit of a repercussion when you do.
But you find the right balance for you in terms of, “Okay, I’m not going to do this often because it’s a little bit annoying when my skin looks a bit broken out for a couple days afterward. But every once in a while in X, Y, or Z context, it’s worth it for me.”

And I’ll put a graph in here. And I’ll link to the study and also the write up of this study (subscription required) that appeared in the Future of Functional Medicine Review clinical newsletter. This is the multi-center Italian study that looked at 12,225 patients. And they were able to break down in 486 patients extra-intestinal manifestations of non-celiac gluten sensitivity. This is what makes this novel. This is non-celiac gluten sensitivity.
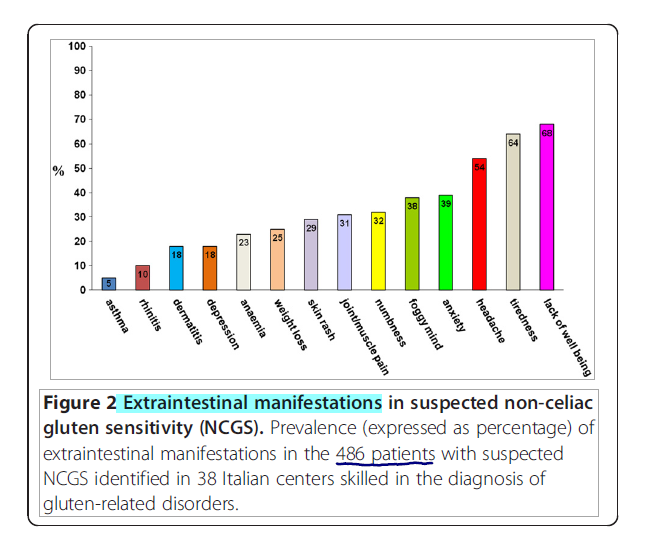
I’m assuming you do not have celiac. So the celiac data may not fully apply to you per se. But non-celiac gluten sensitivity may be more relevant. And they found an 18% occurrence of dermatitis in those with non-celiac gluten sensitivity. So that’s certainly something. I would start there. And you’ve essentially already started there. I would continue there to find what works for your body.
Now, what’s interesting about this particular study is they found that up to 30% of cases of non-celiac gluten sensitivity were actually being driven by another problem in the gut like carbohydrate malabsorption or potentially a bacterial overgrowth.
So to your next point, this ties in. The beta glucan intolerance, or prebiotic intolerance, may indicate firstly, simply that you may be a bit FODMAP sensitive. The fact that someone is FODMAP sensitive in my mind does not guarantee that they have other items present like small intestinal bacterial overgrowth. It suggests that that could be the case. But I don’t want to contribute to this ethos in functional medicine that if you have a symptom it means 10 things are wrong with you. You may just be a little bit sensitive to FODMAPs. And it may not be a huge deal.
But a low FODMAP diet would be something to try. And also investigating any kind of dysbiosis in your gut, which includes SIBO, would also be something to consider.
Now, clinically I agree with the old adage of natural medicine which is, “The skin is a reflection of the gut.” In your experience and also some of the literature reflects that, especially the celiac/ non-celiac gluten sensitivity connection to dermatitis herpetiformis. So skin, gut—there’s a connection. FODMAP would also be something to consider. I don’t know of anything published there. But certainly clinically, I’ve seen that.
In that same web of causality, we have histamine. And dysbiosis in my mind certainly can fuel histamine. We know that a low FODMAP diet has been shown in at least one trial to cause an eight-fold decrease in histamine. And a low histamine diet would also be something to consider.
So what this all boils down to conceptually simply is improving the health of your gut. And in Healthy Gut, Healthy You, I lay out the best possible approach I could come up with to achieve that endpoint. You may be able to completely rectify your gut imbalances, if you will, and help your skin by simple dietary modifications. You might need diet plus probiotics. You might need diet, probiotics, plus herbal antimicrobials or occasional liquid fasting with a modified fast or even with an elemental shake like our Elemental Heal. But the book protocol will help you get there.
And there are, I believe, some topical treatments recommended. I’m not very well versed in those. Exposure to the sun may help with dermatitis herpetiformis. I can’t recall. There are so many different conditions that have been looked at regarding the sun. I would certainly say try some reasonable sun exposure. If it seems to help your skin, continue. If it’s one of the rarer conditions that seems to flare from sun exposure, like melasma, then I’d still get some sun exposure. But I’d be a little bit more measured in that.
But essentially, start with your gut. And that can go a very long way. We see some of the published literature starting to reflect that certainly. And I’ve seen a number of patients who’ve had everything from dermatitis herpetiformis all the way through paradoxical, unidentifiable skin conditions that have improved after improving one’s gut health. It’s not a guarantee. But it’s certainly a great place to start.
Firmicutes/Bacteroidetes Ratio
Okay. Our last question comes from Mary Reynolds. And she asks,
“Hi. Thank you for such an informative article. We are trying to figure out an issue with our daughter’s F/B ratio from a Genova stool test.”
F/B is the Firmicutes/Bacteroidetes ratio. We’ve talked about this in the past on the podcast.
“She has Hashimoto’s and is starting to struggle with weight even though she’s an athlete and eats the autoimmune paleo diet.”
I’m going to stop there for one minute. So a young girl on the autoimmune paleo diet is probably a bit too restrictive. I hope you don’t have your daughter on the autoimmune paleo diet for her Hashimoto’s because in my mind that would be a mistake. We do know that the incidence of eating disorders increases in children who have to be on diets. I would be very careful. And I would not be overly idealistic here and have your child go on any dietary restriction that she does not notice clear benefit from.
And that includes gluten. Yes, there is an association. Coming back to that study in Italy I mentioned a moment ago of 12,225 patients. They found that 3% of those patients surveyed—so 12,000 patients were surveyed. 3% of those had non celiac gluten sensitivity. Of that 3%, 14% had autoimmune conditions, and about 9-10% were thyroid autoimmunity.
So is there evidence documenting the connection between gluten, non-celiac gluten sensitivity, and thyroid autoimmunity? Yes. Is it 100%? No. Is it even close to 100%? No.
Now, people will criticize. And they will say, “Well, what about the United States? There’s more glycophosphate used. And it’s different wheat. It’s more GMO. It’s more processed. There’s more gluten.”

Okay. Well, the data, as far as I understand it, in the United States documenting non celiac gluten sensitivity ranges from 0.6% of the population to 6% of the population. Now in Italy, it was 3. So even if we doubled these—so even if Italy is three. And let’s say, best case scenario (or worst case scenario, depending on your vantage point), that in the United States it’s 6%. So you can double from 3 to 6.
So all the percentages I give you, we could double. So instead of 14% of people having autoimmunity, it was 28%. And instead of 10% of people having thyroid autoimmunity, it became 20. That is still far from 100%.
So does that mean that this could be an issue? Yes, absolutely. You’ve got my support. You’re preaching to the choir. I get it, guys. We want to use diet and natural medicine wherever we can. Do we want to indoctrinate people into thinking that everyone has to be gluten-free and potentially have a negative impact on a child’s life and potentially put her at greater risk for an eating disorder because of that? No, we absolutely don’t.
How do we solve this quandary? We use the person’s response to navigate this landscape. So if she feels better off a food, have her avoid that food as much as she can. If she doesn’t notice anything, she can eat the food.
How to interpret the thyroid antibodies, I’ve talked about in other posts. So I’ll direct you to those posts. But remember that if your child does or does not eat gluten or nightshades is not going to be the difference between her having a frank thyroid problem or not. Could it help? Yes, but likely—and this is where I’m speculating a little bit. But I’m drawing inferences as responsibly as I can from the literature.
If she has a problem with gluten, it will almost certainly be manifest symptomatically. And to say that she will have silent progression with no discernible symptoms I don’t think is valid. And that’s why this same Italian study—again, over 12,000 patients rigorously tracked, monitored, and followed—showed that they had a reaction to gluten, a discernible, symptomatic reaction to gluten, some type of symptom, anything from bloating to brain fog within 24 hours of ingestion of gluten.
So for those people, I would say, yes. Avoid gluten. Perhaps it’s fueling your Hashimoto’s because you’re not feeling well on it. But if you’re eating gluten and feeling fine, I’m hard-pressed to lay someone underneath that heavy dietary restriction.
Okay. So continuing on with the question here. Sorry. Sometimes, I get lost in this context. But it’s important.
“Her functional doctor has her taking a very good probiotic. And we think it might be causing weight issues for her because when she ran out of the probiotic three weeks ago, she was finally losing inflammation. And then when she restarted on the probiotic without any other changes, her weight started to go up again.”
That could be possible. The majority of the studies have shown probiotics can lead to a small—we’re talking 2, 3 pounds—of weight loss. One study recently did show a slight weight gain from probiotics. So it is possible.
This is why I always recommend that people use their body’s response to determine where they fall because guess what? The scientific evidence can guide us. But we never get a 100% answer with the research because people aren’t the same. And rather than arguing over who’s right or who’s wrong, let’s use that energy to try to help people find where they should be on a given side of an argument—on probiotics or not on probiotics, as an example.
In this case, I would recommend not using that probiotic. Of course, clear this with her doctor or whatever clinician is guiding you. Trying the other two categories of probiotics. I’m assuming that he or she has your daughter on a category 1 Lactobacillus/Bifidobacterium probiotic. But if not, whatever category the probiotic falls into, stop that category. Try the other categories to see if you can garner a benefit. If so, continue. If not, stop.
And then let’s continue the rest of the question here.
“Her F/B ratio is 4, very low. We are also considering that she may have histamine issues with the probiotics,” because of the probiotic response. Probiotics contain histamine. “Any insight with the ratio and if you think that this is a possibility, it would be so wonderful. Is a low ratio just as telling for weight issues as a high ratio? Or do you think it’s totally outdated? Thank you very much in advance.”
Okay. So we’ve already spoken to some of that. The F/B ratio in obesity, in my opinion—and this has been corroborated by probably one of the leading experts in the world on microbiota research specifically, Professor Robert Knight. I’ve linked to his last appearance on the podcast where he corroborated this—the data is just not there in humans. It’s very mixed.
And this is truly mixed. And this was actually a section of the book. And I cut it out because it was just too detailed. But if you look at the data, you see a pretty much 50/50, maybe even a 60/40 weighting showing that this ratio is not valid in humans. That may have skewed a little bit since a year ago when I was writing this. But essentially, it doesn’t seem to be a consistent corollary to weight in humans. That’s just correlation. We haven’t even gotten all the way to therapeutics yet.
Okay. Now, here’s something else interesting. Recently, I was at a seminar. Appreciate what the gentleman was trying to do who was teaching the seminar. I want to be careful here because I realize that I’m in a fortunate position where part of my job is to be learning all the time and then be on the cusp of this.
So I don’t want to knock a clinician who might be in the clinic five days a week, also trying to teach and share what he’s learned but doesn’t have the luxury of having some research assistants behind him and a couple days off of the clinic a week where he can delve into this stuff. So I want to be appreciative on the one hand. But also, we need to be correct on the other hand.
He talked about the F/B ratio. And again, there was excited sharing of some of the cherry-picked data. Again, it probably not was intentionally cherry-picked. But what happens here is people get excited about this. They write about it. And the cherry-picking feeds itself. So there’s a citing of the F/B ratio, its promise for obesity, yada, yada, yada. All right.
So he also cites a study showing that glutamine could improve the F/B ratio. So what’s the first thing we should be asking? If glutamine improved the F/B ratio, did it lead to a change in weight? This was left out of the narrative at the seminar, really unfortunately.
So the F/B ratio improved. And I’m going to pull up a quote. “We did not observe any difference in body weight, waist circumference, or fasting serum glucose between the two groups.” So this is why I get so frustrated when people cite mechanism instead of citing outcome. And people do! A decent proportion of functional medicine burns people’s money and resources with this kind of nonsense—the nonsense of looking at mechanisms that could be promising but not being a cautious, careful scientist and reserving recommendations until there’s something solid to move on.

And if you’re saying to yourself, “Well, what about being progressive and being ahead of the curve?” I’m all for that, guys. But there are things that do work for weight loss, for improving gut health. And in my observation, clinicians could do themselves a huge favor by mastering what does work rather than muddling in the things that may work. And that’s the big miss I see many clinicians making. They get so distracted in the new and novel. And they bumble. And they don’t even understand the therapies that have been shown to work.
And that’s the big problem. If you have a solid foundational understanding and mastery of the therapies that do work, okay, then you can be progressive in a certain time at a certain place.
But unfortunately, it’s like an inverted pyramid where we’re trying to balance a pyramid on its peak and bumbling through the non-valued therapies at the expense of the therapies that have been validated.
Now, I should also mention that I immediately went, and I checked. And I said, “Well, if glutamine is something that can lead to weight loss, I want to know.” And I did find, actually, one study that found significant weight loss after utilizing glutamine. And that was the only one of its kind. I’ve got a very strong suspicion that that study was the outlier because you’re talking 3 to, I believe it was 9 pounds of weight loss. And that just seems unusually high.
And I almost don’t even want to mention that. I don’t want to put that in people’s heads that glutamine could be this miracle weight loss.
I use glutamine in the clinic with patients. And I don’t think I’ve ever heard someone remark that they lost weight after using glutamine. Given, they’re typically being given glutamine after we’ve gone through more foundational therapies that do lead to weight loss like optimizing their diet and optimizing their gut health. So I may not be seeing it because of the point at which, in the clinical process, I’m utilizing glutamine. I’m totally open to that.
But the point I’m making here is we want to be careful not to get pulled into this sort of nonsense. And right now, unfortunately, I think for your daughter, functional medicine is probably doing more harm than it is good.
I’m assuming that the functional medicine has gotten your daughter on the autoimmune paleo diet in an overzealous fashion to try to manage the Hashimoto’s. And you could probably achieve the same improvements with the Hashimoto’s with a whole lot less intervention.
And the probiotic, I would simply listen to her body. Your doctor is saying one thing. But your daughter’s body is saying another. I would reconcile those two.
And then the F/B ratio, I would not treat the F/B ratio. I would treat your daughter and see what works well for her. Focus on the health of the host. And that is the best thing to do.
Now, what does that mean? Well, it’s hard to say. You may want to first start playing around with your macros. You may want to try to heal her gut if anything is wrong with her gut. You may want to undergo fewer dietary restrictions. If she’s going low carb and taking a probiotic and gaining weight, she may do better on high carb/lower fat and no probiotics. You’ve got to do a little bit of tinkering here.
But certainly, I’d be careful how far down this path you traverse because I’m getting some early indicators that you may be chasing something that’s not really there. And so hopefully that’s helpful with the F/B ratio.
If you wanted to try glutamine, fine. Glutamine is fairly inexpensive. And it only really has any health benefit that I can ascertain. Try it for a month. See how she does. If she loses a significant amount of weight or is trending in that direction, give a little while longer or continue. And if not, discontinue.

So hopefully that helps. Be cautious with Hashimoto’s. There’s a lot of unneeded fear and overzealousness around Hashimoto’s. Yes, you want to intervene to get your daughter as healthy as possible. No, you don’t need to treat her like the most sensitive patient out there who can only eat the autoimmune paleo diet unless you qualify that that’s actually how she needs to eat. And I get the sense that she probably does not.
Also with your daughter, I’d tread lightly with this stuff. Functional medicine uses a lot of terms and diagnoses that sound scary. And children, I think, have the least ability to discern, how is this any different from cancer or heart disease or what have you? So I really try to tread lightly with patients.
And something I think is helpful to say—if you can only do one thing, if you can only go in one direction, you can’t hit perfect. You can only shoot a little over or shoot a little under. I’d always rather a patient leave an interaction with me feeling healthier than they are rather than feeling sicker than they are because we know that someone’s self-perception of their health has a measurable impact on the outcome of their health.
So rather than trying to tell someone, “Oh my god. You have Hashimoto’s. You need to do this. This is a big deal. Blah, blah, blah.” And making them feel sicker than they are. I would use conservative language that, “Oh, we found some inflammation in your thyroid gland. You may benefit from not eating these things or reducing them most of the time. But the good news is that with your levels, the chances of any problem popping up in the future are mild.” Or moderate, depending on the level of elevation of the antibodies.
Episode Wrap Up
And I know some of that is more clinician speak. But the point I’m making is I think we should start using language in such a way to help people walk away from a conversation feeling empowered and hopeful rather than fearful because, again, your self-perception of your health does affect your health outcomes.
And I really applaud Dr. Brian Walsh for bringing some of that information to my attention. So this is serious stuff, guys. And hopefully, this is helping. If I’m getting too in the weeds here and too theoretical and on top of my soapbox too much, please let me know. And I’ll reel it in. But hopefully, this is helping.
And this has been another episode of listener questions. Thank you, guys, so much for your support and your patronage. And I will talk to you guys next time. All right. Bye-bye.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ Resources & Links
- Growth hormone replacement therapy in patients with traumatic brain injury.
- Effect of Growth Hormone Replacement Therapy on Cognition after Traumatic Brain Injury
- Carrick Institute
- How to Feed Your Brain with Cavin Balaster
- An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity.
- Elemental Heal
- Professor Robert Knight
- Microbiota and Obesity; What You Haven’t Been Told – Episode 40
- Gluten Sensitivity – Prevalence & Association with Thyroid Autoimmunity
- Just Thrive Probiotics
- Healthy Gut Healthy You
- drruscio.com/resources







Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!