Fasting and Gut Health, Finding Your Right Diet, Inflammation, and More with Melanie Avalon and Gin Stephens on the Intermittent Fasting Podcast
I was recently on the Intermittent Fasting Podcast hosted by Melanie Avalon, author of What When Wine Diet: Lose Weight And Feel Great with Paleo-Style Meals, Intermittent Fasting, And Wine and Gin Stephens, author of Delay, Don’t Deny: Living An Intermittent Fasting Lifestyle. We discussed how to fix your gut, find your right diet, SIBO, IBS, low-FODMAPs, gluten, inflammation, gut microbiome, functional practitioners, tackling food fears & more!
Episode Intro
Melanie Avalon: I’m Melanie Avalon, and I’m here with Gin Stephens.
Gin Stephens: Hi everybody.
MA: And I’m not just here with Gin Stephens. We have a very special guest today. We’re so excited to have him here. We have Dr. Ruscio. Am I saying it right? Is it Ruscio or “Rush-i-o”?
Dr. Michael Ruscio: It’s Ruscio. You nailed it.
MA: Dr. Ruscio. I should know that. I listen to your podcast all the time. We have him on the podcast. And I’m just so honored, so excited to have you. Thank you for being here.
DrMR: It’s a pleasure to be here.
[Continue reading below]
Dr. R’s Fast Facts Summary
Where to Start When Experiencing Health Issues
- Improve your diet and lifestyle first
- Eat whole fresh foods
- Improve sleep
- Exercise
- If not improved, start with optimizing your gut
- All detailed in the Healthy Gut, Healthy You book
Low FODMAP Diet
- Has proven very helpful for many people that are trying to heal their gut
- There is substantial evidence on the low FODMAP diet
- Reduces symptoms and inflammation
- Low FODMAP would likely be ok for long term use but clinical studies are needed
Intermittent Fasting
- Helps facilitate digestive motility
- Reduces stress on the gut (for most)
- An important part of meal spacing, codified in the HGHY book protocol
How to find a good functional medicine doctor
- Helpful guide here
Categories of Probiotics
- Lactobacillus and bifidobacterium
- Well studied, numerous clinical trials
- Saccharomyces boulardii
- A healthy type of fungus
- Soil-based probiotics
- Usually start with bacillus
- B. coagulans (most studied)
- B. subtilis (second most studied)
- B. clausii (third most studied)
- B. licheniformis (hovers around the third most studied)
- Usually start with bacillus
- E. coli Nissle 1917
- Has shown benefit in clinical trials for IBD
- Trade name Mutaflor
- Not available in the U.S.
How to find the best treatment option for you
- Listen to your body
- Try different therapeutic options
- How long to try different approaches/protocols before moving on
- For some dietary approaches it can take just a few days
- For others it could take 2-3 weeks
How to Address Your Relationship to Food
- Look at who is educating you on food, are they speaking from indoctrination or research and clinical evidence?
- Don’t listen to people on blind faith, do your own testing and see how YOU feel
- Get help with intermittent fasting.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Download Episode (Right click on link and ‘Save As’)
*Thank you to Melanie Avalon and Gin Stephens for sharing this interview with us. To learn more, visit the Intermittent Fasting Podcast*
MA: So for listeners who aren’t familiar with Dr. Ruscio, even though I imagine many of you are. Side note: We actually get a lot of questions to the podcast, and they’ll often mention things they heard on your podcast or in your book. So I know a lot of listeners are familiar with you. But for those who are not, Dr. Ruscio is a superstar, basically, in the world of functional medicine, especially when it comes to gut health. He’s so amazing, and knows so much about that. He’s a doctor. He’s also a clinical researcher, involved in clinical studies.
He hosts the Dr. Ruscio Radio Podcast, which I listen to, I would say every day. A little bit of it here and there. And then he also recently released the bestselling book, Healthy Gut, Healthy You. For really just tackling gut health through a food-based approach rather than prescriptions and pills and all the things. And it’s just really a wonderful foundation, and a wonderful resource for people to have. So thank you, Dr. Ruscio, for being here with us today.
DrMR: Thank you. That’s quite the intro. I’ll try to live up to the expectation.
MA: You already have, I promise. To start things off, I’d love to hear a little bit about your background, and how you came into functional medicine and just the whole thing.
DrMR: Sure. Absolutely. I’ll try to give you the concise version. But when I was in college, I was premed. And fairly set on going into conventional medicine. At least, I was type A. I was driven. I had a high GPA. I didn’t really have anything happen in my life to steer me in a certain niche direction in the field of healthcare. Until I went from being also a college athlete and having tons of energy and feeling great at 23 years old, to having fairly debilitating insomnia, brain fog, bouts of depression, feeling cold and lethargy.

Unfortunately, none of them could find anything. They all said, you have good blood sugar. Good cholesterol and body composition. And this is likely stress, or something else. Now, the context is I was getting enough sleep. I was studying also fitness and nutrition. So I was eating really well, and I had a very balanced life in all of those aspects.
So, they couldn’t find anything wrong. And it ended up being an alternative medicine/functional medicine provider who thought that I had a parasite. And I remember when he informed me of this, I thought he was crazy at first. I didn’t go to Mexico, and have food poisoning, and then all this started. I had never left the country. I really didn’t have any digestive symptoms, which is actually a key lesson for us, which is, you can have digestive inflammation that is silent digestively, only exhibiting itself as extra-intestinal manifestations. Fatigue, brain fog, joint pain, depression, skin lesions, what have you. And that’s what I had learned.
So I thought this doctor was crazy at suggesting this. But he turned out being right. And upon some investigation, we determined I had a parasitic infection, an amoeba. And that diverted my path into alternative and integrative medicine.
But the important aspects of the back story, don’t stop there. Because then when I got into the field of integrative and alternative medicine, I didn’t see the academic rigor that I gravitated to in the conventional medical field. And I felt like some aspects were way out over the skis. They were making claims that weren’t supported. They were making claims that seemed overzealous. And there certainly seemed to be a fair level of permeation of dogma into the field.
So there were some very good things, but there were also some things that I was cautious about. And these are the things now that I speak about in my writing, or trying to investigate with our research and I discuss in my podcast, which is essentially trying to be progressive, but also conservative and somewhat evidence based so that we can give people the most accurate recommendations so we don’t subject them to more excessive dietary restrictions than they need, more excessive testing than they need, or any other type of natural treatments that are in excess of what they need. So we can be practical, we can be precise. And we can get people well with minimal energy and time and money invested.
MA: Yeah, that’s wonderful. And that’s one of the things I really like about your approach in general, and one reason I really wanted to have you on the podcast. I love how you really look at all of the studies coming in, and you look at everything the study is actually saying. You look at all the viewpoints, and you really provide listeners and readers with a very objective interpretation, in my opinion, of everything. And let people decide for themselves where to go with that.
And I think that’s just so refreshing. Because we encounter so many biases in this world. And also people enter specialties who are convinced everything is due to one thing, and lots of restrictions with dietary habits. And just all the things. So I love the approach you bring. I think it’s refreshing.
DrMR: Thank you.
Where to Start When Experiencing Health Issues
MA: So, this is the Intermittent Fasting podcast. So we’ll probably really tackle a lot of questions about that. But before we go into the specifics, I was just going to ask you, in general. You talked about your history with your own problems, and realizing that it did involve your digestive state. And we get a lot of questions from listeners about things that you mentioned. Fatigue. Energy problems. A lot of listeners do struggle with apparent food intolerance. Things like that. So this is a very general, overarching question. But if a listener, or a person is experience health issues. And they don’t know the cause. And they don’t really know what to do. Where should somebody start? Because there is just so much to tackle, and so much you could research, and so much that you could test. What do you suggest for people as a starting guide, to finding the root cause?

Now, there’s a caveat. You have to at least have taken a couple of steps in improving your diet. I wouldn’t go into interventions to optimize your gut health if you’re still drinking soda, eating processed foods, eating at McDonalds. But I think we all kind of get that. We should at least have some of the basic bases covered in terms of taking at least some simple steps to improve our diet, focusing on whole, fresh foods. Getting enough sleep. Exercising.
After you’ve made those changes, if you’re still floundering, then I would recommend looking into your gut health. And that’s not to say that that will be a cure-all. But if you look at the probability of optimizing your gut health, and the likelihood that that will produce an improvement in your symptoms. And you weight that against other interventions. Thyroid, adrenal fatigue, metal detox, mold, Lyme, biotoxins, mitochondrial health. You have the highest probability, in my opinion, of seeing the results that you’re looking to see. Seeing your symptoms clear. After optimizing the health of your gut.
So I would absolutely start there. And then re-evaluate. And fortunately for many people, once they optimize their gut health, and they re-evaluate, they go, wow. I’m feeling good. I fixed the problem. Yay. There’s no need to dig any further.
For some people, there may be a need to dig further. But at least you checked the box of optimizing your gut health, which also tends to optimize the results of other interventions like adrenal support, or thyroid, or detox, or whatever it is.
GS: Yeah, I think that’s great. One thing, Dr. Ruscio, this is Gin. I wanted to tell you that I loved your book. And as listeners, we said it at the beginning, again it’s Healthy Gut, Healthy You. The thing I loved the most about it, I’m going to read a quote from it. This is my favorite sentence out of the whole thing. “Our goal is to get you on the broadest diet possible gradually with time and observation.” And that’s the point that people can heal their gut. And move to a diet that includes things they couldn’t include at one point. Could you talk about that a little bit?
DrMR: Great point. And thank you for the kind words about the book. We do see this, and when I say we. The published scientific literature is really starting to substantiate that people who are otherwise thought to be reactive to a food. If they can fix a problem in the gut, they can often times expand their diet, and no longer be encumbered with that dietary restriction. And gluten is a good one. It’s a good example of this.
Diet After Healing The Gut
Now, in the research the term that’s often used, or prominently used, for gluten sensitivity is non-Celiac gluten sensitivity. So these are people who do not have Celiac disease, but they notice a problem, or they think they have a problem with gluten. And some of the evidence is showing, perhaps as much of 30% of people who report a sensitivity to gluten may actually be able to eat gluten without any problem once they addressed underlying infections, or things like FODMAP sensitivity. This has been echoed in a handful of papers.
In fact, one paper even went as far as to document people who actually had Celiac. This is a group of Celiac people. But they all went gluten free, 13 of these people. And none of them saw improvements. And the researchers were saying, wow, what is happening here? How are people with Celiac disease going gluten free and not feeling better?
Well, it turns out that three of them had a various type of infection. And then 10 of them had small intestine bacterial overgrowth. And when they were all treated with various antimicrobial therapies, they then responded. They then finally saw their symptoms clear. So it paints a little bit of a different example. But it tells you that if you’re not responding to diet, there maybe an imbalance in the intestines that’s leading to that lack of responsiveness.

But I lead with the outcome. Because the outcome is what we care about. And I’ll fill it in with mechanism. But a word of caution to the audience, don’t be mislead by mechanistic tidbits of factoids that sound interesting. You always want to make sure that whatever someone is trying to pitch you, it’s been verified to have an outcome. Meaning the person is less bloated. They have less abdominal pain. They’re sleeping better. They lost weight.
The mechanism behind this is likely, when we have intestinal inflammation caused by any variety of factors, that can interfere with the barrier function in the intestines. It can also interfere with the ability of the intestines to secrete enzymes to break down foods. And thirdly, you may be more pain sensitive. Your nociception may be turned up when there’s inflammation.
So we know when we heal the intestines, you’re less reactive from an immune perspective, from a gut barrier perspective, from a pain perspective. And also from the perspective of your intestines being able to secrete the enzymes needed to breakdown the foods that you’re trying to digest in the first place. So yes, if you fix your gut, you often times can expand your diet, and eat foods that you were otherwise unable to eat previously.
GS: I love that. That’s my favorite part.
MA: I knew Gin would love that. That was one of the takeaways I really remember about the book. Just the importance of eating to reduce inflammation, rather than eating based on a preset paradigm in your head. Or thinking that you need this certain type of fiber, or this certain type of food for A, B, and C. When really the overall picture of an anti-inflammatory approach seemed to be really key for the individual. And how that varies from individual.
GS: I also, I wrote something else down that relates to that, Melanie, that was like my big ah-ha. And you know how you just talked about inflammatory foods. Dr. Ruscio, I love how you talked in your book about how inflammatory foods are individual.
For example, so often people in the nutrition field make a list, “These are the inflammatory foods.” As if everyone is going to find inflammation from the same foods. And I really loved, in your book, how you emphasized that everyone has to find their own inflammatory foods.
Low FODMAP
DrMR: Exactly. And I think that the low FODMAP diet is a really powerful example of how a food we all stereotype as “healthy” may not be healthy for some people. Or at least may not be healthy for some people, initially. Now, FODMAPs are foods that are rich in prebiotics that feed bacteria. And this isn’t necessarily a good or a bad thing in isolation. But we do know that when people, especially have preexisting digestive symptoms. Abdominal pain, bloating, and altered bowel function. Whether that be constipation, diarrhea, or an oscillation between the two, that they are often times FODMAP sensitive.
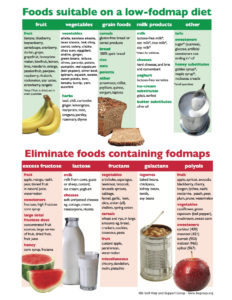
So, it’s important not to pigeon hole yourself into thinking, I’ve got to do paleo, and I’ve got to comply with these foods. Because these are the healthiest foods. Yes, there is data showing that a paleo diet can be health promoting. Clearly. But it’s not 100% of the time. So to your earlier comment about looking at the evidence from both sides, in a broad perspective, we clearly see that various diets can be beneficial for different people with different situations.
So what we want to do is not have a dietary camp that we’re ardently supporting. But we want to provide people with clues to help them navigate to the dietary camp that will work best and the endpoint of healing their gut and then hopefully allowing them not to have to reside in one dietary camp. And have the digestive resilience to eat out of any dietary camp with minimal repercussion.
Listener Question: How Does A LOW FODMAP Diet Help?
MA: Yeah. And speaking to that. We got a question from a listener, Marique. And she wanted to know the workings of and the results of low FODMAP diets. She said, “I never hear about FODMAPs. My doctor only gives the advice for medicine, no advice for intermittent fasting or FODMAP. So I’ve been experimenting by myself.”
And I do have a question, this is coming from me personally. Because one reason I love everything that you research and talk about is because I do personally struggle with a lot of digestive problems. Ever since I had food poisoning quite a few years ago. Gin, on the other hand has a resilient gut. I’m so jealous.
GS: I do.
MA: I’m so jealous. I get more on the struggle bus with everything. But I do have a question for you, Dr. Ruscio. This is me speaking. For me personally, I do the best with low-FODMAP. That’s just what works really well for me. And I’m really happy in that zone. If that’s the case, do you think it’s really necessary to broaden my diet even more, and get to a place where I can eat “all the things.” Or is it ok if you stay within a certain diet paradigm that does work for you, even if it’s not as expansive? It’s kind of the flip side question. Rather than, we want your diet to be really broad. Is it ok to be in a world that you feel safer? Maybe it’s a mental thing.
Is Long-Term low FODMAP OK?
DrMR: Technically, I don’t think we know the answer to that specific question just yet. Because what we would really need to fully and accurately answer that question is long-term data following people on a low FODMAP diet, and tacking their outcomes. And when I say long-term, I would like to see a study between anywhere of 5 to 15 years. The maximum we have right now is about 2 to 2.5 years. That study has not shown any detriment. So that’s what we can say from a published literature perspective.
Now, we can speculate a little bit and draw some inferences based on what we do know. And based upon that, I don’t see any compelling evidence. Although I’m happy to change my opinion as the body of evidence here evolves. But I don’t see any evidence that suggests a restriction of FODMAPs in the longer term would have a deleterious health benefit when the person is clearly symptomatically benefiting.
So there’s a weighing of pros and cons here that should be engaged in to help answer this question. So we know that when people have symptoms, they likely have underlying inflammation. And we know that that inflammation can be bad. And that inflammation often correlates with poor outcomes in the individual. Whether that be time off of work due to debilitation from the symptoms, or potentially even more serve things like development of certain cancers. Although I think that may be a little bit more debatable. But bottom line, we know that inflammation in the gut is bad. And typically when people have symptoms, they have inflammation.
So we have to juxtapose that against the observation of, well, the low FODMAP diet may decrease some bacterial populations, like Bifidobacterium. And we think Bifidobacterium is health promoting. So wouldn’t it be a bad idea to eat low FODMAP in the long-term? Well, if we had to make a decision based upon a dwindling of Bifidobacterium, or a lowering of inflammation, I’d say the greater good is served by eating a diet that reduces inflammation. And also, reduces your symptoms, right? That’s probably one of the most important things for just day to day function.
So, while I don’t think we know the answer to that question from a published research perspective, it makes sense that if the host is feeling better on a certain dietary plan, and is trying to broaden as best they can, and have identified their boundaries, and their boundaries are somewhat FODMAP restricted, I don’t see any reason that would post a problem in the long-term.
With one additional caveat, which is, I would take steps to investigate other imbalances in the gut that may be driving that sensitivity. Like small intestine bacterial overgrowth is just one example. Or just as general dysbiosis. And I’ve been using the term dysbiosis more because I want to get people away from the thinking of, it’s this one thing in my gut. It is SIBO. It is candida. It is H. pylori. When people come in doing that, they often times get in their own way. Because for everything that we can test, there’s probably another thing we can’t test.
So, what I don’t want to do is just use the proxy of SIBO to represent some of the evidence showing that imbalances in the gut can lead to food reactivity. And then everyone rushes out and wants to do a SIBO test, and the SIBO protocol, and they miss the boat. They missed the broader perspective of trying to heal their gut holistically. So I know that’s kind of a long answer to your question. But in short summary, I see no reason that would be a problem to follow low FODMAP in the longer term. As long as you try to eat the broadest diet that you can, in conjunction with making sure you’ve investigated any other thwarting factors that may be driving the need to be FODMAP restricted.
MA: I’m so glad you said that. I actually got the symptom of SIBO when I got that food poisoning about four or five years ago. And I think I got too wrapped up in the label of SIBO. And I was convinced that everything was due to SIBO, and everything I was experiencing was that. And that I needed to always be in this kill, kill, kill phase for SIBO. It can get overwhelming. So I definitely think that a broader picture is definitely more important.
And we actually have a listener question about SIBO, and it also ties into intermittent fasting.
Dieticians should start patients off with a general healthy diet. Meaning, avoiding processed foods and trans fats. Just kind of your standard dietary advice, which, some of us may not fully agree with. But if that does not produce results for the person, they are then recommending, as across the board recommendations for all their dieticians, to then consider a low FODMAP diet.
So it’s permeating enough into the health medical community, because the evidence is there. So yeah, I would say there is definitely some very promising literature there. And a well-informed gastroenterologist should at least entertain the idea of a low FODMAP diet. Because there’s enough evidence to really support that.
Sponsored Resources
DrMR: Hey, everyone. Let’s talk about one of my favorite tests for digestive health, the GI map from Diagnostic Solutions, who has helped to make this podcast possible. Now, if you’ve been reading any of the case studies I’ve published in the Future of Functional Medicine Review clinical newsletter, you’ve likely seen that this test, the GI map, is a test I frequently use in my practice. Why?
Well, one of my favorite things about this test is it has excellent insurance coverage. This is a few hundred dollars I save patients. This lab is also CLIA certified, which is essentially the quality assurance bureau for labs. So it’s important that these labs are being monitored, not cutting any corners. That’s where you get your CLIA certification.
Now, this test uses quantitative PCR technology, so it’s a DNA test. And you’ll get a good read on dysbiosis with this test, because they will assess and report out various types of bacteria, yeast, and parasites. Including protozoa, worms, and amoeba. They also have some valuable and helpful clinical markers, like calprotectin, which can help rule in or out inflammatory bowel disease, and zonulin, a marker of leaky gut.
So head over to DiagnosticSolutionsLab.com to learn more, and to order your tests.
MA: So for listeners, if you go to IFPodcast.com/episode68, we’ll put links there to Dr. Ruscio’s book, which has all of these studies. We’ll also put some of the studies, as well. And I will also put a link to, I created a free low-FODMAP guide. So if you want to learn more about that, definitely check that out.
Listener Q: Can IF Help Heal the Gut, Reduce Microbial Load?
So I’ll read this question from Jennifer. Because it kind of, she has a lot of questions, but it ties in, kind of all that we’re talking about. And then also gravitates towards intermittent fasting, which we can get into, as well. So Jennifer says, “Hi, ladies! I’ll jump right in. I’m recently diagnosed with SIBO after years of GI issues. Six months of being bloated, pain, tons of food sensitivities, constipation, etc. I’m using intermittent fasting. I’m trying 16/8 and 18/6, and a few 24-hour fasts a week while I’m on an herbal treatment protocol. I’m also eating a severely restricted diet of basically meat, fat, and well-cooked carrots, which is so hard for a former vegan. So this is the specific carbohydrate diet, plus the low-FODMAP diet. And it is the only thing that brings any relief in bloating, along with intermittent fasting.”

So her first question, she wants to know about intermittent fasting and SIBO. And I will clarify, just for listeners. Small intestine bacterial overgrowth, it’s what it sounds like. It’s basically where there is an overgrowth of bacteria in the small intestine, which compared to the large intestine, should be relatively sterile. And it does create a lot of GI distress for a lot of people.
So Jennifer sounds like she’s on a very restrictive diet, because it does help her bloating. She’s doing intermittent fasting because it helps her bloating. Dr. Ruscio, do you have any experience with intermittent fasting and SIBO? And how all of that goes together?
DrMR: Yeah. I absolutely do. So, we don’t have any research on intermittent fasting and SIBO, per se, as I understand it. But we do have research with both inflammatory bowel disease, and irritable bowel syndrome. And they have both shown positive outcome with intermittent fasting.
We know that intermittent fasting can help facilitate digestive motility, which is essentially a SIBO preventative measure, as well as the ability of intermittent fasting to reduce stress on the gut, said loosely. And with my patients, it’s something I see benefits clearly for some patients. Not for all. And it’s also codified into step one of the healing plan in Healthy Gut, Healthy You because meal frequency is important.
So, yes. I would continue to intermittent fast if it’s benefiting you. The length is something you can experiment with. And certainly, I am empathetic for the position you’re in. This GAPS plus low-FODMAP combination. It’s a restrictive point, and it would definitely be the goal to get you away from that restrictive point.
Now, I believe she was on a course of herbal antimicrobials, which is a good place to start. You may want to use some probiotics before you do that. Again, this is absolutely codified into the plan in Healthy Gut, Healthy You. So all of this is laid out for you in detail. And in some cases, these details do matter.
One of the quotes I use in the book is, the difference between knowledge and wisdom is experience. One can fairly easily find a protocol on the internet for SIBO. That’s knowledge. But knowing how to use that protocol in the right place, at the right time, in the right sequence, that is wisdom. And that’s harder to come by. That’s what I try to lay out in the book.
So, the reason why probiotics may be a good idea first, is because probiotics have been shown according to one meta-analysis, very high-level scientific evidence to decontaminate the small intestine of small intestine bacterial overgrowth. In addition to being broadly antimicrobial. Meaning if you also have some candida that wasn’t found, or some H pylori that wasn’t found. Or some blastocystis hominis that wasn’t found on testing. The probiotics can start shifting the tide in that positive direction, as well as reducing leaky gut.
Now, regarding probiotics. There are three different categories. You can read more about that in the book. But it’s important to try one probiotic from each category. Because sometimes people try one type of probiotic, and they keep trying the same category of probiotic, but they keep trying different formulations of the same category. And they go, well, I’ve tried five different probiotics. Yes, but you’ve tried the same category time and time again. You haven’t used a different category of probiotics. So that can be a key thing to piece together.
Not everyone will have a positive reaction to probiotics, but I do think it is the majority. In the SIBO community, unfortunately, some of the experts in the SIBO community have an anti-probiotic opinion, which I think is totally against what the preponderance of the evidence shows. And I think actually is doing more harm than it is good. And unfortunately, this is an example of where the expert opinion is at odds with what the literature actually shows. And I can tell you that clearly there are patients.
We’ve written up, I think, at least three case studies of patients who have done testing and come back positive with either SIBO or candida or something like that. And we did not need to treat their lab results, because we had put them on a good probiotic protocol ahead of time. And by the time we saw them at their follow-up visit to interpret their lab results, their symptoms were gone from the probiotic protocol.
GS: Oh, that’s great.
DrMR: So, probiotics, I would certainly codify them earlier in the sequence than antimicrobials. But, if you have a negative reaction to probiotics, which a small subset do. Or you don’t see complete resolution, which some people don’t. Then you may want to consider escalation to antimicrobial therapies.
Now, within antimicrobial therapies, there’s herbals and there’s pharmaceuticals. And there are some nuances with the herbals. And you can also escalate the effectiveness of the herbals, at least according to some preliminary data that was conducted at our office, and is currently being drawn up for publication, with the addition of antibiofilm agents, which may help clear stubborn cases. And only then would I recommend considering escalating to an elemental diet.
Now, yes, the elemental diets do contain some sugars. I would throw everything out the window in terms of what you think you know about what is good and bad. I would quite simply just try the therapy. Because what you don’t want to do is learn enough to talk yourself out of a therapy. And I see that somewhat frequently.
MA: Yes, yes.
DrMR: Right? So, people think, oh, there’s maltodextrin in here. And I have to have a four-minute conversation with them convincing them that it’s ok. They come back after a week on the elemental diet, and they feel incredibly better. Now, does that happen all the time? No. But the point I’m making is, don’t take a little bit of knowledge, and use that to convince yourself not to do something. As long as you’re working with someone whose approach you have confidence in.
And then some people need a combination of the elemental diet in small doses on the longer term, along with a little touch of a light dusting of antimicrobials. That’s also kind of codified into the approach in the book. And I don’t mean to keep referring back to that protocol. But I can tell is some of what I just outlined is a difference between people who have seen five doctors, and then they come in to see us and succeed and fail. It’s some of those small modifications to the protocol that allow people to succeed.
I know that’s kind of a lot. And there’s a lot in the book for you to work through. But those are all some things to consider in that situation.
GS: You mentioned someone may have seen a bunch of doctors, and not had success. How can someone have their best chance of finding a doctor like you, who could guide them through this process that’s knowledgeable? Do you have any advice for people who are looking? Because I know that’s something we hear a lot. That they’re frustrated by what they hear from different doctors.
How To Find A Good Functional Medical Doc
DrMR: So you’re saying that people don’t like what they’re hearing when they’re trying to vet a doctor?
GS: I think people have a hard time finding a doctor that’s going to be able to walk them through a protocol, such as yours, and help them to heal. That sort of thing.
DrMR: We did a podcast that’s fully transcribed, entitled something along the lines of “How to Find a Good Functional Medicine Provider.” And it was about 30 minutes in duration. So there are a lot of things that I lay out. So people may want to go to our home page, and go to our search box, and type in how to find a good functional medicine provider.
It can be challenging, but there are some things you want to look for. There are some easy giveaways that this person may not be a good fit. And those are things that indicate rigidity and dogma. So, if in your investigation with what you read from them, or listen to, or watch. If they seem to make a lot of absolute claims, a lot of strong claims, then I would be very cautious. Because, and I also quote in the book, I’m a strong believer that dogmatism can only exist in the presence of ignorance. So someone can really only be hardheaded and fervently believing in a position if they’re ignorant to the contradictory information that does not support their position.
So essentially what I’m saying is the more someone knows about something, the less strongly they make certain claims. So look for that strong language. That absolutist thinking. “Everyone has to be gluten free forever. Everyone has a parasite.” These kind of strong, absolute claims. Look for someone who is a little bit more measured and cautious. And you can tell they’re being very careful with what they say.
And sometimes, it’s funny. The people that make the loudest, strongest claims may be the most appealing from a marketing perspective. Especially if they’re telling you what you want to hear confidently, but you have to be careful not to fall into that trap.
Also, look at someone’s billing structure. This is not an absolute rule, and I do think there are some exceptions, especially if it’s a nutritionist who’s offering like a package of coaching. But more so with doctors. If they’re doing these bundles of all your visits and lab tests in this one $5,000-6,000 bundle. Usually what happens there is you have a model, and they try to cram the person into the model rather than making the model adaptable to the patient’s needs.

Now, neither one of these is right or wrong. But there’s pros and cons to each. Usually, it’s less expensive to work with a health coach or a nutritionist. And they’re more available. And then with the specialists, often times you have to wait a few months, at least to be seen, and it’s more expensive. So, again, neither one of those is right or wrong. It’s just knowing where you are and making sure that you start off with someone who is corresponding with your needs because of course, if all you need to do is go on a low-FODMAP diet, you don’t need to see a guy like me to figure that out. Right? That would be wasteful. So those are a few things to help you finding someone.
GS: That was great. And we’ll put a link to this on our show notes for this episode to that episode for our listeners. So they can find it.
MA: Yeah, so that will all be there. I know once you write a book, I guess because we all have books here. One of the reasons, at least I know for me, and it sounds like for you, and I know for Gin. One of the reasons we write a book is so that we do have all the information in one place as a resource. So it will all be there, and people can check that out.
And the way your book works that I really like, it’s kind of like a choose your own adventure. You have the different steps that people can, it’s like, where are you at? And then that’s where you start, based on where the person is feeling. And they see how they react to different levels in the book. It’s hard to explain, but I really like. It’s like having a guide there with you, without actually having a guide.
DrMR: Sure. We adapt the protocol. So at the end of every step, we then check in. And depending on someone’s response, we go in one of a number of directions. So to put this quite simply, if step one, the dietary step, people are feeling 80% improved, then they go into more of a maintenance mode. Or finishing touches/maintenance.
If someone changes their diet, and even escalates to the most restrictive diet, like a low-FODMAP/SCD combination diet, and they’re still not feeling well, then we escalate therapies from there. And we check in symptomatically at the end of each step. And someone’s response dictates where we go. So just like you’re saying, it’s kind of like a choose your own adventure guide, except your symptoms help you choose the adventure that’s right for you.
And I should also mention that the same information about how to find a good doctor is also listed in my book, along with some things to consider discussing with your doctor.
MA: Perfect. So we’ll definitely put links to all of that.
View Dr. Ruscio’s Additional Resources
MA: Jennifer did have one more question. I guess we’ve touched on it briefly. She did say, “Does eating a limited diet actually harm gut bacteria in the long run? I’ve read that a more diverse microbiome is better for long-term health. I’m afraid that eating so restrictively will change my microbiome and prevent me from ever being able to eat normally again.” And then she just reiterates that she would just love to know how intermittent fasting could help with all of that.
The Healthy Gut, Healthy You Protocol
DrMR: So, kind of coming back to my earlier answer on this, I would look at the health of the host as the primary barometer of if you should or should not do what you’re doing. This is a good example of where a little knowledge is enough to get you to doubt what you’re doing.
Regarding diversity, we are still very early in our understanding of diversity. One of the things I outline quite meticulously in the book is that the health of the host is a main driver of diversity. So this is evidenced by the fact that people who are sedentary and then start exercising have healthier microbiotas. People who don’t sleep well, and/or have a time zone change, or a circadian disruption have less healthy microbiomes. So, we know that exercise, sleep, stress also has a negative effect on the microbiome.
Now, how can we support that statement even further yet still. Well, we know that intervention to “feed” gut bacteria in patients with preexisting gut problems make those patients worse. So this whole philosophy of needing to feed your gut bacteria is severely flawed, and I think it really hurts people. Because it prevents them from listening to their body. And in some cases, prevents them from undergoing diets that they should undergo, like a low-FODMAP diet, and coaxes them or inculcates them into thinking they should do things that are bad for them, like take whopping doses of prebiotics or resistance starch, which then flare them and cause bad side effects.
And again, I think I do a very good job of detailing this in the book, but also not going so deep that we lose people. The assumption that diversity is a cause of health is very, very flawed. And we are extremely early in our understanding here. And to make it simple, I would throw that out the window. And I would focus on finding the interventions that help you feel well. Because at the end of the day, you probably wouldn’t even be listening to this podcast if you had no symptoms. Right? So that is what we want to get you to. We want to get you to a point where you’re feeling well, and then you can be done with your concerns.
So follow the path of outcome. Follow the path of what works well for you. And that is usually what will create the plan for you that will have the best overall net effect on your health.
Do Restrictive Diets Hurt Your Microbiome?
MA: Yeah, I love that. There was also this study that showed that those who went on different fasting protocols. I don’t know exactly what fasting protocol they did, but I’m pretty sure you mentioned it in your book, as well. They actually experienced increased microbial diversity from the fasting, which is kind of the opposite of what you would expect.

So, again, it’s a bit in a kind way, ignorant. But using the term ignorant literally, not knowing, to think that we need to feed the microbiota to be healthy. It just takes a complex ecosystem, and reduces it down to, well, we just need to put prebiotics in there and everything will be ok. And if you went to a forest, and the forest was dying, it’s like, well, let’s just throw a bunch of fertilizer around. You would need to look at the forest ecosystem to figure out, is there some type of infection? Is there deforestation from mining or lumbar companies that’s causing overexposure of sun, and that sun is causing a deforestation type of effect? Is there a drought?
You have to look at the environment holistically. So just thinking you can throw fertilizer into an infinitely complex ecosystem and have a beneficial effect is really actually a very reductionistic medical-like way of thinking. We’re doing it in the guise of this holistic paradigm, but it’s actually a very reductionistic way of thinking about things.
The Three Probiotic Categories
MA: So I will say one thing for listeners because I knew if I was listening to this podcast, when you had said earlier about the three categories of probiotics, I would have been like, “What are the three categories?” It would be in my head. So I will tell the listeners, just in case anybody was wondering. And correct me if I’m wrong. But the stereotypical probiotic that a lot of doctors prescribe or a lot of people are familiar with, so the bifidobacteria-lactobacillus type blend. So that’s very popular on the market. Then there’s the soil-based probiotics, which are a different world altogether.
Speaking of, I actually just recently ordered. I listened to the interview, Dr. Ruscio, that you had with the Just Thrive probiotic. Was that the name? Just Thrive? Or Thrive?
DrMR: Yep. That’s the one.
MA: So I ordered that, and I’ve been liking it. And then the third one was the Saccharomyces boulardii, which is basically a yeast, but can help with healthy yeast levels. I will say you were probably the person who changed my own mind, and my mental chatter that I had in my head about probiotics and bacteria. Because like I said, I got diagnosed with SIBO, and I was so scared of bacteria, in general. I was like, kill all the bacteria, all the time. No probiotics, no nothing.

GS: Oh yeah, me too. I thought that was fascinating. I had never read that before. I was like, wow.
MA: Me neither. Mind blown. So, yeah. There’s just a lot there.
GS: Basically, we’re just learning so much. There’s so much out there that you could just lost in all of the information. It’s still developing.
Avoiding Information Overload, Knowing What is Accurate vs. Noise
DrMR: Yeah, it’s true. You absolutely can. And that’s one of the reasons why, I believe it’s in chapter 3 of the book. I lay out that section entitled how to evaluate health claims. And I keep this concise, but I think it’s helpful nonetheless, which is, when we have a lot of information, it’s helpful to know what information is the most accurate, and the most meaningful. And what kind of information is less meaningful, and might just be noise.
And just as a quick example, if we took a group of rats, and did something to those rats, we shouldn’t then say, “This happened in rats, so let’s go do it in humans.” That would be irresponsible. Yet, you will see all the time on the internet people marketing their products or services or philosophies based upon animal model evidence, which I find it abhorrent. Because it’s so misleading, and intellectually dishonest.
Now, what we want to do, is look at, “we took a group of 30 patients with IBS or with SIBO or with general digestive symptoms, and then half of them got placebo and the other half of them got treatment X. And here’s what happened.” If it was a successful outcome, then we could say, “Treatment X is something to consider.” Now, you still need to know when to do that in the greater sequence. But at least we now have something valuable to take away.
Significance of The Placebo Effect
Now, the reason why the placebo is so important is because 45% is the average affect of placebo in digestive symptom studies. And these are in studies where the researchers are trying to design out of the study any impact from placebo. So it’s very, very important that we have placebo controlled, because if you tell someone, “I’m going to give you this, and it’s going to make you better.” They will probably tell you a few weeks later, “Yeah, I feel better.” So it’s very important with the placebo.
And I make this parallel regarding gluten digesting enzymes. Where the evidence showing benefit from gluten-digesting enzymes is quite weak. However, you can go on Amazon and read reviews about gluten-digesting enzymes, and people are raving about it. And so, you have to be careful. Because we are creatures of habit, and we are very easily influenced by what we see other people doing. So if we hear everyone raving over a product, and we go and try that product, we have an extremely high probability that we will be “placeboed” into thinking that product is helping us.
Now, I’m not necessarily against the placebo. I think we can use the placebo effect in a responsible way. But if we’re using the placebo effect to make someone more afraid of a food that they don’t need to be afraid of, and spending $100 a month on a supplement that’s doing nothing, then I think that is irresponsible use of the placebo effect. So for all those reasons, it’s really important to know what type of evidence to look at. Because you’re right. There’s so much evidence out there. And if you don’t have some kind of system for filtering out the low level evidence, and focusing on the high level evidence, you’ll get lost. Absolutely.
MA: So maybe if you’re trying a dietary approach, or something, you should only Google. I mean, this would be a bias. But only Google the benefits of it. If you want to benefit from it. Don’t Google the negative effects. I know that’s not a good approach.
DrMR: No, that would be using the placebo effect in a healthy way, I suppose.
MA: It’s like the study where the people who, even the people who knew they were receiving placebo would see beneficial effects from placebo.
GS: Right.
DrMR: Yes. There have been a number of studies that have found that same thing. So yeah, this is why controlling for the placebo in a placebo-controlled trial is important because if you give people encapsulated anything and tell them your bloating is going to get better, even if there’s nothing in that pill, people will tend to report a reduction in their bloating. So we have to factor it against placebo. And that’s why I hold the standard of evidence that we review in the book to a high standard. Just so we don’t make that mistake.
How Does Intermittent Fasting Affect Gut Health?
MA: That’s great. So just in general, to just touch on the topic of our podcast, what are your immediate go-to thoughts about intermittent fasting, and how it affects gut health? What’s your first thought when you say, “Can intermittent fasting benefit gut health?” Because we do get a lot of just general questions like that.
DrMR: Yes, it can. And this is why it’s organized into step one in the healing protocol of the book. Meal frequency, which includes potentially intermittent fasting. And like I mentioned earlier, we have some published evidence that supports the beneficial effect of fasting on the gut. And not only gut, but also there maybe some metabolic benefit and some neurological benefit. Certainly, fasting is something to consider as a foundational factor in optimizing one’s gut health.
Now, it’s not going to work for everyone. And there is a subset of people that should be cautious. And these are people who exhibit burnout like symptoms. They’re overworked, they’re over stressed. They’re not sleeping well. They’re exercising a lot, especially people who are underweight. They may want to be more careful. It’s not to say they may not benefit. But one of the things we should factor in is how much stress is that biological system under?

You can still run an experiment to see if it helps you, but just go into it being cognizant that, “I may not do well on this. And if I give it a deserving trial and I’m reacting negatively, I won’t keep beating my head against the wall with intermittent fasting. Because I heard it’s good for you. And I’ll move onto something else.”
GS: Yeah, I think that’s a great point. I want to read one more quote from your book, which is actually maybe my favorite quote, actually. Even though I said the other one was. You said, “The most powerful thing you can do to improve your health is to learn to listen to your own body, and stop listening to everyone else.” And I think that’s profound. If everyone could just proceed from that space, I think we’d all be in a better spot. Instead of trying to look for the miracle one cure-all that’s out there.
And I know a lot of us have done that over the years. But instead, learn to trust the wisdom of your own body, and how something makes you feel. Do you better when you’re doing it, or do you feel worse? And that can guide you.
DrMR: Exactly. And that’s actually, I think a fairly defensible statement to make scientifically. And the reason I say that is because we know that for any given condition, there’s a number of different interventions that may work. But none of those interventions will work 100% of the time. So by listening to your body, picture in front of you this menu of options. I’m bloated. Just as an example. This could apply to anything. It could apply to joint pain, diarrhea, constipation, SIBO, whatever.
There’s a menu of options in front of you. And all the different things on the menu are research studies showing a positive effect on the condition that you’re struggling with. But, no one of those menu items is guaranteed to work for you. So how can you figure out what menu item to select? You can listen to your own body’s experience as you try a couple of different bites from each of these dishes on the menu. And then settle on the item that works best for you.
So by listening to your body, you can navigate the menu of validated treatment options, and find the one that works best for you. The travesty is, when people don’t allow themselves an opportunity to try these different therapeutic options on the menu, because they think they’re not good, or they’ve read something like probiotics and SIBO as an example.
I can’t tell you the number of patients who don’t need to do anything other than take probiotics for their SIBO. But, many of them come in, indoctrinated into thinking that they can never take a probiotic because they have SIBO. And they haven’t tried that item on the menu because of that. So it’s important, as you’re saying, absolutely to listen to your body. It will oftentimes get you to the treatment that works for you faster.
GS: Perfect.
How Long Should You Try a Dietary Approach Before Evaluating?
MA: Absolutely love that. And I will ask when we are trying different approaches, and seeing how we react, how long do we need to give any specific approach before we evaluate it? Because I know we can react or feel different effects from different things maybe immediately, or a few days later. So how long do you suggest that listeners, if they’re trying different dietary approaches. Or trying probiotics. Or trying different things. How long do they commit to each different thing before they move on?
DrMR: It’s very important. Because what you don’t want to do is stay in a therapy way longer than you need to, and not move off of it. Because if you waste time on a therapy, then that’s time taken away from you getting to where you ultimately want to be. So, this is a crucially important question.
The fastest people tend to respond, these are just rough approximations. But the fasted the people tend to respond is within a couple of days. So, two, three, four days. Wow, I’m already feeling better. Are you totally healed and at 100%? No. But you’re at least able to say, yeah, I’m clearly feeling different. I’m clearly feeling better.

Now, be careful that, I say that I’m very careful in the language that I use there. People feel a little bit worse. A little bit worse may denote an irritation reaction. Feeling a lot worse may indicate an intolerance reaction. So, we don’t want to just say, I’m feeling terrible! So I’m just going to push through. If you’re feeling really bad, then you may have crossed the threshold of being a little bit irritated by an item to this item is not a good idea, and we need to try a different option. So just bear that in mind.
How To Address Your Relationship To Food In A Healthy Way
MA: Alright. Thank you so much for that. So I do have one more question, this is more a mental thing. It’s more of an overview, and a general question. But how do you feel about people and their relationship to food. We get a lot of questions from listeners who just struggle with food. It’s the reason we have this whole podcast, that we have intermittent fasting. Oftentimes, it’s just people struggle so much with food today. Especially with how it’s processed. It can be addictive. So whether it’s fear of food, or thoughts of bingeing with food, or restriction with food. Do you have any advice for people just dealing with their relationship with food in a healthy way?
DrMR: I do. I think a foundational point here is having a well-crafted education on food. Because, sometimes someone’s tenuous relationship with food is due to a hysterical or an absolutist or a fear mongering or alarmist, whatever you want to call it, perspective on the food that they’ve obtained from whoever they’re learning about the food from.
So, a great example of this is gluten. There are some people on the internet who are taking way too extreme of a position on gluten. Now, one of the first thing I recommend across the board people do is a gluten-elimination. So I’m on the side of eliminating gluten. But what I’m not on the side of is indoctrinating people into thinking that 100% of the population has to avoid gluten 100% of the time. This is not true. This is not what the evidence shows.
And the pernicious effect of this is that when we coax people into thinking that they need to avoid gluten all the time, the people who are disservice by this are the people who don’t need to avoid gluten. And they may have other food sensitivities that are legitimately important for them to avoid. So now we’ve made their life more difficult. Because they have to not only avoid the food group that they react negatively to. But they also have to avoid gluten. And they’re only avoiding gluten on blind faith.
We’ve published, I believe, two case studies, not formally, on our website, of people who started bringing some grains and even some gluten into their diet, and they felt a lot better. It’s very interesting to see how some people have a hard time, and want to fight me on that after someone has clearly gone through a gluten elimination and reintroduction and noticed no problem with it, and maybe actually even feel a little bit better. And certainly has this heavy weight of fear regarding eating out, and social functions, lifted off of them once they’re no longer encumbered by the “Avoid gluten all the time” recommendation.

Now, if someone has qualified that they really have a problem with gluten, and every time they eat it they react. You have my full support in avoiding gluten. Unfortunately, there’s a fairly strong level of indoctrination. The best evidence that we have shows that 6, perhaps, and this is a bit inferential, 16% of the population may have non-celiac gluten sensitivity. So that is something, and it’s verifiable, and it’s identifiable, and it’s legitimate. But is that 100% of the people? No.
The same thing occurs with FODMAPs. If you’ve done some reading, you’ve kind of gotten into the SIBO community, people will think they should never have any FODMAPs, ever. That’s not how this is designed to be. These diets are meant to be eliminations, followed by reintroduction. And this is where you figure out what you can and what you can’t eat. They are not meant to be elimination and inculcation, meaning you never reintroduce the foods because you heard that this food might be bad some of the time. So you avoid it forever on blind faith, without figuring out if you can or cannot have it later on down the line once you’ve improved your gut health.
So, we kind of take the elimination part of elimination-reintroduction diet, and just focus on the elimination and we forget about the reintroduction, which can be a huge disservice. And there are people walking around where this is the thing they need to change. And I tell this story all the time, because this one was just so marked of this very intelligent psychologist who came into my office. And she had seen a few other doctors, not gotten any results.
And she came in with the attitude of, this is the expert. We’re going to roll up our sleeves. We’re going to dig in. We’re going to figure this out. It’s going to be cerebral, and meticulous, and intense. And we’re going to test. And that’s not what she got from me. Because when I looked at everything, it was fairly evident that there was really nothing “wrong” with her in terms of digestion. But she was getting so indoctrinated into this narrow paradigm of not being able to eat or do anything, that she was literally having a psychosomatic manifestation of symptoms, because her life had become so devoid of any joy and so encumbered by restriction.
So I told her that, in a diplomatic way. And that I think she needed to loosen her grip on her health. And eat off plan, and maybe have a couple of drinks, and have some fun with her partner. She did not want to hear that. It was a very tense visit. I remember, you could cut the tension in the room with a knife.
GS: I love that.
MA: I think that’s a wonderful way to end things. A lot of information, we tackled a lot of subjects. But in the end, definitely moving towards intuition and not having a fear of food seems to be the best approach.
GS: And, Dr. Ruscio, I just have to tell you. You probably don’t know this. I’ve written a couple of books, but my second book is called Feast without Fear. So you’ll probably like that title.
DrMR: Great title. Yeah, great title.
Episode Wrap Up
MA: Well, this has been absolutely wonderful. So for listeners, if you go to IFPodcast.com/episode68, that’s where we’ll put all the links to everything – so Dr. Ruscio’s book, all the studies that we talked about, FODMAP guides, all the things. So definitely check that out.
Dr. Ruscio, besides the book, what are the best ways for the listeners to follow your content and learn more about you?
DrMR: We have a weekly podcast, article, and video. And all that can be plugged into at DrRuscio.com. And if there are any health care providers listening, we also have a monthly subscription newsletter that’s essentially a clinical training newsletter that’s written with case studies and research studies, summaries for any clinicians who want to get into this on the clinical end.
MA: Perfect. So listeners, definitely check that out. That will also be in the show notes as well. You can also go to IFPodcast.com/stuffwelike. That’s where we put a link to all of the stuff that we like. Dr. Ruscio, your book is on that page already. But there’s lots of stuff there, lots of things to check out.
And then a few other things for listeners before we go. If you’d like to submit your own questions for the podcast, there are a few ways you can do that. You can directly email questions at IFPodcast.com. You can also go to our website and submit questions there. You can also get on our email list there, as well, if you would like updates each week about the podcast. You can also subscribe in iTunes to get the podcast downloaded automatically each and every week. You won’t even have to do anything. You can follow us on Instagram. We are IFPodcast. You can also follow us on Twitter, we are theIFPod. So lots of things.
Again, thank you Dr. Ruscio so much. This has been an absolute pleasure. I wish I could talk to you for about 10 more hours. I could ask you so many things. You should see my list. It’s like, candida, carnivore diet, keto, mindset. So many things. But we’ll just have to table that for now.
DrMR: Well, thank you. It’s been a lot of fun on this end. It’s always nice to discuss these issues with fellow gut enthusiasts. So it’s been a pleasure talking with you guys also.
GS: Thank you. We are glad to be called gut enthusiasts. I like that.
MA: Yes. Wonderful. Well, thank you, everybody.
GS: Thank you.
MA: Bye.
GS: Bye-bye.
- Melanie Avalon’s Website
- Gin Stephens’ Website
- The Intermittent Fasting Podcast
- Asian Federation of Dietetic Association
- How to Find a Good Functional Medicine Doctor
- Feast without Fear
- IFPodcast Stuff We Like
- IFPodcast on iTunes
- IFPodcast on Instagram
- IFPodcast on Twitter
- Dr. Ruscio’s Additional Resources
What do you think? I would like to hear your thoughts or experience with this.
- Get help using this information to become healthier.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Dr. Ruscio is your leading functional and integrative doctor specializing in gut related disorders such as SIBO, leaky gut, Celiac, IBS and in thyroid disorders such as hypothyroid and hyperthyroid. For more information on how to become a patient, please contact our office. Serving the San Francisco bay area and distance patients via phone and Skype.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!