Everything You Need to Know About Probiotics, Part 2
A new and comprehensive guide to probiotics.
I’ve recently published a comprehensive, 43-page guide to getting the most out of your probiotic supplements on my website. I’ve also developed this podcast series to highlight some of the key takeaways that you need to know about probiotic therapy. This episode is part 2 in a 3-part podcast series.
Imbalances of the gut microbiota are becoming increasingly common and can cause distressing digestive symptoms and an array of seemingly unrelated symptoms and conditions. These include mood, energy, skin, joint health, metabolism, sleep, immune function, hormone balance, and thyroid health. Thankfully, probiotics can help to correct these imbalances and relieve symptoms. Hundreds of research studies provide evidence for these benefits.
When used correctly, probiotics are a powerful therapy with a surprisingly long list of health benefits. But for many health care consumers, the results of probiotic therapy can be suboptimal due to lack of information or poor probiotic quality.
[Continue reading below]
Episode Intro … 00:00:40
Your Doctor May Be Wrong … 00:03:31
Evidence for Effectiveness … 00:08:25
Probiotics & Intestinal Imbalances … 00:12:43
Probiotics vs. Antibiotics … 00:15:33
Leaky Gut, IBD, Depression and Anxiety … 00:21:012
Brain Fog, Mental Clarity & Sleep … 00:26:24
Metabolism & Weight Control … 00:30:51
Food & Seasonal Allergies … 00:32:21
Probiotics, PCOS & Female Hormones …00:33:48
Blood Pressure & Cholesterol … 00:35:51
The Gut Skin Connection … 00:41:11
Infant & Mother Health … 00:42:18
Episode Wrap Up …00:43:31
Download this Episode (right click link and ‘Save As’)
Episode Intro
Dr. Michael Ruscio: Hi everyone. In today’s episode, I perform the second of a three-part reading from my recent probiotic article. It is an approximately 43-page article that we’re publishing on our website, which is a comprehensive deep dive into everything that you need to know about probiotics. It is a lot to digest all at once, which is why I broke it down into three different sections. The goal here will be to provide you with everything that you need to know about probiotics, what they are, how they help, how to use them, some very important strategic guideposts to prevent you from falling prey to marketing BS that you will invariably be confronted with on the internet and empower you as much as possible to be able to understand probiotics and use them effectively. I also want to save you from the marketing merry-go-round of trying the newest in vogue probiotic one month, and then another one when you stumble across a different new formulation, and so on and so forth.
I want to use this to direct you to the three probiotics I use in my clinic and that I recommend in Healthy Gut, Healthy You. These are the only three I can say I’ve fully vetted to fit all of the quality assurance criteria that are important.
Now it’s not to say these are the only three on the market. That would be a ridiculous claim for me to make. But I can tell you I took the time to make sure that the companies we are using to procure these materials are companies that adhere to specific quality assurance practices. You will be surprised. We actually had to go through a long list and most on the list did not meet these criteria.
So this is not something that all companies are doing. In fact, when we get to the third section of this article, I go through the quality assurance practices and there are some independent studies, one by Labdoor, essentially finding that perhaps up to half of the probiotics on the market do not meet their label claims. So quality does matter, it is not the only metric, and some companies hide behind quality to gouge you with pricing. We also want to be careful about that. But in any case, today is our second read of the comprehensive probiotic article. I highly recommend checking out the article on the website for all of the charts and images, but otherwise, we’ll continue going through kind of the narration so that if you don’t have much time to read, you can just grab the info via audio.
*All study reference links can be found in the Probiotic Article on our website.
Your Doctor May Be Wrong
Hi everyone, welcome back to another episode of Dr. Ruscio Radio. This is Dr. Ruscio. We will be picking up today with the narration of the comprehensive probiotic article. If you were listening to our last episode, we left off right before a section titled, Your Doctor Could Be Wrong: Why A Science-Based Summary Matters. Again, the reason I give this somewhat strong language is because, unfortunately, there are those who would be considered experts in the field of gastroenterology, either integrative and naturopathic or conventional, who are making statements about probiotics that are not in conformity with what the data shows.
Unfortunately, the person who suffers because of that is the healthcare consumer. It is a travesty the number of SIBO patients who are afraid to use probiotics. We’ll go into the evidence here in a moment about how effective probiotics can be for SIBO. But first, let’s really drill into helping you understand why I say it’s untenable for a gastroenterologist to handwave and say, “Well, we need better data regarding probiotics.”
I put this section in the article before we go into the evidence for the effectiveness of probiotics in a given condition such as IBS, IBD, thyroid conditions or depression to drive home how much or little we can assign value to probiotics for those given areas. The reason why evidence-based opinion matters is because it protects you from bad advice.
Your doctor may remark there is no evidence for probiotics. Again, being totally candid here, and I apologize if I’m being too candid throughout this article, but it is irritating to me when someone hides behind what sounds like a highly scientific retort. When in actuality their opinion is not based on science at all and is ill-informed. You get this when people say, “Well, there’s no good evidence for probiotics.” That is not true at all. Or, “We need better research.” That’s true in some conditions, but there are some other conditions where we have plenty of research. So they sit there and say, “Well, we just need better research. I’m a really concerned scientist and we don’t want to be irresponsible. We need better research.” That irritates me because that harms the people who have conditions for which we have adequate evidence justifying a therapeutic trial on probiotics.
Of course, we also want to be wary of the marketers who will proclaim that a given probiotic is the best or a cure-all. We need to be wary of these claims. We want to look at what the evidence says because, again, there are those who would mislead you one way or the other. The evidence is really the anchor that makes sure that we have accurate information.
As a reminder, the evidence-based pyramid that medicine is built upon assigns the least value to cell, Petri, and animal studies, more weight to observational studies, and then the most weight, the peak of the pyramid, to placebo-controlled clinical trials.
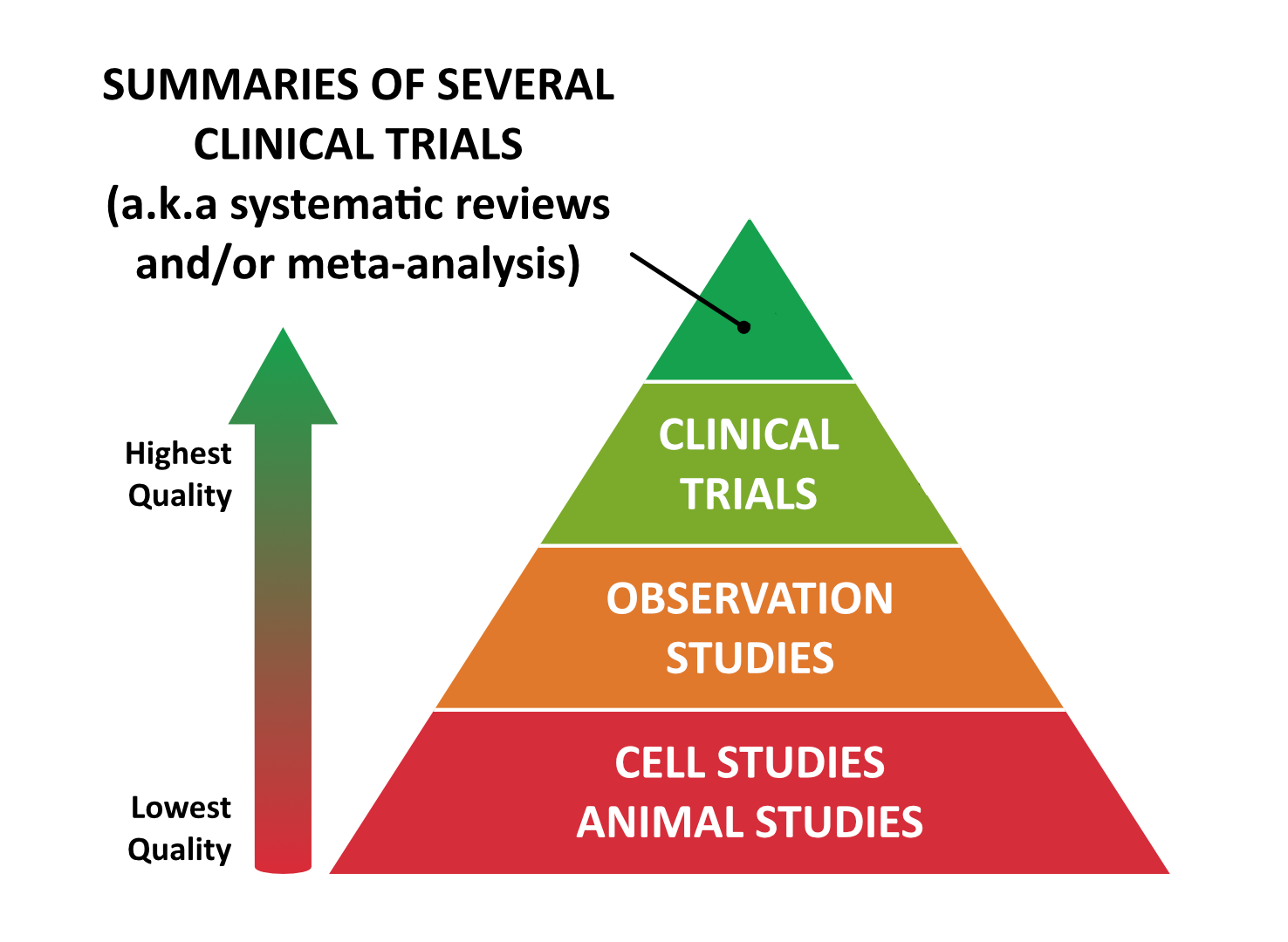
A bit of a definition here. Placebo-controlled clinical trials are where we intervene with humans and see what kind of outcome we have. Even better than that, the very tip of the evidence-based pyramid are summaries of clinical trials, AKA systematic reviews or meta-analyses.
It is important to understand the differences between types of trials to protect you from the people who may be looking at a rat study and tell you that because these rats lost weight on a probiotic that, “Now, this probiotic is a miracle cure for weight loss.” Or again, on the other end of the spectrum, the gastroenterologists who are saying, “Well, not enough research yet on probiotics” even though we have hundreds of clinical trials namely with IBS and probiotics.
This is why the evidence matters. Because it exposes those who don’t know what they’re talking about.
Evidence for Effectiveness
With that kind of prelude, let’s go into the evidence for IBS. Two meta-analyses have shown probiotics to be an effective treatment for IBS with no side effects. That’s important to keep in mind. A multi-strain mixture containing a blend of predominantly lactobacillus and Bifidobacterium strains seems to be the best according to this meta-analysis. Does that sound familiar? Of course, that would be exactly a category one probiotic. Now, when we say two meta-analyses have shown probiotics to be an effective treatment for IBS, what does this mean? In this case, it means that over 1,100 patients were tracked in order to assess how effective probiotics were for IBS. The subjects were given either probiotic or placebo thus guarding against the placebo effect. After a number of weeks, analysis of the subjects’ symptoms was conducted and there was a clear and consistent benefit documented in those using the probiotics than in those on placebo. This is huge.
This is exactly the type of evidence the consumer should be looking to because this asks the question: when you go on a probiotic, just like the group of people in this study, will you see a consistent and notable benefit when you reassess symptoms a number of weeks later? In an additional meta-analysis, the results of 20 clinical trials were reviewed with a total of 1,400 subjects and in all the studies, the subjects were given either probiotics or placebo again, safeguarding against the placebo effect and the probiotic groups showed improvements in global IBS symptoms when compared to the placebo control. This included improvements in constipation, diarrhea, and loose stools. Also, abdominal pain, bloating, flatulence, food intolerance, fatigue, and difficulty sleeping.
This is compelling data and likely why the Canadian Association of Gastroenterology in Clinical Practice, in their guidelines for clinical practice and management of irritable bowel syndrome recommends a trial on probiotics for IBS. That seems pretty darn reasonable to me given the evidence and that some of the other medications for IBS have side effects that we shouldn’t just sweep under the rug.
I should also mention this reference may or may not be in the article by the time you read it because there are a few updates. Before this has even been proofed there are already updates that I want to add to this. Hopefully, this shows you how fervently I tried to stay abreast of the science. But even when consolidating to only the highest quality of clinical trials, probiotics still show benefit. There was another meta-analysis consolidating only to the highest quality clinical trials, 19 of them actually, and they still found a benefit.
To give you a parallel example of this, there are those that would have you believe when using a thyroid medication, you must have a combination of T4 plus T3. So instead of using your standard levothyroxine or Synthroid, you need WP thyroid or nature Throid or Armour. However, when we re-analyze the data looking only at high-quality studies, any benefit that suggests T4 plus T3 is better, is attenuated, meaning that the perceived benefit might be due to bias in the research or poor-quality studies.
Studies show that probiotics can improve digestive issues
- IBS:
- Two meta-analyses showing probiotics to be an effective treatment for IBS with no side effects
- SIBO:
- Multiple studies conclude that probiotics are beneficial in the treatment of SIBO
- Any of the 3 categories have been shown to improve symptoms
- Leaky Gut: Two studies have shown that probiotics promote intestinal repair
- Fungal Overgrowth: Some probiotics are as effective as antifungal drugs and antiparasitic medications
- IBD: Probiotics help to prolong IBD relapse
Probiotics and Intestinal Imbalances
This is important to keep in mind because if something is true, as the quality of data improves, the association will not be wiped away. This is the case for probiotics with IBS. What about probiotics for intestinal imbalances? SIBO, leaky gut, fungus, H. pylori, and infection.
We clearly see probiotics help with SIBO. We also have evidence showing that some probiotics are as effective as antifungal drugs and that probiotics are as effective as antiparasitic medication. So let’s drill into a few of the details here. Again, in clinical trials, probiotics have shown to be effective in treating SIBO and in improving symptoms and lab values. These clinical trials were even summarized in a meta-analysis concluding that probiotics are an effective therapy for SIBO.
Even further to this point, one study found that probiotics were more effective than metronidazole for blasto. We have pretty good evidence. I’m kind of scanning the article and trying to narrow it down because there is so much here to pull from. So another citation, data from 18 clinical trials were summarized in a meta-analysis, which concluded that probiotics are an effective treatment for SIBO. Specifically, they found probiotics reduce bacterial overgrowth in SIBO patients. Probiotics reduce hydrogen concentration in SIBO patients. SIBO patients who take probiotics, experience symptomatic improvement and SIBO patients who take probiotics experience marked reduction in abdominal pain. So the question is, what type of probiotic? Well, a wide variety of probiotic strains were used in these clinical trials and they mostly fell into either category one or category three. This would be our Lacto-Bifido blend probiotic or our soil-based probiotics.
Again, this is important to understand because it frees you from thinking, “I’ve got to find the specific magic protocol or probiotic for SIBO, and if I don’t get the exact one, I might explode or have some other kind of problem.”
Probiotics vs. Antibiotics
Coming back to this comparison between probiotics versus antibiotics and an exciting study looking at 50 subjects diagnosed with SIBO who had chronic abdominal distension. There was a treatment group with half the subjects being treated with metronidazole while the other half took a multi-strain probiotic.
The result: 52% of the subjects taking metronidazole showed improvements in symptoms. 82% of those taking probiotics saw improvements in their symptoms. Conclusion: Probiotics were more effective than standard antibiotic treatments for patients with SIBO and chronic abdominal distension. Do you see now why even though I tried to be pretty cautious and conservative with my language, I don’t take a very cautious stance regarding SIBO and probiotics? Because it hurts patients telling them that they shouldn’t use probiotics if they have SIBO. Again, it’s not a panacea and it’s not going to completely resolve every SIBO case. But to withhold or not use probiotics because you have SIBO is idiotic.
Continuing even further, another exciting study found that probiotics work better for digestive symptoms if you also have SIBO. Patients with IBS and SIBO experienced a 71% reduction in their IBS symptoms as compared to IBS patients without SIBO who only saw a 10% reduction.
So in patients with IBS symptoms placebo, probiotics led to a 71% reduction of their symptoms. IBS patients without SIBO, there was only a 10% reduction in symptoms from using probiotics. In this study, in particular, the probiotic used was actually a combination of category one and category two. So you had predominantly lactobacillus and bifidobacterium plus Saccharomyces boulardii.
So what does this show us? It shows us that any category of probiotic may be able to help for SIBO which is really freeing. It doesn’t mean there’s a magic SIBO probiotic. It means coming back to the three-legged stool analogy or the 3 for BALANCE Probiotic protocol, that any can be used and my clinical observation using all three together at the same time seems to be the most effective. Remember if you are a sensitive person who does react to one category, you can use the two that you tolerate or if you’re extremely sensitive, you can use just one probiotic, but you want to aim for and try to go on all three at the same time. Some people do react. That’s pretty rare from being honest, and I think using a quality formula that’s devoid of any substantial amount of prebiotic also helps to diminish the likelihood that someone will have a negative reaction.
Antibiotic associated diarrhea
- A meta-analysis of 82 randomised control trials showed that all three categories of probiotics worked equally well for improving antibiotic associated diarrhea
Sponsored Resources
I’d like to thank Transcend Labs for making this podcast possible. As per our last interview with Dr. Alex Capano, who has her Ph.D. in cannabinoid research, the best evidence for CBD is regarding the treatment of pain, sleep, and mood conditions like anxiety. You have to be very wary of cure-all health claims. You also have to be cognizant of quality assurance, and this is why I’m happy to say that Transcend Labs pays close attention to this.
They use full-spectrum CBD across all of their products. In fact, they have pretty delicious gummies that I’ve sampled a number of times. They use third party analysis, verifying the safety and potency of all of their products. They use a minimal dosage of 25 milligrams per serving across all products, making it easy to switch from an edible to an oil. You don’t have to do all these dosage conversions. You’re going to have the consistency of dosage across products, and they only use the most effective CBD delivery systems, such as oil, edibles and topical creams.
Leaky Gut, IBD, Depression, and Anxiety
What about probiotics for leaky gut? There have been at least two studies showing that probiotics promote intestinal repair in humans and can help to reduce leaky gut. Regarding fungus, Candida and parasites, in a study of 181 infants, Saccharomyces boulardii or category two was as effective as nystatin and antifungal medication in reducing fungal infection and improved food intolerances.
Additionally, as previously mentioned, probiotics have been shown to have anti-parasitic effects. In a clinical trial of 65 adults infected with Giardia, one group was given standard antibiotic treatment, in this case, metronidazole. A second group was given metronidazole and Saccharomyces boulardii. Results showed a full recovery from the infection for those taking a combination of medication and probiotic. But in the group taking only the medication, 17% of the subjects were still infected with Giardia after treatment.
So you’re looking at a 100% clearance rate to about a 75% clearance rate. So we see a better impact at clearing the infection when we have the synergist of a probiotic.

Moving on. There have been studies that focus on category one and category two probiotics for inflammatory bowel disease. I linked to a number of those studies here. We do have a study showing the ability to help with remission. I think the better data is showing prolonged time relapse-free, and all the data here don’t necessarily show a benefit. We have a better case from an evidence-based perspective for IBS than we do for IBD.
However, there are also fewer studies for IBD. It also would be logical to assume IBD, inflammatory bowel disease, might be a harder condition knowing that severe IBD can lead to the literal surgical removal of part of the colon or small intestine. It can be a more severe condition, so it may be harder to see the same result that we’re looking to get from a mono-therapeutic approach, meaning just probiotics.
What about antibiotic-associated diarrhea? The prestigious Journal of the American Medical Association published a meta-analysis of 82 randomized control trials. They found all three categories of probiotics worked equally well for antibiotic-associated diarrhea. So to those who think maybe I shouldn’t take probiotics while taking antibiotics for whatever reason, there doesn’t seem to be great evidence to support that.
Mood, depression, and anxiety. The Journal of Affective Disorders published a meta-analysis of 10 clinical trials with a total of 1,300 subjects. They compared the effect of probiotics versus placebo on mood. To quote “significant improvements in the moods of individuals with mild to moderate depressive symptoms were noted”. So if you have depression, probiotics may help. If your mood is already fine, they likely won’t take you from regular to super congenial, which again seems reasonable.
In another systematic review and meta-analysis of clinical trials, it was found that probiotics led to a significant reduction in depression and there was also data showing anxiety can be improved from probiotics. The data here are not as strong but still have documented an antianxiety effect in human clinical trials.
Now, what is the best probiotic for depression and anxiety? Well, to the chagrin of some supplement companies here is some powerful and empowering news from the Annals of General Psychiatry. The dose and type of probiotic have varied among these above studies. So what this means is you don’t need a special mood-enhancing probiotic to improve your mood from probiotic supplementation.
Unfortunately, what happens more often than not here, and I understand where this comes from, but I think it reflects an inability to think rather than just regurgitate.
Doctors will say, “Well, there’s inconsistency among the trials, so we can’t really recommend a probiotic for anxiety or depression because we just don’t know which one is the best yet.” Okay, I guess that’s one way of thinking about this.

Another way to approach this would be to see this as good news, as it turns out any quality probiotic seems to have a positive benefit. However, because the studies have been done a bit differently and there is heterogeneity in the data, which researchers don’t like, they tend to err on the side of not offering any probiotics, because there is no study that specifically identifies one that is the best in this situation. We can look at the data here and say, “Okay, well, it’d be great if all the studies use the same formula and we had homogeneity in the data and we could say with super confidence that this was the best formula.” Sure, that would be ideal. But in the real world, we sometimes have to grapple with non-perfect data sets. So in this case, thankfully, different probably optics have been used and all have shown benefit. This is the gut-brain connection.
Mood, Depression and Anxiety
- Studies support that probiotics can help with these conditions
- Best probiotic for these conditions?
- The dose and type vary, there is no special mood-enhancing probiotic
Brain Fog, Mental Clarity, and Sleep
So be wary of the marketers that will tell you that this is the best probiotic for depression, anxiety, what have you. Again, to keep inserting this note of caution, this does not mean that the only thing one should do to repair their gut-brain connection is probiotics and probiotics should not be looked at as such. But certainly, we have enough evidence to undergo a reasonable trial.
Now, what about brain fog? Data here are preliminary but encouraging. Brain fog itself isn’t a popular topic of study.
What we have here are mostly neurodegenerative disease states and then looking at the associated impaired cognition or fuzzy thinking that are subsequent to those and showing that probiotic supplementation can improve cognition or mental clarity in these disease states.

There are two studies showing this in Alzheimer’s, one in bipolar and one in fibromyalgia. So not a strong case, we made there, but certainly it seems reasonable to say, “Hey, grab a few bottles of probiotics, give it about a month or so, and see if you’re noticing a clear improvement. And if you are, let’s continue and if not, perhaps we need to look elsewhere.” It seems pretty darn reasonable to me. Regarding sleep, there was an interesting study published looking at fourth-year medical students and a trial was done over a two year period comparing sleep during times of exam stress.
The students who took category one probiotics showed superior sleep quality. In another clinical trial, participants reported that their sleep quality improved after six weeks of taking probiotics.
In yet another, sleep quality improved in those with IBS. There was definitely this kind of gut sleep connection. So not surprising to see that as the gut health improved in a given individual, their sleep also improved.

Additional study in depressive patients showed that probiotics led to less sleep disruption in the placebo group. What about auto-immunity? I have two competing thoughts here. One, the evidence in autoimmune conditions is preliminary. There is some exciting evidence but it’s not as robust of the cases I’d like to see. That being said, at least from a theoretical perspective, and again I want to be cautious, knowing the impact that gut health has on the immune system, it does seem that if we’re going to recommend conservative and noninvasive therapies such as diet, gut-healing nutrients, probiotics that improve one’s gut health, that in the worst-case scenario, the individual may have fewer symptoms with probiotics. Best case scenario, they may have fewer symptoms and improved autoimmunity.
There was one study that found early probiotic administration to type one diabetics essentially prevented type one diabetes formation in those who were predisposed. In multiple sclerosis, there’s been one study finding that patients showed less disability and lower insulin resistance and fewer inflammatory markers. So it didn’t seem to really make a significant impact on the disease itself but some of the associated comorbidities.
In rheumatoid arthritis, three different studies found that probiotic mixtures essentially reduced RA activity, although one study did not show any improvement. The findings here essentially looked like joint swelling and tenderness were reduced, less pain, improved inflammatory markers, improved function and/or improved imaging findings.
Sleep Quality
- In one study, students who took category one probiotics showed improved sleep quality
- Sleep quality improved with those with IBS
- Probiotics led to less sleep disruption in those with depression
Metabolism and Weight Control
So again, some preliminary data, we don’t want to infer too much from that, but also exciting in metabolism. First of all, there’s an association between SIBO and being overweight. The data bit here that is interesting is essentially regarding the ability of those with SIBO to see improvements in metabolism. Treating SIBO hasn’t shown a robust impact on weight. I don’t think anything on weight itself has been published in terms of a treatment impact. But we do see improved blood sugar and cholesterol. How much of an impact gut interventions have on metabolism, I think it’s up for debate. That being said, I’ve seen some patients who do experience somewhat remarkable weight loss as they improve their gut health, but that doesn’t seem to be the norm and perhaps that’s why we’re not seeing a ton being published nor may we ever.
I think it’s reasonable to say, “Let’s improve your gut health and hope for the best regarding your metabolism.” It’s not reasonable to say that this probiotic is going to lead to massive reductions in blood sugar, cholesterol or body weight. Although that being said, prebiotics have shown some fairly impressive abilities to lower blood glucose levels.
Food and Seasonal Allergies
Now moving on to food allergy and seasonal allergy. A systematic review of 15 clinical trials found that probiotics can improve dairy tolerance. Great news for those who are dairy intolerant. A meta-analysis of 22 randomized controlled trials concluded that probiotics can improve seasonal allergy. So to those who say, “Well, you can’t give probiotics to someone with histamine intolerance.” 22 clinical trials looking at the histamine-mediated condition of seasonal allergy counter that.
There may be a little too much speculation there. There are also mixed data showing that in children, probiotic administration may reduce the formation of allergy. So there does seem to be a positive impact on the immune system, on food tolerance, at least dairy tolerance, and seasonal allergies as mediated by histamine. Now, what about female hormone imbalances? There’s less evidence here. I mean, there’s definitely some mechanistic evidence that we point to in the study. I’m going to gloss over that for now.
Key Takeaways
- Probiotics can improve dairy tolerance
- Can improve seasonal allergies
Probiotics, PCOS and Female Hormones
One study that I think is the most important is looking at… This is either a meta-analysis or a systematic review of 13 studies looking at 855 women with PCOS and finding that probiotic use improved hormonal and inflammatory markers in these women. So there is something there, but not a ton of data. Also, not a ton of research. It’s not to say there’s a bunch of research showing no effect. I don’t believe there’d be much research at all, but from what quality research has been done, we’re seeing some encouraging findings.
I should also mention female hormones. The reason in Healthy Gut, Healthy You, I recommend Estro-Harmony and Progest-Harmony for women who have symptoms of hot flashing, PMS and other types of female hormone mediated symptoms is because I found out to be quite effective. So to see digestive imbalances co-occurring with female hormone imbalances seems to be somewhat common and they tend to respond very well when using both gut supports. In this case, probiotics is a great place to start combined with female hormone supports, namely our Estro-Harmony and Progest-Harmony, which are just herbs that help you balance out female hormones.
Female Hormone Imbalances
- Probitoic use improved hormonal and inflammatory markers in women with PCOS
- Gut imbalances tend to be common with female hormone imbalances
Blood Pressure and Cholesterol
Okay. Moving on to blood pressure and cholesterol, the short story here is yet we’ve got data showing positive effects. One meta-analysis looking at 68 clinical trials with 3,800 participants found benefit. This includes benefits in improving cholesterol profiles, other data showing the ability to reduce LDL, other data showing the ability to lower homocysteine, and other data showing a modest effect on blood pressure. But the key point there is the effect seems to be what I would consider clinically insignificant.
So statistically or mathematically nothing was significant. But in terms of, is this anything that’s going to move the needle clinically? It doesn’t really seem to be so. But another way we can look at this is, this is a small side benefit of using a probiotic. Now, what about thyroid function? Well, one of the things we just reviewed in this article is that study appearing in the World Journal of Gastroenterology and they looked at just over 1,800 patients to determine what factors were most tightly associated with SIBO. They looked at surgical removal of the stomach, acid lowering drug use, surgery of the colons, stenosis, gastro-paresis, neuropathy or nerve damage, immunosuppressive drug use, diabetes, being hypothyroid, and being on thyroid medication.
To the shock of the researchers, being hypothyroid or being on Levothyroxine were the most tightly associated factors with SIBO. So there definitely seems to be an association between thyroid and the gut, in this case SIBO.
View Dr. Ruscio’s Additional Resources
Now, I think it is important to understand here. A couple other things that are important to appreciate here are the connection between SIBO, H. pylori, and autoimmune thyroid. You can read about that in the article. We’ve talked about that before. There’s definitely some data drawing an association. I don’t know if we can go as far to say it’s causal, but we do know that H. pylori may potentiate Hashimoto’s or Graves.
We also know that SIBO can be associated with hypothyroid. There’s a nice diagram here. Saccharomyces boulardii may have the strongest anti H. pylori action, and most of the studies looking at probiotics for SIBO have used the category one and category three probiotics. So we can kind of paint this tacit recommendation that these three probiotics, by helping to combat SIBO and reduce H. pylori, may benefit the gut thyroid connection.
There’s one additional study. Again, this may or may not be in the article by the time that you read it because, again, I’m updating this article regularly. When I say updating, the essence is not going to change, just the amount of evidence backing up these claims is going to continue to evolve. Of course, if there’s ever any evidence that refutes one of the claims, I will make a strong editorial note about that and we will walk back any claim. But again, we’re not making any strong claims that don’t have strong evidence so I doubt that’s ever going to happen.
One very exciting study showing that the category of one probiotic led to a decrease in the amount of thyroid medication that these subjects needed. There are a number of studies showing that antibiotics, namely when treating H. pylori, can lead to reduced dosage of thyroid hormone medication. This was the first, but not surprising study to show that a probiotic could achieve the same thing. Why is that? Well, again, we know that when there is dysbiosis in the gut that can lead to malabsorption and because thyroid hormone is exclusively absorbed in the small intestine, it makes sense that any intervention that improves small intestinal health will improve absorption and that will lead to reduced medication needs. Encouraging stuff there.
Key Takeaways
- Data shows a positive effect – more research is needed
- Probiotics improve cholesterol, reduce LDL, lower homocysteine
The Gut Skin Connection
Then finally, moving on to skin health. There is a gut skin connection as you’ve likely heard me remark in the past. There’s an old saying in naturopathic medicine, which is, “The health of the skin is a reflection of the health of one’s gut.” It doesn’t surprise me to see that in a recent review paper summarizing the research into acne and the microbiota, this connection is confirmed. Three clinical trials provide the strongest evidence and two of these clinical trials showed that in this case topical probiotics were effective for treating acne.
Another study essentially found that probiotics were about as effective as antibiotics for treating acne. This is something we see somewhat routinely in the clinic that as gut health improves these weird lesions, breakouts, highs, atopic dermatitis, pimples, rashing tend to improve.
Key Takeaways
- The health of the skin is a reflection of the health of the gut
- Topical probiotics were effective for treating acne
- Probiotics were about as effective as antibiotics for acne
Infant and Mother Health
The final point I want to make here is what about infant and mom health? We’ll go into a little bit more detail about using probiotics with infants later, but the short summary is researchers have found benefits from probiotic use in infants, including less colic and less irritability, improved diarrhea, few respiting episodes, and fewer respiratory infections.
Now, women who took probiotics during pregnancy had fewer incidences of gestational diabetes, preeclampsia, which is essentially high blood pressure during pregnancy, improvements in excessive weight gain, and less vaginal bacteria infections. More studies show that probiotics appear safe for infants even preterm infants, protect infants against intestinal fungus, AKA candida, reduce the risk of ear and respiratory infection in babies and reduce colic. So some pretty good evidence there…
Key Takeaways
- Benefits of probiotic use in infants include less colic, less irritability, reduced risk for infections, improved diarrhea, and less spitting up episodes
- Women who took probiotics during pregnancy had less incidences of vaginal bacterial infections, preeclampsia, less excessive weight gain and gestational diabetes
Episode Wrap Up
And what we will do in the third and final part of this read is to establish what probiotic formulas are best for infants. I’m sure it’s not surprising to hear me say there is no magic infant formula even though some formulas are marketed as being especially for infants. So we’ll detail that later. So I’ll cut off the second read here.
The next section that we’ll go into is probably the most important, which is the 3 for BALANCE Probiotic Protocol. I’ll talk about specifics of this protocol, how to dose it, how long to stay on it for, and then also just fill in some of the nuances in terms of how we use all this knowledge that we now have about probiotics effectively in this 3 for BALANCE Probiotic Protocol. Again, this gives you the tools to use a probiotic protocol effectively and then reevaluate. It arms you to get off of the merry-go-round of new blogs, new podcasts, probiotic on the market. The “I’m going to try this, try that” mindset. I’d love to tell you that the newest means the best, but it reflects a lack of understanding about how to use probiotics effectively. So that is what we will go into detail next on is the 3 for BALANCE Probiotic Protocol. Okay, guys, hopefully this is helping and I will talk to you again soon.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.



Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!