How Should I Use Thyroid Supplements?
Best Supplements for Thyroid Conditions
- Use the Right Supplements|
- Supplements for All Thyroid Conditions|
- Probiotics|
- Vitamin D|
- Selenium|
- Supplements for Hypothyroid|
- Betaine HCL|
- Iron|
- Zinc|
- Supplements for Hyperthyroid|
- L-Carnitine|
- Bugleweed & Lemon Balm|
- Short-Term Iodine|
- Iodine Supplementation?|
- Assess Iodine|
- Bottom Line|
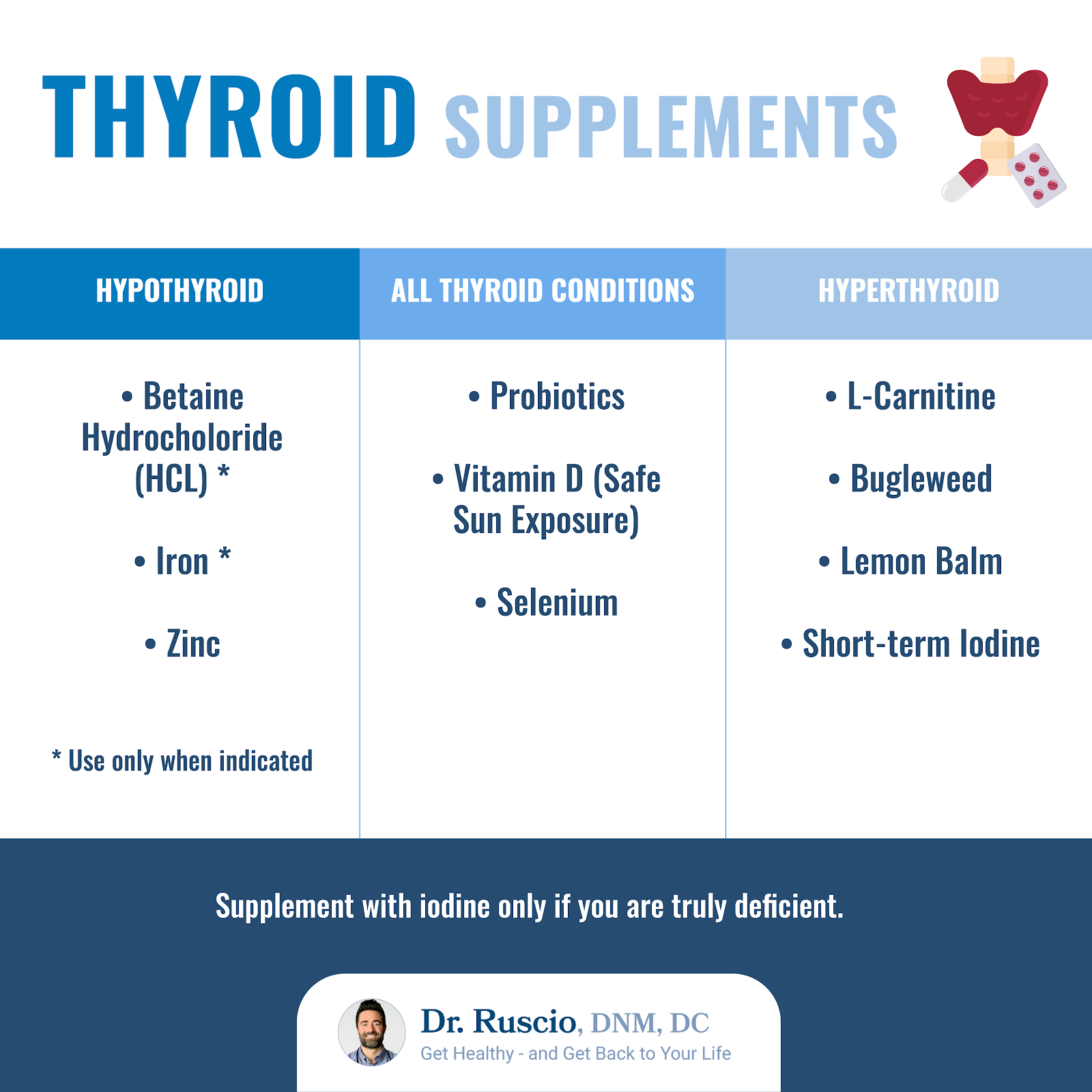
- Use the right supplements for your particular thyroid problem.
- Most thyroid patients can benefit from probiotics, vitamin D, and selenium supplementation.
- Some hypothyroid patients may benefit from betaine HCL, iron, and zinc.
- Hyperthyroid patients may benefit from L-Carnitine, bugleweed, lemon balm, and short-term iodine.
- Only supplement with iodine if you have clear evidence of deficiency.
If you’ve been diagnosed with a thyroid condition or you’re experiencing thyroid symptoms like fatigue, weight gain or hair loss, you may understandably want to know what dietary supplements could help support your thyroid health. Let’s take a look at what you need to know about choosing thyroid supplements for your thyroid condition.

Use the Right Thyroid Supplements for Your Thyroid Condition
Different thyroid supplements are recommended for different types of thyroid conditions. Be sure to work with your doctor and only include supplements that are indicated for your particular situation.
And before you reach for supplements to support your thyroid health, let’s keep the big picture in mind: A healthy thyroid begins with a healthy gut, so make sure to include thyroid support supplements only after you have addressed your gut health.
Thyroid Support Supplements for All Thyroid Conditions
There are a few particular supplements that research suggests are helpful for your thyroid, no matter which type of thyroid imbalance you have. These include:
- Probiotics
- Vitamin D
- Selenium
Let’s take a look at what the science says about how these supplements can support your thyroid health.
Support Gut Health with Probiotics
Research suggests there is a close link between gut and thyroid health, and supporting your gut health first may resolve some cases of thyroid imbalance.
Probiotics can powerfully balance your gut microbiome and repair your gut environment, with few side effects. [1, 2, 3, 4]
Probiotics help treat a range of intestinal problems, including:
- IBS (Irritable Bowel Syndrome) [5, 6, 7]
- IBD, including Crohn’s disease [8, 9, 10]
- One interesting study even found that probiotics may reduce your need for the thyroid medication, levothyroxine (synthroid). [11]
- Leaky Gut [12, 13, 14, 15]
- Small Intestinal Bacterial Overgrowth (SIBO) [16, 17], which has been associated with thyroid disease. [18]
If you have a thyroid disorder, include probiotics to help balance your gut and improve your thyroid health.
Vitamin D
Research shows that vitamin D deficiency is associated with higher levels of thyroid antibodies.
- One small study showed that hypothyroidism severity was correlated with low vitamin D levels. [19]
- Another study found significantly lower vitamin D levels in those with hypothyroid disease compared to those without. [20]
Research also suggests that supplementing with vitamin D to correct this deficiency can improve autoimmune hypothyroidism:
- A meta-analysis (the highest quality science) concluded that vitamin D supplementation improves thyroid antibody levels. [21]
Though more research is needed, it appears that supplementing vitamin D may improve your thyroid health and lower thyroid antibodies, especially for patients with Hashimoto’s thyroiditis. And though vitamin D supplements can help, safe sun exposure is a free, and more bioavailable way to ensure you’re getting adequate vitamin D.
Selenium
Selenium has been shown to be supportive for both hypothryoid and hyperthryoid patients, but some of the data are unclear. [22] Let’s review the evidence.
Research shows selenium improves thyroid antibodies and ultrasound findings for hypothyroid patients:
- A systematic review and meta-analysis (the highest quality science) showed that selenium supplementation reduced thyroid antibodies for patients on prescription thyroid medication as well as in untreated patients. [23]
- In two clinical trials, hypothyroid patients who took selenium showed reduced thyroid antibodies compared to a placebo [24] and improved ultrasound findings. [25]
Selenium has also been shown to be beneficial for hyperthyroidism:
- A systematic review determined that selenium supplementation reduced thyroid hormone levels and antibodies for hyperthryoid patients. [26]
- Another study showed that hyperthyroid patients with higher levels of selenium on blood tests were less likely to relapse after treatment. [27]
In spite of these positive effects, not all the research agrees.
- A systematic review and meta-analysis concluded that long-term supplementation with selenium had no effect on thyroid hormone levels or symptoms for hypothyroid patients. [28]
- Another systematic review of selenium supplementation showed decreased thyroid antibodies at 6 months but not at 9 months. [29]
- Several small studies didn’t show decreased thyroid antibodies after selenium supplementation. [30, 31, 32, 33]
The Bottom Line: Even though the evidence isn’t totally clear, a trial of selenium therapy seems reasonable because selenium is neither expensive nor invasive. You can try including selenium for 3 months and assess how you respond. There is no need for long-term, ongoing supplementation with selenium.

Supplements for Hypothyroidism
There are a few additional supplements that may be helpful for some — but not all — hypothyroid patients. The key here is to add these supplements only if your unique situation suggests their use. Let’s take a look.
Betaine Hydrochloride (HCL)
If you’re hypothyroid (have an underactive thyroid gland), you may need supplemental stomach acid.
Research shows that up to 40% of hypothyroid patients also have stomach autoimmunity, resulting in low stomach acid, [34, 35] as well as anemia and vitamin B12 deficiency. [36, 37, 38, 39, 40, 41, 42]
Supplemental betaine hydrochloride (HCL) can increase stomach acid levels, which can help your body better absorb iron and vitamin B12, but not all hypothyroid patients need this.
You’re most likely to benefit from betaine HCL if you:
- Are over 65
- Have a history of anemia (see Iron, below)
- Have a history of an autoimmune condition
If you are hypothyroid and meet these criteria, consider including a betaine HCL supplement.
As with all supplements, do a trial to see how you feel and adjust accordingly. If you feel a warmness or burning when you take HCL, it’s a sign that you do not need this supplement and you should stop taking it. Extremely high doses of HCL, as advised by some practitioners, are not needed.
Iron
If you’re taking prescription medication for hypothyroidism but it doesn’t seem to be working, low iron levels can be one reason why. Iron deficiency anemia is correlated with hypothyroid symptoms, especially fatigue. But not all hypothyroid patients require iron supplementation.
- One study found that when two-thirds of hypothyroid women on thyroid medication increased their serum ferritin (the storage form of iron) levels to greater than 100 micrograms per liter with iron, their fatigue improved. [43]
- A small study showed that low serum ferritin was correlated with hypothyroid lab markers. [44]
- Another study showed that iron deficiency was related to thyroid hormone status. [45]
If you are hypothyroid and have a history of iron deficiency anemia or your ferritin blood test is below 100 mcg/L, iron supplementation may help improve your thyroid symptoms.
Zinc
If you are hypothyroid, you may be deficient in zinc and supplementing may help.
- A systematic review found a correlation between severity of hypothyroidism and low zinc and selenium levels. [46]
- A clinical trial of obese hypothryoid women found that both zinc alone and zinc in combination with selenium improved thyroid hormone levels. [47]
- In a clinical trial, 6 months of zinc supplementation improved serum thyroid markers. [48]
- In another small study, low zinc levels were correlated with higher thyroid antibodies, and increased thyroid volume in patients with goiter. [49]
These data show a correlation between zinc status and thyroid function, but they don’t yet show a definitive improvement from zinc supplementation. Adding supplemental zinc may be worth a 1-month trial. If you haven’t noticed any improvement, you may not need to continue.
Supplements for Hyperthyroidism
A few supplements stand out as supports for hyperthyroidism. For a more thorough discussion of natural treatment of Graves’ disease and supplements for hyperthyroidism, see Natural Management of Graves’ Disease.
L-Carnitine
L-Carnitine is an amino acid that can both help prevent and reverse hyperthyroid symptoms. It has no known toxicity or drug interactions, and causes minimal side effects. [50, 51]
Bugleweed and Lemon Balm
Bugleweed and Lemon Balm are two herbs that can help manage hyperthryoid symptoms. [52] They help impact T3, T4, and thyroid stimulating hormone (TSH) levels to reduce symptoms, and may help with increased heart rate [53] and blood pressure common in hyperthyroidism.
Iodine (for Hyperthyroid Flares)
Iodine seems to have utility as a short-term therapy to help manage hyperthyroidism but shouldn’t be considered a primary approach. [54] (See Iodine Supplements, below)
What About Iodine Supplements?
Too much or too little iodine can cause health problems. Supplement only if you have true iodine deficiency.
Many practitioners recommend supplementing iodine for hypothyroid patients, sometimes in very high doses, because the thyroid hormone molecule is made up partly of iodine.
The data do not support using iodine supplements for thyroid health, except in cases of true iodine deficiency. Multiple studies have shown that iodine supplements increase the overall incidence of hypothyroid conditions, including goiter and autoimmunity. [55, 56, 57]
Interestingly, reducing iodine intake with a low-iodine diet has been shown to normalize serum thyroid markers and symptoms for some. [58, 59, 60]
These data suggest many hypothyroid patients may, in fact, benefit from less iodine. Unless you are truly iodine deficient, you probably don’t need more iodine.
Assessing Your Iodine Levels
The most accessible and affordable way to assess your need for iodine would be to track your diet for one-to-two weeks with the food-tracking app Chronometer. Once complete, you can print out a micronutrient report of your diet. If it looks like you aren’t getting enough dietary iodine, first increase your intake of iodine-rich foods, including seafoods, kelp, whole eggs, dairy products (if tolerated), and iodized salt.
If you’re still concerned about your iodine levels, you can do a 24-hour urinary iodine-creatinine ratio test. This test is the most accurate option. [61]
If you truly believe you are iodine deficient, you can run a short experiment. Use 1,000-1,200 milligrams of iodine per day, and work with your health care provider to monitor your TSH levels to see how you respond.
The Bottom Line
The first line of defense for managing your thyroid condition will always be to restore your gut health. After that, include appropriate thyroid support supplements to help support your thyroid function and gut health. Only include an iodine supplement if you are truly iodine deficient.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
-
Sindhu KN, Sowmyanarayanan TV, Paul A, et al. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014;58(8):1107-1115. doi:10.1093/cid/ciu065
-
Dinleyici EC, Eren M, Dogan N, Reyhanioglu S, Yargic ZA, Vandenplas Y. Clinical efficacy of Saccharomyces boulardii or metronidazole in symptomatic children with Blastocystis hominis infection. Parasitol Res. 2011;108(3):541-545. doi:10.1007/s00436-010-2095-4
-
Besirbellioglu BA, Ulcay A, Can M, et al. Saccharomyces boulardii and infection due to Giardia lamblia. Scand J Infect Dis. 2006;38(6-7):479-481. doi:10.1080/00365540600561769
-
Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017;51(4):300-311. doi:10.1097/MCG.0000000000000814
-
Yuan F, Ni H, Asche CV, Kim M, Walayat S, Ren J. Efficacy of Bifidobacterium infantis 35624 in patients with irritable bowel syndrome: a meta-analysis. Curr Med Res Opin. 2017;33(7):1191-1197. doi:10.1080/03007995.2017.1292230
-
Tiequn B, Guanqun C, Shuo Z. Therapeutic effects of Lactobacillus in treating irritable bowel syndrome: a meta-analysis. Intern Med. 2015;54(3):243-249. doi:10.2169/internalmedicine.54.2710
-
McFarland LV, Dublin S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J Gastroenterol. 2008;14(17):2650-2661. doi:10.3748/wjg.14.2650
-
Hedin C, Whelan K, Lindsay JO. Evidence for the use of probiotics and prebiotics in inflammatory bowel disease: a review of clinical trials. Proc Nutr Soc. 2007;66(3):307-315. doi:10.1017/S0029665107005563
- Hedin C, Whelan K, Lindsay JO. Evidence for the use of probiotics and prebiotics in inflammatory bowel disease: a review of clinical trials. Proc Nutr Soc. 2007;66(3):307-315. doi:10.1017/S0029665107005563
-
Kruis W, Fric P, Pokrotnieks J, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut. 2004;53(11):1617-1623. doi:10.1136/gut.2003.037747
-
Talebi S, Karimifar M, Heidari Z, Mohammadi H, Askari G. The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial. Complement Ther Med. 2020;48:102234. doi:10.1016/j.ctim.2019.102234
-
McFarlin BK, Henning AL, Bowman EM, Gary MA, Carbajal KM. Oral spore-based probiotic supplementation was associated with reduced incidence of post-prandial dietary endotoxin, triglycerides, and disease risk biomarkers. World J Gastrointest Pathophysiol. 2017;8(3):117-126. doi:10.4291/wjgp.v8.i3.117
-
Sindhu KN, Sowmyanarayanan TV, Paul A, et al. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014;58(8):1107-1115. doi:10.1093/cid/ciu065
-
Lamprecht M, Bogner S, Schippinger G, et al. Probiotic supplementation affects markers of intestinal barrier, oxidation, and inflammation in trained men; a randomized, double-blinded, placebo-controlled trial. J Int Soc Sports Nutr. 2012;9(1):45. Published 2012 Sep 20. doi:10.1186/1550-2783-9-45
-
McFarlin BK, Henning AL, Bowman EM, Gary MA, Carbajal KM. Oral spore-based probiotic supplementation was associated with reduced incidence of post-prandial dietary endotoxin, triglycerides, and disease risk biomarkers. World J Gastrointest Pathophysiol. 2017;8(3):117-126. doi:10.4291/wjgp.v8.i3.117
-
Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017;51(4):300-311. doi:10.1097/MCG.0000000000000814
-
Soifer LO, Peralta D, Dima G, Besasso H. Eficacia comparativa de un probiótico vs un antibiótico en la respuesta clínica de pacientes con sobrecrecimiento bacteriano del intestino y distensión abdominal crónica funcional: un estudio piloto [Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study]. Acta Gastroenterol Latinoam. 2010;40(4):323-327.
-
Konrad P, Chojnacki J, Kaczka A, Pawłowicz M, Rudnicki C, Chojnacki C. Ocena czynności tarczycy u osób z zespołem przerostu bakteryjnego jelita cienkiego [Thyroid dysfunction in patients with small intestinal bacterial overgrowth]. Pol Merkur Lekarski. 2018;44(259):15-18.
-
Mackawy AM, Al-Ayed BM, Al-Rashidi BM. Vitamin d deficiency and its association with thyroid disease. Int J Health Sci (Qassim). 2013;7(3):267-275. doi:10.12816/0006054
-
Bozkurt NC, Karbek B, Ucan B, et al. The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis. Endocr Pract. 2013;19(3):479-484. doi:10.4158/EP12376.OR
-
Wang S, Wu Y, Zuo Z, Zhao Y, Wang K. The effect of vitamin D supplementation on thyroid autoantibody levels in the treatment of autoimmune thyroiditis: a systematic review and a meta-analysis. Endocrine. 2018;59(3):499-505. doi:10.1007/s12020-018-1532-5
-
Drutel A, Archambeaud F, Caron P. Selenium and the thyroid gland: more good news for clinicians. Clin Endocrinol (Oxf). 2013;78(2):155-164. doi:10.1111/cen.12066
-
Wichman J, Winther KH, Bonnema SJ, Hegedüs L. Selenium Supplementation Significantly Reduces Thyroid Autoantibody Levels in Patients with Chronic Autoimmune Thyroiditis: A Systematic Review and Meta-Analysis. Thyroid. 2016;26(12):1681-1692. doi:10.1089/thy.2016.0256
-
Gärtner R, Gasnier BC. Selenium in the treatment of autoimmune thyroiditis. Biofactors. 2003;19(3-4):165-170. doi:10.1002/biof.5520190309
-
Gärtner R, Gasnier BC, Dietrich JW, Krebs B, Angstwurm MW. Selenium supplementation in patients with autoimmune thyroiditis decreases thyroid peroxidase antibodies concentrations. J Clin Endocrinol Metab. 2002;87(4):1687-1691. doi:10.1210/jcem.87.4.8421
-
Zheng H, Wei J, Wang L, et al. Effects of Selenium Supplementation on Graves’ Disease: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2018;2018:3763565. Published 2018 Sep 26. doi:10.1155/2018/3763565
-
Wertenbruch T, Willenberg HS, Sagert C, et al. Serum selenium levels in patients with remission and relapse of graves’ disease. Med Chem. 2007;3(3):281-284. doi:10.2174/157340607780620662
-
Winther KH, Wichman JE, Bonnema SJ, Hegedüs L. Insufficient documentation for clinical efficacy of selenium supplementation in chronic autoimmune thyroiditis, based on a systematic review and meta-analysis. Endocrine. 2017;55(2):376-385. doi:10.1007/s12020-016-1098-z
-
Zheng H, Wei J, Wang L, et al. Effects of Selenium Supplementation on Graves’ Disease: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2018;2018:3763565. Published 2018 Sep 26. doi:10.1155/2018/3763565
-
Eskes SA, Endert E, Fliers E, et al. Selenite supplementation in euthyroid subjects with thyroid peroxidase antibodies. Clin Endocrinol (Oxf). 2014;80(3):444-451. doi:10.1111/cen.12284
-
Mao J, Pop VJ, Bath SC, Vader HL, Redman CW, Rayman MP. Effect of low-dose selenium on thyroid autoimmunity and thyroid function in UK pregnant women with mild-to-moderate iodine deficiency. Eur J Nutr. 2016;55(1):55-61. doi:10.1007/s00394-014-0822-9
-
Esposito D, Rotondi M, Accardo G, et al. Influence of short-term selenium supplementation on the natural course of Hashimoto’s thyroiditis: clinical results of a blinded placebo-controlled randomized prospective trial. J Endocrinol Invest. 2017;40(1):83-89. doi:10.1007/s40618-016-0535-4
-
Kahaly GJ, Riedl M, König J, Diana T, Schomburg L. Double-Blind, Placebo-Controlled, Randomized Trial of Selenium in Graves Hyperthyroidism. J Clin Endocrinol Metab. 2017;102(11):4333-4341. doi:10.1210/jc.2017-01736
-
Lahner E, Annibale B. Pernicious anemia: new insights from a gastroenterological point of view. World J Gastroenterol. 2009;15(41):5121-5128. doi:10.3748/wjg.15.5121
-
Sterzl I, Hrdá P, Matucha P, Cerovská J, Zamrazil V. Anti-Helicobacter Pylori, anti-thyroid peroxidase, anti-thyroglobulin and anti-gastric parietal cells antibodies in Czech population. Physiol Res. 2008;57 Suppl 1:S135-S141.
-
Toh BH. Pathophysiology and laboratory diagnosis of pernicious anemia. Immunol Res. 2017;65(1):326-330. doi:10.1007/s12026-016-8841-7
-
Rodriguez-Castro KI, Franceschi M, Miraglia C, et al. Autoimmune diseases in autoimmune atrophic gastritis. Acta Biomed. 2018;89(8-S):100-103. Published 2018 Dec 17. doi:10.23750/abm.v89i8-S.7919
-
Utiyama SRR, De Bem RS, Skare TL, et al. Anti-parietal cell antibodies in patients with autoimmune thyroid diseases. J Endocrinol Invest. 2018;41(5):523-529. doi:10.1007/s40618-017-0755-2
-
Collins AB, Pawlak R. Prevalence of vitamin B-12 deficiency among patients with thyroid dysfunction. Asia Pac J Clin Nutr. 2016;25(2):221-226. doi:10.6133/apjcn.2016.25.2.22
-
Jabbar A, Yawar A, Waseem S, et al. Vitamin B12 deficiency common in primary hypothyroidism [published correction appears in J Pak Med Assoc. 2009 Feb;59(2):126. Wasim, Sabeha [corrected to Waseem, Sabiha]]. J Pak Med Assoc. 2008;58(5):258-261.
-
Ness-Abramof R, Nabriski DA, Braverman LE, et al. Prevalence and evaluation of B12 deficiency in patients with autoimmune thyroid disease. Am J Med Sci. 2006;332(3):119-122. doi:10.1097/00000441-200609000-00004
-
Gyftaki H, Kesse-Elias M, Koutras D, Pandos P, Papazoglou S, Moulopoulos S. Serum vitamin B12 and folic acid levels in hyperthyroidism. Nuklearmedizin. 1979;18(6):278-282.
-
Rayman MP. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc Nutr Soc. 2019;78(1):34-44. doi:10.1017/S0029665118001192
- Sachdeva A, Singh V, Malik I, Roy PH, Madaan H, Nair R. Association between serum ferritin and thyroid hormone profile in hypothyroidism. Int J Med Sci Public Health. 2015; 4(6): 863-865. doi: 10.5455/ijmsph.2015.24012015174
-
Soliman AT, De Sanctis V, Yassin M, Wagdy M, Soliman N. Chronic anemia and thyroid function. Acta Biomed. 2017;88(1):119-127. Published 2017 Apr 28. doi:10.23750/abm.v88i1.6048
-
Talebi S, Ghaedi E, Sadeghi E, et al. Trace Element Status and Hypothyroidism: A Systematic Review and Meta-analysis. Biol Trace Elem Res. 2020;197(1):1-14. doi:10.1007/s12011-019-01963-5
-
Mahmoodianfard S, Vafa M, Golgiri F, et al. Effects of Zinc and Selenium Supplementation on Thyroid Function in Overweight and Obese Hypothyroid Female Patients: A Randomized Double-Blind Controlled Trial. J Am Coll Nutr. 2015;34(5):391-399. doi:10.1080/07315724.2014.926161
-
Kandhro GA, Kazi TG, Afridi HI, et al. Effect of zinc supplementation on the zinc level in serum and urine and their relation to thyroid hormone profile in male and female goitrous patients. Clin Nutr. 2009;28(2):162-168. doi:10.1016/j.clnu.2009.01.015
-
Ertek S, Cicero AF, Caglar O, Erdogan G. Relationship between serum zinc levels, thyroid hormones and thyroid volume following successful iodine supplementation. Hormones (Athens). 2010;9(3):263-268. doi:10.14310/horm.2002.1276
-
Benvenga S, Ruggeri RM, Russo A, Lapa D, Campenni A, Trimarchi F. Usefulness of L-carnitine, a naturally occurring peripheral antagonist of thyroid hormone action, in iatrogenic hyperthyroidism: a randomized, double-blind, placebo-controlled clinical trial. J Clin Endocrinol Metab. 2001;86(8):3579-3594. doi:10.1210/jcem.86.8.7747
-
Benvenga S, Amato A, Calvani M, Trimarchi F. Effects of carnitine on thyroid hormone action. Ann N Y Acad Sci. 2004;1033:158-167. doi:10.1196/annals.1320.015
-
Auf’mkolk M, Ingbar JC, Kubota K, Amir SM, Ingbar SH. Extracts and auto-oxidized constituents of certain plants inhibit the receptor-binding and the biological activity of Graves’ immunoglobulins. Endocrinology. 1985;116(5):1687-1693. doi:10.1210/endo-116-5-1687
-
Beer AM, Wiebelitz KR, Schmidt-Gayk H. Lycopus europaeus (Gypsywort): effects on the thyroidal parameters and symptoms associated with thyroid function. Phytomedicine. 2008;15(1-2):16-22. doi:10.1016/j.phymed.2007.11.001
-
Philippou G, Koutras DA, Piperingos G, Souvatzoglou A, Moulopoulos SD. The effect of iodide on serum thyroid hormone levels in normal persons, in hyperthyroid patients, and in hypothyroid patients on thyroxine replacement. Clin Endocrinol (Oxf). 1992;36(6):573-578. doi:10.1111/j.1365-2265.1992.tb02267.x
-
Foley TP Jr. The relationship between autoimmune thyroid disease and iodine intake: a review. Endokrynol Pol. 1992;43 Suppl 1:53-69.
-
Katagiri R, Yuan X, Kobayashi S, Sasaki S. Effect of excess iodine intake on thyroid diseases in different populations: A systematic review and meta-analyses including observational studies. PLoS One. 2017;12(3):e0173722. Published 2017 Mar 10. doi:10.1371/journal.pone.0173722
-
Gaberšček S, Gaberšček B, Zaletel K. Incidence of thyroid disorders in the second decade of adequate iodine supply in Slovenia [published online ahead of print, 2020 May 6]. Wien Klin Wochenschr. 2020;10.1007/s00508-020-01662-5. doi:10.1007/s00508-020-01662-5
-
Yoon SJ, Choi SR, Kim DM, et al. The effect of iodine restriction on thyroid function in patients with hypothyroidism due to Hashimoto’s thyroiditis. Yonsei Med J. 2003;44(2):227-235. doi:10.3349/ymj.2003.44.2.227
-
Tajiri J, Higashi K, Morita M, Umeda T, Sato T. Studies of hypothyroidism in patients with high iodine intake. J Clin Endocrinol Metab. 1986;63(2):412-417. doi:10.1210/jcem-63-2-412
-
Kasagi K, Iwata M, Misaki T, Konishi J. Effect of iodine restriction on thyroid function in patients with primary hypothyroidism. Thyroid. 2003;13(6):561-567. doi:10.1089/105072503322238827
-
Ji C, Lu T, Dary O, et al. Systematic review of studies evaluating urinary iodine concentration as a predictor of 24-hour urinary iodine excretion for estimating population iodine intake. Rev Panam Salud Publica. 2015;38(1):73-81.
➕ Links & Resources
More About the Thyroid:
- What Does Your Thyroid Do?
- What are Optimal Thyroid Levels?
- Do You Need A Thyroid Detox?
- What Does Pain in the Thyroid Mean?
- What Causes Thyroiditis?
- Low Iodine Diet: Improve Hypothyroidism
- When Should I Worry About My Thyroid Nodule?
- What Causes Thyroid Nodules to Grow?
- How Long Can You Go Without Thyroid Medication?
- The Gut-Thyroid Connection
- What are Healthy Levels for Thyroid Antibodies?
- Find Your Ideal Thyroid Medication in 4 Simple Steps

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!