What Causes Thyroiditis?
Everything You Need to Know About Thyroid Inflammation
- Types of Thyroiditis|
- Hashimoto’s Thyroiditis|
- Silent Thyroiditis|
- Subacute Thyroiditis|
- Postpartum Thyroiditis|
- Radiation-Induced Thyroiditis|
- Drug-Induced Thyroiditis|
- Suppurative Thyroiditis|
- Testing for Thyroiditis|
- Treating Thyroiditis|
- The most common cause of thyroid inflammation is autoimmunity.
- Poor gut health may play a significant role in autoimmune thyroid disease.
- Short-term thyroid inflammation may be caused by recent childbirth, drug reactions, radiation treatments, or viral infections.
Thyroiditis is an inflammation of the thyroid gland, which can affect thyroid function.
Thyroiditis may cause the thyroid gland to overproduce or underproduce thyroid hormone. Some types of thyroiditis can cause pain in the thyroid. However, the more common types of thyroiditis are painless.
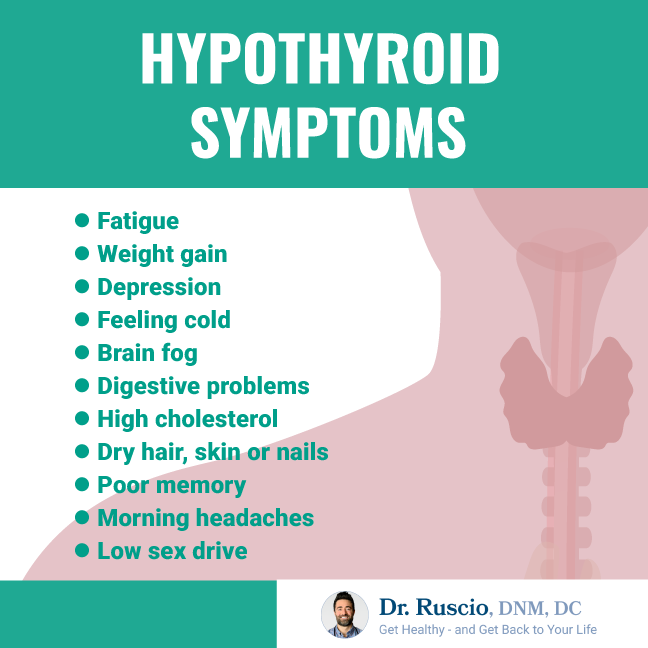
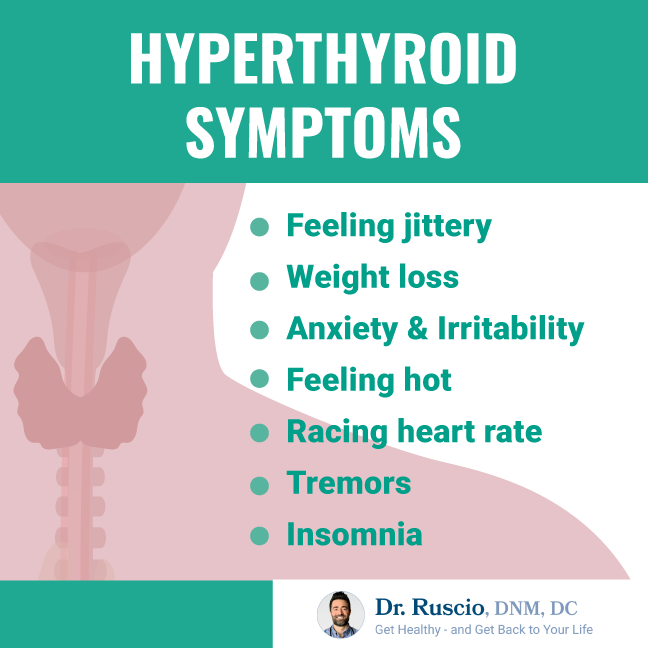
Typically, the first signs of thyroiditis are hypothyroid or hyperthyroid symptoms. Some patients may initially have hyperthyroidism and then develop hypothyroidism. In this article, we’ll cover all you need to know about thyroiditis, including its different types and how to test and treat it.
Types of Thyroiditis
First, let’s review what thyroiditis is. To do this, we need to discuss inflammation. Inflammation is your immune system’s natural response to injury or infection.
Think of a red, inflamed area that you’ve seen on your skin. It might be caused by a cut that’s not healing well, a sliver, or even a burn. This same inflammation process can happen to your thyroid gland.
Many different things can injure or infect your thyroid gland, causing thyroiditis. We’ll take each in turn.
Hashimoto’s Thyroiditis

By far, the most common cause of thyroiditis [1] is an autoimmune thyroid disease called Hashimoto’s thyroiditis or Hashimoto’s disease.
Autoimmune thyroiditis is 10 times more common in women than men. [2]
With Hashimoto’s thyroiditis, your own immune system attacks your thyroid gland in a case of mistaken identity, causing inflammation. This attack leads to chronic thyroiditis. Just like a badly infected wound, chronic inflammation of the thyroid gland can result in scar tissue and permanent damage to thyroid cells. Once damaged, the thyroid gland is less able to produce the thyroid hormones your body needs for metabolism. This damage is the most common cause of hypothyroidism.
Some patients with Hashimoto’s thyroiditis may not have obvious symptoms. Other patients struggle with symptoms of hypothyroidism, including fatigue, weight gain, constipation, brain fog, hoarseness, and hair loss. These symptoms may be a result of low thyroid hormone levels. They can also be caused by gut imbalances which are commonly found in patients with autoimmune thyroiditis.
Hashimoto’s patients may also have thyroid nodules. These are usually small, painless, and benign lumps in the thyroid gland. Generally, thyroid nodules aren’t a cause for worry, but you should see a doctor if they are growing or are painful.
Hashimoto’s disease is diagnosed through blood tests for thyroid antibodies.
While Hashimoto’s disease is typically considered a lifetime autoimmune disease, there’s good news. Research shows a correlation between autoimmune thyroid conditions and poor gut health. [3, 4, 5, 6, 7] This gives us a thyroiditis treatment avenue that goes beyond levothyroxine (e.g. Synthroid) or thyroid hormone replacement.
It’s possible to reduce or even eliminate your symptoms, dampen the autoimmune process, and feel good with Hashimoto’s disease with better gut health.
Silent Thyroiditis
Silent thyroiditis is a type of painless thyroiditis that is also caused by an autoimmune response. Silent thyroiditis is much less likely to become a chronic condition than Hashimoto’s disease.
Patients may show symptoms of hypothyroidism, hyperthyroidism, or hyperthyroidism followed by hypothyroidism. Symptoms usually resolve on their own in 6-18 months, but, in a small number of cases, patients will become permanently hypothyroid.
Silent thyroiditis is much less common than Hashimoto’s thyroiditis.
Like other types of autoimmune thyroiditis, patients with silent thyroiditis may have underlying gut health issues. Patients may benefit from dietary and lifestyle changes and treatments that improve gut health.
Subacute Thyroiditis (De Quervain’s Thyroiditis)
Subacute thyroiditis is caused by a viral infection (like the mumps or the flu) and can cause thyroid pain. It is also known as de Quervain’s thyroiditis or, sometimes, subacute granulomatous thyroiditis.
Patients with subacute thyroiditis experience rapid and painful inflammation of the thyroid gland and may feel ill and have a fever. Subacute thyroiditis often results in hyperthyroid symptoms such as rapid heart rate, palpitations, and weight loss.
In most cases, subacute thyroiditis is temporary and will resolve on its own. The most common treatments are aspirin to help reduce inflammation and bed rest.
Up to 11% of patients may develop a permanent thyroid disorder and become hypothyroid. [8]
Postpartum Thyroiditis
Although not common, some women develop thyroiditis within a year of childbirth.
Patients with postpartum thyroiditis may start off with hyperthyroidism that eventually transitions into an underactive thyroid (hypothyroid). Other patients may only have symptoms of hypothyroidism.
One theory is that patients who suffer from postpartum thyroiditis have underlying, subclinical autoimmune thyroiditis. [9]This condition flares after childbirth due to fluctuations in hormones and immune function.
Postpartum thyroiditis resolves on its own for most patients, though up to 25% of them will become permanently hypothyroid. [10] Also, women who have had postpartum thyroiditis are likely to have a recurrence if they become pregnant again.
Radiation-Induced Thyroiditis
High-dose radiation treatments for cancers or radioactive iodine therapy for Graves’ disease can cause inflammation of the thyroid gland for some patients. Symptoms usually appear 5-10 days after radiation treatment and may include thyroid pain, tenderness, and hyperthyroid symptoms.
Radiation-induced thyroiditis usually resolves on its own in about a month. In the meantime, anti-inflammatory medications may relieve symptoms.
Drug-Induced Thyroiditis
Certain drugs can cause inflammation of the thyroid, including:
- Interferons (used to treat cancer)
- Amiodarone (for heart-rhythm problems)
- Lithium (taken for bipolar disorder)
This side effect only occurs in a small fraction of patients using these drugs. Drug-induced thyroiditis may cause pain in the thyroid and can lead to both hyperthyroid and hypothyroid symptoms.
Swelling of the thyroid gland will resolve on its own once you stop taking the drugs. If you suspect drug-induced thyroiditis, talk to your doctor before discontinuing any medications.
Suppurative Thyroiditis
Suppurative thyroiditis is a bacterial infection of the thyroid gland which becomes abscessed. It is a serious condition and potentially fatal if not treated with antibiotics. Luckily this is a very rare condition. [11]
Patients with this bacterial infection usually have fever, thyroid pain, and difficulty swallowing.
Thyroid cancer, large goiters, and Hashimoto’s thyroiditis may be risk factors for suppurative thyroiditis. It is also possible for the thyroid gland to be infected as a result of a fine-needle aspiration biopsy thyroid test.

Testing for Thyroiditis
Your physician may order one or more of the following tests to diagnose thyroiditis:
- Thyroid function tests are standard blood tests that measure thyroid hormone levels. Thyroid function tests can determine if you are hypothyroid or hyperthyroid. Thyroid tests check your levels of:
- T4 and T3 hormone: These are thyroid hormones produced by your thyroid gland. They play an important role in regulating your body’s metabolism, heart rate, and body temperature. Too much thyroid hormone can cause symptoms of hyperthyroidism. Too little thyroid hormone can cause symptoms of hypothyroidism.
- TSH (thyroid-stimulating hormone): A hormone produced in the pituitary gland. TSH signals the thyroid gland to produce T4 and T3. High levels of TSH in the blood are associated with hypothyroidism. In this case, the body is trying to stimulate more thyroid hormone production. Low TSH levels in the blood are associated with hyperthyroidism, as the body tries to reduce thyroid hormone production.
Overdiagnosis of hypothyroid is a significant problem in both conventional and natural medicine. For detailed information about thyroid hormone testing and optimal thyroid levels, check out our blog.
- Thyroid antibody tests are blood tests that detect autoimmune thyroid disease. Elevated levels of anti-thyroid antibodies suggest the presence of an autoimmune thyroiditis.
- Erythrocyte sedimentation rate (ESR) is a blood test that looks for markers of inflammation in the body. ESR testing is used to diagnose subacute thyroiditis.
- Thyroid ultrasound (or sonogram) is used to visualize the anatomy of the thyroid gland. This method can detect thyroid nodules, swelling and changes in thyroid density.
- Radioactive iodine uptake is another test that can detect overactive or underactive thyroid function. Patients are given a very small amount of radioactive iodine, and testing is done over a 24-hour period to see how much of the radioactive iodine is absorbed by the thyroid gland.
Treating Thyroiditis
Short-term, acute inflammation of the thyroid gland usually resolves on its own once the cause of inflammation (for example, medication, radiation, or childbirth) recedes.
Various treatment options are available for thyroiditis. The best option depends on the cause and symptoms:
Standard Treatments
- Painful thyroid inflammation may be treated with non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. NSAIDs can be very helpful for short-term pain management. However, it’s very important to avoid using them for extended periods of time. Research shows that NSAIDs can damage the intestinal walls and lead to leaky gut. [12]
- Prednisone is sometimes recommended for patients with subacute thyroiditis when NSAIDs do not provide adequate pain relief.
- Hypothyroidism may need to be treated with levothyroxine, a synthetic thyroid hormone.
- For hyperthyroidism, beta blockers may be prescribed.
Natural Treatments
- Supplements such as selenium,[13, 14, 15, 16] vitamin D, [17, 18, 19] and for some patients iron [20, 21] and stomach acid, [22, 23] may improve thyroid markers, including the antibodies that may cause thyroiditis.
- Autoimmune thyroiditis can often be managed very successfully by improving gut health.
Bottom Line
There are many possible reasons for inflammation of the thyroid gland, but the most common reason by far is an autoimmune thyroid disorder. Thyroiditis can have far-reaching effects on your overall health and well-being.
If you suspect a thyroid disorder, it’s important to get a proper diagnosis and address the root cause of your thyroid symptoms.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
-
Sweeney LB, Stewart C, Gaitonde DY. Thyroiditis: an integrated approach. Am Fam Physician. 2014;90(6):389-396.
-
Vanderpump MP. The epidemiology of thyroid disease. Br Med Bull. 2011;99:39-51. doi:10.1093/bmb/ldr030
-
Choi YM, Kim TY, Kim EY, et al. Association between thyroid autoimmunity and Helicobacter pylori infection. Korean J Intern Med. 2017;32(2):309-313. doi:10.3904/kjim.2014.369
-
Shi WJ, Liu W, Zhou XY, Ye F, Zhang GX. Associations of Helicobacter pylori infection and cytotoxin-associated gene A status with autoimmune thyroid diseases: a meta-analysis. Thyroid. 2013;23(10):1294-1300. doi:10.1089/thy.2012.0630
-
Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017;23(5):842-852. doi:10.3748/wjg.v23.i5.842
- Bertalot G, Montresor G, Tampieri M, et al. Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection. Clin Endocrinol (Oxf). 2004;61(5):650-652. doi:10.1111/j.1365-2265.2004.02137.x
-
El-Zawawy HT, Farag HF, Tolba MM, Abdalsamea HA. Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17. Ther Adv Endocrinol Metab. 2020;11:2042018820907013. Published 2020 Feb 21. doi:10.1177/2042018820907013
-
Sweeney LB, Stewart C, Gaitonde DY. Thyroiditis: an integrated approach. Am Fam Physician. 2014;90(6):389-396.
-
Keely EJ. Postpartum thyroiditis: an autoimmune thyroid disorder which predicts future thyroid health. Obstet Med. 2011;4(1):7-11. doi:10.1258/om.2010.100041
-
Sweeney LB, Stewart C, Gaitonde DY. Thyroiditis: an integrated approach. Am Fam Physician. 2014;90(6):389-396.
- Falhammar, H., Wallin, G. & Calissendorff, J. Acute suppurative thyroiditis with thyroid abscess in adults: clinical presentation, treatment and outcomes. BMC Endocr Disord 19, 130 (2019). https://doi.org/10.1186/s12902-019-0458-0
-
Bjarnason I, Takeuchi K. Intestinal permeability in the pathogenesis of NSAID-induced enteropathy. J Gastroenterol. 2009;44 Suppl 19:23-29. doi:10.1007/s00535-008-2266-6
-
Wichman J, Winther KH, Bonnema SJ, Hegedüs L. Selenium Supplementation Significantly Reduces Thyroid Autoantibody Levels in Patients with Chronic Autoimmune Thyroiditis: A Systematic Review and Meta-Analysis. Thyroid. 2016;26(12):1681-1692. doi:10.1089/thy.2016.0256
-
Gärtner R, Gasnier BC. Selenium in the treatment of autoimmune thyroiditis. Biofactors. 2003;19(3-4):165-170. doi:10.1002/biof.5520190309
-
Gärtner R, Gasnier BC, Dietrich JW, Krebs B, Angstwurm MW. Selenium supplementation in patients with autoimmune thyroiditis decreases thyroid peroxidase antibodies concentrations. J Clin Endocrinol Metab. 2002;87(4):1687-1691. doi:10.1210/jcem.87.4.8421
-
Zheng H, Wei J, Wang L, et al. Effects of Selenium Supplementation on Graves’ Disease: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2018;2018:3763565. Published 2018 Sep 26. doi:10.1155/2018/3763565
-
Bozkurt NC, Karbek B, Ucan B, et al. The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis. Endocr Pract. 2013;19(3):479-484. doi:10.4158/EP12376.OR
-
Bozkurt NC, Karbek B, Ucan B, et al. The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis. Endocr Pract. 2013;19(3):479-484. doi:10.4158/EP12376.OR
-
Wang S, Wu Y, Zuo Z, Zhao Y, Wang K. The effect of vitamin D supplementation on thyroid autoantibody levels in the treatment of autoimmune thyroiditis: a systematic review and a meta-analysis. Endocrine. 2018;59(3):499-505. doi:10.1007/s12020-018-1532-5
-
Rayman MP. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc Nutr Soc. 2019;78(1):34-44. doi:10.1017/S0029665118001192
- Singh V, Sachdeva A, Malik I, Saha Roy P, Madaan H, & Nair R. Association between serum ferritin and thyroid hormone profile in hypothyroidism . Int J Med Sci Public Health. 2015; 4(6): 863-865. doi: 10.5455/ijmsph.2015.24012015174
-
Lahner E, Annibale B. Pernicious anemia: new insights from a gastroenterological point of view. World J Gastroenterol. 2009;15(41):5121-5128. doi:10.3748/wjg.15.5121
-
Sterzl I, Hrdá P, Matucha P, Cerovská J, Zamrazil V. Anti-Helicobacter Pylori, anti-thyroid peroxidase, anti-thyroglobulin and anti-gastric parietal cells antibodies in Czech population. Physiol Res. 2008;57 Suppl 1:S135-S141.
➕ Links & Resources
More on Thyroiditis:
- What Does Your Thyroid Do?
- What are Optimal Thyroid Levels?
- Do You Need a Thyroid Detox?
- What Does Pain in the Thyroid Mean?
- Is a Low-Iodine Diet Good for the Thyroid?
- Thyroid Nodules – When to Worry
- What Causes Thyroid Nodules to Grow
- How Long Can You Go Without Thyroid Medication?
- How Should I Use Thyroid Supplements?
- The Gut-Thyroid Connection
- What are Healthy Levels for Thyroid Antibodies?
- Find Your Ideal Thyroid Medication in 4 Simple Steps

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!