Meditation for IBS: Harnessing the Gut-Mind Connection
Meditation Has Been Proven to Help With Irritable Bowel Syndrome
- About Meditation & Mindfulness|
- The Gut-Mind Connection|
- Meditation and Stress Relief|
- Is Meditation All I Need?|
- Additional Interventions|
- Meditation Combined with Gut Healing|
- Recommended Products|
- Meditation and other practices that work on the gut-mind connection have been shown to be very effective at reducing IBS symptoms, even months after the intervention.
- Meditation works by assisting in regulation of neurotransmitters, decreasing inflammation, improving the gut microbiome and regulating stress.
- For people who have improved gut health but still have IBS symptoms, meditation may be a missing link in healing.
If you have been dealing with irritable bowel syndrome (IBS), adding in meditation can be a helpful, but often overlooked, tool in your treatment toolbox. It accesses the gut-mind connection to help improve symptoms of IBS such as abdominal pain, bloating, constipation, and brain fog. Meditation may also help to improve symptoms of other gastrointestinal conditions, such as inflammatory bowel disease (IBD).

What Is Meditation? What Is Mindfulness?
Meditation, as defined in the dictionary, is the act of focusing the mind, in silence or with chanting, for religious, spiritual, or relaxation purposes.
Meditation has a long tradition in religion that may date back to as early as 5,000 BCE. It was used in ancient Egypt and China and in the faith traditions of Judaism, Hinduism, Jainism, Sikhism, and Buddhism. Meditative practices came to the West in the 1900s, and researchers began studying it for its medical benefits starting in the 1960s [1].
When studying meditation for health purposes, the National Institute of Health National Center for Complementary and Integrative Health explains that the process of meditation generally requires these four components:
- A quiet, distraction-free location
- A comfortable posture, whether sitting, lying down, walking, or otherwise
- Something to focus your attention on, such as a word, phrase, object, or bodily sensations (like inhales and exhales or a guided meditation)
- Openness of mind and attitude to allow distracting thoughts to come and go without judgment
Mindfulness is often discussed along with meditation. Mindfulness is the term for the fourth component of the process of meditation: paying attention to the present moment, without judgment.
This article will share the research on a few different types of mindfulness and meditation interventions that work to support a healthy gut-mind connection.
The Gut-Mind Connection
The gut and mind are connected in many ways. In fact, some of the pharmaceutical drugs that are used to treat irritable bowel syndrome (IBS) symptoms work because of their effects on neurotransmitters, including dopamine and serotonin [2, 3].
There are few mechanisms by which anything that affects the brain affects the gut, and vice versa.
- Neurotransmitters (chemical messengers that transmit signals from the brian to various cells) such as dopamine, serotonin, and norepinephrine are made in the gut and taken to the brain via the vagus nerve. These neurotransmitters affect appetite, regulate pain, affect mood, and regulate the digestive system [4, 5].
- The gut and brain communicate in part via the vagus nerve. The vagus nerve is the 10th and longest cranial (starts in the head) nerve, and it creates a two-way messaging system, which is called the gut-brain axis. This nerve travels from the base of the brain all the way down throughout the digestive tract, which allows the brain and gut to communicate. The vagus nerve releases neurotransmitters that affect both gut and brain function such as mood and digestion. The vagus nerve also controls other body functions such heart rate, breathing, and reflex actions like coughing and sneezing [6].
- Psychological stress typically triggers a fight-or-flight response, which releases hormones that disturb the gut microbiome and increases inflammation [7].
What this really shows us is that anything that causes stress to the mind, such as psychological stress, affects how the gut works. Anything that affects how the gut works affects how the mind works.
A treatment approach that positively affects the gut and the mind, therefore, will likely be especially powerful when it comes to healing.

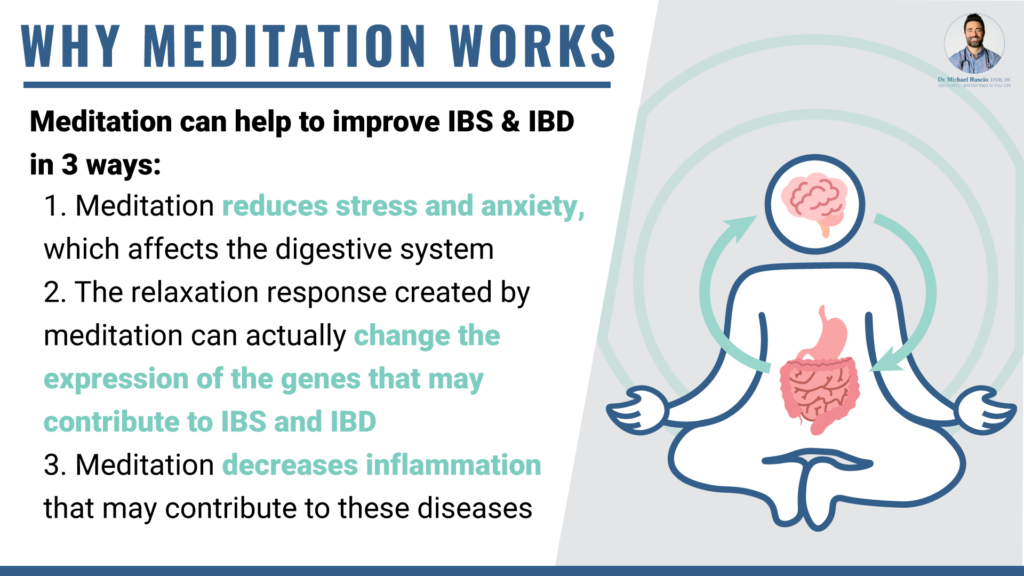
Why Meditation Works
Meditation works to improve IBS and IBD in three ways.
- Meditation reduces stress and anxiety, which affects the digestive system.
- The relaxation response created by meditation can actually change gene expression in the genes that contribute to IBS and IBD.
- Meditation decreases inflammation that may contribute to these diseases.
Let’s look at these three mechanisms a bit closer. What you will notice is that they are all related in the complex but amazing system of the gut-brain connection.
Stress Reduction and the Gut
Managing stress is important for general gut health and proper digestion, and can help with symptom reduction.
Stress changes the microbiome (the balance of bacteria that live in the gut and keep it healthy) and those changes can lead to IBS symptoms [8]. Stress also changes the balance of neurotransmitters that are needed for proper digestion and movement of food through the GI tract.
Reducing stress may help improve this neurotransmitter balance and improve gastrointestinal symptoms. Regulating stress response also helps calm states of chronic inflammation (which we will talk more about below) and decrease leaky gut by maintaining a healthy gut lining [7, 9].
People with chronic illnesses, such as IBS and IBD (irritable bowel disease) including Crohns and ulcerative colitis tend to have higher levels of anxiety and/or depression. In fact, one study found that IBS patients were three times as likely as healthy subjects to have either anxiety or depression [10]. The chronic pain and life disruption that comes with gastrointestinal illness causes a lot of psychological stress, creating a circular system where the stress from the illness increases illness symptoms. Decreasing that stress can help improve overall symptoms.
Meditation Can Change Gene Expression
This research is pretty fascinating and is one of the first looks into the mechanism of action (exactly why in the body) meditation which reduces stress and creates a relaxation response (a state of rest that changes the response to stress) works to improve IBS and IBD.
A 2015 study of a nine-week relaxation response-based mind-body group intervention found that not only were IBS and IBD symptoms improved, but there was also altered gene expression. In particular, the intervention suggested that NF-κB (nuclear factor kappa,) a protein complex that controls DNA transcription, is a target molecule in both IBS and IBD. The study noted that the ability of mindfulness practices to help regulate NF-κB may be one of the reasons why meditation helps improve IBS and IBD [11]. The study also found 1,059 other genes in IBD and 119 genes in IBS related to inflammation, stress, or DNA degeneration that can contribute to IBS and IBD.
NF-κB contributes to immunity, inflammation, cancer, and nervous system function, basically helping to improve both the stress response and inflammation that can lead to IBS and IBD [12].
Meditation Can Reduce Inflammation
Inflammation has been found to be a contributing factor to both IBS and IBD [12, 13, 14]. Meditation and mindfulness techniques have been shown to decrease inflammation, even decreasing C-reactive protein (a blood marker for inflammation) in patients with IBD [11, 15].
Stress increases inflammation as well as changes the microbiome in the gut, both of which can lead to symptoms of IBS or IBD [7]. A healthy gut makes short-chain fatty acids that have an anti-inflammatory effect, but during stress the corticotropin-releasing hormone is triggered which disrupts the microbiome leading to an unhealthy gut [7]. Since meditation decreases inflammation it also improves the gut microbiome. A poor gut microbiome can contribute to leaky gut, which also increases inflammation [14].
Meditation Interventions for Irritable Bowel Syndrome and Inflammatory Bowel Disease
There are many different forms of meditation/mindfulness-based interventions with research-backed benefits for IBS, IBD, and other gastrointestinal issues. Let’s look at some of the methods and their effectiveness.
| Intervention | Description | Results |
| Mindfulness-Based Meditation | Focusing attention on the present moment without judgment. This can be done by using many different forms of meditation. | • Chronic and acute pain decreases with mindfulness practices [16, 17]. • Meditation may reduce IBS symptoms, ulcerative colitis flare-ups (IBD), anxiety, depression, and insomnia. |
| Gut-directed Hypnotherapy | Typically a seven-session protocol where a therapist employs relaxation techniques and imagery to induce a hypnotic state, a state of deep relaxation. The therapist then uses suggestions focused on calming the digestive tract, possibly improving any miscommunication between the brain and the gut [9, 18]. | • This form of hypnotherapy can help relieve abdominal pain, bloating, and bowel dysfunction, and improve quality of life for IBS sufferers [9]. • The American Gastroenterological Association recommends gut- directed hypnotherapy as an intervention for moderate to severe IBS [9]. • Around 35% of IBS patients doing individual or group hypnotherapy had adequate IBS symptom relief at three months [19]. |
| Cognitive Behavioral Therapy (CBT) | CBT helps patients assess unhelpful thought patterns and create more helpful emotional responses, thus decreasing psychological stress [20]. It is used for treating many different mental health issues but is also used in IBS and IBD… For example, in the case of IBS, a patient who feels abdominal pain may expect the pain will always lead to a bowel accident. This creates anxiety and fear every time they have any stomach distress. With CBT, the patient learns to break that thought pattern and remember that stomach pain often does not result in bowel accidents, thus not allowing a few bad incidents to create anxiety every time pain is felt [9]. | • CBT is one of the most effective IBS treatments, decreasing risk of becoming symptomatic by around 38% [21]. • CBT is more effective at reducing symptoms than just general relaxation therapies [22]. |
| Mindfulness-based stress reduction (MBSR) | An eight-week class that teaches people to cultivate mindfulness by focusing on their bodily sensations, thoughts, and emotions with curiosity and compassion rather than judgment [23] | • MBSR may improve the GI symptoms associated with IBS. • Feelings of anxiety around GI issues are decreased with MBSR because it cultivates a non-reactive response to GI distress [23]. • MBSR reduces illness-related anxiety, improving the gut-mind connection [24]. • Significant improvements in stress, depression, and quality of life in IBD patients were seen with the use of MBSR [25]. • MBSR improved inflammatory markers in IBS and IBD, which did relate to less symptoms in IBS, but was inconclusive in IBD symptoms [11, 15, 26]. |
Can You Treat IBS With Meditation Alone?
While there is great evidence supporting meditation and other gut-mind interventions in treatment of IBS, it is not a perfect intervention for digestive health. The way the intervention is administered and underlying health issues matter in the effectiveness of meditation for IBS sufferers.
For example, online CBT was not shown to significantly improve IBS related anxiety [27]. However, as mentioned above, in-person CBT did improve IBS anxiety and symptoms in another study.
As you can tell from all of the contributing factors to IBS and IBD, many factors contribute to these illnesses. While meditation reduces inflammation, if someone is eating a highly inflammatory diet or has extremely poor sleep, their inflammation levels may still be high enough that some symptoms are still present [28].
Additionally, if something like too many bad bugs in the gut microbiome are contributing to IBS or IBD, such as in the case of small intestinal bacterial overgrowth or H. pylori, that may need to be taken care of in order to have meditation be more effective.
For these reasons, most people do best with a plan that includes additional lifestyle interventions to additionally support gut healing, along with meditation techniques.
Additional Interventions

Resolving any additional issues, such as leaky gut, inflammation, or offending gut bugs generally involves a few simple steps that you can take at home: an anti-inflammatory diet and probiotics, plus herbal antimicrobials if they are needed.
Anti-Inflammatory Diet
Reducing systemic inflammation is one of the most important first steps when it comes to improving gastrointestinal issues.
To decrease inflammation, I generally suggest starting with a Paleo diet, which removes a number of common foods that create an immune response [29]. The Paleo diet also improves the gut microbiome, further reducing inflammation [30].
If the Paleo diet does not resolve symptoms enough, there is good evidence to try a low-FODMAP diet, particularly for IBS. A low-FODMAP diet restricts bacteria-feeding carbs, or, fermentable oligo-, di-, mono-saccharides and polyols such as wheat, onion, legumes, dairy, and fructose. These can ferment in the gut and cause gut symptoms [31, 32].
Probiotics
As we mentioned earlier in the article, the balance of gut bacteria is extremely important in supporting good gut functioning and relieving gut symptoms. Good gut bacteria also supports a healthy gut-mind connection, which improves effectiveness of meditation-based interventions. One way to support a good balance of gut bacteria is to use probiotics.
Specifically, in IBS, probiotics have been shown in double-blind studies to improve symptoms such as gas, bloating, diarrhea, constipation, and abdominal pain [33, 34, 35].
- Probiotics have been shown to be an effective treatment for SIBO [36].
- Probiotics improve constipation and bloating associated with IBS [35, 37].
You can learn more about adding probiotics to your regimen with my probiotics starter guide.
Herbal Antimicrobials
If trying an anti-inflammatory diet and probiotics do not resolve your symptoms, you may want to try herbal antimicrobials. These can remove any gut microbes that are causing stomach issues, such as the microbes in SIBO [38, 39, 40].

Meditation for IBS and Gut Healing
Creating your own meditation practice or working with a practitioner to try a structured mindfulness-based intervention such as mindfulness-based cognitive therapy (MBCT,) CBT, or gut-directed hypnotherapy may be a missing piece to your IBS treatment plan.
Just like how meditation may not be all that is needed, if you have healed your gut but keep experiencing the deep psychological stress related to having had a chronic illness, it may be damaging your gut. If you are struggling with parsing out exactly what issues you need to work on to heal your gut and improve your quality of life, please reach out to our clinic. We would be honored to help you on your path to wellness.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.



Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!