H pylori Probiotics, and Treatment Success
How to Use Probiotics as Allies During H. Pylori Treatment
- What Is H. Pylori?|
- Symptoms|
- Probiotics & H. Pylori|
- Lacto-Bifido Probiotics|
- Saccharomyces boulardii|
- Soil-Based Probiotics|
- How To Use Probiotics|
- Probiotics With Antibiotics|
- The Bottom Line|
Download this Episode (right click link and ‘Save As’)
If you’re experiencing the classic H. pylori symptoms of pain, burning in your stomach, or ulcers, or you’ve tried to treat H. pylori but didn’t succeed, you’ll be happy to know that probiotics can be a simple, effective helper.
It might not seem like ordinary probiotics could make much of a difference against the pathogenic bacteria Helicobacter pylori. But the surprising news is that various probiotic strains appear to prevent H. pylori infection 1, significantly improve the success of H. pylori treatment 2, and even sometimes completely treat it (in a minority of cases) 3.
Let’s explore what research says about H. pylori, the effects of probiotics on H. pylori, and how probiotics best fit into H. pylori treatment.
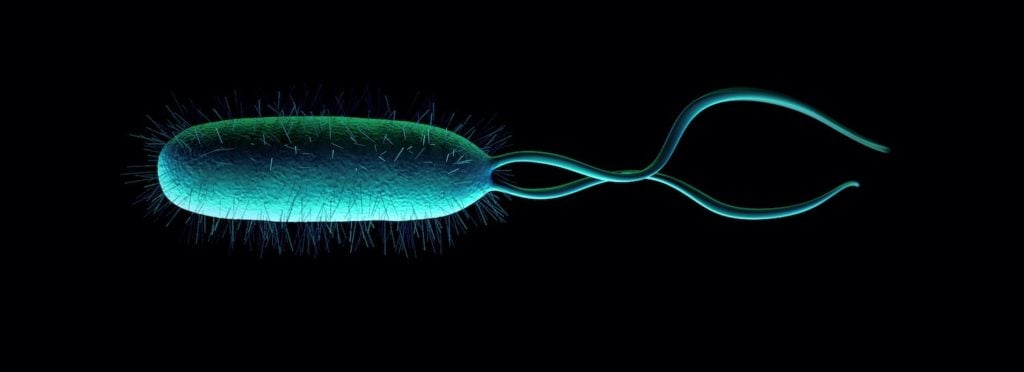
What is Helicobacter Pylori?
Helicobacter pylori — known as H. pylori for short — is a spiral-tailed pathogenic bacteria that primarily resides in the stomach, though it can also live anywhere in the gastrointestinal tract 4.
H. pylori was discovered by two Australian researchers, Barry Marshall and Robin Warren, one of whom proved H. pylori caused gastritis by infecting himself with the bacteria 5. They were awarded the Nobel Prize in 2005 for this important discovery for gastroenterology.
It’s estimated that more than half of the world’s population has H. pylori present in their gut 6 7. Only 10-20% of people infected will develop symptoms like peptic ulcers, and a very small percentage will develop gastric cancer 8.
H. pylori burrows into and inflames the stomach lining, which affects the acid-producing parietal cells of the stomach 9. A chronic decrease in stomach acid due to H. pylori infection is a risk factor for many conditions and side effects downstream. Low stomach acid can lead to vitamin B12 and iron deficiency, poor protein digestion, low bile and enzyme secretion, and slow gut motility 10 11.
Eradication of H. pylori leads to the resolution of symptoms in people with peptic ulcer disease and prevents recurrence 12 13 14.
Symptoms of H. Pylori Infection
H. pylori activity causes stomach symptoms, including:
- Bloating, gas, and abdominal pain
- Burning stomach
- Stomach pain on an empty stomach
- Loss of appetite
- Nausea
- Frequent burping
- Heartburn, reflux, or GERD
- Peptic ulcers or duodenal ulcers
- Gastritis (inflammation of the stomach lining)
H. pylori colonizes the gastric epithelial cells (stomach lining cells). As the bacteria break down proteins in the stomach wall, it produces the enzyme urease. High levels of urease increase ammonia in the stomach, which leads to gastric inflammation and damages the gastric mucosa 15.
Eradication of Helicobacter pylori usually resolves these symptoms.
Probiotics are Allies for H. Pylori Treatment
Probiotic bacteria have been shown in multiple meta-analyses and systematic reviews (the highest quality data) to improve the outcome of standard H. pylori treatment (antibiotics).
Specifically, probiotic supplementation has been shown to:
- Reduce side effects of standard treatment (antibiotics) and increase the likelihood of patients finishing their antibiotic therapy 16.
- Improve treatment success by 10-15% compared to antibiotic therapy without probiotics 17 18.
- Suppress H. pylori in the stomach and improve dyspeptic symptoms by correcting the stomach microbiota 19.
The long-term use of probiotics also appears to reduce the risk of developing disorders associated with the gastric inflammation caused by H. pylori infection, such as ulcers, gastritis, and cancer 20.
Some data doesn’t agree. One meta-analysis concluded that probiotics didn’t improve Helicobacter pylori eradication rates, but did find that side effects from standard antibiotic treatment, such as diarrhea and nausea, were reduced 21. A small clinical study came to similar conclusions 22.
However, a wide range of meta-analyses, systematic reviews, and clinical trials conclude that probiotics can make a significant difference in H. pylori treatment. Given these data, the role of probiotics should be prominent during treatment.
Best Probiotics for H. Pylori Treatment
Scientists have studied many different types of probiotics for their effect on H. pylori eradication rates. Some studies have tested single strains, but many different strains and combinations have been shown to be effective at improving treatment success. Let’s summarize what we know about the best probiotics for H. pylori treatment.
Lactobacillus and Bifidobacteria Probiotics and H. Pylori
Lactobacillus and Bifidobacteria probiotics have been shown in multiple meta-analyses and systematic reviews to support successful H. pylori treatment (with antibiotics), though this may be partly because these are the most commonly studied probiotics.
Notable research about Lactobacillus (lactic acid bacteria) and Bifidobacteria probiotics (such as Lactobacillus acidophilus and Lactobacillus reuteri) for H. pylori found:
- Lactobacillus casei was identified as the best for improving H. pylori eradication rates of standard treatment 23.
- Probiotic combinations that include Lactobacillus casei, L. plantarum, L. reuteri, L. salivarius, L. sporogenes, L. acidophilus, L. rhamnosus, Bifidobacterium infantis, and B. longum can help with antibiotic side effects such as diarrhea, constipation, nausea, vomiting, and taste disturbance 24.
- A broad range of Lactobacillus probiotics increased the success of H. pylori treatment and reduced side effects from the antibiotics 25.
- A randomized controlled trial led by H. pylori researcher Cruchet showed that Lactobacillus johnsonii La1 reduced H. pylori infection in children compared to controls 26.
- Lactobacillus gasseri strain LG21 has been shown to increase the eradication of H. pylori and to reduce side effects of the antibiotics 27.
- A promising pilot study in mice showed that Lactobacillus gasseri OLL2716 reduced inflammatory cytokines and inhibited growth in antibiotic-resistant H. pylori 28. More research will have to be done to confirm the clinical utility of this finding.
Saccharomyces Boulardii Probiotics and H. Pylori
Saccharomyces boulardii is a beneficial yeast that has probiotic properties. It has been widely studied and has been shown to also be supportive for eradicating H. pylori.
In a systematic review, Saccharomyces boulardii alone was shown to eliminate H. pylori infection in 12% of cases 29, though more research is needed to confirm this result.
Saccharomyces boulardii has also been shown in at least two meta-analyses to increase the success of antibiotic triple therapy and reduce side effects 30 31.
Additionally, it was shown in a systematic review to specifically improve bloating during H. pylori treatment 32.
Soil-Based (Bacillus) Probiotics
There is a lot less research on soil-based probiotics compared to the other two types, but limited research shows that soil-based probiotics can help with standard (antibiotic) H. pylori treatment.
A systematic review concluded that a multi-strain probiotic including soil-based bacteria such as Bacillus mesentericus and Streptococcus faecalis improved loss of appetite during antibiotic treatment 33.
A review of the evidence for Bacillus probiotics in H. pylori treatment concluded that they were particularly effective at reducing antibiotic-associated diarrhea 34. This review suggested that the likely mechanism is due to their ability to inhibit pathogens and modulate the body’s immune response.
With all these data that suggest probiotics support H. pylori treatment, let’s explore how to best use them.
H. Pylori Testing and Treatment
If you have symptoms associated with H. pylori, like peptic or duodenal ulcers, or persistent and chronic heartburn or burning in your stomach, being tested for H. pylori may be a good idea.
There are four ways to test for H. pylori infection.
A stomach biopsy during endoscopy is one option but is quite invasive. Results may vary depending on the sampling method, how widespread the infection is, and how the sample is tested after collection 35. For this reason, other testing methods may yield better results, and will certainly be less expensive and invasive.
The Urea Breath Test (UBT) looks for the urease-virulence factor in your breath after ingesting a challenge solution. Any LabCorp or Quest laboratory can run a Urea Breath Test (UBT) for H. pylori.
An H. pylori blood test looks for antibodies to H. pylori. A positive result indicates present or past infection. This test is the least reliable for diagnosing H. pylori 36.
Stool testing screens for H. pylori. Some labs Use PCR-DNA tests to screen for H. pylori DNA in your stool sample. The test also looks for how virulent the H. pylori strains you have are, which can provide some clues as to how damaging the infection is.
Speak with your doctor for advice about testing for H. pylori.
Should You Treat a Positive H. Pylori Test?
H. pylori has definitely been associated with stomach and duodenal ulcers and gastritis, but there is some debate about whether H. pylori is a commensal (normal) bacteria in the gut or an infectious bacteria that needs to be removed.
Because H. pylori is common among the population, having it doesn’t necessarily require action. Probably the best measure of whether or not you should treat H. pylori infection is whether or not you have clear symptoms of H. pylori, like burning in the stomach, peptic or duodenal ulcers, or chronic heartburn and reflux.
If you are positive for H. pylori but do not have symptoms of the infection, treatment is likely not necessary. If you do have symptoms, then pursuing treatment is likely a good idea.
Treating H. Pylori with Probiotics Alone
If you have tested positive for H. pylori but don’t have common H. pylori symptoms, you may simply benefit from using probiotics to balance your microbiota.
A systematic review did find that a small percentage of H. pylori infections can be eradicated with probiotics alone [37]. So, if you have tested positive for H. pylori and you DO have common H. pylori symptoms, such as gastritis, ulcers, stomach pain, or bloating, you may also choose to try a trial of probiotics alone before treating with more intensive therapy.
If your symptoms or H. pylori test don’t resolve with probiotics alone, then you can consider escalating your treatment to include probiotics plus antimicrobial therapy. Be sure to discuss your treatment plans with your doctor.
Standard H. Pylori Treatment
The standard, first-line antibiotic treatment of Helicobacter pylori infection, called “triple therapy”, is 14 days of:
- A proton pump inhibitor (PPI) such as omeprazole, for its inhibitory effect on stomach acid, to allow healing of the stomach lining.
- Two antibiotics together, such as amoxicillin, metronidazole, or clarithromycin
However, H. pylori eradication rates with this regimen are variable, depending on the antibiotic resistance of the H. pylori strains 38. New antibiotic therapy strategies have recently been designed, including sequential therapy 39, where a series of antibiotics are given over the treatment course, and quadruple therapy, where a PPI with multiple antibiotics are given along with bismuth 40.
Among functional medicine and naturopathic doctors, a standard treatment in clinical practice may include herbal antibiotics and probiotics as an anti-H. pylori approach.
No matter which treatment course your doctor prescribes, a lot of patients experience adverse events and side effects on antibiotics or herbal antimicrobials. This is where probiotics really shine.
Probiotics with Antibiotic H. Pylori Treatment
Blending probiotics with the standard Helicobacter pylori eradication therapy increases the rate of treatment success and decreases side effects, such as antibiotic-associated diarrhea, nausea, and bloating 41.
Including probiotics during your anti-Helicobacter pylori treatment is highly likely to minimize these side effects, and increase your likelihood of success.
Research suggests using a diverse range of probiotics together provides better results than a single strain or variety 42 43, and the research on H. pylori supports this 44 45. A simple protocol that includes one quality probiotic from each of the three main categories of probiotics simultaneously— Lactobacillus-Bifidobacteria blends, Saccharomyces boulardii, and a soil-based probiotic — is best. (For more on how to use probiotics properly, see our Probiotics Starter Guide.)
The Bottom Line
Though eradication of H. pylori infection can be challenging due to antibiotic resistance and side effects, probiotics are a wonderful ally. Probiotics have been shown to increase eradication of H. pylori, reduce unpleasant side effects such as nausea, diarrhea, and bloating. Give probiotic therapy a trial before moving on to more conventional treatment, and then include probiotics as part of your H. pylori treatment plan to ensure success.
For personalized help with your digestive health, schedule an appointment with the Ruscio Institute for Functional Medicine.
Sponsored Resources
Hey everyone. I’d like to thank Athletic Greens for making this podcast possible. And if you’re like me, you may sometimes struggle with getting in enough nutrient dense foods. One thing that I’ve really appreciated about Athletic Greens’ AG1 is not only are they the best tasting one that I’ve had to date. They also help ensure that I’m getting adequate nutrition and really hitting the mark regarding nutrient density. And I’ve been using them every morning, pretty much every morning, as part of my morning shake.
Now, one scoop of AG1 contains 75 vitamins minerals and whole foods sourced ingredients, including a multivitamin, a multimineral, a probiotic, and a green super food blend all in one serving.
The other thing I really like about the company is Athletic Greens continues to improve this one holistic formula based upon the latest research. And they’ve produced 53 improvements in their formula over the past decade, which is pretty remarkable and a hat tip to them for that commitment. So I highly recommend Athletic Greens as part of your daily routine. And right now, if you visit athleticgreens.com/Ruscio, you can get a free one year supply of vitamin D and five free Athletic Greens or AG1 travel packs. Again, visit athleticgreens.com/Ruscio to really cover your bases for a well-rounded immune support vis-à-vis AG1, and that one year supply of vitamin D.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.



Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!