Understanding the Foods That Cause Eczema: Your Guide
How Food Intolerances and the Gut Influence Your Skin Health
- Eczema Overview|
- Foods that Cause Eczema|
- Is Eczema an Autoimmune Condition?|
- Treatment|
- A Gut-Focused Approach|
- Recommended Products|
Eczema has become increasingly common over the last few decades. Worldwide, up to 20% of children and 3% of adults are estimated to have eczema, with rates continuing to rise [1].
Specific causes of eczema are not fully understood or agreed upon. Like most chronic conditions, there are likely a number of factors involved in the development and severity of eczema.
Food intolerances or sensitivities and underlying gut issues may be among the factors contributing to the rise in eczema and other chronic, inflammatory skin conditions [2, 3, 4, 5, 6, 7, 8].
In this article, we’ll explore some of the foods that may lead to or trigger eczema, including gluten, high histamine foods, and dairy products. We’ll also look at emerging evidence that suggests eczema may be an autoimmune condition. Finally, we’ll discuss how dietary adjustments and other gut-oriented approaches may help you resolve eczema for good.

Eczema Overview
The most common type of eczema, atopic dermatitis, is a chronic condition characterized by skin inflammation and itchiness.
Symptoms of eczema may include:
- Persistent itchy skin
- Redness or rashes
- Sensitive, inflamed skin
- Small, raised bumps or hives
- Itchy blisters on the feet and hands (as in dyshidrotic eczema)
Conventional treatment for eczema is generally limited to topical steroid creams and ointments. In more severe cases, systemic oral medications like Prednisone may be recommended.
At best, these treatments may provide temporary relief of symptoms, and at worst, they may offer no help at all. Prednisone has serious, known side effects. In any event, these treatments require ongoing use and fail to address the underlying cause of skin inflammation.
Foods That Cause Eczema
A systematic review of 66 studies show a strong link between eczema, food sensitivities, and food allergies [2].
Certain foods have been shown to trigger both immediate reactions and eczema flares that occur up to two days after consumption [3].
If you have eczema, you may want to explore possible food triggers. A few common food sensitivities, like gluten, dairy, and histamine, have been linked to eczema.
Gluten

Gluten, a protein found in grains including wheat, barley, and rye, has been shown to trigger skin reactions and conditions in some patients [9, 10].
- Individuals with celiac disease are more likely to have eczema than those without [11]. This may lend support to an emerging autoimmunity theory of eczema, as celiac disease is also an autoimmune condition.
- Wheat allergies have been linked to eczema and found to trigger symptoms [9].
- One study found that more than 30% of eczema patients had antibodies that reacted with gliadin (a component of gluten), compared to 6.5% of healthy individuals.
- The researchers suggest that gluten may be a trigger for eczema even among those who don’t have celiac disease or a wheat allergy (i.e., non-celiac gluten sensitivity).
- A survey of patient-reported outcomes found that more than half of those who removed white flour and/or followed gluten-free diets showed improvements in eczema symptoms [12].
Histamine
Histamine is a chemical compound your body releases as part of a healthy immune system response. It is also found in certain foods.
Research suggests that excess histamine contributes to eczema in some patients [13, 14]. Histamine is also involved in asthma and allergic reactions, both of which are common alongside eczema [15, 16, 17].
- A small study of 36 patients saw a significant improvement of eczema symptoms in a third of patients after following a low histamine diet for just one week [13]. After the dietary trial, provocation with histamine aggravated eczema in a subgroup of patients.
- A study of 360 individuals found that markers of high histamine levels were significantly more common among those with eczema than among those without [14]. A low histamine diet was shown to reduce the severity of histamine intolerance symptoms, including eczema.
If you have already tried a standard anti-inflammatory or elimination diet without much improvement in eczema symptoms, a low histamine diet may be worth a try.
Foods to avoid on a low histamine diet include:
- Fermented foods including yogurt, kimchi, and sauerkraut
- Aged or cured meats and cheeses
- Certain fruits and vegetables including spinach, tomatoes, and citrus fruits
- Alcohol
Other Eczema-Related Foods
Let’s discuss research behind other foods that may cause eczema.
- Milk and dairy products: A higher percentage of eczema patients have been shown to have antibodies to cow’s milk compared with healthy individuals [18].
- Eggs: Especially in pediatric cases, common allergens like milk and eggs have been shown to trigger eczema flare-ups [19].
- Nightshades: A survey found that 51.4% of patients who eliminated nightshades reported improvements in eczema symptoms [12]. Nightshades are a group of vegetables that include tomatoes, peppers, eggplants, and potatoes.
- Dyes and preservatives: In a study involving 50 adult eczema patients, more than half showed significant symptom improvement when avoiding common irritants including dyes and preservatives [20].
- Fast food: Diets high in fast food have been associated with an increased risk of developing eczema [21].
Is Eczema an Autoimmune Condition?
In autoimmune conditions, the immune system attacks your cells or tissues. Symptoms of autoimmunity vary significantly depending on the area of the body that is being attacked. For example, in the case of Hashimoto’s thyroiditis, the immune system attacks the thyroid.
In autoimmune skin conditions, the immune system attacks your skin cells [22]. Skin conditions that are classified as autoimmune diseases include psoriasis, dermatomyositis, and autoimmune vasculitis.
Emerging research suggests that atopic eczema might fall under this category too [23].
Why does this matter? If we can connect external symptoms like eczema and itchiness to root causes, we can identify true treatment rather than just suppressing symptoms.
Eczema and the Leaky Gut Theory of Autoimmunity
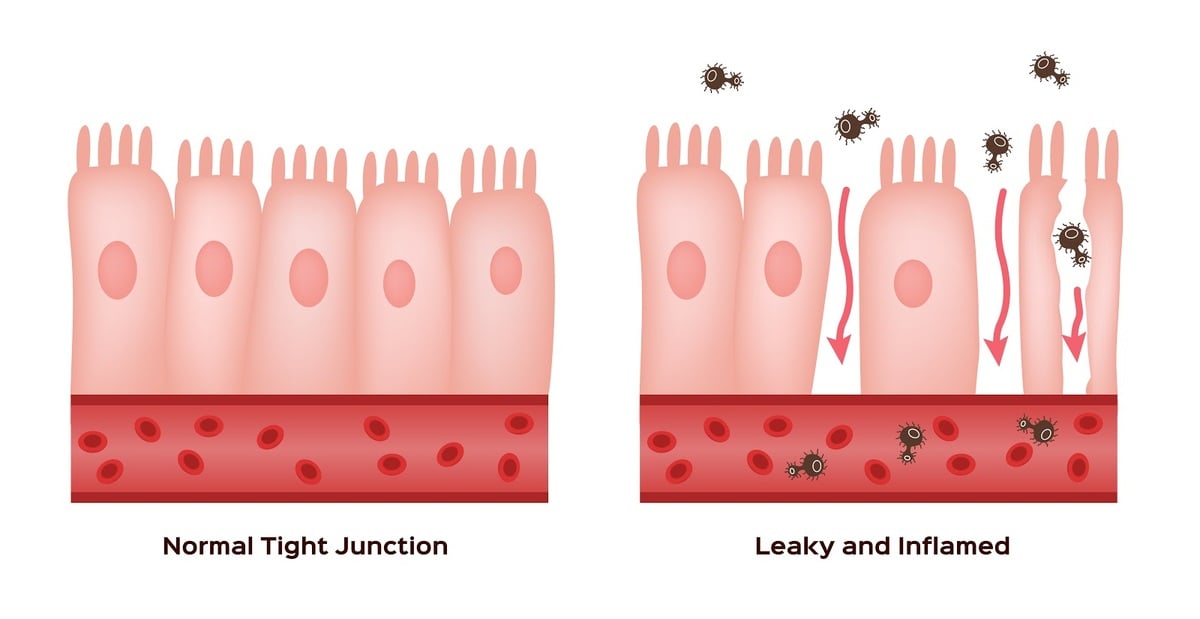
Leaky gut has been linked to the development of eczema [4]. Increased levels of the protein zonulin, often used as an indicator of leaky gut, have also been linked to the presence and severity of eczema [5].
- Leaky gut, which occurs when the intestinal lining becomes damaged and allows bacteria and food particles to leak into the bloodstream, may also connect to autoimmunity and food intolerances [24, 25].
- When the immune system encounters misplaced food particles, it may respond to them as though they are threats.
- This hyperactivity can then contribute to the immune system attacking your own cells.
Studies have shown that healing the gut can help treat some autoimmune conditions, including Hashimoto’s thyroiditis and inflammatory bowel disease (IBD) [26, 27, 28]. This may be relevant for eczema treatment, given that some research now suggests that it is an autoimmune condition as well [23].
Eczema Treatment
Identifying the particular foods that trigger your inflammatory reactions can help to resolve eczema. This can often be done by following an elimination diet.
In addition to dietary changes, working to heal underlying gut issues may be necessary.
Elimination Diets for Eczema
There are large gaps in research when it comes to the use of standard elimination diets for eczema.
An analysis of 43 research papers found mixed results regarding elimination diets specifically focused on eggs and cow’s milk for eczema [29]. Most of these studies only involved children, so the relevance for adults with eczema is not entirely clear. No high-quality studies looking at more general elimination diets or more restrictive versions were available.
If we get more specific, some studies have shown that eliminating gluten or high histamine foods can improve eczema symptoms in certain groups of people [12, 13, 14].
Future research may help elucidate the role that diet plays in eczema more generally and the efficacy of standard elimination diets.
But, as with most chronic conditions, there is no specific “eczema diet” that will work for everyone. An elimination diet is inherently experimental and is meant to be tailored to each individual’s needs and reactions.
With that in mind, here are a few guidelines for following an elimination diet for eczema:
- A good place to start is to follow an anti-inflammatory diet, such as the Paleo diet, for 2-3 weeks. The Paleo diet eliminates many common eczema triggers and inflammatory foods. It focuses on fresh, whole foods.
- If your symptoms improve after 2-3 weeks, you may start to gradually re-introduce some of the foods you have eliminated. This can help you to identify specific foods that trigger your symptoms, including gluten or dairy products. During the re-introduction stage, it’s best to continue to avoid processed foods, fast food, and sugar, which are invariably inflammatory.
- If your symptoms do not improve, try another approach like a low histamine diet.
Can Probiotics Help?
Research on the effectiveness of probiotic supplements for eczema is mixed.
Dysbiosis (an imbalance between beneficial and harmful bacteria) in both the gut and skin microbiomes has been linked to skin conditions including eczema [6, 7, 8].
Treatments like probiotics that target the gut microbiome, therefore, may help in both the prevention and treatment of atopic dermatitis (eczema) and other skin conditions [30]. Additionally, some clinical trials have shown improvements in eczema symptoms with probiotics [31, 4].
Probiotics both during pregnancy and during late infancy have also been shown to help reduce the risk of eczema for young children [32, 33].
However, a meta-analysis of 39 studies concluded that probiotics were not significantly more effective than a placebo in treating eczema symptoms [34].
Other dietary supplements, including omega-3 fatty acids (known for their anti-inflammatory effects), may offer some benefit, although research is still limited [35].
A Gut-Focused Treatment Approach for Eczema
The relationship between the gut and skin, sometimes referred to as the gut-skin axis, is complex.
Leaky gut, intestinal inflammation, and imbalances in the gut microbiome have all been linked to eczema.
Identifying food sensitivities or triggers with the help of an elimination diet can help to reduce inflammation and improve both gut health and eczema symptoms.
Additional treatments that target gut health, like probiotics, may also be useful. For a complete plan to restore your gut health, check out my book, Healthy Gut, Healthy You.
For more personalized guidance on identifying trigger foods, implementing a specialized diet, or improving your gut and skin health, request an appointment at my functional health center.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Nutten S: Atopic Dermatitis: Global Epidemiology and Risk Factors. Ann Nutr Metab 2015;66(suppl 1):8-16. doi: 10.1159/000370220
- Tsakok T, Marrs T, Mohsin M, Baron S, du Toit G, Till S, Flohr C. Does atopic dermatitis cause food allergy? A systematic review. J Allergy Clin Immunol. 2016 Apr;137(4):1071-1078. doi: 10.1016/j.jaci.2015.10.049. Epub 2016 Feb 18. PMID: 26897122.
- Katta R, Schlichte M. Diet and dermatitis: food triggers. J Clin Aesthet Dermatol. 2014 Mar;7(3):30-6. PMID: 24688624; PMCID: PMC3970830.
- Rosenfeldt V, Benfeldt E, Valerius N, Pærregaard A, Michaelsen K. Effect of probiotics on gastrointestinal symptoms and small intestinal permeability in children with atopic dermatitis. The Journal of Pediatrics. 2004. Volume 145, Issue 5, Pages 612-616. DOI: https://doi.org/10.1016/j.jpeds.2004.06.068
- Sheen YH, Jee HM, Kim DH, Ha EK, Jeong IJ, Lee SJ, Baek HS, Lee SW, Lee KJ, Lee KS, Jung YH, Sung M, Kim MA, Han MY. Serum zonulin is associated with presence and severity of atopic dermatitis in children, independent of total IgE and eosinophil. Clin Exp Allergy. 2018 Aug;48(8):1059-1062. doi: 10.1111/cea.13158. Epub 2018 May 21. PMID: 29682826.
- Lee SY, Lee E, Park YM, Hong SJ. Microbiome in the Gut-Skin Axis in Atopic Dermatitis. Allergy Asthma Immunol Res. 2018 Jul;10(4):354-362. doi: 10.4168/aair.2018.10.4.354. PMID: 29949831; PMCID: PMC6021588.
- Fahlén A, Engstrand L, Baker BS, Powles A, Fry L. Comparison of bacterial microbiota in skin biopsies from normal and psoriatic skin. Arch Dermatol Res. 2012 Jan;304(1):15-22. doi: 10.1007/s00403-011-1189-x. Epub 2011 Nov 8. PMID: 22065152.
- Paller A, Kong H, Seed P, Naik S, Scharschmidt T, Gallo R, Luger T, Irvine A. The microbiome in patients with atopic dermatitis. The Journal of Allergy and Clinical Immunology. 2018. Volume 143, Issue 1, Pages 26-35. DOI: https://doi.org/10.1016/j.jaci.2018.11.015
- Varjonen E, Vainio E, Kalimo K. Antigliadin IgE–indicator of wheat allergy in atopic dermatitis. Allergy. 2000 Apr;55(4):386-91. doi: 10.1034/j.1398-9995.2000.00451.x. PMID: 10782525.
- Nosrati A, Afifi L, Danesh MJ, Lee K, Yan D, Beroukhim K, Ahn R, Liao W. Dietary modifications in atopic dermatitis: patient-reported outcomes. J Dermatolog Treat. 2017 Sep;28(6):523-538. doi: 10.1080/09546634.2016.1278071. Epub 2017 Jan 24. PMID: 28043181; PMCID: PMC5736303.
- Ciacci C, Cavallaro R, Iovino P, Sabbatini F, Palumbo A, Amoruso D, Tortora R, Mazzacca G. Allergy prevalence in adult celiac disease. J Allergy Clin Immunol. 2004 Jun;113(6):1199-203. doi: 10.1016/j.jaci.2004.03.012. PMID: 15208605.
- Nosrati A, Afifi L, Danesh MJ, Lee K, Yan D, Beroukhim K, Ahn R, Liao W. Dietary modifications in atopic dermatitis: patient-reported outcomes. J Dermatolog Treat. 2017 Sep;28(6):523-538. doi: 10.1080/09546634.2016.1278071. Epub 2017 Jan 24. PMID: 28043181; PMCID: PMC5736303.
- Worm M, Fiedler EM, Dölle S, Schink T, Hemmer W, Jarisch R, Zuberbier T. Exogenous histamine aggravates eczema in a subgroup of patients with atopic dermatitis. Acta Derm Venereol. 2009;89(1):52-6. doi: 10.2340/00015555-0565. PMID: 19197542.
- Maintz L, Benfadal S, Allam JP, Hagemann T, Fimmers R, Novak N. Evidence for a reduced histamine degradation capacity in a subgroup of patients with atopic eczema. J Allergy Clin Immunol. 2006 May;117(5):1106-12. doi: 10.1016/j.jaci.2005.11.041. Epub 2006 Feb 8. PMID: 16675339.
- Yamauchi K, Ogasawara M. The Role of Histamine in the Pathophysiology of Asthma and the Clinical Efficacy of Antihistamines in Asthma Therapy. Int J Mol Sci. 2019 Apr 8;20(7):1733. doi: 10.3390/ijms20071733. PMID: 30965592; PMCID: PMC6480561.
- Berla T, Angel J, Himadri S, Saqib B, Mahejibin K, Clinton M, Martin C, Rohit S. The Role of Histamine and Histamine Receptors in Mast Cell-Mediated Allergy and Inflammation: The Hunt for New Therapeutic Targets. Frontiers in Immunology. 2018. Volume 9, Pages 1873. ISSN 1664-3224. DOI=10.3389/fimmu.2018.01873
- Schneider L, Hanifin J, Boguniewicz M, Eichenfield LF, Spergel JM, Dakovic R, Paller AS. Study of the Atopic March: Development of Atopic Comorbidities. Pediatr Dermatol. 2016 Jul;33(4):388-98. doi: 10.1111/pde.12867. Epub 2016 Jun 7. PMID: 27273433; PMCID: PMC5649252.
- FINN, R., HARVEY, M., JOHNSON, P., VERBOV, J. and BARNES, R. (1985), Serum IgG antibodies to gliadin and other dietary antigens in adults with atopic eczema. Clinical and Experimental Dermatology, 10: 222-228. https://doi.org/10.1111/j.1365-2230.1985.tb00561.x
- Werfel T, Ballmer-Weber B, Eigenmann PA, Niggemann B, Rancé F, Turjanmaa K, Worm M. Eczematous reactions to food in atopic eczema: position paper of the EAACI and GA2LEN. Allergy. 2007 Jul;62(7):723-8. doi: 10.1111/j.1398-9995.2007.01429.x. PMID: 17573718.
- Worm M, Ehlers I, Sterry W, Zuberbier T. Clinical relevance of food additives in adult patients with atopic dermatitis. Clin Exp Allergy. 2000 Mar;30(3):407-14. doi: 10.1046/j.1365-2222.2000.00722.x. PMID: 10691900.
- Cepeda AM, Del Giacco SR, Villalba S, Tapias E, Jaller R, Segura AM, Reyes G, Potts J, Garcia-Larsen V. A Traditional Diet Is Associated with a Reduced Risk of Eczema and Wheeze in Colombian Children. Nutrients. 2015 Jun 25;7(7):5098-110. doi: 10.3390/nu7075098. PMID: 26121530; PMCID: PMC4516989.
- Vesely MD. Getting Under the Skin: Targeting Cutaneous Autoimmune Disease. Yale J Biol Med. 2020 Mar 27;93(1):197-206. PMID: 32226348; PMCID: PMC7087062.
- Holmes J, Fairclough LC, Todd I. Atopic dermatitis and autoimmunity: the occurrence of autoantibodies and their association with disease severity. Arch Dermatol Res. 2019 Apr;311(3):141-162. doi: 10.1007/s00403-019-01890-4. Epub 2019 Feb 23. Erratum in: Arch Dermatol Res. 2020 Jul;312(5):393. PMID: 30798353; PMCID: PMC7192884.
- Mu Q, Kirby J, Reilly CM, Luo XM. Leaky Gut As a Danger Signal for Autoimmune Diseases. Front Immunol. 2017 May 23;8:598. doi: 10.3389/fimmu.2017.00598. PMID: 28588585; PMCID: PMC5440529.
- Samadi N, Klems M, Untersmayr E. The role of gastrointestinal permeability in food allergy. Annals of Allergy, Asthma & Immunology. 2018. Volume 121, Issue 2, Pages 168-173. DOI:https://doi.org/10.1016/j.anai.2018.05.010
- Bertalot G, Montresor G, Tampieri M, Spasiano A, Pedroni M, Milanesi B, Favret M, Manca N, Negrini R. Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection. Clin Endocrinol (Oxf). 2004 Nov;61(5):650-2. doi: 10.1111/j.1365-2265.2004.02137.x. PMID: 15521972.
- Shi Y, Dong Y, Huang W, Zhu D, Mao H, Su P. Fecal Microbiota Transplantation for Ulcerative Colitis: A Systematic Review and Meta-Analysis. PLoS One. 2016 Jun 13;11(6):e0157259. doi: 10.1371/journal.pone.0157259. PMID: 27295210; PMCID: PMC4905678.
- Imdad A, Nicholson MR, Tanner-Smith EE, Zackular JP, Gomez-Duarte OG, Beaulieu DB, Acra S. Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2018 Nov 13;11(11):CD012774. doi: 10.1002/14651858.CD012774.pub2. PMID: 30480772; PMCID: PMC6517295.
- Wernham AGH, Veitch D, Grindlay DJC, Rogers NK, Harman KE. What’s new in atopic eczema? An analysis of systematic reviews published in 2017. Part 1: treatment and prevention. Clin Exp Dermatol. 2019 Dec;44(8):861-867. doi: 10.1111/ced.14044. Epub 2019 Aug 7. PMID: 31392785.
- Szari, S., Quinn, J.A. Supporting a Healthy Microbiome for the Primary Prevention of Eczema. Clinic Rev Allerg Immunol 57, 286–293 (2019). https://doi.org/10.1007/s12016-019-08758-5
- Isolauri, E., Arvola, T., SÜtas, Y., Moilanen, E. and Salminen, S. (2000), Probiotics in the management of atopic eczema. Clinical & Experimental Allergy, 30: 1605-610. https://doi.org/10.1046/j.1365-2222.2000.00943.x
- , , , et al. Probiotics in late infancy reduce the incidence of eczema: A randomized controlled trial. Pediatr Allergy Immunol. 2019; 30: 335– 340. https://doi.org/10.1111/pai.13018
- Li, Lin & Han, Zhen & Niu, Xiaoping & Zhang, Guozheng & Jia, Yuliang & Zhang, Shunguo & He, Chiyi. (2018). Probiotic Supplementation for Prevention of Atopic Dermatitis in Infants and Children: A Systematic Review and Meta-analysis. American Journal of Clinical Dermatology. 20. 10.1007/s40257-018-0404-3.
- Makrgeorgou A, Leonardi-Bee J, Bath-Hextall FJ, Murrell DF, Tang ML, Roberts A, Boyle RJ. Probiotics for treating eczema. Cochrane Database Syst Rev. 2018 Nov 21;11(11):CD006135. doi: 10.1002/14651858.CD006135.pub3. PMID: 30480774; PMCID: PMC6517242.
- Bath-Hextall FJ, Jenkinson C, Humphreys R, Williams HC. Dietary supplements for established atopic eczema. Cochrane Database Syst Rev. 2012 Feb 15;(2):CD005205. doi: 10.1002/14651858.CD005205.pub3. PMID: 22336810.





Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!