Common Food Intolerances: How to Identify and Treat Them
Breaking Down Gluten, Dairy, FODMAP, and Histamine Intolerances
- Symptoms|
- Causes|
- Common Food Intolerances|
- Treatments|
- Food Sensitivity Testing|
- Recommended Products|
Download this Episode (right click link and ‘Save As’)
Common food intolerances can get in the way of your day-to-day life, but it’s not always clear how to identify and treat them.
Often, food intolerances occur because of an underlying imbalance or inflammation in the gut.
Let’s break down some of the most common food intolerances, what causes them, and how to feel better.

Food Intolerance Basics
You might want to explore possible food intolerances if any of the following apply:
- You’re experiencing vague, nonspecific symptoms like fatigue, brain fog, bloating, or itchy skin, and have not yet been able to determine the cause.
- You’ve made an effort to eat healthier, but you’re still feeling unwell.
- You suspect that you might be having reactions to a certain food or foods.
Some of the most common food intolerances include gluten, dairy, FODMAPs and histamine. There is also a wide range of less common food intolerances [1].
We’ll explore each of these in more detail below.
Symptoms of Food Intolerances

The symptoms of food intolerances vary from person to person and may seem vague or disconnected. Part of what makes food intolerances hard to pinpoint is the fact that symptoms can occur hours or even days after you consume a poorly tolerated food.
If you’re experiencing any combination of these and/or other symptoms that are otherwise unexplained, you may have an underlying food intolerance [1].
- Fatigue
- Brain fog or difficulty focusing or thinking clearly
- Gastrointestinal symptoms including bloating, constipation, diarrhea, or nausea
- Frequent headaches or migraines
- Respiratory symptoms or asthma-like symptoms
- Skin reactions, eczema, itchiness, hives, rashes
Is It an Intolerance or an Allergy?
Before diving too deep into food intolerances, it’s important to understand the key differences between an intolerance and an allergy.
In the case of a true food allergy, the immune system produces a specific kind of antibody (known as IgE) in the presence of a certain kind of food that it perceives as a threat. This triggers an allergic reaction that is usually immediate and often severe.
Food allergies are typically lifelong and easily identified because reactions to the offending food(s) or allergens are quick and strong.
Food intolerances and sensitivities can be trickier to identify. They may spring up later in life, symptoms might seem vague, and reactions don’t necessarily occur immediately after eating the food [1].
The good news is that common food intolerances are not necessarily permanent, and they can often be treated by healing the gut [2, 3, 4, 5, 6].
What Causes Food Intolerances?
Imbalances in the gut are often the cause of common food intolerances [7, 8, 9, 10, 11, 12]. But let’s break that down a little bit further, because different kinds of gut issues can bring on different kinds of food intolerances.
- Immune system dysregulation in the intestines can lead to intolerances of common foods like gluten [7, 8, 9, 10]. Increased intestinal permeability (leaky gut) can cause immune system dysregulation. With leaky gut, food particles can leak into the bloodstream, where the immune system may view them as potential threats. The immune system initiates an inflammatory response, leading to immune reactions and a wide range of potential symptoms.
- Gut microbiome imbalances and/or bacterial overgrowths: An overgrowth of bacteria in the small intestine (SIBO) can lead to symptoms when consuming certain kinds of carbohydrates known as FODMAPs [11]. These FODMAPs can feed pathogenic bacteria or bacterial overgrowths in some people. Other gut bacteria imbalances and/or gut infections can also contribute to food intolerances [12].
- Enzyme deficiencies: Your body produces a number of different enzymes that are responsible for breaking down specific foods into their usable components. If you’re not producing enough of a certain enzyme, you may develop an intolerance to the food it is responsible for digesting. For example, an enzyme called lactase is required in order to break down the milk sugar lactose. If your body does not produce sufficient lactase, you may develop lactose intolerance [13].
Common food intolerances are a perfect example of the many ways in which our bodies are all different. The same foods that might be healing for one person can be problematic for another. Everything from your lifestyle to your gut microbiome to your genetics can influence how you react to various foods.
Food intolerances can also be somewhat fluid and are sometimes just reflections of a particular moment in time. This is especially true when we look at sensitivities that relate to poor gut health. How we react to a certain food can change even from one day to the next depending on what else is going on in the gut and the rest of the body.
Common Food Intolerances

It’s possible to be sensitive to many different kinds of foods, but there are a few common food intolerances that come up more often than others. These include intolerances to gluten, dairy, FODMAPs, and histamine.
Gluten
Gluten, a type of protein found in grains like wheat, barley, and rye, is one of the most common food intolerances.
In contrast to celiac disease, an autoimmune condition involving an immune system response to gluten, there is no specific test to diagnose non-celiac gluten sensitivity.
While non-celiac gluten sensitivity has received some bad press for being a fad diagnosis, research shows it’s a real condition. Estimates range from 0.6% to 6% of the population, with some researchers suggesting a higher estimate to account for the fact that many individuals likely go undiagnosed [14, 15].
Symptoms of gluten intolerance vary widely. A study involving more than 12,000 people documented symptoms from bloating and diarrhea to fatigue, headache, and brain fog among those with gluten intolerances. Bloating and abdominal pain were the most common, followed by lack of well-being and tiredness [16].
This demonstrates the fact that symptoms of common food intolerances can be somewhat vague and don’t always show up as digestive system issues [1].
The simplest way to determine whether or not you have non-celiac gluten sensitivity is to try a gluten elimination diet for a period of 2-3 weeks. If your symptoms improve during the trial, you likely have some level of gluten sensitivity.
Dairy
Dairy products can be difficult to tolerate for a few different reasons.
The inability to properly digest lactose (a sugar found in milk and milk products) is caused by a deficiency in the lactase enzyme. Lactose intolerance is thought to affect more than half of the adult population [17].
Common symptoms of lactose intolerance include diarrhea, bloating, gas, or cramping after eating dairy or cow’s milk products.
Supplementing with the lactase enzyme may be able to help [6]. Interestingly, research also shows that probiotics can help to boost the internal production of the lactase enzyme, which may be a more effective solution over time than taking the enzyme itself [18].
Some individuals also react to casein, a protein found in milk and milk products.
Finally, sensitivity to dairy may sometimes be a result of a FODMAP intolerance, which we’ll get into in more detail below [13].
FODMAPs
FODMAPs are a group of carbohydrates that are not fully digested and are instead fermented (broken down) by gut bacteria, serving as a food source for gut microbes. In the case of a bacterial overgrowth like SIBO, feeding bacteria is not what we want and can lead to a worsening of symptoms [11].
Symptoms of FODMAP intolerance may include bloating, gas, constipation, diarrhea, or abdominal pain, as well as non-GI symptoms like fatigue or foggy thinking.
A growing body of research supports the use of a low FODMAP diet for symptom improvement in SIBO, IBS, and other conditions related to the gut [19, 20]
High FODMAP foods include:
- Dairy products high in lactose (milk, ice cream)
- Garlic
- Onions
- Brussels sprouts
- Asparagus
- Legumes
- High-fructose fruits
Wheat should also be avoided on a low FODMAP diet, and research suggests that some individuals with suspected gluten sensitivity may actually have a FODMAP intolerance [21].
This is an example of an intolerance that’s less intuitive. FODMAP intolerance involves possible reactivity to a number of foods that we tend to think of as healthy as well as foods that we wouldn’t necessarily know to link together. A low FODMAP diet trial can be very helpful for identifying FODMAP intolerances.
Histamine
Histamines are chemicals that are released as part of our normal immune system response. Histamine is also found to varying degrees in a number of different kinds of foods, especially those that are aged, fermented, or processed.
Imbalances in gut bacteria or intestinal inflammation can lead to a buildup of your body’s natural histamine, making it harder to tolerate high histamine foods [22, 23, 24].
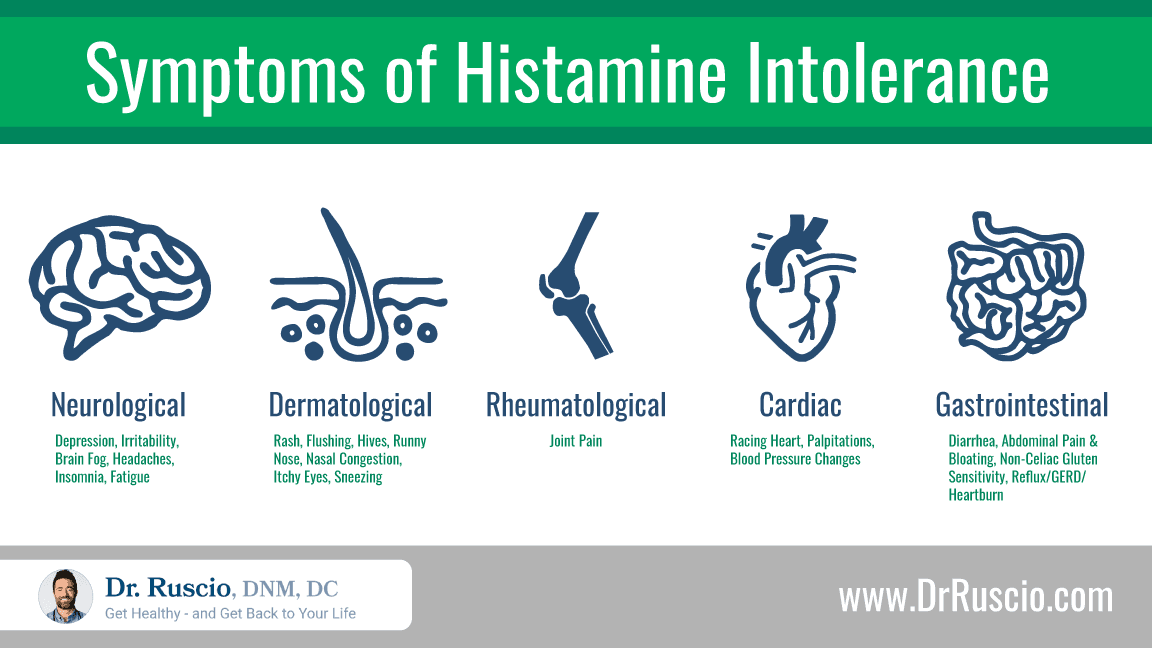
Symptoms of histamine intolerance may mimic those of allergies, but they can also affect various parts of the body [25]. One analysis of 133 histamine intolerance patients found that 97% of patients with histamine intolerance experienced combinations of at least three symptoms involving different organs [26]. An average of 11 different symptoms per individual was documented.
Histamine intolerance is thought to affect about 1% of the population [27]. One study found that among those with non-celiac gluten sensitivity whose symptoms had not improved on a gluten-free diet, 50% also had histamine intolerance [28].
A low histamine diet removes aged and fermented foods, alcohol, and certain foods that trigger histamine release, including spinach, tomatoes, and avocados. It has been shown to improve symptoms of histamine intolerance [25].
Because of the connection to gut bacteria imbalances and/or overgrowths, a modified low FODMAP diet may also be useful in cases of histamine intolerance [29].
Other Possible Food Intolerances
The following foods or groups of foods can be problematic for some people. Of course, this list is not exhaustive, and there may be intolerances of foods not listed here.
- Sulfur (high sulfur foods include meat and dairy products, coffee, black tea, and cruciferous vegetables)
- Eggs
- Nightshades (tomatoes, peppers, potatoes, eggplant)
- Monosodium glutamate (MSG) and other additives
How To Treat Food Intolerances
The general goal for healing from food intolerances is to remove potential trigger foods while working on healing the gut and any underlying issues.
The next step is to slowly reintroduce foods when the gut and immune system are better equipped to tolerate them, monitoring how you feel as you go along.
While avoiding trigger foods is a great first step, some people will require additional supports in order to fully heal and gain dietary tolerance. Supplementation with probiotics and digestive enzymes may also be helpful [2, 3, 4, 5, 6, 30].
Elimination Diet for Food Intolerances
Eating to avoid inflammation is one of the most important principles of a gut-healthy diet. This means avoiding known inflammatory foods (like fast food, sugar, and processed foods) and identifying specific foods that may trigger an immune system response for you.
An elimination diet for food intolerances focuses on these principles. Here are a few guidelines for getting started:
- The Paleo diet is a good starting point, as it eliminates common inflammatory foods (that shouldn’t be part of a healthy diet) as well as some potential trigger foods. The common offenders eliminated on the Paleo diet include dairy, gluten, soy, processed foods, and food additives.
- If you feel better after 2-3 weeks on the Paleo diet, try reintroducing certain foods to see if you can pinpoint your trigger(s). The goal here is to continue with the Paleo diet as a general framework and adapt it to your needs.
- In many cases, following a Paleo diet for a few weeks can lead to a significant improvement of symptoms. Reducing inflammation and symptoms also makes it easier to notice reactivity when foods are re-introduced.
- If the Paleo diet doesn’t bring full resolution, try a specific elimination diet like the low FODMAP diet, low histamine diet, or autoimmune Paleo diet (AIP), based on what you think is the most likely cause of your symptoms.
Keep in mind the importance of listening to your own body. If you notice that you feel unwell when you eat a certain food, even if test results don’t show it, you can always choose not to eat it. But, to limit the burden of stress, try not to panic if you do notice a symptom or a reaction. Elimination diets are by nature a process of trial and error.
Probiotics
Supplementing with probiotics in order to improve gut health is a strategy that has been proven effective in treating various different food intolerances. For example:
- One study found that combining probiotics with a gluten-free diet led to a greater symptom reduction than the diet alone for those with non-celiac gluten sensitivity [2]. Probiotics have also been shown to help reduce IBS-like symptoms in those with celiac disease [3].
- A systematic review of 15 clinical trials showed that probiotics can improve lactose intolerance symptoms [4]. Probiotics have been shown to help improve lactose intolerance by increasing the natural production of the lactase enzyme. One small study also suggests that the benefits of probiotics for enzyme production lasted longer than those of enzyme supplements [18].
- A study of 181 infants found that probiotics were just as effective as the prescription antifungal medication Nystatin in improving both fungal infection and food intolerances [5].
- A meta-analysis of 22 clinical trials showed that probiotics can lead to reduced seasonal allergy symptoms, helping to demonstrate their effect on immune system reactivity [31].
- Since it’s well-documented that probiotics are effective for improving a range of gut conditions, it’s very likely that probiotics are also effective for treating histamine intolerance (although we don’t have any direct evidence yet). While some practitioners recommend taking a low-histamine probiotic, this overlooks the net positive effect of probiotics on the gut ecosystem. Any probiotic supplement should help to reduce histamine levels.
Digestive Enzymes
For food intolerances that are due in part to enzyme deficiencies, taking specific digestive enzyme supplements may be beneficial.
- Some studies have found that supplementing with the lactase enzyme can help to improve lactose tolerance [6].
- Supplementing with the enzyme DAO has been shown to help improve symptoms of histamine intolerance [30].
- A clinical trial of 31 patients with IBS found that supplementation with the α-galactosidase enzyme alongside a low FODMAP diet can help to significantly reduce symptoms [32]. This may be a helpful finding for those with FODMAP intolerances in general.
Is Food Sensitivity Testing Worth it?

Can food sensitivity tests help to identify problematic foods? Some studies say yes [33, 34, 35]. And these types of tests are understandably appealing, as they promise a kind of customized dietary road map for feeling better.
However, there are also a few potential drawbacks that are worth considering. To begin with, the foods that show up in these test results are often the more inflammatory foods and common offenders that should be avoided in an elimination diet anyway.
These blood tests also won’t pick up on intolerances like those to histamines or FODMAPs, nor do they have the ability to identify the underlying causes of reactivity.
Finally, food sensitivity reports may come back with long lists of potentially reactive foods, which can create unnecessary anxiety over what you feel like you “can” or “can’t” eat.
In other words, it’s probably not necessary to spend the money on expensive food sensitivity tests, at least not before trying an elimination and reintroduction diet.
Focus on the Gut To Improve Food Intolerances
Food intolerances can show up in many different ways, but they generally stem from imbalances in the gut.
The best way to identify and improve food intolerances is to follow a Paleo-based elimination and reintroduction diet while taking steps to reduce intestinal inflammation and heal the gut.
The use of high-quality probiotics and/or digestive enzymes may also be helpful.
Sponsored Resources
Hi, everyone. Just a few fairly important updates. I’ve been working diligently behind the scenes tweaking and updating our paperwork, our clinical systems, our treatments, our data gathering, data organization, reporting, and patient monitoring. I’ve refined the algorithm to be even better than it was before.
And how confident am I in our clinical team? Well, my mother is working with our health coach and my father just started working with one of our doctors. So about as confident as you can get. Collectively, we are moving towards our goal of reforming functional medicine. We are gathering data on our patients and working toward publishing our data. We have taken big steps in this direction. So you are part of something big here. You’re not only a patient we aim to serve and help, but also as one of our patients, you become an example of how people can improve their health in less time and for less money compared to what appears to be commonplace in the functional medicine field. So I encourage you to look forward not only to potentially working with me, but also with any of our tremendously skilled, attentive and empathetic clinicians.
And so thank you for being a part of it or thank you for waiting to be a part of it, if you’re about to be seen soon. And if you have not yet reached out and you’re in need of help, we would be pleased and honored to work with you.
Hey there, Erin here from the Dr. Ruscio team. Can I tell you how excited I am that our brand new three in one probiotic formula is now available on our website store. It’s an easy to use powder stick format.
So I’ve been taking Dr. Ruscio’s recommended three for balanced probiotic for two years. Now I seem to take my soil-based probiotic just fine, because it’s right there next to my other supplements. But man, am I lazy about taking all three each day? The barrier for me is literally just walking over to the fridge and uncapping the other two bottles. I know it’s not hard, but that’s how busy and distracted life can be I guess.
With this three in one formula, you mix one stick with your favorite cold beverage, one to two times per day. It’s tasteless, so it won’t ruin your favorite drink. Take it with, or without food. It’s really useful as a part of your gut support and healing program and it can be used for ongoing immune and gut health maintenance. No pills, just poor mix and drink. Visit store.drruscio.com and order now.
➕ References
- Tuck CJ, Biesiekierski JR, Schmid-Grendelmeier P, Pohl D. Food Intolerances. Nutrients. 2019 Jul 22;11(7):1684. doi: 10.3390/nu11071684. PMID: 31336652; PMCID: PMC6682924.
- Di Pierro F, Bergomas F, Marraccini P, Ingenito MR, Ferrari L, Vigna L. Pilot study on non-celiac gluten sensitivity: effects of Bifidobacterium longum ES1 co-administered with a gluten-free diet. Minerva Gastroenterol Dietol. 2020 Sep;66(3):187-193. doi: 10.23736/S1121-421X.20.02673-2. Epub 2020 May 12. PMID: 32397695.
- Francavilla R, Piccolo M, Francavilla A, Polimeno L, Semeraro F, Cristofori F, Castellaneta S, Barone M, Indrio F, Gobbetti M, De Angelis M. Clinical and Microbiological Effect of a Multispecies Probiotic Supplementation in Celiac Patients With Persistent IBS-type Symptoms: A Randomized, Double-Blind, Placebo-controlled, Multicenter Trial. J Clin Gastroenterol. 2019 Mar;53(3):e117-e125. doi: 10.1097/MCG.0000000000001023. PMID: 29688915; PMCID: PMC6382041.
- Oak SJ, Jha R. The effects of probiotics in lactose intolerance: A systematic review. Crit Rev Food Sci Nutr. 2019;59(11):1675-1683. doi: 10.1080/10408398.2018.1425977. Epub 2018 Feb 9. PMID: 29425071.
- Demirel G, Celik IH, Erdeve O, Saygan S, Dilmen U, Canpolat FE. Prophylactic Saccharomyces boulardii versus nystatin for the prevention of fungal colonization and invasive fungal infection in premature infants. Eur J Pediatr. 2013 Oct;172(10):1321-6. doi: 10.1007/s00431-013-2041-4. Epub 2013 May 24. PMID: 23703468.
- Szilagyi A, Ishayek N. Lactose Intolerance, Dairy Avoidance, and Treatment Options. Nutrients. 2018 Dec 15;10(12):1994. doi: 10.3390/nu10121994. PMID: 30558337; PMCID: PMC6316316.
- Coucke F. Food intolerance in patients with manifest autoimmunity. Observational study. Autoimmun Rev. 2018 Nov;17(11):1078-1080. doi: 10.1016/j.autrev.2018.05.011. Epub 2018 Sep 11. PMID: 30213697.
- Pietschmann N. Food Intolerance: Immune Activation Through Diet-associated Stimuli in Chronic Disease. Altern Ther Health Med. 2015 Jul-Aug;21(4):42-52. PMID: 26030116.
- Levy J, Bernstein L, Silber N. Celiac disease: an immune dysregulation syndrome. Curr Probl Pediatr Adolesc Health Care. 2014 Dec;44(11):324-7. doi: 10.1016/j.cppeds.2014.10.002. PMID: 25499458.
- Briani C, Samaroo D, Alaedini A. Celiac disease: from gluten to autoimmunity. Autoimmun Rev. 2008 Sep;7(8):644-50. doi: 10.1016/j.autrev.2008.05.006. Epub 2008 Jun 25. PMID: 18589004.
- Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017 Mar 15;11(2):196-208. doi: 10.5009/gnl16126. PMID: 28274108; PMCID: PMC5347643.
- Caminero, A., Meisel, M., Jabri, B. et al. Mechanisms by which gut microorganisms influence food sensitivities. Nat Rev Gastroenterol Hepatol 16, 7–18 (2019). https://doi.org/10.1038/s41575-018-0064-z
- Deng Y, Misselwitz B, Dai N, Fox M. Lactose Intolerance in Adults: Biological Mechanism and Dietary Management. Nutrients. 2015 Sep 18;7(9):8020-35. doi: 10.3390/nu7095380. PMID: 26393648; PMCID: PMC4586575.
- DiGiacomo DV, Tennyson CA, Green PH, Demmer RT. Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: results from the Continuous National Health and Nutrition Examination Survey 2009-2010. Scand J Gastroenterol. 2013 Aug;48(8):921-5. doi: 10.3109/00365521.2013.809598. Epub 2013 Jul 8. PMID: 23834276.
- Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DS, Schumann M, Ullrich R, Villalta D, Volta U, Catassi C, Fasano A. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012 Feb 7;10:13. doi: 10.1186/1741-7015-10-13. PMID: 22313950; PMCID: PMC3292448.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR; Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12:85. doi: 10.1186/1741-7015-12-85. PMID: 24885375; PMCID: PMC4053283.
- Storhaug C, Fosse S, Fadnes L. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. The Lancet Gastroenterology and Hepatology. 2017 Oct 1. VOLUME 2, ISSUE 10, P738-746. DOI:https://doi.org/10.1016/S2468-1253(17)30154-1
- Almeida CC, Lorena SL, Pavan CR, Akasaka HM, Mesquita MA. Beneficial effects of long-term consumption of a probiotic combination of Lactobacillus casei Shirota and Bifidobacterium breve Yakult may persist after suspension of therapy in lactose-intolerant patients. Nutr Clin Pract. 2012 Apr;27(2):247-51. doi: 10.1177/0884533612440289. Epub 2012 Mar 8. PMID: 22402407.
- Marsh A, Eslick EM, Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016 Apr;55(3):897-906. doi: 10.1007/s00394-015-0922-1. Epub 2015 May 17. PMID: 25982757.
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2):252-8. doi: 10.1111/j.1440-1746.2009.06149.x. PMID: 20136989.
- Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, Veierød MB, Henriksen C, Lundin KEA. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology. 2018 Feb;154(3):529-539.e2. doi: 10.1053/j.gastro.2017.10.040. Epub 2017 Nov 2. PMID: 29102613.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Manzotti G, Breda D, Di Gioacchino M, Burastero SE. Serum diamine oxidase activity in patients with histamine intolerance. Int J Immunopathol Pharmacol. 2016 Mar;29(1):105-11. doi: 10.1177/0394632015617170. Epub 2015 Nov 16. PMID: 26574488; PMCID: PMC5806734.
- Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol. 2018 Aug;69(4). doi: 10.26402/jpp.2018.4.09. Epub 2018 Dec 9. PMID: 30552302.
- Schnedl W.J., Lackner S., Enko D., Schenk M., Holasek S.J., Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intest. Res. 2019;17:427–433. doi: 10.5217/ir.2018.00152.
- Schnedl WJ, Lackner S, Enko D, Schenk M, Holasek SJ, Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intest Res. 2019 Jul;17(3):427-433. doi: 10.5217/ir.2018.00152. Epub 2019 Mar 7. PMID: 30836736; PMCID: PMC6667364.
- Kohn JB. Is there a diet for histamine intolerance? J Acad Nutr Diet. 2014 Nov;114(11):1860. doi: 10.1016/j.jand.2014.09.009. Epub 2014 Oct 24. PMID: 25439083.
- Schnedl W, Mangge H, Schenk M, Enko D. Non-responsive celiac disease may coincide with additional food intolerance/malabsorption, including histamine intolerance. Medical Hypotheses. 2021. Volume 146, 110404. ISSN 0306-9877. https://doi.org/10.1016/j.mehy.2020.110404.
- Enko D, Meinitzer A, Mangge H, Kriegshäuser G, Halwachs-Baumann G, Reininghaus EZ, Bengesser SA, Schnedl WJ. Concomitant Prevalence of Low Serum Diamine Oxidase Activity and Carbohydrate Malabsorption. Can J Gastroenterol Hepatol. 2016;2016:4893501. doi: 10.1155/2016/4893501. Epub 2016 Nov 30. PMID: 28042564; PMCID: PMC5155086.
- Schnedl WJ, Schenk M, Lackner S, Enko D, Mangge H, Forster F. Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food Sci Biotechnol. 2019 May 24;28(6):1779-1784. doi: 10.1007/s10068-019-00627-3. PMID: 31807350; PMCID: PMC6859183.
- Güvenç IA, Muluk NB, Mutlu FŞ, Eşki E, Altıntoprak N, Oktemer T, Cingi C. Do probiotics have a role in the treatment of allergic rhinitis? A comprehensive systematic review and meta-analysis. Am J Rhinol Allergy. 2016 Sep 1;30(5):157-175. doi: 10.2500/ajra.2016.30.4354. Epub 2016 Jul 20. PMID: 27442711.
- Tuck CJ, Taylor KM, Gibson PR, Barrett JS, Muir JG. Increasing Symptoms in Irritable Bowel Symptoms With Ingestion of Galacto-Oligosaccharides Are Mitigated by α-Galactosidase Treatment. Am J Gastroenterol. 2018 Jan;113(1):124-134. doi: 10.1038/ajg.2017.245. Epub 2017 Aug 15. PMID: 28809383.
- Jian L, Anqi H, Gang L, Litian W, Yanyan X, Mengdi W, Tong L. Food Exclusion Based on IgG Antibodies Alleviates Symptoms in Ulcerative Colitis: A Prospective Study. Inflamm Bowel Dis. 2018 Aug 16;24(9):1918-1925. doi: 10.1093/ibd/izy110. PMID: 29788288.
- Aydinlar EI, Dikmen PY, Tiftikci A, Saruc M, Aksu M, Gunsoy HG, Tozun N. IgG-based elimination diet in migraine plus irritable bowel syndrome. Headache. 2013 Mar;53(3):514-25. doi: 10.1111/j.1526-4610.2012.02296.x. Epub 2012 Dec 6. PMID: 23216231.
- Guo H, Jiang T, Wang J, Chang Y, Guo H, Zhang W. The value of eliminating foods according to food-specific immunoglobulin G antibodies in irritable bowel syndrome with diarrhoea. J Int Med Res. 2012;40(1):204-10. doi: 10.1177/147323001204000121. PMID: 22429360.






Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!