The Surprising Autoimmune Skin Disease-Gut Health Connection
Improve Skin Autoimmune Disease Symptoms by Paying Attention to Your Gut
- The Gut-Skin Connection|
- Autoimmune Skin Diseases|
- Gut Health and Autoimmune Disease|
- Diet and Lifestyle Improvements|
- Bottom Line |
Download this Episode (right click link and ‘Save As’)
- The gut microbiome and the skin are connected via the skin-gut axis, and microbial imbalances (dysbiosis) in your gut or on your skin can contribute to the development of skin diseases.
- There are several categories of autoimmune skin diseases, including connective tissue diseases, autoimmune blistering diseases, blood disorders, and discoloration diseases.
- Symptoms of autoimmune skin disease vary and can include blistering, skin rashes, visible blood vessels, thickening of the skin, scaly patches, and lesions.
- Research suggests some autoimmune diseases respond well to gut support.
- Mild to moderate cases of autoimmune skin disease can benefit from natural therapies such as an anti-inflammatory diet, exercise, time in nature, natural sunlight, and probiotics

Autoimmune diseases, including skin autoimmune diseases, are on the rise. While the development of a skin manifestation of autoimmune disease is multifactorial, autoimmune skin diseases like psoriasis or vitiligo are the result of an immune response gone awry. Essentially, your immune system mistakenly attacks your healthy skin.
Just as with other autoimmune diseases, the body is affected systemically, which can impact quality of life and create less-than-ideal outcomes if left untreated [1]. In addition, while many autoimmune diseases are invisible to the naked eye, skin autoimmune diseases are on display for the world to see, which can impact your mental health.
If you’ve been struggling to manage your autoimmune skin disease, improving your gut health may be the missing link. In this article, we’ll discuss the connection between your gut and skin microbiomes, the current research about skin autoimmune diseases, how gut health impacts autoimmunity, and what you can do to improve your autoimmune skin condition.
The Gut-Skin Connection
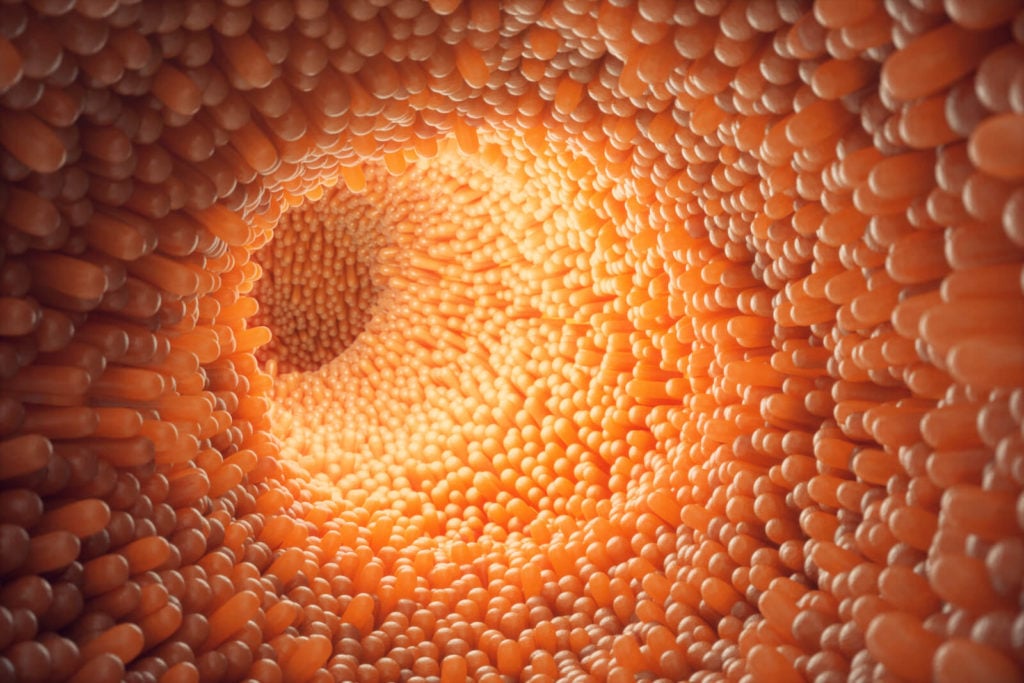
Research is solidifying the importance of the gut microbiome as an overall driver of health, but did you know the goings on in your gut can also affect your skin? It may seem far-fetched that a scaly psoriasis patch could be connected to your gut health, but we now know there’s a link between the gut and the skin, called the skin-gut axis [2, 3].
The gut and the skin are both important immune system regulators and they each have their own unique microbiomes. When imbalances occur in either, your skin can be affected [4, 5]. As reported in one 2021 literature review, “dysbiosis in the skin and/or gut microbiome is associated with an altered immune response, promoting the development of skin diseases” [6].
Here are a few examples of how the gut-skin axis is involved in the development of skin manifestation of autoimmune disease and immune-mediated skin diseases (IMSDs):
- Atopic dermatitis (eczema): While not confirmed as autoimmune in nature, skin microbial diversity is reduced, allowing for the proliferation of Staphylococcus aureus, which is a common cause of skin infections. In addition, there are lower concentrations of Faecalibacterium prausnitzii, which stimulate the production of short-chain fatty acids in the gut to provide an anti-inflammatory benefit [4].
- Psoriasis: The skin lesions of psoriasis patients have higher levels of Proteobacteria, which are typically pathogenic, along with a higher Streptococcus-to-Proteobacteria ratio when compared to controls. In addition, the stool of psoriasis patients often has less beneficial bacteria and more of the pathogenic strains of E. coli. [4, 5, 7]. And one 2020 observational study and meta-analysis found gut dysbiosis among psoriasis patients when compared to controls, indicating a role of gut dysbiosis in the development of the disease [8].
- Vitiligo: Patients with vitiligo experience the destruction of melanocytes (cells that give the skin its color) from immune cells, cytokines, or autoantibodies. Whereas their healthy skin sites have mainly Actinobacteria, the lesional sites have been found to be high in Firmicutes and Proteobacteria [4].
- Systemic lupus erythematosus (SLE): Patients have been shown to have lower ratios of Firmicutes to Bacteroidetes bacteria on their skin and in their mouths [9], and they commonly have leaky gut [10].
- Dermatitis herpetiformis: The skin manifestation of celiac disease (an autoimmune disease), resulting from small intestinal damage related to the consumption of gluten [11].
While more research needs to be completed, it does appear that skin autoimmune diseases are related in part to gut health. One example being the association between psoriasis and gut-related autoimmune diseases such as celiac and inflammatory bowel disease (IBD) [12, 13].
Common Autoimmune Skin Diseases
The full list of autoimmune skin conditions is exhaustive, but some of the more common ones include bullous pemphigoid, scleroderma, psoriasis, autoimmune vasculitis, and dermatomyositis. Additionally, while not previously considered autoimmune in nature, one 2019 systematic review and meta analysis found a strong association between autoantibodies and atopic dermatitis, indicating an immune-mediated connection [14].
There are several categories of skin autoimmune diseases:
- Connective tissue diseases, such as dermatomyositis, morphea, scleroderma, psoriatic arthritis, and psoriasis. These diseases are often characterized by rashes, thickening of the skin, or changes in the collagen and connective tissue. Psoriasis is the most-researched autoimmune skin condition.
- Autoimmune blistering diseases, such as linear IgA bullous disease, pemphigus and other pemphigoid diseases, and dermatitis herpetiformis. As the name implies, patients commonly have blisters or blister-like rashes.
- Blood disorders like autoimmune-mediated vasculitis, which causes inflamed blood vessels in the skin.
- Discoloration diseases, like systemic lupus erythematosus (SLE) — otherwise known as lupus — and vitiligo, in which the skin cells that create pigment die.
It’s difficult to say how many people have autoimmune skin conditions, as there are so many different types. The incidence of individual conditions is low, varying between 0.2% for scleroderma [15] and 3.2% for psoriasis [16].
Autoimmune Skin Disease Symptoms
Symptoms of autoimmune skin diseases vary widely, but skin manifestation of autoimmune disease is typical along with some of the common autoimmune symptoms, such as joint pain, fatigue [17], recurrent fevers, and problems with internal organs.
The most common symptoms include:
- Blisters or blistering
- Skin rashes
- Visible blood vessels
- Thickening of the skin or scaly patches
- Lesions
Skin autoimmune diseases are typically diagnosed by a dermatologist or rheumatologist, who may evaluate your symptoms along with a general screening blood test for antinuclear antibodies (ANA). If the ANA test is positive, your doctor may order follow-up testing, such as skin biopsies or additional blood tests, to determine a diagnosis.
In moderate to severe cases, the skin manifestation of autoimmune disease can have a significant impact on quality of life by disrupting cosmetic appearance, sleep, and general comfort.
Gut Health and Autoimmune Disease

Many researchers and doctors have hypothesized that leaky gut — otherwise known as intestinal permeability — is a root cause of and a major risk factor for autoimmune diseases. While there is certainly evidence to suggest they’re connected, there isn’t research to confirm this yet.
Autoimmune diseases are thought to develop from a genetic predisposition, an environmental trigger, and the element of increased intestinal permeability [18]. While there is not yet data to suggest that repairing intestinal permeability improves autoimmune skin conditions directly, it makes sense that targeting root cause in the gut could lead to symptom improvement.
Research does suggest that some autoimmune disorders are responsive to gut support, particularly Hashimoto’s thyroiditis and IBD [19, 20, 21]. Let’s summarize what we know about how improving gut health can improve autoimmune diseases.
Hashimoto’s Thyroiditis and Gut Health
Hashimoto’s thyroiditis has been closely associated with small intestinal bacterial overgrowth (SIBO) [22, 23, 24], and resolving gut infections such as H. pylori [19] and Blastocystis hominis (a parasite) [25] has been shown to improve thyroid autoantibodies. Additionally, treatment with probiotic supplements has been shown to reduce fatigue and needed thyroid medication, likely because they help restore balance to the gut microbiome [26, 27, 28, 29, 30, 31, 32, 33].
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease encompasses several digestive diseases, including Crohn’s disease and ulcerative colitis. IBD appears to be related to the composition of the gut microbiome. In two studies, at least one-third of IBD patients had pathogenic bacterial infections in their guts [34, 35].
Fecal microbiota transplant (FMT) has been shown in several research studies to improve or resolve IBD [20, 21]. And finally, probiotic supplementation has been shown to improve the success rate of conventional IBD treatment [36] and to improve symptoms and quality of life for IBD patients [37, 38, 39, 40].
IBD is associated with the skin autoimmune disease psoriasis.
Other Autoimmune-Gut Connections
Type 1 diabetes and rheumatoid arthritis have also been shown to be related to gut health.
In one clinical trial, all the type 1 diabetes patients had results indicating leaky gut [41], leading the researchers to suggest small intestinal health plays a role in the development of type 1 diabetes.
Rheumatoid arthritis (RA) has also been shown in several studies to be affected by gut health. A meta-analysis suggests that more virulent strains of H. pylori are likely to increase the risk of rheumatoid arthritis, as well as lupus, autoimmune gastritis, and autoimmune pancreatitis [42]. Other research suggests that RA patients are more likely to have dysbiosis than controls [43, 44], and that probiotic supplementation improves inflammatory markers and disease activity [41, 45].
So while we have limited specific evidence that improving gut health can improve autoimmune skin disease, research suggests that improving the gut microbiome and gut health can impact autoimmune disease symptoms and disease markers. So we can cautiously presume that enhancing gut health would positively affect autoimmune skin conditions. Some limited evidence supports this notion.
Let’s discuss diet and lifestyle strategies that can be an adjunct to your standard medical treatment.
Can Diet and Lifestyle Improve Skin Autoimmunity?

Conventional treatment for skin autoimmune diseases typically includes immunosuppressive medications such as azathioprine. However, many of these medications come with challenging side effects [46]. Biologic medications are also used, and a 2021 systematic review and meta-analysis of randomized controlled trials found biologic medications such as infliximab, risankizumab, and brodalumab to be safe and effective for the treatment of psoriasis [47].
While immunosuppressive and biologic medications may be required for the treatment of severe skin autoimmune diseases, those with mild to moderate symptoms may experience significant relief from nutrition and lifestyle-related strategies like an anti-inflammatory diet, exercise, sun exposure, and probiotics.
Anti-Inflammatory Diet

A well-balanced, anti-inflammatory diet is foundational for improving gut and overall health for people with autoimmune diseases, and this goes for autoimmune skin conditions as well.
Let’s take a look at some of the research regarding diet and autoimmunity:
Gluten
- Some evidence suggests that gluten may be a trigger for some skin conditions such as eczema [48, 49].
- Celiac disease, an autoimmune condition that damages small intestine villi due to an immune reaction to gluten proteins, is associated with psoriasis [12].
- A gluten-free diet has been shown to improve autoimmune thyroid disease and IBD [50, 51, 52, 53].
Low FODMAP
- A 2019 systematic review found a low FODMAP diet may be helpful for improving gastrointestinal symptoms in those with scleroderma [54].
While more research needs to be completed, a whole-foods diet that’s gluten-free and low in processed and sensitive foods, sugars, and trans fats is worth a trial to reduce the inflammation that is the hallmark of autoimmune disease [55, 56, 57, 58, 59].
You can begin by incorporating more fresh, whole foods, or try an anti-inflammatory meal plan such as the Paleo diet.
If the Paleo diet doesn’t lead to symptom improvement, you might consider trying the low FODMAP diet or the Autoimmune Protocol (AIP) diet.
Exercise
If you have an autoimmune skin condition, creating good exercise habits can help improve your health, quality of life, and possibly disease activity.
Regular moderate exercise has been shown to decrease inflammation and general intestinal permeability [60, 61]. And one 2021 systematic review found exercise improved disease activity, pain, fatigue, skin symptoms, and quality of life in psoriatic arthritis patients [62]. In addition, a few studies have shown exercise to improve psoriasis [63], especially when combined with weight loss [64].
In the case of scleroderma, high-intensity interval training (HIIT) and resistance training twice a week for 12 weeks led to symptom reduction [65], and an at-home exercise program improved physical performance, quality of life, and disability [66].
A 2020 randomized controlled trial found resistance training to improve physical function and quality of life, but not disease activity, in women with Sjogren’s syndrome [67].
While SLE patients didn’t experience improvements in disease activity in one trial of moderate to high-intensity aerobic exercise, they did see improvements in fitness level, fatigue, and depression [68].
Time in Nature and Sun Exposure
Spending time in nature isn’t just a good way to tame your stress. It’s also been shown to help autoimmune skin symptoms. Some studies indicate that low vitamin D is associated with greater gut permeability and worse outcomes for people with IBD [69, 70, 71], and sun exposure has been shown to protect against digestive tract disease and inflammation, specifically diverticulitis and IBD [72].
A systematic review and meta-analysis also found that people with alopecia areata (an autoimmune skin condition) were more likely to be deficient in vitamin D [73].
Sun exposure specifically has been shown to reduce symptom severity for people with psoriasis [74]. It’s possible this may be due to increases in vitamin D status. If you have an autoimmune skin condition, consider discussing your vitamin D level and vitamin D supplementation with your healthcare provider.
Other Natural Therapies
- Light therapy: Ultraviolet light therapy is a common treatment for those with psoriasis. One 2020 systematic review and meta-analysis of randomized controlled trials found some evidence to suggest a salt bath in addition to UVB light can help improve psoriasis symptoms [75].
- Selenium: A 2020 randomized controlled trial found topical and oral selenium helped to improve oral lichen planus lesions as much as topical corticosteroids [76].
- Tripterygium glycosides: An active compound of a Chinese herb has been found in a 2021 systematic review and meta-analysis of randomized controlled trials to decrease symptoms and inflammation in people with Sjogren’s syndrome [77].
In additional studies, a combination of Melissa officinalis (lemon balm), Damask rose, and fennel didn’t improve psoriasis more than placebo [78], and fecal microbiota transplant (FMT) was worse than placebo in those with psoriatic arthritis [79].
Probiotics
Probiotics can help promote a healthy immune system [80, 81, 82], rebalance the gut microbiome [80], reduce inflammation [83], and reduce leaky gut [84, 85, 86]. In addition to all the data we have that demonstrate their effectiveness for other autoimmune diseases, a few studies indicate probiotics can improve specific autoimmune skin conditions:
- In one study, a group of patients with psoriasis were given a probiotic blend of Bifidobacterium longum, B. lactis, and Lactobacillus rhamnosus alongside topical steroid treatment. After 12 weeks, 67% of patients in the probiotic group had better symptom control compared to 42% of patients in the placebo group [87], and the probiotic group had a lower risk of relapse after six months.
- In one additional study, participants with systemic sclerosis who were given a probiotic blend of Lactobacillus paracasei, L. rhamnosus, L. acidophilus, and Bifidobacterium lactis probiotics had lower levels of inflammatory T cells [88].
- A 2020 systematic review and meta-analysis of randomized controlled trials found probiotics to improve the skin in atopic dermatitis (which may have an immune-mediated component) [89].
- One study found probiotics helpful in improving gastrointestinal symptoms in scleroderma [54].
Given their potential to improve your gut and immune system function and to decrease your autoimmune symptoms without side effects, a trial of probiotic therapy may be worth your while if you have an autoimmune skin condition. For more about how to use probiotics to improve your gut health, see our Probiotics Starter Guide.
The Bottom Line
While more research needs to be completed, there does seem to be some good evidence that the health of the gut microbiome can affect autoimmune skin conditions.
For severe skin manifestations of autoimmune disease, medication may be necessary, but a healthy diet, lifestyle modification, and the addition of probiotics are low-cost, safe interventions that may significantly improve your symptoms and quality of life.
For more information on optimizing your gut health, check out my book Healthy Gut, Healthy You. If you’ve completed the step-by-step process outlined there, but still struggle with autoimmune skin disease symptoms or you desire a more personalized plan, contact the clinic at the Ruscio Institute for Functional Health.
The Ruscio Institute has developed a range of high-quality formulations to help our patients and audience. If you’re interested in learning more about these products, please click here. Note that there are many other options available, and we encourage you to research which products may be right for you.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Vesely MD. Getting under the skin: targeting cutaneous autoimmune disease. Yale J Biol Med. 2020 Mar 27;93(1):197–206. PMID: 32226348. PMCID: PMC7087062.
- O’Neill CA, Monteleone G, McLaughlin JT, Paus R. The gut-skin axis in health and disease: A paradigm with therapeutic implications. Bioessays. 2016 Nov;38(11):1167–76. DOI: 10.1002/bies.201600008. PMID: 27554239.
- Polkowska-Pruszyńska B, Gerkowicz A, Krasowska D. The gut microbiome alterations in allergic and inflammatory skin diseases – an update. J Eur Acad Dermatol Venereol. 2020 Mar;34(3):455–64. DOI: 10.1111/jdv.15951. PMID: 31520544.
- Catinean A, Neag MA, Mitre AO, Bocsan CI, Buzoianu AD. Microbiota and Immune-Mediated Skin Diseases-An Overview. Microorganisms. 2019 Aug 21;7(9). DOI: 10.3390/microorganisms7090279. PMID: 31438634. PMCID: PMC6781142.
- Fahlén A, Engstrand L, Baker BS, Powles A, Fry L. Comparison of bacterial microbiota in skin biopsies from normal and psoriatic skin. Arch Dermatol Res. 2012 Jan;304(1):15–22. DOI: 10.1007/s00403-011-1189-x. PMID: 22065152.
- De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms. 2021 Feb 11;9(2). DOI: 10.3390/microorganisms9020353. PMID: 33670115. PMCID: PMC7916842.
- Eppinga H, Sperna Weiland CJ, Thio HB, van der Woude CJ, Nijsten TEC, Peppelenbosch MP, et al. Similar Depletion of Protective Faecalibacterium prausnitzii in Psoriasis and Inflammatory Bowel Disease, but not in Hidradenitis Suppurativa. J Crohns Colitis. 2016 Sep;10(9):1067–75. DOI: 10.1093/ecco-jcc/jjw070. PMID: 26971052.
- Dei-Cas I, Giliberto F, Luce L, Dopazo H, Penas-Steinhardt A. Metagenomic analysis of gut microbiota in non-treated plaque psoriasis patients stratified by disease severity: development of a new Psoriasis-Microbiome Index. Sci Rep. 2020 Jul 29;10(1):12754. DOI: 10.1038/s41598-020-69537-3. PMID: 32728075. PMCID: PMC7391695.
- van der Meulen TA, Harmsen HJM, Vila AV, Kurilshikov A, Liefers SC, Zhernakova A, et al. Shared gut, but distinct oral microbiota composition in primary Sjögren’s syndrome and systemic lupus erythematosus. J Autoimmun. 2019 Feb;97:77–87. DOI: 10.1016/j.jaut.2018.10.009. PMID: 30416033.
- Azzouz D, Omarbekova A, Heguy A, Schwudke D, Gisch N, Rovin BH, et al. Lupus nephritis is linked to disease-activity associated expansions and immunity to a gut commensal. Ann Rheum Dis. 2019 Jul;78(7):947–56. DOI: 10.1136/annrheumdis-2018-214856. PMID: 30782585. PMCID: PMC6585303.
- Salmi TT. Dermatitis herpetiformis. Clin Exp Dermatol. 2019 Oct;44(7):728–31. DOI: 10.1111/ced.13992. PMID: 31093998.
- Bhatia BK, Millsop JW, Debbaneh M, Koo J, Linos E, Liao W. Diet and psoriasis, part II: celiac disease and role of a gluten-free diet. J Am Acad Dermatol. 2014 Aug;71(2):350–8. DOI: 10.1016/j.jaad.2014.03.017. PMID: 24780176. PMCID: PMC4104239.
- Fu Y, Lee C-H, Chi C-C. Association of Psoriasis With Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. JAMA Dermatol. 2018 Dec 1;154(12):1417–23. DOI: 10.1001/jamadermatol.2018.3631. PMID: 30422277. PMCID: PMC6583370.
- Holmes J, Fairclough LC, Todd I. Atopic dermatitis and autoimmunity: the occurrence of autoantibodies and their association with disease severity. Arch Dermatol Res. 2019 Apr;311(3):141–62. DOI: 10.1007/s00403-019-01890-4. PMID: 30798353. PMCID: PMC7192884.
- Mayes MD. Classification and epidemiology of scleroderma. Semin Cutan Med Surg. 1998 Mar;17(1):22–6. DOI: 10.1016/s1085-5629(98)80058-8. PMID: 9512103.
- Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014 Mar;70(3):512–6. DOI: 10.1016/j.jaad.2013.11.013. PMID: 24388724.
- Autoimmune Skin Disease: Skin Lupus, Pemphigus, & Other Autoimmune Skin Disorders | University of Utah Health [Internet]. Available from: https://healthcare.utah.edu/dermatology/services/autoimmune-skin-diseases/
- Fasano A. All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. [version 1; peer review: 3 approved]. F1000Res. 2020 Jan 31;9. DOI: 10.12688/f1000research.20510.1. PMID: 32051759. PMCID: PMC6996528.
- Bertalot G, Montresor G, Tampieri M, Spasiano A, Pedroni M, Milanesi B, et al. Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection. Clin Endocrinol (Oxf). 2004 Nov;61(5):650–2. DOI: 10.1111/j.1365-2265.2004.02137.x. PMID: 15521972.
- Shi Y, Dong Y, Huang W, Zhu D, Mao H, Su P. Fecal Microbiota Transplantation for Ulcerative Colitis: A Systematic Review and Meta-Analysis. PLoS ONE. 2016 Jun 13;11(6):e0157259. DOI: 10.1371/journal.pone.0157259. PMID: 27295210. PMCID: PMC4905678.
- Imdad A, Nicholson MR, Tanner-Smith EE, Zackular JP, Gomez-Duarte OG, Beaulieu DB, et al. Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2018 Nov 13;11:CD012774. DOI: 10.1002/14651858.CD012774.pub2. PMID: 30480772. PMCID: PMC6517295.
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017 Feb 7;23(5):842–52. DOI: 10.3748/wjg.v23.i5.842. PMID: 28223728. PMCID: PMC5296200.
- Konrad P, Chojnacki J, Kaczka A, Pawłowicz M, Rudnicki C, Chojnacki C. [Thyroid dysfunction in patients with small intestinal bacterial overgrowth]. Pol Merkur Lekarski. 2018 Jan 23;44(259):15–8. PMID: 29374417.
- Choi YM, Kim TY, Kim EY, Jang EK, Jeon MJ, Kim WG, et al. Association between thyroid autoimmunity and Helicobacter pylori infection. Korean J Intern Med. 2017 Mar;32(2):309–13. DOI: 10.3904/kjim.2014.369. PMID: 28092700. PMCID: PMC5339455.
- El-Zawawy HT, Farag HF, Tolba MM, Abdalsamea HA. Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17. Ther Adv Endocrinol Metab. 2020 Feb 21;11:2042018820907013. DOI: 10.1177/2042018820907013. PMID: 32128107. PMCID: PMC7036484.
- Eslami M, Yousefi B, Kokhaei P, Jazayeri Moghadas A, Sadighi Moghadam B, Arabkari V, et al. Are probiotics useful for therapy of Helicobacter pylori diseases? Comp Immunol Microbiol Infect Dis. 2019 Jun;64:99–108. DOI: 10.1016/j.cimid.2019.02.010. PMID: 31174707.
- Zhou B-G, Chen L-X, Li B, Wan L-Y, Ai Y-W. Saccharomyces boulardii as an adjuvant therapy for Helicobacter pylori eradication: A systematic review and meta-analysis with trial sequential analysis. Helicobacter. 2019 Oct;24(5):e12651. DOI: 10.1111/hel.12651. PMID: 31414551.
- Koga Y, Ohtsu T, Kimura K, Asami Y. Probiotic L. gasseri strain (LG21) for the upper gastrointestinal tract acting through improvement of indigenous microbiota. BMJ Open Gastroenterol. 2019 Aug 12;6(1):e000314. DOI: 10.1136/bmjgast-2019-000314. PMID: 31523442. PMCID: PMC6711431.
- Lü M, Yu S, Deng J, Yan Q, Yang C, Xia G, et al. Efficacy of Probiotic Supplementation Therapy for Helicobacter pylori Eradication: A Meta-Analysis of Randomized Controlled Trials. PLoS ONE. 2016 Oct 10;11(10):e0163743. DOI: 10.1371/journal.pone.0163743. PMID: 27723762. PMCID: PMC5056761.
- Tong JL, Ran ZH, Shen J, Zhang CX, Xiao SD. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther. 2007 Jan 15;25(2):155–68. DOI: 10.1111/j.1365-2036.2006.03179.x. PMID: 17229240.
- Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017 Apr;51(4):300–11. DOI: 10.1097/MCG.0000000000000814. PMID: 28267052.
- Soifer LO, Peralta D, Dima G, Besasso H. [Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study]. Acta Gastroenterol Latinoam. 2010 Dec;40(4):323–7. PMID: 21381407.
- Leventogiannis K, Gkolfakis P, Spithakis G, Tsatali A, Pistiki A, Sioulas A, et al. Effect of a Preparation of Four Probiotics on Symptoms of Patients with Irritable Bowel Syndrome: Association with Intestinal Bacterial Overgrowth. Probiotics Antimicrob Proteins. 2019 Jun;11(2):627–34. DOI: 10.1007/s12602-018-9401-3. PMID: 29508268. PMCID: PMC6541575.
- Darfeuille-Michaud A, Boudeau J, Bulois P, Neut C, Glasser A-L, Barnich N, et al. High prevalence of adherent-invasive Escherichia coli associated with ileal mucosa in Crohn’s disease. Gastroenterology. 2004 Aug;127(2):412–21. PMID: 15300573.
- Lapaquette P, Glasser A-L, Huett A, Xavier RJ, Darfeuille-Michaud A. Crohn’s disease-associated adherent-invasive E. coli are selectively favoured by impaired autophagy to replicate intracellularly. Cell Microbiol. 2010 Jan;12(1):99–113. DOI: 10.1111/j.1462-5822.2009.01381.x. PMID: 19747213. PMCID: PMC3743084.
- Hedin C, Whelan K, Lindsay JO. Evidence for the use of probiotics and prebiotics in inflammatory bowel disease: a review of clinical trials. Proc Nutr Soc. 2007 Aug;66(3):307–15. DOI: 10.1017/S0029665107005563. PMID: 17637082.
- Astó E, Méndez I, Audivert S, Farran-Codina A, Espadaler J. The Efficacy of Probiotics, Prebiotic Inulin-Type Fructans, and Synbiotics in Human Ulcerative Colitis: A Systematic Review and Meta-Analysis. Nutrients. 2019 Jan 30;11(2). DOI: 10.3390/nu11020293. PMID: 30704039. PMCID: PMC6412539.
- Yoshimatsu Y, Yamada A, Furukawa R, Sono K, Osamura A, Nakamura K, et al. Effectiveness of probiotic therapy for the prevention of relapse in patients with inactive ulcerative colitis. World J Gastroenterol. 2015 May 21;21(19):5985–94. DOI: 10.3748/wjg.v21.i19.5985. PMID: 26019464. PMCID: PMC4438034.
- McFarland LV. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J Gastroenterol. 2010 May 14;16(18):2202–22. PMID: 20458757. PMCID: PMC2868213.
- Ganji-Arjenaki M, Rafieian-Kopaei M. Probiotics are a good choice in remission of inflammatory bowel diseases: A meta analysis and systematic review. J Cell Physiol. 2018 Mar;233(3):2091–103. DOI: 10.1002/jcp.25911. PMID: 28294322.
- Bosi E, Molteni L, Radaelli MG, Folini L, Fermo I, Bazzigaluppi E, et al. Increased intestinal permeability precedes clinical onset of type 1 diabetes. Diabetologia. 2006 Dec;49(12):2824–7. DOI: 10.1007/s00125-006-0465-3. PMID: 17028899.
- Youssefi M, Tafaghodi M, Farsiani H, Ghazvini K, Keikha M. Helicobacter pylori infection and autoimmune diseases; Is there an association with systemic lupus erythematosus, rheumatoid arthritis, autoimmune atrophy gastritis and autoimmune pancreatitis? A systematic review and meta-analysis study. J Microbiol Immunol Infect. 2021 Jun;54(3):359–69. DOI: 10.1016/j.jmii.2020.08.011. PMID: 32891538.
- Sandhya P, Danda D, Sharma D, Scaria V. Does the buck stop with the bugs?: an overview of microbial dysbiosis in rheumatoid arthritis. Int J Rheum Dis. 2016 Jan;19(1):8–20. DOI: 10.1111/1756-185X.12728. PMID: 26385261.
- Zhang X, Zhang D, Jia H, Feng Q, Wang D, Liang D, et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med. 2015 Aug;21(8):895–905. DOI: 10.1038/nm.3914. PMID: 26214836.
- Zamani B, Golkar HR, Farshbaf S, Emadi-Baygi M, Tajabadi-Ebrahimi M, Jafari P, et al. Clinical and metabolic response to probiotic supplementation in patients with rheumatoid arthritis: a randomized, double-blind, placebo-controlled trial. Int J Rheum Dis. 2016 Sep;19(9):869–79. DOI: 10.1111/1756-185X.12888. PMID: 27135916.
- Azathioprine [Internet]. Drugs.com Know more,. Be sure. – Azathioprine. Available from: https://www.drugs.com/monograph/azathioprine.html
- Sbidian E, Chaimani A, Garcia-Doval I, Doney L, Dressler C, Hua C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2021 Apr 19;4:CD011535. DOI: 10.1002/14651858.CD011535.pub4. PMID: 33871055. PMCID: PMC8408312.
- Varjonen E, Vainio E, Kalimo K. Antigliadin IgE–indicator of wheat allergy in atopic dermatitis. Allergy. 2000 Apr;55(4):386–91. DOI: 10.1034/j.1398-9995.2000.00451.x. PMID: 10782525.
- Nosrati A, Afifi L, Danesh MJ, Lee K, Yan D, Beroukhim K, et al. Dietary modifications in atopic dermatitis: patient-reported outcomes. J Dermatolog Treat. 2017 Sep;28(6):523–38. DOI: 10.1080/09546634.2016.1278071. PMID: 28043181. PMCID: PMC5736303.
- Krysiak R, Szkróbka W, Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes. 2019 Jul;127(7):417–22. DOI: 10.1055/a-0653-7108. PMID: 30060266.
- Virili C, Bassotti G, Santaguida MG, Iuorio R, Del Duca SC, Mercuri V, et al. Atypical celiac disease as cause of increased need for thyroxine: a systematic study. J Clin Endocrinol Metab. 2012 Mar;97(3):E419-22. DOI: 10.1210/jc.2011-1851. PMID: 22238404.
- Asik M, Gunes F, Binnetoglu E, Eroglu M, Bozkurt N, Sen H, et al. Decrease in TSH levels after lactose restriction in Hashimoto’s thyroiditis patients with lactose intolerance. Endocrine. 2014 Jun;46(2):279–84. DOI: 10.1007/s12020-013-0065-1. PMID: 24078411.
- Konijeti GG, Kim N, Lewis JD, Groven S, Chandrasekaran A, Grandhe S, et al. Efficacy of the autoimmune protocol diet for inflammatory bowel disease. Inflamm Bowel Dis. 2017 Nov;23(11):2054–60. DOI: 10.1097/MIB.0000000000001221. PMID: 28858071. PMCID: PMC5647120.
- Smith E, Pauling JD. The efficacy of dietary intervention on gastrointestinal involvement in systemic sclerosis: A systematic literature review. Semin Arthritis Rheum. 2019 Aug;49(1):112–8. DOI: 10.1016/j.semarthrit.2018.12.001. PMID: 30612705.
- Zhang Y-Z, Li Y-Y. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. 2014 Jan 7;20(1):91–9. DOI: 10.3748/wjg.v20.i1.91. PMID: 24415861. PMCID: PMC3886036.
- Coates LC, FitzGerald O, Helliwell PS, Paul C. Psoriasis, psoriatic arthritis, and rheumatoid arthritis: Is all inflammation the same? Semin Arthritis Rheum. 2016 Dec;46(3):291–304. DOI: 10.1016/j.semarthrit.2016.05.012. PMID: 27388027.
- Carrizales-Sepúlveda EF, Ordaz-Farías A, Vera-Pineda R, Flores-Ramírez R. Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ. 2018 Nov;27(11):1327–34. DOI: 10.1016/j.hlc.2018.05.102. PMID: 29903685.
- Clemente JC, Manasson J, Scher JU. The role of the gut microbiome in systemic inflammatory disease. BMJ. 2018 Jan 8;360:j5145. DOI: 10.1136/bmj.j5145. PMID: 29311119. PMCID: PMC6889978.
- Shah PK, Lecis D. Inflammation in atherosclerotic cardiovascular disease. [version 1; peer review: 4 approved]. F1000Res. 2019 Aug 9;8. DOI: 10.12688/f1000research.18901.1. PMID: 31448091. PMCID: PMC6694447.
- Petersen AMW. The anti-inflammatory effect of exercise. J Appl Physiol. 2005 Apr 1;98(4):1154–62. DOI: 10.1152/japplphysiol.00164.2004. PMID: 15772055.
- Ticinesi A, Lauretani F, Tana C, Nouvenne A, Ridolo E, Meschi T. Exercise and immune system as modulators of intestinal microbiome: implications for the gut-muscle axis hypothesis. Exerc Immunol Rev. 2019;25:84–95. PMID: 30753131.
- Kessler J, Chouk M, Ruban T, Prati C, Wendling D, Verhoeven F. Psoriatic arthritis and physical activity: a systematic review. Clin Rheumatol. 2021 Nov;40(11):4379–89. DOI: 10.1007/s10067-021-05739-y. PMID: 33913069.
- Zheng Q, Sun XY, Miao X, Xu R, Ma T, Zhang YN, et al. Association between physical activity and risk of prevalent psoriasis: A MOOSE-compliant meta-analysis. Medicine (Baltimore). 2018 Jul;97(27):e11394. DOI: 10.1097/MD.0000000000011394. PMID: 29979432. PMCID: PMC6076093.
- Naldi L, Conti A, Cazzaniga S, Patrizi A, Pazzaglia M, Lanzoni A, et al. Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol. 2014 Mar;170(3):634–42. DOI: 10.1111/bjd.12735. PMID: 24641585.
- Mitropoulos A, Gumber A, Akil M, Klonizakis M. Exploring the microcirculatory effects of an exercise programme including aerobic and resistance training in people with limited cutaneous systemic sclerosis. Microvasc Res. 2019 Sep;125:103887. DOI: 10.1016/j.mvr.2019.103887. PMID: 31220505.
- Filippetti M, Cazzoletti L, Zamboni F, Ferrari P, Caimmi C, Smania N, et al. Effect of a tailored home-based exercise program in patients with systemic sclerosis: A randomized controlled trial. Scand J Med Sci Sports. 2020 Sep;30(9):1675–84. DOI: 10.1111/sms.13702. PMID: 32350931. PMCID: PMC7496851.
- Minali PA, Pimentel C, de Mello MT, Lima G, Dardin LP, Garcia A, et al. Effectiveness of resistance exercise in functional fitness in women with primary Sjögren’s syndrome: randomized clinical trial. Scand J Rheumatol. 2020 Jan;49(1):47–56. DOI: 10.1080/03009742.2019.1602880. PMID: 31244376.
- Alexanderson H, Boström C. Exercise therapy in patients with idiopathic inflammatory myopathies and systemic lupus erythematosus – A systematic literature review. Best Pract Res Clin Rheumatol. 2020 Apr;34(2):101547. DOI: 10.1016/j.berh.2020.101547. PMID: 32819833.
- Luthold RV, Fernandes GR, Franco-de-Moraes AC, Folchetti LGD, Ferreira SRG. Gut microbiota interactions with the immunomodulatory role of vitamin D in normal individuals. Metab Clin Exp. 2017 Apr;69:76–86. DOI: 10.1016/j.metabol.2017.01.007. PMID: 28285654.
- Abbasnezhad A, Amani R, Hajiani E, Alavinejad P, Cheraghian B, Ghadiri A. Effect of vitamin D on gastrointestinal symptoms and health-related quality of life in irritable bowel syndrome patients: a randomized double-blind clinical trial. Neurogastroenterol Motil. 2016 Oct;28(10):1533–44. DOI: 10.1111/nmo.12851. PMID: 27154424.
- López-Muñoz P, Beltrán B, Sáez-González E, Alba A, Nos P, Iborra M. Influence of vitamin D deficiency on inflammatory markers and clinical disease activity in IBD patients. Nutrients. 2019 May 11;11(5). DOI: 10.3390/nu11051059. PMID: 31083541. PMCID: PMC6567866.
- Maguire LH, Song M, Strate LL, Giovannucci EL, Chan AT. Association of geographic and seasonal variation with diverticulitis admissions. JAMA Surg. 2015 Jan;150(1):74–7. DOI: 10.1001/jamasurg.2014.2049. PMID: 25409019. PMCID: PMC4504233.
- Liu Y, Li J, Liang G, Cheng C, Li Y, Wu X. Association of Alopecia Areata with Vitamin D and Calcium Levels: A Systematic Review and Meta-analysis. Dermatol Ther (Heidelb). 2020 Oct;10(5):967–83. DOI: 10.1007/s13555-020-00433-4. PMID: 32772238. PMCID: PMC7477029.
- Søyland E, Heier I, Rodríguez-Gallego C, Mollnes TE, Johansen FE, Holven KB, et al. Sun exposure induces rapid immunological changes in skin and peripheral blood in patients with psoriasis. Br J Dermatol. 2011 Feb;164(2):344–55. DOI: 10.1111/j.1365-2133.2010.10149.x. PMID: 21271993.
- Peinemann F, Harari M, Peternel S, Chan T, Chan D, Labeit AM, et al. Indoor salt water baths followed by artificial ultraviolet B light for chronic plaque psoriasis. Cochrane Database Syst Rev. 2020 May 5;5:CD011941. DOI: 10.1002/14651858.CD011941.pub2. PMID: 32368795. PMCID: PMC7199317.
- Qataya PO, Elsayed NM, Elguindy NM, Ahmed Hafiz M, Samy WM. Selenium: A sole treatment for erosive oral lichen planus (Randomized controlled clinical trial). Oral Dis. 2020 May;26(4):789–804. DOI: 10.1111/odi.13285. PMID: 31975475.
- Luo Y, Zhang Y, Kuai L, Xing M, Ru Y, Luo Y, et al. Efficacy and safety of Tripterygium glycosides in Sjögren’s syndrome treatment: evidence from 12 randomized controlled trials. Ann Palliat Med. 2021 Jul 5;10(7):8215–31. DOI: 10.21037/apm-21-256. PMID: 34263629.
- Yargholi A, Shirbeigi L, Rahimi R, Mansouri P, Ayati MH. The effect of Melissa officinalis syrup on patients with mild to moderate psoriasis: a randomized, double-blind placebo-controlled clinical trial. BMC Res Notes. 2021 Jun 30;14(1):253. DOI: 10.1186/s13104-021-05667-9. PMID: 34193264. PMCID: PMC8246655.
- Kragsnaes MS, Kjeldsen J, Horn HC, Munk HL, Pedersen JK, Just SA, et al. Safety and efficacy of faecal microbiota transplantation for active peripheral psoriatic arthritis: an exploratory randomised placebo-controlled trial. Ann Rheum Dis. 2021 Sep;80(9):1158–67. DOI: 10.1136/annrheumdis-2020-219511. PMID: 33926922.
- Toribio-Mateas M. Harnessing the power of microbiome assessment tools as part of neuroprotective nutrition and lifestyle medicine interventions. Microorganisms. 2018 Apr 25;6(2). DOI: 10.3390/microorganisms6020035. PMID: 29693607. PMCID: PMC6027349.
- Stenman LK, Lehtinen MJ, Meland N, Christensen JE, Yeung N, Saarinen MT, et al. Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults-Randomized Controlled Trial. EBioMedicine. 2016 Nov;13:190–200. DOI: 10.1016/j.ebiom.2016.10.036. PMID: 27810310. PMCID: PMC5264483.
- Frei R, Akdis M, O’Mahony L. Prebiotics, probiotics, synbiotics, and the immune system: experimental data and clinical evidence. Curr Opin Gastroenterol. 2015 Mar;31(2):153–8. DOI: 10.1097/MOG.0000000000000151. PMID: 25594887.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106–13. DOI: 10.2174/1389200219666180813144834. PMID: 30101706. PMCID: PMC6340155.
- Mujagic Z, de Vos P, Boekschoten MV, Govers C, Pieters H-JHM, de Wit NJW, et al. The effects of Lactobacillus plantarum on small intestinal barrier function and mucosal gene transcription; a randomized double-blind placebo controlled trial. Sci Rep. 2017 Jan 3;7:40128. DOI: 10.1038/srep40128. PMID: 28045137. PMCID: PMC5206730.
- Sindhu KNC, Sowmyanarayanan TV, Paul A, Babji S, Ajjampur SSR, Priyadarshini S, et al. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014 Apr;58(8):1107–15. DOI: 10.1093/cid/ciu065. PMID: 24501384. PMCID: PMC3967829.
- Lamprecht M, Bogner S, Schippinger G, Steinbauer K, Fankhauser F, Hallstroem S, et al. Probiotic supplementation affects markers of intestinal barrier, oxidation, and inflammation in trained men; a randomized, double-blinded, placebo-controlled trial. J Int Soc Sports Nutr. 2012 Sep 20;9(1):45. DOI: 10.1186/1550-2783-9-45. PMID: 22992437. PMCID: PMC3465223.
- Navarro-López V, Martínez-Andrés A, Ramírez-Boscá A, Ruzafa-Costas B, Núñez-Delegido E, Carrión-Gutiérrez MA, et al. Efficacy and Safety of Oral Administration of a Mixture of Probiotic Strains in Patients with Psoriasis: A Randomized Controlled Clinical Trial. Acta Derm Venereol. 2019 Nov 1;99(12):1078–84. DOI: 10.2340/00015555-3305. PMID: 31453631.
- Marighela TF, Arismendi MI, Marvulle V, Brunialti MKC, Salomão R, Kayser C. Effect of probiotics on gastrointestinal symptoms and immune parameters in systemic sclerosis: a randomized placebo-controlled trial. Rheumatology (Oxford). 2019 Nov 1;58(11):1985–90. DOI: 10.1093/rheumatology/kez160. PMID: 31056685.
- Knackstedt R, Knackstedt T, Gatherwright J. The role of topical probiotics in skin conditions: A systematic review of animal and human studies and implications for future therapies. Exp Dermatol. 2020 Jan;29(1):15–21. DOI: 10.1111/exd.14032. PMID: 31494971.




Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!