Brain Fog: A Research-Based Guide to Restoring Mental Clarity
Brain Fog May Be a Sign That You Need to Improve Your Gut Health
- What Is Brain Fog|
- Patient Challenges|
- What Causes Brain Fog|
- Brain Fog and Alzheimer’s|
- What to Do About Brain Fog|
- The Bottom Line|
- Recommended Products|
Download this Episode (right click link and ‘Save As’)
Life is demanding enough without the extra challenge of brain fog. When you can’t think clearly, can’t focus, can’t find the right word, and constantly forget why you walked into the kitchen, even simple tasks can seem difficult. Plus brain fog leaves you feeling mentally exhausted. I know this because I’ve struggled with brain fog myself.
Brain fog is a symptom that we see and treat often in the clinic. And the good news is most patients resolve their brain fog quickly with improved gut health. That’s because even the simplest steps towards better gut health result in less systemic inflammation, less brain inflammation, and, as a result, less brain fog.
In this article, we’ll look at what the research tells us about the causes of brain fog and what you can do to regain your mental clarity.
What Is Brain Fog?
Brain fog is a very common symptom characterized by slowed or cloudy thinking, forgetfulness, inability to focus, mental fatigue, and poor mental stamina [1]. Brain fog is not associated with any physical abnormalities in the brain [2].

The symptoms of brain fog are found in a wide array of seemingly-unrelated medical conditions and have been reported in patients with:
- Crohn’s disease [3]
- SIBO and IBS [4, 5]
- Celiac disease [6]
- Non-celiac gluten sensitivity [7, 8]
- Hypothyroidism [9, 10]
- Chronic fatigue syndrome [11]
- Fibromyalgia [12]
- Postural orthostatic tachycardia syndrome (POTS) [13]
- Mast cell disorders [14]
- Obesity [15]
- Menopause [16]
- Multiple sclerosis [17]
- Rheumatoid arthritis [18]
- Lupus [2]
Brain fog is also common after chemotherapy treatments and may be called “chemo fog” or “chemo brain” [19]. Recently, chronic brain fog has also been linked to the coronavirus pandemic as one symptom experienced by “COVID long-haulers,” those who recover from a COVID-19 viral infection but continue to have debilitating symptoms [20].
The Challenge for Patients With Brain Fog

Patients looking for medical advice on how to relieve brain fog may feel like their concerns are not taken seriously.
Despite being common and debilitating, brain fog doesn’t always get the attention it deserves. There’s no test or standard treatment for brain fog and there’s little research conducted specifically about brain fog. According to one group of researchers who studied brain fog in celiac patients [6]:
“These mild degradations of cognitive functions, referred to as “brain fog,” are yet to be formally recognized as a medical or psychological condition.”
Because it’s associated with so many other conditions, healthcare practitioners may assume that brain fog is caused by menopause, autoimmune diseases, or one of many other conditions, and conclude that nothing can be done.
But all of this ignores the true mechanisms behind brain fog, which can be addressed and resolved. Let’s take a closer look.
What Causes Brain Fog?
Current research suggests that inflammation in the brain, also known as neuroinflammation, is one of the primary reasons for brain fog [15, 21, 22].
In one small study, researchers gave 20 healthy subjects a variety of cognitive tests, both before and after short-term brain inflammation was induced. The result? A greater cognitive effort was required when subjects were experiencing acute brain inflammation [23].
Inflammation is the immune system’s natural response to protect your body from harmful toxins, bacteria, viruses, and other pathogens. Your brain has its own, separate immune system and extra safeguards to protect this essential organ:
- The blood-brain barrier is regulated by the central nervous system and filters out toxins in the blood, preventing them from circulating in the brain [24].
- Microglial cells are immune cells that are unique to the brain and central nervous system. When these cells sense the presence of harmful substances, they become activated to protect brain cells. However, they can also become over-activated, causing excessive inflammation in the brain.
Brain fog may occur when toxic substances cross the blood-brain barrier, triggering the brain’s immune system and causing inflammation. A number of underlying conditions can drive this process. Let’s explore a few of them.
Gut Imbalances and Leaky Gut
Research recognizes that imbalances in the gut ecosystem can alter brain function by producing neuroinflammation [25, 26, 27, 8, 9]. Here’s how a gut condition can lead to inflammation in your brain:
- When bad microorganisms crowd out the healthy bacteria in your gut, your immune system activates to defend your digestive tract from these invaders.
- This immune response creates inflammation in the intestinal tract.
- Over time, chronically inflamed intestines become damaged and more permeable, leading to a condition known as “leaky gut.”
- A leaky gut allows bacteria, undigested food particles and other toxins to enter the bloodstream.
- Toxins in your bloodstream can migrate across the blood-brain barrier, where they become neurotoxins.
- Neurotoxins create inflammation in the brain, leading to brain fog, poor mood, and other neuropsychological symptoms.
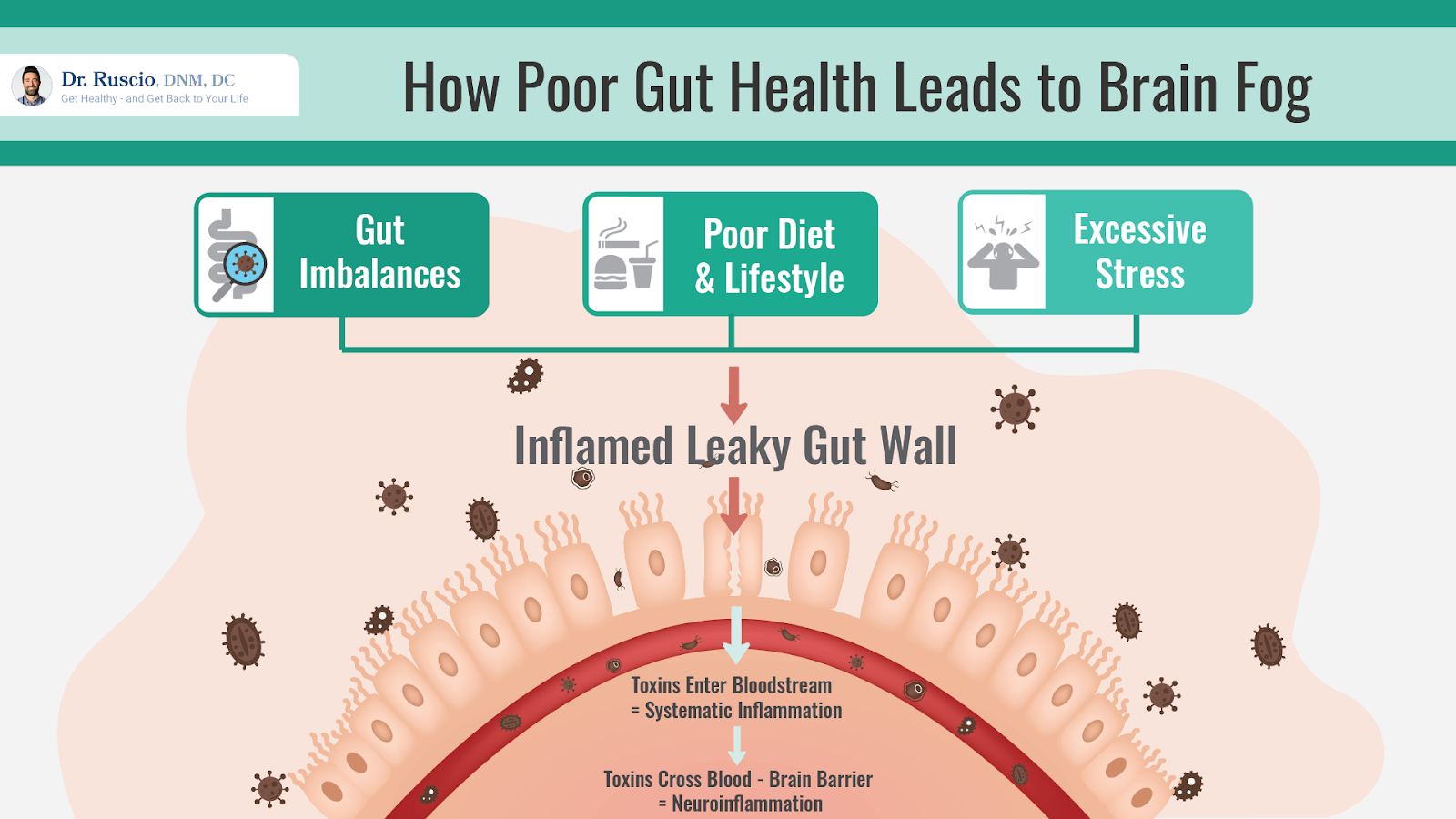
Research shows that brain fog is associated with many gut health conditions, including IBS and SIBO [4, 5], Crohn’s disease [3], celiac disease [6], and non-celiac gluten sensitivity [7, 8]. All of these conditions involve imbalances in the gut ecosystem.
Other conditions that are associated with brain fog include hypothyroidism, chronic fatigue syndrome, fibromyalgia, obesity, difficult menopause transition, and rheumatoid arthritis. In many cases, these conditions also involve imbalances in the gut. This suggests that brain fog may not be caused by these health conditions and instead may share the same underlying mechanism: poor gut health.
Gut Imbalances and Liver Dysfunction
Hepatic encephalopathy (HE) is a loss of brain function observed in people with liver disorders. HE can be severe in patients with serious liver disease, resulting in confusion, personality changes, and even coma. However, a milder form of HE, called minimal hepatic encephalopathy (MHE), can be easily recognized as brain fog.
The job of the liver is to filter toxins from the blood. When the liver is diseased, it can’t fully perform this function, leading to more toxins in the bloodstream which can cross the blood-brain barrier and cause neuroinflammation.
Recent research suggests a connection between MHE and SIBO (small intestine bacterial overgrowth).
Three studies found high rates of SIBO in patients with liver cirrhosis (scarring of liver tissue resulting from chronic liver inflammation) [28, 29, 30]. SIBO rates were higher (88.9% and 55.9%) among cirrhosis patients with MHE. However, a fourth study did not find any indication of SIBO among cirrhosis patients [31].
Additional studies show that rifaximin (an antibiotic used to treat SIBO) significantly improved symptoms of MHE in patients with both liver disease and SIBO [30, 32, 33]. In one of these studies, two groups of cirrhosis patients were treated for different gut imbalances [30]. Patients treated for SIBO showed significant improvement in MHE symptoms. Those treated for H. Pylori did not experience significant improvements.
One group of researchers suggest that “an altered balance of gut microflora might also be involved in HE [34],” suggesting a possible gut-liver-brain connection. It appears that SIBO may play a significant role here.
Histamine Intolerance and Mast Cell Disorders
Mast cells and histamine are key players in your body’s immune function.
Mast cells are a specific kind of white blood cell that produces histamine and can trigger inflammation in the body and brain. In some cases, mast cells are triggered too often or without appropriate cause, leading to excess histamine levels and inflammation.
Histamine is known for its role in allergic reactions and is the reason you may occasionally take anti-histamine medication. Histamine also acts as a neurotransmitter in the brain and speeds up communications between brain cells. Appropriate levels of histamine help with alertness, learning, and motivation. Excess histamine, however, may contribute to cognitive impairment [15].
Histamine intolerance is a condition of excess histamine in the body. It’s known to produce allergy-like symptoms, such as rashes, hives, racing heart, and joint pain.
Levels of histamine in the brain can increase as a result of an overactive immune system and mast cell response as well as the intake of foods that contain histamine. Mast cell disorders and histamine intolerance are both known to cause brain fog [21, 15].
Food Sensitivities
Food sensitivities may also trigger inflammation that leads to brain fog.
For example, brain fog is common in those with celiac disease and non-celiac gluten sensitivity [6, 7, 8]. In both of these conditions, gluten consumption triggers an immune response that creates inflammation in the gut. The process that leads to brain fog unfolds in the same way as with gut imbalances.
One study showed that brain fog resolved in untreated celiac patients after 12 months on a gluten-free diet [6].
Exposure to Toxins
Exposure to other types of toxins is also linked to brain fog. This includes chemotherapy drugs [19] and airborne molds [35]. In these examples, toxins enter the bloodstream through different routes (through IV infusion or by inhaling mycotoxins into the lungs). It seems likely that these toxins also cross the blood-brain-barrier and create inflammation in the brain.
Can Brain Fog Lead to More Serious Cognitive Dysfunction?

Brain fog is a sign that all is not well with your brain health and your overall health.
Chronic brain inflammation is one of the key factors associated with the development of Alzheimer’s disease. Research suggests that this process starts decades before severe memory loss becomes apparent [36, 37]. Neuroinflammation is also involved with the development of neurodegenerative diseases like MS and ALS.
While there’s no specific evidence that directly links brain fog to the development of more serious cognitive conditions, the evidence is clear that chronic neuroinflammation carries significant risks for brain health in the long term.
What To Do About Brain Fog
In the clinic, the steps we take to improve gut health and reduce inflammation help patients clear up brain fog. For many patients, brain fog starts to lift once they work on improving their diet and lifestyle.
While supplements can be helpful to reduce inflammation, the most important approaches address the sources of inflammation. Poor diet, too much stress, lack of exercise, and lack of sleep are the big culprits here.
A standard American diet (high in sugar, carbohydrates, unhealthy fats, and processed foods) tends to feed bad bacteria in the gut, initiating the process that leads to neuroinflammation.
An anti-inflammatory diet, such as the Paleo diet, can be very helpful for reducing brain fog. Anti-inflammatory diets focus on fresh, whole foods instead of processed foods. Including sources of omega 3 fatty acids, such as sardines, mackerel, and salmon, was found to be especially helpful for reducing brain fog in patients undergoing chemotherapy [38].
Probiotics can be very helpful for rebalancing the gut ecosystem and preventing inflammatory neurodegeneration [39]. Probiotics have been shown to improve cognition in patients with IBS [40, 41], Fibromyalgia [42], and Alzheimer’s [43, 44].
Other supplements that may help to reduce your overall inflammation are curcumin, fish oil, and resveratrol. Luteolin supplements may also help reduce brain fog [15].
Lifestyle changes that can be very helpful include:
- Getting 7-9 hours of sleep every night
- Getting regular physical activity, such as walking for 30 minutes a day
- Reducing and managing stress as much as possible
While most people will experience considerable improvement with these fundamental steps, some may require further support to identify and treat specific root causes, including:
- Identifying specific food triggers, such as gluten, FODMAPs, or high-histamine foods
- Treating a gut infection, such as SIBO
- Getting blood work to test thyroid hormone levels
For more detailed information about resolving brain fog, see our detailed guide.
If basic dietary and lifestyle changes, combined with probiotics aren’t enough to eliminate your brain fog, our experienced clinical team can help you develop a personalized treatment approach.
The Bottom Line
Brain fog is a distressing symptom that can significantly impact your day-to-day life. It’s important to recognize this cognitive problem as a sign of neuroinflammation and to take steps to improve your brain function and overall wellness.
Common causes of brain fog include gut imbalances, leaky gut, liver dysfunction, SIBO, histamine intolerance, food sensitivities, and exposure to toxins.
For many who struggle with brain fog, basic dietary and lifestyle changes can help to resolve these issues. Others may need to dig a bit deeper to identify and treat the root causes of mild cognitive dysfunction. Your brain health is important. Take steps to improve your mental clarity today.
The Ruscio Institute has developed a range of high quality formulations to help our patients and audience. If you’re interested in learning more about these products, please click here. Note that there are many other options available, and we encourage you to research which products may be right for you.
Sponsored Resources
Hi, everyone. Just a few fairly important updates. I’ve been working diligently behind the scenes tweaking and updating our paperwork, our clinical systems, our treatments, our data gathering, data organization, reporting, and patient monitoring. I’ve refined the algorithm to be even better than it was before.
And how confident am I in our clinical team? Well, my mother is working with our health coach and my father just started working with one of our doctors. So about as confident as you can get. Collectively, we are moving towards our goal of reforming functional medicine. We are gathering data on our patients and working toward publishing our data. We have taken big steps in this direction. So you are part of something big here. You’re not only a patient we aim to serve and help, but also as one of our patients, you become an example of how people can improve their health in less time and for less money compared to what appears to be commonplace in the functional medicine field. So I encourage you to look forward not only to potentially working with me, but also with any of our tremendously skilled, attentive and empathetic clinicians.
And so thank you for being a part of it or thank you for waiting to be a part of it, if you’re about to be seen soon. And if you have not yet reached out and you’re in need of help, we would be pleased and honored to work with you.
Hey there, Erin here from the Dr. Ruscio team. Can I tell you how excited I am that our brand new three in one probiotic formula is now available on our website store. It’s an easy to use powder stick format.
So I’ve been taking Dr. Ruscio’s recommended three for balanced probiotic for two years. Now I seem to take my soil-based probiotic just fine, because it’s right there next to my other supplements. But man, am I lazy about taking all three each day? The barrier for me is literally just walking over to the fridge and uncapping the other two bottles. I know it’s not hard, but that’s how busy and distracted life can be I guess.
With this three in one formula, you mix one stick with your favorite cold beverage, one to two times per day. It’s tasteless, so it won’t ruin your favorite drink. Take it with, or without food. It’s really useful as a part of your gut support and healing program and it can be used for ongoing immune and gut health maintenance. No pills, just poor mix and drink. Visit store.drruscio.com and order now.
➕ References
- Ocon AJ. Caught in the thickness of brain fog: exploring the cognitive symptoms of Chronic Fatigue Syndrome. Front Physiol. 2013 Apr 5;4:63. doi: 10.3389/fphys.2013.00063. PMID: 23576989; PMCID: PMC3617392.
- Lynall M. Neuropsychiatric symptoms in lupus. Lupus. 2018 Oct;27(1_suppl):18-20. doi: 10.1177/0961203318801672. PMID: 30452327.
- van Langenberg DR, Yelland GW, Robinson SR, Gibson PR. Cognitive impairment in Crohn’s disease is associated with systemic inflammation, symptom burden and sleep disturbance. United European Gastroenterol J. 2017 Jun;5(4):579-587. doi: 10.1177/2050640616663397. Epub 2016 Aug 8. PMID: 28588890; PMCID: PMC5446137.
- Rao SSC, Rehman A, Yu S, Andino NM. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018 Jun 19;9(6):162. doi: 10.1038/s41424-018-0030-7. PMID: 29915215; PMCID: PMC6006167.
- Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020 Jul 10;11:664. doi: 10.3389/fpsyt.2020.00664. PMID: 32754068; PMCID: PMC7366247.
- Yelland GW. Gluten-induced cognitive impairment (“brain fog”) in coeliac disease. J Gastroenterol Hepatol. 2017 Mar;32 Suppl 1:90-93. doi: 10.1111/jgh.13706. PMID: 28244662.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR; Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12:85. doi: 10.1186/1741-7015-12-85. PMID: 24885375; PMCID: PMC4053283.
- Isasi C, Tejerina E, Morán LM. Non-celiac gluten sensitivity and rheumatic diseases. Reumatol Clin. 2016 Jan-Feb;12(1):4-10. English, Spanish. doi: 10.1016/j.reuma.2015.03.001. Epub 2015 May 5. PMID: 25956352.
- Pasqualetti G, Pagano G, Rengo G, Ferrara N, Monzani F. Subclinical Hypothyroidism and Cognitive Impairment: Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2015 Nov;100(11):4240-8. doi: 10.1210/jc.2015-2046. Epub 2015 Aug 25. PMID: 26305618.
- Samuels MH. Psychiatric and cognitive manifestations of hypothyroidism. Curr Opin Endocrinol Diabetes Obes. 2014 Oct;21(5):377-83. doi: 10.1097/MED.0000000000000089. PMID: 25122491; PMCID: PMC4264616.
- Ocon AJ. Caught in the thickness of brain fog: exploring the cognitive symptoms of Chronic Fatigue Syndrome. Front Physiol. 2013 Apr 5;4:63. doi: 10.3389/fphys.2013.00063. PMID: 23576989; PMCID: PMC3617392.
- Galvez-Sánchez CM, Reyes Del Paso GA, Duschek S. Cognitive Impairments in Fibromyalgia Syndrome: Associations With Positive and Negative Affect, Alexithymia, Pain Catastrophizing and Self-Esteem. Front Psychol. 2018 Mar 22;9:377. doi: 10.3389/fpsyg.2018.00377. PMID: 29623059; PMCID: PMC5874325.
- Ross AJ, Medow MS, Rowe PC, Stewart JM. What is brain fog? An evaluation of the symptom in postural tachycardia syndrome. Clin Auton Res. 2013 Dec;23(6):305-11. doi: 10.1007/s10286-013-0212-z. Epub 2013 Sep 3. PMID: 23999934; PMCID: PMC3896080.
- Moura DS, Sultan S, Georgin-Lavialle S, Barete S, Lortholary O, Gaillard R, Hermine O. Evidence for cognitive impairment in mastocytosis: prevalence, features and correlations to depression. PLoS One. 2012;7(6):e39468. doi: 10.1371/journal.pone.0039468. Epub 2012 Jun 20. PMID: 22745762; PMCID: PMC3379977.
- Theoharides TC, Stewart JM, Hatziagelaki E, Kolaitis G. Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015 Jul 3;9:225. doi: 10.3389/fnins.2015.00225. PMID: 26190965; PMCID: PMC4490655.
- Gava G, Orsili I, Alvisi S, Mancini I, Seracchioli R, Meriggiola MC. Cognition, Mood and Sleep in Menopausal Transition: The Role of Menopause Hormone Therapy. Medicina (Kaunas). 2019 Oct 1;55(10):668. doi: 10.3390/medicina55100668. PMID: 31581598; PMCID: PMC6843314.
- Jongen PJ, Ter Horst AT, Brands AM. Cognitive impairment in multiple sclerosis. Minerva Med. 2012 Apr;103(2):73-96. PMID: 22513513.
- Meade T, Manolios N, Cumming SR, Conaghan PG, Katz P. Cognitive Impairment in Rheumatoid Arthritis: A Systematic Review. Arthritis Care Res (Hoboken). 2018 Jan;70(1):39-52. doi: 10.1002/acr.23243. PMID: 28371512.
- Kovalchuk A, Kolb B. Chemo brain: From discerning mechanisms to lifting the brain fog-An aging connection. Cell Cycle. 2017 Jul 18;16(14):1345-1349. doi: 10.1080/15384101.2017.1334022. Epub 2017 Jun 28. PMID: 28657421; PMCID: PMC5539816.
- Belluck, P. (2020, October 11). ‘I feel Like I Have DEMENTIA’: Brain fog PLAGUES COVID SURVIVORS. https://www.nytimes.com/2020/10/11/health/covid-survivors.html
- Conti P, D’Ovidio C, Conti C, Gallenga CE, Lauritano D, Caraffa A, Kritas SK, Ronconi G. Progression in migraine: Role of mast cells and pro-inflammatory and anti-inflammatory cytokines. Eur J Pharmacol. 2019 Feb 5;844:87-94. doi: 10.1016/j.ejphar.2018.12.004. Epub 2018 Dec 6. PMID: 30529470.
- Jones KA, Thomsen C. The role of the innate immune system in psychiatric disorders. Mol Cell Neurosci. 2013 Mar;53:52-62. doi: 10.1016/j.mcn.2012.10.002. Epub 2012 Oct 12. PMID: 23064447.
- Balter LJ, Bosch JA, Aldred S, Drayson MT, Veldhuijzen van Zanten JJ, Higgs S, Raymond JE, Mazaheri A. Selective effects of acute low-grade inflammation on human visual attention. Neuroimage. 2019 Nov 15;202:116098. doi: 10.1016/j.neuroimage.2019.116098. Epub 2019 Aug 12. PMID: 31415883.
- Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol. 2015 Jan 5;7(1):a020412. doi: 10.1101/cshperspect.a020412. PMID: 25561720; PMCID: PMC4292164.
- Dopkins N, Nagarkatti PS, Nagarkatti M. The role of gut microbiome and associated metabolome in the regulation of neuroinflammation in multiple sclerosis and its implications in attenuating chronic inflammation in other inflammatory and autoimmune disorders. Immunology. 2018 Jun;154(2):178-185. doi: 10.1111/imm.12903. Epub 2018 Feb 27. PMID: 29392733; PMCID: PMC5980216.
- Sun MF, Shen YQ. Dysbiosis of gut microbiota and microbial metabolites in Parkinson’s Disease. Ageing Res Rev. 2018 Aug;45:53-61. doi: 10.1016/j.arr.2018.04.004. Epub 2018 Apr 26. PMID: 29705121.
- Lin L, Zheng LJ, Zhang LJ. Neuroinflammation, Gut Microbiome, and Alzheimer’s Disease. Mol Neurobiol. 2018 Nov;55(11):8243-8250. doi: 10.1007/s12035-018-0983-2. Epub 2018 Mar 9. PMID: 29524051.
- Jun DW, Kim KT, Lee OY, Chae JD, Son BK, Kim SH, Jo YJ, Park YS. Association between small intestinal bacterial overgrowth and peripheral bacterial DNA in cirrhotic patients. Dig Dis Sci. 2010 May;55(5):1465-71. doi: 10.1007/s10620-009-0870-9. Epub 2009 Jun 11. PMID: 19517230.
- Gupta A, Dhiman RK, Kumari S, Rana S, Agarwal R, Duseja A, Chawla Y. Role of small intestinal bacterial overgrowth and delayed gastrointestinal transit time in cirrhotic patients with minimal hepatic encephalopathy. J Hepatol. 2010 Nov;53(5):849-55. doi: 10.1016/j.jhep.2010.05.017. Epub 2010 Jul 17. PMID: 20675008.
- Abid S, Kamran M, Abid A, Butt N, Awan S, Abbas Z. Minimal Hepatic Encephalopathy: Effect of H. pylori infection and small intestinal bacterial overgrowth treatment on clinical outcomes. Sci Rep. 2020 Jun 22;10(1):10079. doi: 10.1038/s41598-020-67171-7. PMID: 32572109; PMCID: PMC7308324.
- Schulz C, Schütte K, Reisener N, Voss J, Kandulski A, Malfertheiner P. Small Intestinal Bacterial Overgrowth is not Associated with Minimal Hepatic Encephalopathy in Patients with Liver Cirrhosis. J Gastroenterol Hepatol Endosc. 2016; 1(1): 1001.
- Zhang Y, Feng Y, Cao B, Tian Q. Effects of SIBO and rifaximin therapy on MHE caused by hepatic cirrhosis. Int J Clin Exp Med. 2015 Feb 15;8(2):2954-7. PMID: 25932262; PMCID: PMC4402909.
- Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, Sigal S, Sheikh MY, Beavers K, Frederick T, Teperman L, Hillebrand D, Huang S, Merchant K, Shaw A, Bortey E, Forbes WP. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010 Mar 25;362(12):1071-81. doi: 10.1056/NEJMoa0907893. PMID: 20335583.
- Losurdo G, Salvatore D’Abramo F, Indellicati G, Lillo C, Ierardi E, Di Leo A. The Influence of Small Intestinal Bacterial Overgrowth in Digestive and Extra-Intestinal Disorders. Int J Mol Sci. 2020 May 16;21(10):3531. doi: 10.3390/ijms21103531. PMID: 32429454; PMCID: PMC7279035.
- Crago BR, Gray MR, Nelson LA, Davis M, Arnold L, Thrasher JD. Psychological, neuropsychological, and electrocortical effects of mixed mold exposure. Arch Environ Health. 2003 Aug;58(8):452-63. doi: 10.3200/AEOH.58.8.452-463. PMID: 15259424.
- Hodges JR, Erzinçlioğlu S, Patterson K. Evolution of cognitive deficits and conversion to dementia in patients with mild cognitive impairment: a very-long-term follow-up study. Dement Geriatr Cogn Disord. 2006;21(5-6):380-91. doi: 10.1159/000092534. Epub 2006 Apr 4. PMID: 16601329.
- Jonker C, Comijs HC. Lichte cognitieve stoornissen (MCI): Prodromen van dementie? [Mild cognitive impairment: a prodromal phase of dementia?]. Tijdschr Gerontol Geriatr. 2007 Jul;38(3):115-21. Dutch. PMID: 17642317.
- Orchard TS, Gaudier-Diaz MM, Weinhold KR, Courtney DeVries A. Clearing the fog: a review of the effects of dietary omega-3 fatty acids and added sugars on chemotherapy-induced cognitive deficits. Breast Cancer Res Treat. 2017 Feb;161(3):391-398. doi: 10.1007/s10549-016-4073-8. Epub 2016 Dec 8. PMID: 27933449; PMCID: PMC5526680.
- Alexandrov P, Zhai Y, Li W, Lukiw W. Lipopolysaccharide-stimulated, NF-kB-, miRNA-146a- and miRNA-155-mediated molecular-genetic communication between the human gastrointestinal tract microbiome and the brain. Folia Neuropathol. 2019;57(3):211-219. doi: 10.5114/fn.2019.88449. PMID: 31588707.
- Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014 May 28;20(20):6024-30. doi: 10.3748/wjg.v20.i20.6024. PMID: 24876725; PMCID: PMC4033442.
- Frändemark Å, Jakobsson Ung E, Törnblom H, Simrén M, Jakobsson S. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil. 2017 Jan;29(1). doi: 10.1111/nmo.12898. Epub 2016 Jul 11. PMID: 27401139.
- Roman, P., Estévez, A.F., Miras, A. et al. A Pilot Randomized Controlled Trial to Explore Cognitive and Emotional Effects of Probiotics in Fibromyalgia. Sci Rep 8, 10965 (2018). https://doi.org/10.1038/s41598-018-29388-5
- Akbari E, Asemi Z, Daneshvar Kakhaki R, Bahmani F, Kouchaki E, Tamtaji OR, Hamidi GA, Salami M. Effect of Probiotic Supplementation on Cognitive Function and Metabolic Status in Alzheimer’s Disease: A Randomized, Double-Blind and Controlled Trial. Front Aging Neurosci. 2016 Nov 10;8:256. doi: 10.3389/fnagi.2016.00256. PMID: 27891089; PMCID: PMC5105117.
- Tamtaji OR, Heidari-Soureshjani R, Mirhosseini N, Kouchaki E, Bahmani F, Aghadavod E, Tajabadi-Ebrahimi M, Asemi Z. Probiotic and selenium co-supplementation, and the effects on clinical, metabolic and genetic status in Alzheimer’s disease: A randomized, double-blind, controlled trial. Clin Nutr. 2019 Dec;38(6):2569-2575. doi: 10.1016/j.clnu.2018.11.034. Epub 2018 Dec 10. PMID: 30642737.





Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!