What Are the Symptoms of an Unhealthy Gut? Signs To Look For
Poor Gut Health Affects Your Mood, Energy, Brain, Hormones, Skin, and More
- Meet Your Microbiota|
- Symptoms of Unhealthy Gut|
- Why Is Poor Gut Health Common|
- How To Get Your Gut Health Back on Track|
- Your Gut Holds the Key|

Your gut health has a tremendous impact on your overall health. If you think that digestive symptoms are the only signs of an unhealthy gut, you are only partially right. Your gut health also affects your mood, energy, brain function, hormonal health, immune health, skin health, and much more. In fact, some people with gut problems don’t have obvious digestive issues. Instead, they struggle with symptoms and conditions that most people don’t associate with gut health.
In this article, we’ll help you explore if your health symptoms and conditions may be connected to your digestive system. Then, we’ll explain the fundamental steps you can take for a healthy gut and better overall health.
Meet Your Microbiota
Problems in the gut, and many symptoms outside the gut have their root in an unhealthy microbiota, the community of microorganisms that live in your digestive tract. Your microbiota (sometimes called a microbiome) is a complex ecosystem that science is only beginning to understand.
What we do know is that your digestive tract contains roughly a thousand different species of bacteria. We live in symbiosis with these living microorganisms, meaning it’s a win-win relationship. They help us with important bodily processes, and we provide them with food and shelter. However, when bad bacteria take over, a parasitic relationship develops. In this case, bacteria thrive, but you don’t.
Changes in the microbiota have been observed in a vast array of diseases, health conditions, and symptoms. There are a few different changes in the microbiota that can affect your health:
- Reduced diversity in the species of microorganisms
- Imbalance of good and bad bacteria
- Infection where bad bacteria take over
- Bacterial overgrowth — when normal bacteria grows where it shouldn’t
What Are the Symptoms of an Unhealthy Gut?



Unhealthy changes in your gut microbiota can have far-reaching effects on your health by causing inflammation, immune dysregulations, and poor nutrient absorption. These changes can cause a wide array of symptoms. Let’s take a closer look.
Inflammation—Signs and Symptoms
For many people, the digestive tract is the leading cause of inflammation in the body. When your gut microbiota is unbalanced, it becomes inflamed. This can cause inflammation throughout your entire body and lead to a wide variety of symptoms, including:
- Fatigue: Inflammation causes fatigue by creating imbalances in stress hormones. Sometimes called adrenal fatigue or chronic fatigue, the root cause is usually in the gut. Research shows that fatigue is extremely common in patients with IBS [1, 2], non-celiac gluten sensitivity [3], leaky gut [4], and people with gastrointestinal complaints [5].
- Depression or anxiety: When inflammation from the gut travels to the brain, it can alter your neurotransmitters, like serotonin that affect your mood. Research connects poor mental health (anger, irritability, tension, depression, and anxiety) to IBS [6, 7, 8], IBD [9], and non-celiac gluten sensitivity [10, 11].
- Brain fog: Inflammation in the brain can also cause brain fog [12, 13], characterized by slowed thinking, forgetfulness, inability to focus, and poor mental stamina [14]. Even worse, chronic brain inflammation over decades of life can lead to Alzheimer’s disease [15].
- Insomnia: Inflammation in the digestive tract can affect your body’s sleep/wake cycle and can lead to insomnia [16].
- Skin problems: Your skin health is a reflection of your gut health, and research supports this connection [17, 18, 19]. Skin issues related to gut health include acne [20], eczema [21, 22, 23], psoriasis [24, 25], and other autoimmune skin conditions.
- Female hormone imbalances: Gut inflammation can disturb the balance of female hormones [26]. Conditions associated with unbalanced hormones, such as PMS, PCOS, obesity, endometriosis, and breast cancer, are associated with imbalances in the digestive tract [27].
- Male hormone imbalances: Inflammation can also cause male hormone imbalances [28], resulting in fatigue, low libido, erectile dysfunction, muscle loss, and poor memory.
- Hypothyroid symptoms: Hypothyroid symptoms, such as fatigue, hair loss, dry skin, and weight gain, without evidence of low thyroid function on lab tests can often be linked to inflammation in the gut. Inflammation damages your body’s ability to use thyroid hormone, and this can lead to hypothyroid symptoms [29].
Immune System and Autoimmunity—Signs and Symptoms
The greatest density of immune cells in your body can be found in your small intestine [30]. Bacterial overgrowths or chronic inflammation in the small intestine can send the immune system into a constant state of hyperreactivity and immune reactions.
Research shows that those with IBS have overactive immune responses in the gut [31]. A large body of research makes a strong association between autoimmune conditions and imbalances in the gut microbiota.
Here are some of the symptoms and conditions that can occur because of immune dysregulation that starts in the gut:
- Food reactivity: Food allergies or food intolerances are often caused by immune system imbalances in the intestines [32, 33].
- Celiac disease and gluten intolerance: Both can occur because of immune dysregulation in the small intestine [34, 35].
- Histamine intolerance: Histamine symptoms like hay fever, hives, itching, and even heart palpitations are an immune response that can be triggered by poor gut health [36, 37, 38, 39, 40].
- Autoimmune thyroid disease: Hashimoto’s disease and Grave’s disease are autoimmune conditions that are closely linked to gut imbalances [41]. Treating certain gut infections has been shown to improve thyroid autoimmunity [42, 43, 44, 45, 46].
- Joint pain—Joint pain is a common symptom in patients with gut issues. Research shows a connection between rheumatoid arthritis, a painful autoimmune disease, and gut imbalances [47, 48, 49]. Gut dysbiosis may also contribute to the development of osteoarthritis [50].
Poor Nutrient Absorption—Signs and Symptoms
Your gut health affects how well you absorb nutrients [51, 52, 53]. Poor digestion and nutrient absorption, or malabsorption, can lead to a number of symptoms:
- Dry or thinning hair: This may be due to protein and fat malabsorption or iron deficiency [54, 55]
- Dry or aged skin: This may be due to fat malabsorption and micronutrient deficiency [56, 57]
- Fatigue: This is the result of general malnourishment [58, 59]
Gut Symptoms
Let’s not forget that problems in the gut can cause digestive symptoms too. Bloating, abdominal pain, excessive belching and farting, constipation, loose stools, reflux, indigestion, and heartburn are obvious signs that all is not well in your digestive tract.
Experiencing any of these digestive symptoms on an ongoing basis strongly indicates an unhealthy gut.
Why Is Poor Gut Health So Common?
People living in Westernized societies tend to have less bacterial diversity in their gut compared to those living in non-Westernized societies [60, 61].
Why are our microbiotas less diverse in more developed societies? As Westernized societies have become increasingly sterile and hygienic, we’ve become more disconnected from environmental sources of microbes — through contact with soil, animals, and nature. In contrast, a modern-day hunter-gatherer is in constant contact with all of these sources [62, 63, 64].
Our decreased bacterial exposure starts at birth, with more C-sections and less breastfeeding [65]. Antibiotic use, antibacterial products, and higher sanitation standards have provided many benefits. However, there are negative impacts on the health and diversity of our gut microbiome [66].
Finally, our Western lifestyles of fast food (poor diet), stress, prescription medications, deskbound days, and sleepless nights take their toll on our gut health [67, 68, 69, 70, 71, 72, 73, 74].
How To Get Your Gut Health Back on Track
I developed the Great-in-8 Action Plan as a system for restoring good gut health. It’s a step-by-step approach that addresses the most fundamental issues first. Here’s an overview:
The Great-in-8 Action Plan
1. Reset — Improve your diet and lifestyle.
2. Support — Support your gut with probiotics and digestive enzymes/acid.
3. Remove — Remove/reduce unwanted gut bacteria with antimicrobial herbs.
4. Rebalance — Rebalance gut bacteria after treatment with antimicrobial herbs.
5. Reintroduce — Reintroduce the foods you removed.
6. Feed — Feed the good bacteria.
7. Wean — Wean yourself off the supplements in your plan.
8. Maintenance and fun — Maintain your improvements, and enjoy your newfound health.

Anyone can get started with the Great-in-8 Action Plan at home to improve their digestive and non-digestive symptoms by improving their diet, addressing stress and lifestyle issues, and boosting beneficial bacteria through probiotic supplementation.
For some people, these first steps, described below, are enough to get gut health back on track. Those with more complex gut issues may need to take additional steps described in my book, Healthy Gut, Healthy You.
Diet Options for Better Gut Health
Sugar, alcohol, and processed foods feed bad bacteria in the gut and increase inflammation. There are several anti-inflammatory diet options that can improve your digestive health. However, the most important strategy is to focus on eating whole, unprocessed foods and to listen to your body.
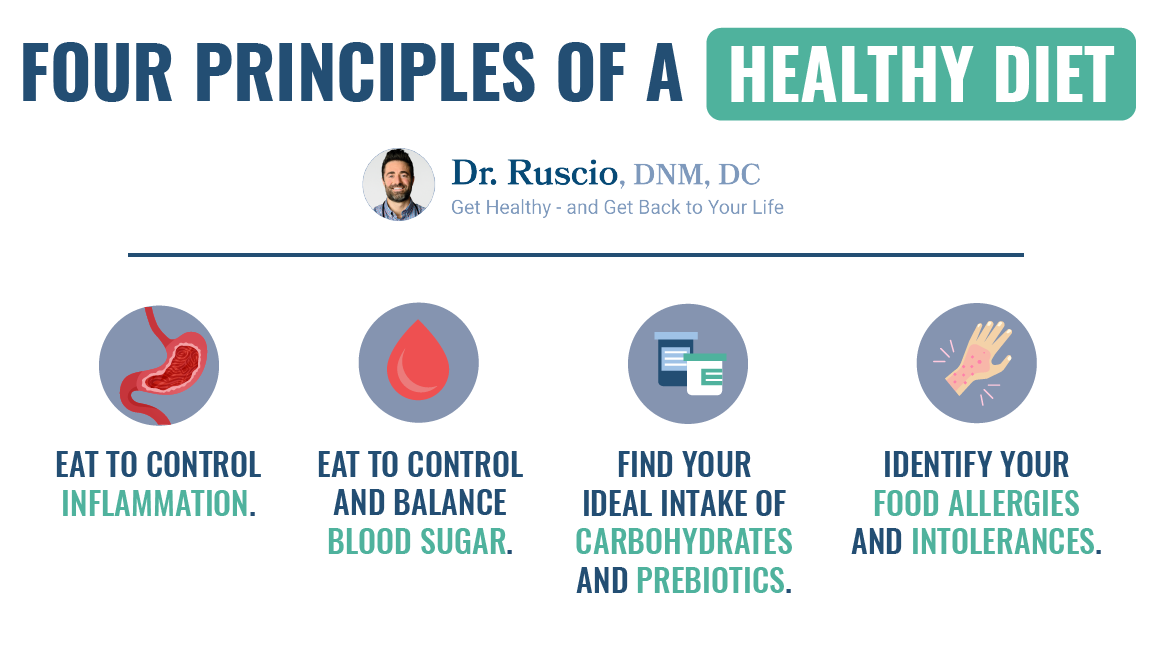
There are four important principles when it comes to healthy eating:
- Eat to control inflammation.
- Eat to control and balance blood sugar.
- Find your ideal intake of carbohydrates and prebiotics.
- Identify your food allergies and intolerances. (This relates to #1.)
I often recommend the Paleo diet to patients, as it can help you address all four dietary principles.
Lifestyle Options for Better Gut Health
Poor lifestyle habits can contribute significantly to poor gut health, for example:
- Chronic stress increases cortisol and other stress hormones which contribute to poor gut health [75, 76]. Over-exercising is a form of chronic stress that has been shown to negatively impact gut health [77].
- Sleeping poorly or not getting enough sleep can also impact your gut health and lead to intestinal permeability [78].
Taking time to take care of yourself is important for your gut health. Strive for 7-8 hours of sleep per night, spend time in nature, enjoy hobbies and friendships, and move your body. Moderate exercise, such as walking and yoga are both known for their stress-busting benefits.
While medications have their place, they are often overused, for example:
- Antibiotics negatively affect your beneficial bacteria populations [79].
- NSAIDs (nonsteroidal anti-inflammatory drugs) and aspirin increase intestinal permeability [80, 81, 82].
- Long-term use of PPIs (proton pump inhibitors) create conditions that invite bacterial overgrowth [83, 84].
You might be using medication to relieve what are the symptoms of an unhealthy gut while causing further damage to your gut health. For example, NSAIDs like Ibuprofen and Aleve temporarily calm inflammation but cause leaky gut and more inflammation in the long term. If this is the case for you, work to wean yourself off while taking other steps to heal your gut.
Probiotics for Better Gut Health
Another fundamental approach for better gut health is taking high-quality probiotic supplements.
Probiotics can help improve the balance of organisms in your gut, reduce overzealous immune system activity, and reduce the inflammation which many of us suffer from. The benefits of probiotics are clearly shown in hundreds of clinical studies and include:
- Increase bacterial diversity, or health, of your gut flora [85]
- Fight bad bacteria and other harmful gut bugs [86, 87, 88]
- Promote more rapid recovery from imbalances in your microbiome [89]
- Promote a healthy immune response in your gut [90, 91, 92]
- Reduce gut inflammation [93]
- Encourage the growth of healthier microbes in your gut [94]
- Reduce leaky gut and damage to your gut lining [95, 96, 97]
Probiotic foods like kimchi, kefir, sauerkraut, and kombucha are healthy dietary choices that provide small doses of beneficial bacteria. However, for higher daily probiotic doses and therapeutic effects, probiotic supplements are the best choice.
Your Gut Holds the Key To Better Health
The health and diversity of the microorganisms in your digestive tract don’t just help with digesting food. They play a major role in your overall wellness.
Poor gut health can show up as digestive symptoms or as seemingly unrelated symptoms like fatigue, poor mood, insomnia, or brain fog. Poor gut health can also manifest as hormonal, inflammatory, or immune conditions.
There’s lots you can do to support better gut health. Start by eating a whole foods diet, getting enough sleep, managing stress, and taking probiotic supplements. If you need more help, schedule an appointment with our clinic.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Frändemark Å, Jakobsson Ung E, Törnblom H, Simrén M, Jakobsson S. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil. 2017 Jan;29(1). doi: 10.1111/nmo.12898. Epub 2016 Jul 11. PMID: 27401139.
- Han CJ, Yang GS. Fatigue in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis of Pooled Frequency and Severity of Fatigue. Asian Nurs Res (Korean Soc Nurs Sci). 2016 Mar;10(1):1-10. doi: 10.1016/j.anr.2016.01.003. Epub 2016 Feb 1. PMID: 27021828.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR; Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12:85. doi: 10.1186/1741-7015-12-85. PMID: 24885375; PMCID: PMC4053283.
- Maes M, Leunis JC. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Neuro Endocrinol Lett. 2008 Dec;29(6):902-10. PMID: 19112401.
- (2016) Extra-intestinal symptoms in patients with irritable bowel syndrome: related to high total IgE levels and atopic sensitization?, Scandinavian Journal of Gastroenterology, 51:8, 908-913, DOI: 10.3109/00365521.2016.1157890
- (2016) Extra-intestinal symptoms in patients with irritable bowel syndrome: related to high total IgE levels and atopic sensitization?, Scandinavian Journal of Gastroenterology, 51:8, 908-913, DOI: 10.3109/00365521.2016.1157890
- Simpson CA, Mu A, Haslam N, Schwartz OS, Simmons JG. Feeling down? A systematic review of the gut microbiota in anxiety/depression and irritable bowel syndrome. J Affect Disord. 2020 Apr 1;266:429-446. doi: 10.1016/j.jad.2020.01.124. Epub 2020 Jan 22. PMID: 32056910.
- Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016 Sep;44(6):592-600. doi: 10.1111/apt.13738. Epub 2016 Jul 22. PMID: 27444264.
- Geng Q, Zhang QE, Wang F, Zheng W, Ng CH, Ungvari GS, Wang G, Xiang YT. Comparison of comorbid depression between irritable bowel syndrome and inflammatory bowel disease: A meta-analysis of comparative studies. J Affect Disord. 2018 Sep;237:37-46. doi: 10.1016/j.jad.2018.04.111. Epub 2018 May 4. Erratum in: J Affect Disord. 2019 Jun 15;253: PMID: 29758449.
- Skodje GI, Minelle IH, Rolfsen KL, Iacovou M, Lundin KEA, Veierød MB, Henriksen C. Dietary and symptom assessment in adults with self-reported non-coeliac gluten sensitivity. Clin Nutr ESPEN. 2019 Jun;31:88-94. doi: 10.1016/j.clnesp.2019.02.012. Epub 2019 Mar 11. PMID: 31060839.
- Ng QX, Peters C, Ho CYX, Lim DY, Yeo WS. A meta-analysis of the use of probiotics to alleviate depressive symptoms. J Affect Disord. 2018 Mar 1;228:13-19. doi: 10.1016/j.jad.2017.11.063. Epub 2017 Nov 16. PMID: 29197739.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR; Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12:85. doi: 10.1186/1741-7015-12-85. PMID: 24885375; PMCID: PMC4053283.
- Frändemark Å, Jakobsson Ung E, Törnblom H, Simrén M, Jakobsson S. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil. 2017 Jan;29(1). doi: 10.1111/nmo.12898. Epub 2016 Jul 11. PMID: 27401139.
- Ocon AJ. Caught in the thickness of brain fog: exploring the cognitive symptoms of Chronic Fatigue Syndrome. Front Physiol. 2013 Apr 5;4:63. doi: 10.3389/fphys.2013.00063. PMID: 23576989; PMCID: PMC3617392.
- Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, Lamb BT. Inflammation as a central mechanism in Alzheimer’s disease. Alzheimers Dement (N Y). 2018 Sep 6;4:575-590. doi: 10.1016/j.trci.2018.06.014. PMID: 30406177; PMCID: PMC6214864.
- Khanijow V, Prakash P, Emsellem HA, Borum ML, Doman DB. Sleep Dysfunction and Gastrointestinal Diseases. Gastroenterol Hepatol (N Y). 2015 Dec;11(12):817-25. PMID: 27134599; PMCID: PMC4849511.
- O’Neill CA, Monteleone G, McLaughlin JT, Paus R. The gut-skin axis in health and disease: A paradigm with therapeutic implications. Bioessays. 2016 Nov;38(11):1167-1176. doi: 10.1002/bies.201600008. Epub 2016 Aug 24. PMID: 27554239.
- Levkovich T, Poutahidis T, Smillie C, Varian BJ, Ibrahim YM, Lakritz JR, Alm EJ, Erdman SE. Probiotic bacteria induce a ‘glow of health’. PLoS One. 2013;8(1):e53867. doi: 10.1371/journal.pone.0053867. Epub 2013 Jan 16. PMID: 23342023; PMCID: PMC3547054.
- Polkowska-Pruszyńska B, Gerkowicz A, Krasowska D. The gut microbiome alterations in allergic and inflammatory skin diseases – an update. J Eur Acad Dermatol Venereol. 2020 Mar;34(3):455-464. doi: 10.1111/jdv.15951. Epub 2019 Nov 19. PMID: 31520544.
- Lee YB, Byun EJ, Kim HS. Potential Role of the Microbiome in Acne: A Comprehensive Review. J Clin Med. 2019 Jul 7;8(7):987. doi: 10.3390/jcm8070987. PMID: 31284694; PMCID: PMC6678709.
- Lee SY, Lee E, Park YM, Hong SJ. Microbiome in the Gut-Skin Axis in Atopic Dermatitis. Allergy Asthma Immunol Res. 2018 Jul;10(4):354-362. doi: 10.4168/aair.2018.10.4.354. PMID: 29949831; PMCID: PMC6021588.
- Varjonen E, Vainio E, Kalimo K. Antigliadin IgE–indicator of wheat allergy in atopic dermatitis. Allergy. 2000 Apr;55(4):386-91. doi: 10.1034/j.1398-9995.2000.00451.x. PMID: 10782525.
- Nosrati A, Afifi L, Danesh MJ, Lee K, Yan D, Beroukhim K, Ahn R, Liao W. Dietary modifications in atopic dermatitis: patient-reported outcomes. J Dermatolog Treat. 2017 Sep;28(6):523-538. doi: 10.1080/09546634.2016.1278071. Epub 2017 Jan 24. PMID: 28043181; PMCID: PMC5736303.
- Bhatia BK, Millsop JW, Debbaneh M, Koo J, Linos E, Liao W. Diet and psoriasis, part II: celiac disease and role of a gluten-free diet. J Am Acad Dermatol. 2014 Aug;71(2):350-8. doi: 10.1016/j.jaad.2014.03.017. Epub 2014 Apr 26. PMID: 24780176; PMCID: PMC4104239.
- Fu Y, Lee CH, Chi CC. Association of Psoriasis With Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. JAMA Dermatol. 2018 Dec 1;154(12):1417-1423. doi: 10.1001/jamadermatol.2018.3631. PMID: 30422277; PMCID: PMC6583370.
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas. 2017 Sep;103:45-53. doi: 10.1016/j.maturitas.2017.06.025. Epub 2017 Jun 23. PMID: 28778332.
- Goedert JJ, Jones G, Hua X, Xu X, Yu G, Flores R, Falk RT, Gail MH, Shi J, Ravel J, Feigelson HS. Investigation of the association between the fecal microbiota and breast cancer in postmenopausal women: a population-based case-control pilot study. J Natl Cancer Inst. 2015 Jun 1;107(8):djv147. doi: 10.1093/jnci/djv147. PMID: 26032724; PMCID: PMC4554191.
- Tremellen K, McPhee N, Pearce K, Benson S, Schedlowski M, Engler H. Endotoxin-initiated inflammation reduces testosterone production in men of reproductive age. Am J Physiol Endocrinol Metab. 2018 Mar 1;314(3):E206-E213. doi: 10.1152/ajpendo.00279.2017. Epub 2017 Nov 28. PMID: 29183872; PMCID: PMC5899218.
- Mancini A, Di Segni C, Raimondo S, Olivieri G, Silvestrini A, Meucci E, Currò D. Thyroid Hormones, Oxidative Stress, and Inflammation. Mediators Inflamm. 2016;2016:6757154. doi: 10.1155/2016/6757154. Epub 2016 Mar 8. PMID: 27051079; PMCID: PMC4802023.
- El Aidy S, van den Bogert B, Kleerebezem M. The small intestine microbiota, nutritional modulation and relevance for health. Curr Opin Biotechnol. 2015 Apr;32:14-20. doi: 10.1016/j.copbio.2014.09.005. Epub 2014 Oct 8. PMID: 25308830.
- Martin-Viñas JJ, Quigley EM. Immune response in irritable bowel syndrome: A systematic review of systemic and mucosal inflammatory mediators. J Dig Dis. 2016 Sep;17(9):572-581. doi: 10.1111/1751-2980.12379. PMID: 27426409.
- Coucke F. Food intolerance in patients with manifest autoimmunity. Observational study. Autoimmun Rev. 2018 Nov;17(11):1078-1080. doi: 10.1016/j.autrev.2018.05.011. Epub 2018 Sep 11. PMID: 30213697.
- Pietschmann N. Food Intolerance: Immune Activation Through Diet-associated Stimuli in Chronic Disease. Altern Ther Health Med. 2015 Jul-Aug;21(4):42-52. PMID: 26030116.
- Levy J, Bernstein L, Silber N. Celiac disease: an immune dysregulation syndrome. Curr Probl Pediatr Adolesc Health Care. 2014 Dec;44(11):324-7. doi: 10.1016/j.cppeds.2014.10.002. PMID: 25499458.
- Briani C, Samaroo D, Alaedini A. Celiac disease: from gluten to autoimmunity. Autoimmun Rev. 2008 Sep;7(8):644-50. doi: 10.1016/j.autrev.2008.05.006. Epub 2008 Jun 25. PMID: 18589004.
- Sander LE, Lorentz A, Sellge G, Coëffier M, Neipp M, Veres T, Frieling T, Meier PN, Manns MP, Bischoff SC. Selective expression of histamine receptors H1R, H2R, and H4R, but not H3R, in the human intestinal tract. Gut. 2006 Apr;55(4):498-504. doi: 10.1136/gut.2004.061762. Epub 2005 Nov 18. PMID: 16299042; PMCID: PMC1856162.
- Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol. 2018 Aug;69(4). doi: 10.26402/jpp.2018.4.09. Epub 2018 Dec 9. PMID: 30552302.
- Enko D, Meinitzer A, Mangge H, Kriegshäuser G, Halwachs-Baumann G, Reininghaus EZ, Bengesser SA, Schnedl WJ. Concomitant Prevalence of Low Serum Diamine Oxidase Activity and Carbohydrate Malabsorption. Can J Gastroenterol Hepatol. 2016;2016:4893501. doi: 10.1155/2016/4893501. Epub 2016 Nov 30. PMID: 28042564; PMCID: PMC5155086.
- Lappinga PJ, Abraham SC, Murray JA, Vetter EA, Patel R, Wu TT. Small intestinal bacterial overgrowth: histopathologic features and clinical correlates in an underrecognized entity. Arch Pathol Lab Med. 2010 Feb;134(2):264-70. doi: 10.1043/1543-2165-134.2.264. PMID: 20121616.
- Bures J, Cyrany J, Kohoutova D, Förstl M, Rejchrt S, Kvetina J, Vorisek V, Kopacova M. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010 Jun 28;16(24):2978-90. doi: 10.3748/wjg.v16.i24.2978. PMID: 20572300; PMCID: PMC2890937.
- Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function? Nutrients. 2020 Jun 12;12(6):1769. doi: 10.3390/nu12061769. PMID: 32545596; PMCID: PMC7353203.
- Shi WJ, Liu W, Zhou XY, Ye F, Zhang GX. Associations of Helicobacter pylori infection and cytotoxin-associated gene A status with autoimmune thyroid diseases: a meta-analysis. Thyroid. 2013 Oct;23(10):1294-300. doi: 10.1089/thy.2012.0630. Epub 2013 Sep 11. PMID: 23544831.
- Choi YM, Kim TY, Kim EY, Jang EK, Jeon MJ, Kim WG, Shong YK, Kim WB. Association between thyroid autoimmunity and Helicobacter pylori infection. Korean J Intern Med. 2017 Mar;32(2):309-313. doi: 10.3904/kjim.2014.369. Epub 2017 Jan 16. PMID: 28092700; PMCID: PMC5339455.
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017 Feb 7;23(5):842-852. doi: 10.3748/wjg.v23.i5.842. PMID: 28223728; PMCID: PMC5296200.
- Konrad P, Chojnacki J, Kaczka A, Pawłowicz M, Rudnicki C, Chojnacki C. Ocena czynności tarczycy u osób z zespołem przerostu bakteryjnego jelita cienkiego [Thyroid dysfunction in patients with small intestinal bacterial overgrowth]. Pol Merkur Lekarski. 2018 Jan 23;44(259):15-18. Polish. PMID: 29374417.
- El-Zawawy HT, Farag HF, Tolba MM, Abdalsamea HA. Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17. Ther Adv Endocrinol Metab. 2020 Feb 21;11:2042018820907013. doi: 10.1177/2042018820907013. PMID: 32128107; PMCID: PMC7036484.
- Horta-Baas G, Romero-Figueroa MDS, Montiel-Jarquín AJ, Pizano-Zárate ML, García-Mena J, Ramírez-Durán N. Intestinal Dysbiosis and Rheumatoid Arthritis: A Link between Gut Microbiota and the Pathogenesis of Rheumatoid Arthritis. J Immunol Res. 2017;2017:4835189. doi: 10.1155/2017/4835189. Epub 2017 Aug 30. PMID: 28948174; PMCID: PMC5602494.
- Wu X, He B, Liu J, Feng H, Ma Y, Li D, Guo B, Liang C, Dang L, Wang L, Tian J, Zhu H, Xiao L, Lu C, Lu A, Zhang G. Molecular Insight into Gut Microbiota and Rheumatoid Arthritis. Int J Mol Sci. 2016 Mar 22;17(3):431. doi: 10.3390/ijms17030431. PMID: 27011180; PMCID: PMC4813281.
- Maeda Y, Kumanogoh A, Takeda K. [Altered composition of gut microbiota in rheumatoid arthritis patients]. Nihon Rinsho Meneki Gakkai Kaishi. 2016;39(1):59-63. Japanese. doi: 10.2177/jsci.39.59. PMID: 27181236.
- Maeda Y, Kurakawa T, Umemoto E, Motooka D, Ito Y, Gotoh K, Hirota K, Matsushita M, Furuta Y, Narazaki M, Sakaguchi N, Kayama H, Nakamura S, Iida T, Saeki Y, Kumanogoh A, Sakaguchi S, Takeda K. Dysbiosis Contributes to Arthritis Development via Activation of Autoreactive T Cells in the Intestine. Arthritis Rheumatol. 2016 Nov;68(11):2646-2661. doi: 10.1002/art.39783. PMID: 27333153.
- Adike A, DiBaise JK. Small Intestinal Bacterial Overgrowth: Nutritional Implications, Diagnosis, and Management. Gastroenterol Clin North Am. 2018 Mar;47(1):193-208. doi: 10.1016/j.gtc.2017.09.008. Epub 2017 Dec 7. PMID: 29413012.
- Clark R, Johnson R. Malabsorption Syndromes. Nurs Clin North Am. 2018 Sep;53(3):361-374. doi: 10.1016/j.cnur.2018.05.001. Epub 2018 Jul 11. PMID: 30100002.
- Owens SR, Greenson JK. The pathology of malabsorption: current concepts. Histopathology. 2007 Jan;50(1):64-82. doi: 10.1111/j.1365-2559.2006.02547.x. PMID: 17204022.
- Vergnat M, Suzanne J, Entraygues H, Laurent R, Gisselbrecht H, Agache P. Manifestations cutanées et syndrome de malabsorption [Cutaneous manifestations of malabsorption diseases (author’s transl)]. Ann Dermatol Venereol. 1978 Dec;105(12):1009-16. French. PMID: 380445.
- Trost LB, Bergfeld WF, Calogeras E. The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J Am Acad Dermatol. 2006 May;54(5):824-44. doi: 10.1016/j.jaad.2005.11.1104. PMID: 16635664.
- DiBaise M, Tarleton SM. Hair, Nails, and Skin: Differentiating Cutaneous Manifestations of Micronutrient Deficiency. Nutr Clin Pract. 2019 Aug;34(4):490-503. doi: 10.1002/ncp.10321. Epub 2019 May 29. PMID: 31144371.
- Vergnat M, Suzanne J, Entraygues H, Laurent R, Gisselbrecht H, Agache P. Manifestations cutanées et syndrome de malabsorption [Cutaneous manifestations of malabsorption diseases (author’s transl)]. Ann Dermatol Venereol. 1978 Dec;105(12):1009-16. French. PMID: 380445.
- Borren NZ, van der Woude CJ, Ananthakrishnan AN. Fatigue in IBD: epidemiology, pathophysiology and management. Nat Rev Gastroenterol Hepatol. 2019 Apr;16(4):247-259. doi: 10.1038/s41575-018-0091-9. PMID: 30531816.
- Tardy AL, Pouteau E, Marquez D, Yilmaz C, Scholey A. Vitamins and Minerals for Energy, Fatigue and Cognition: A Narrative Review of the Biochemical and Clinical Evidence. Nutrients. 2020 Jan 16;12(1):228. doi: 10.3390/nu12010228. PMID: 31963141; PMCID: PMC7019700.
- Karkman A, Lehtimäki J, Ruokolainen L. The ecology of human microbiota: dynamics and diversity in health and disease. Ann N Y Acad Sci. 2017 Jul;1399(1):78-92. doi: 10.1111/nyas.13326. Epub 2017 Mar 20. PMID: 28319653.
- Oddy WH. Breastfeeding, Childhood Asthma, and Allergic Disease. Ann Nutr Metab. 2017;70 Suppl 2:26-36. doi: 10.1159/000457920. Epub 2017 May 19. PMID: 28521318.
- Segata N. Gut Microbiome: Westernization and the Disappearance of Intestinal Diversity. Curr Biol. 2015 Jul 20;25(14):R611-3. doi: 10.1016/j.cub.2015.05.040. PMID: 26196489.
- Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, Magris M, Hidalgo G, Baldassano RN, Anokhin AP, Heath AC, Warner B, Reeder J, Kuczynski J, Caporaso JG, Lozupone CA, Lauber C, Clemente JC, Knights D, Knight R, Gordon JI. Human gut microbiome viewed across age and geography. Nature. 2012 May 9;486(7402):222-7. doi: 10.1038/nature11053. PMID: 22699611; PMCID: PMC3376388.
- Mancabelli L, Milani C, Lugli GA, Turroni F, Ferrario C, van Sinderen D, Ventura M. Meta-analysis of the human gut microbiome from urbanized and pre-agricultural populations. Environ Microbiol. 2017 Apr;19(4):1379-1390. doi: 10.1111/1462-2920.13692. Epub 2017 Feb 28. PMID: 28198087.
- Oddy WH. Breastfeeding, Childhood Asthma, and Allergic Disease. Ann Nutr Metab. 2017;70 Suppl 2:26-36. doi: 10.1159/000457920. Epub 2017 May 19. PMID: 28521318.
- Feng Y, Huang Y, Wang Y, Wang P, Song H, Wang F. Antibiotics induced intestinal tight junction barrier dysfunction is associated with microbiota dysbiosis, activated NLRP3 inflammasome and autophagy. PLoS One. 2019 Jun 18;14(6):e0218384. doi: 10.1371/journal.pone.0218384. PMID: 31211803; PMCID: PMC6581431.
- Vanuytsel T, van Wanrooy S, Vanheel H, Vanormelingen C, Verschueren S, Houben E, Salim Rasoel S, Tόth J, Holvoet L, Farré R, Van Oudenhove L, Boeckxstaens G, Verbeke K, Tack J. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut. 2014 Aug;63(8):1293-9. doi: 10.1136/gutjnl-2013-305690. Epub 2013 Oct 23. PMID: 24153250.
- Costa RJS, Snipe RMJ, Kitic CM, Gibson PR. Systematic review: exercise-induced gastrointestinal syndrome-implications for health and intestinal disease. Aliment Pharmacol Ther. 2017 Aug;46(3):246-265. doi: 10.1111/apt.14157. Epub 2017 Jun 7. PMID: 28589631.
- Swanson GR, Burgess HJ. Sleep and Circadian Hygiene and Inflammatory Bowel Disease. Gastroenterol Clin North Am. 2017 Dec;46(4):881-893. doi: 10.1016/j.gtc.2017.08.014. PMID: 29173529.
- Bode C, Bode JC. Effect of alcohol consumption on the gut. Best Pract Res Clin Gastroenterol. 2003 Aug;17(4):575-92. doi: 10.1016/s1521-6918(03)00034-9. PMID: 12828956.
- Utzeri E, Usai P. Role of non-steroidal anti-inflammatory drugs on intestinal permeability and nonalcoholic fatty liver disease. World J Gastroenterol. 2017 Jun 14;23(22):3954-3963. doi: 10.3748/wjg.v23.i22.3954. PMID: 28652650; PMCID: PMC5473116.
- Graham DY, Opekun AR, Willingham FF, Qureshi WA. Visible small-intestinal mucosal injury in chronic NSAID users. Clin Gastroenterol Hepatol. 2005 Jan;3(1):55-9. doi: 10.1016/s1542-3565(04)00603-2. PMID: 15645405.
- Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993 Jun;104(6):1832-47. doi: 10.1016/0016-5085(93)90667-2. PMID: 8500743.
- Swanson GR, Burgess HJ. Sleep and Circadian Hygiene and Inflammatory Bowel Disease. Gastroenterol Clin North Am. 2017 Dec;46(4):881-893. doi: 10.1016/j.gtc.2017.08.014. PMID: 29173529.
- Vanuytsel T, van Wanrooy S, Vanheel H, Vanormelingen C, Verschueren S, Houben E, Salim Rasoel S, Tόth J, Holvoet L, Farré R, Van Oudenhove L, Boeckxstaens G, Verbeke K, Tack J. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut. 2014 Aug;63(8):1293-9. doi: 10.1136/gutjnl-2013-305690. Epub 2013 Oct 23. PMID: 24153250.
- Costa RJS, Snipe RMJ, Kitic CM, Gibson PR. Systematic review: exercise-induced gastrointestinal syndrome-implications for health and intestinal disease. Aliment Pharmacol Ther. 2017 Aug;46(3):246-265. doi: 10.1111/apt.14157. Epub 2017 Jun 7. PMID: 28589631.
- Costa RJS, Snipe RMJ, Kitic CM, Gibson PR. Systematic review: exercise-induced gastrointestinal syndrome-implications for health and intestinal disease. Aliment Pharmacol Ther. 2017 Aug;46(3):246-265. doi: 10.1111/apt.14157. Epub 2017 Jun 7. PMID: 28589631.
- Swanson GR, Burgess HJ. Sleep and Circadian Hygiene and Inflammatory Bowel Disease. Gastroenterol Clin North Am. 2017 Dec;46(4):881-893. doi: 10.1016/j.gtc.2017.08.014. PMID: 29173529.
- Feng Y, Huang Y, Wang Y, Wang P, Song H, Wang F. Antibiotics induced intestinal tight junction barrier dysfunction is associated with microbiota dysbiosis, activated NLRP3 inflammasome and autophagy. PLoS One. 2019 Jun 18;14(6):e0218384. doi: 10.1371/journal.pone.0218384. PMID: 31211803; PMCID: PMC6581431.
- Utzeri E, Usai P. Role of non-steroidal anti-inflammatory drugs on intestinal permeability and nonalcoholic fatty liver disease. World J Gastroenterol. 2017 Jun 14;23(22):3954-3963. doi: 10.3748/wjg.v23.i22.3954. PMID: 28652650; PMCID: PMC5473116.
- Graham DY, Opekun AR, Willingham FF, Qureshi WA. Visible small-intestinal mucosal injury in chronic NSAID users. Clin Gastroenterol Hepatol. 2005 Jan;3(1):55-9. doi: 10.1016/s1542-3565(04)00603-2. PMID: 15645405.
- Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993 Jun;104(6):1832-47. doi: 10.1016/0016-5085(93)90667-2. PMID: 8500743.
- Theisen J, Nehra D, Citron D, Johansson J, Hagen JA, Crookes PF, DeMeester SR, Bremner CG, DeMeester TR, Peters JH. Suppression of gastric acid secretion in patients with gastroesophageal reflux disease results in gastric bacterial overgrowth and deconjugation of bile acids. J Gastrointest Surg. 2000 Jan-Feb;4(1):50-4. doi: 10.1016/s1091-255x(00)80032-3. PMID: 10631362.
- Williams C. Occurrence and significance of gastric colonization during acid-inhibitory therapy. Best Pract Res Clin Gastroenterol. 2001 Jun;15(3):511-21. doi: 10.1053/bega.2001.0191. PMID: 11403543.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106-1113. doi: 10.2174/1389200219666180813144834. PMID: 30101706; PMCID: PMC6340155.
- Wang F, Feng J, Chen P, Liu X, Ma M, Zhou R, Chang Y, Liu J, Li J, Zhao Q. Probiotics in Helicobacter pylori eradication therapy: Systematic review and network meta-analysis. Clin Res Hepatol Gastroenterol. 2017 Sep;41(4):466-475. doi: 10.1016/j.clinre.2017.04.004. Epub 2017 May 25. PMID: 28552432.
- García-Collinot G, Madrigal-Santillán EO, Martínez-Bencomo MA, Carranza-Muleiro RA, Jara LJ, Vera-Lastra O, Montes-Cortes DH, Medina G, Cruz-Domínguez MP. Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020 Apr;65(4):1134-1143. doi: 10.1007/s10620-019-05830-0. Epub 2019 Sep 23. PMID: 31549334.
- Greco A, Caviglia GP, Brignolo P, Ribaldone DG, Reggiani S, Sguazzini C, Smedile A, Pellicano R, Resegotti A, Astegiano M, Bresso F. Glucose breath test and Crohn’s disease: Diagnosis of small intestinal bacterial overgrowth and evaluation of therapeutic response. Scand J Gastroenterol. 2015;50(11):1376-81. doi: 10.3109/00365521.2015.1050691. Epub 2015 May 19. PMID: 25990116.
- Sanders ME. Impact of probiotics on colonizing microbiota of the gut. J Clin Gastroenterol. 2011 Nov;45 Suppl:S115-9. doi: 10.1097/MCG.0b013e318227414a. PMID: 21992949.
- Toribio-Mateas M. Harnessing the Power of Microbiome Assessment Tools as Part of Neuroprotective Nutrition and Lifestyle Medicine Interventions. Microorganisms. 2018 Apr 25;6(2):35. doi: 10.3390/microorganisms6020035. PMID: 29693607; PMCID: PMC6027349.
- Stenman LK, Lehtinen MJ, Meland N, Christensen JE, Yeung N, Saarinen MT, Courtney M, Burcelin R, Lähdeaho ML, Linros J, Apter D, Scheinin M, Kloster Smerud H, Rissanen A, Lahtinen S. Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults-Randomized Controlled Trial. EBioMedicine. 2016 Nov;13:190-200. doi: 10.1016/j.ebiom.2016.10.036. Epub 2016 Oct 26. PMID: 27810310; PMCID: PMC5264483.
- Frei R, Akdis M, O’Mahony L. Prebiotics, probiotics, synbiotics, and the immune system: experimental data and clinical evidence. Curr Opin Gastroenterol. 2015 Mar;31(2):153-8. doi: 10.1097/MOG.0000000000000151. PMID: 25594887.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106-1113. doi: 10.2174/1389200219666180813144834. PMID: 30101706; PMCID: PMC6340155.
- Toribio-Mateas M. Harnessing the Power of Microbiome Assessment Tools as Part of Neuroprotective Nutrition and Lifestyle Medicine Interventions. Microorganisms. 2018 Apr 25;6(2):35. doi: 10.3390/microorganisms6020035. PMID: 29693607; PMCID: PMC6027349.
- Mujagic Z, de Vos P, Boekschoten MV, Govers C, Pieters HH, de Wit NJ, Bron PA, Masclee AA, Troost FJ. The effects of Lactobacillus plantarum on small intestinal barrier function and mucosal gene transcription; a randomized double-blind placebo controlled trial. Sci Rep. 2017 Jan 3;7:40128. doi: 10.1038/srep40128. PMID: 28045137; PMCID: PMC5206730.
- Sindhu KN, Sowmyanarayanan TV, Paul A, Babji S, Ajjampur SS, Priyadarshini S, Sarkar R, Balasubramanian KA, Wanke CA, Ward HD, Kang G. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014 Apr;58(8):1107-15. doi: 10.1093/cid/ciu065. Epub 2014 Feb 5. PMID: 24501384; PMCID: PMC3967829.
- Lamprecht M, Bogner S, Schippinger G, Steinbauer K, Fankhauser F, Hallstroem S, Schuetz B, Greilberger JF. Probiotic supplementation affects markers of intestinal barrier, oxidation, and inflammation in trained men; a randomized, double-blinded, placebo-controlled trial. J Int Soc Sports Nutr. 2012 Sep 20;9(1):45. doi: 10.1186/1550-2783-9-45. PMID: 22992437; PMCID: PMC3465223.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!