Is SIBO a Real Condition?

SIBO stands for Small Intestinal Bacterial Overgrowth and essentially means someone has too much bacteria in their small intestine. This may cause the symptoms associated with IBS (such as abdominal pain, diarrhea and/or constipation and bloating), food sensitivities, and even things like skin breakouts, fatigue and depression. SIBO can be tested via a simple breath test. Recently this concept has been criticized and some have suggested that SIBO is not a real condition.
In light of this I wanted to provide an updated account of what SIBO is, what it is not, how we can test for it, and what testing pitfalls should be avoided. Most importantly, how one can use a SIBO breath test and SIBO treatments to feel better. Below you will find a combination of true statements, which I will then further support. Key points, that will help make sure you heal your gut effectively. Or, a statement labeled as incorrect which I will refute.
It’s important to challenge assumptions and beliefs. In part because, as helpful as natural and functional medicine is, there is also a tendency to over react, over diagnose and over treat.
Important Clarifications
- SIBO is not a ‘condition’ per se, it is a lab finding that can underlie the condition of IBS, and likely contributes to a number of other conditions like rheumatoid arthritis, restless leg syndrome, rosacea, fibromyalgia and non-responsive celiac disease. It seems to increase risk of, or at least be associated with hypothyroid, overweight, high blood sugar and high cholesterol. This is important to realize because some perfectly healthy people will test positive for SIBO. So, a positive SIBO test does not mean anything by itself.
- We can organize SIBO under a broader umbrella term of digestive tract dysbiosis. Dysbiosis simply means an imbalance of bacteria, fungus and other organisms of the gut.
- Treatment of digestive tract dysbiosis (which includes SIBO) can have far reaching beneficial effects: rheumatoid arthritis, rosacea, thyroid autoimmunity, mood, cholesterol and blood sugar, weight, sleep, non-responsive celiac. Support for all these points to follow.
- There is more to digestive health than SIBO. For example, a common SIBO diet called the Low FODMAP diet does more than reduce gas levels and symptoms associated with SIBO and IBS. It also reduces leaky gut, inflammation and histamine (a marker of immune activation in the gut). The low FODMAP diet also normalizes serotonin and PYY producing cell levels in the gut. These are neurotransmitters which are abnormal in those with IBS, but after using the SIBO friendly low FODMAP diet, become more like that of normal controls. (1 and see my study summary here 2 {subscription required}, 3, 4, 5, 6, 7)
- IBS is not all about having too much gas. Some with IBS may have a normal gas level but are hypersensitive to gas pressure. So, they may do better with lower than normal gas levels.
- “Patients with IBS who developed symptoms on FODMAP challenge did not, in fact, have greater colonic volume than those who do not report symptoms, suggesting that visceral hypersensitivity to luminal distension, rather than increased luminal distension per se, is key to symptom provocation during colonic fermentation” (8)
- The importance of the small intestine is often overlooked in conversations regarding gut health. For example, while high intake of prebiotics and fiber may be beneficial for the large intestine this may hurt many people with IBS. This is because these interventions may help the large intestine but irritate the small intestine. Remember:
- The small intestine represents over 56% of your digestive tract
- Is responsible for 90% of caloric absorption
- Contains the largest density of immune cells in the entire body
- Is more prone to damage and leaky gut than any other part of the gut
Points Where I Agree with Criticisms
Over diagnosis of SIBO creates confusion and fear
I agree. Testing is overused and overly relied on. Diagnoses are often handed out too quickly and without adequate substantiation. Patients are sometimes indoctrinated into thinking SIBO is a chronic condition, that can never be cleared and will require lifelong management. This is simply not true for most and is an example of the damage done by overzealousness.
- Get help with Small Intestinal Bacterial Overgrowth (SIBO).
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Not everyone with “SIBO” will require treatment or will have symptoms
In those with digestive symptoms, there is a range of positivity for SIBO from about 4-84%. (9) More conservative estimates suggest 40% of SIBO occurrence in those with IBS. The prestigious Rome Foundation concluded that a 30-46% occurrence of SIBO in those with IBS compared to only 4% in healthy controls is more accurate. (10)
Subsequent studies, based on GBT for SIBO diagnosis, confirmed a correlation between SIBO and IBS. In fact, the prevalence of SIBO in patients with IBS fluctuated between 30% and 46%, as compared to 4% in healthy controls.
So SIBO can cause the symptoms of IBS, but it is not guaranteed to. If you reserve testing until after you have undergone other foundation therapies, this could include diet, lifestyle changes and probiotics, you will increase the likelihood that a positive test will require treatment. So, don’t test overzealously.
However, there are also those who only exhibit non-digestive symptoms of “SIBO”. Symptoms could include rosacea, restless leg syndrome, high cholesterol and blood sugar. And potentially depression, joint pain, and not responding fully to a gluten free diet.
Treating SIBO improves;
- Rosacea (11)
- Restless Leg Syndrome (12, 13)
- Blood sugar, cholesterol, and potentially weight (14, 15, 16, 17)
- Probiotics, a SIBO treatment (more on this in a moment), improved depression (18)
- Rheumatoid Arthritis. Here is a case study with one of my patients and here is a published research study, both supporting how SIBO treatment can improve RA. (19, 20)
- SIBO treatment lead to full improvement in those who did not fully respond to a gluten free diet. Lets expand on this.
A pivotal study illustrates this concept. 15 celiac patients were studied who all had gone gluten free, but still had some lingering symptoms. These patients were then tested, and the following was found:
- 2 patients could not digest dairy
- 1 patient had a Giardia lamblia infection and 1 patient had giant roundworm infection (Ascaris lumbricoides)
- 10 patients showed small intestinal bacterial overgrowth (SIBO)
The two patients went off dairy. Giardia and roundworm were treated with antibiotics in the other two patients. And the ten SIBO patients were treated with a different antibiotic (Rifaximin). A month after treatment all of these patients were symptom free. This study beautifully illustrates the point that if diet doesn’t work, the next step should be investigating a gut infection, overgrowth or imbalance (aka dysbiosis). This recommendation has been echoed by other researchers as well. (22, 23, 24)
You’re probably better off treating IBS than treating SIBO
SIBO is one potential cause of IBS and ill health, it is not the only cause. There are many things that can cause IBS and problems in the gut. Therefore, it’s better to treat IBS which is broader than SIBO. Even better yet still would be an approach to treat your gut holistically and not limit your gut treatments to only SIBO and/or IBS. This is exactly what I recommend in Healthy Gut, Healthy You, to treat your individual gut as an ecosystem and work to find the factors that will work for your gut ecosystem.
Points Where I Disagree
SIBO treatments are ineffective – Incorrect
One author recently made a particularly pointed criticism here. I agree that we should be cautious of overtreatment, however overall this statement is misleading and ill informed. Treatments for gut health can be quite effective and lead to a wide range of improvements. Including improvements that extend beyond the gut, as we detailed above. I will develop this more below.
Diets for SIBO don’t work – Incorrect
&
Carbs do not have a unique impact upon SIBO bacterial production in the small intestine – Incorrect
These statements are again ill informed and misleading. While we know other compounds impact your gut bacteria, by far the most impact is through ingestion of prebiotic and fiber rich carbohydrate.
It has been clearly documented that diets that restrict carbohydrates that feed bacteria improve SIBO and IBS symptoms. These are known as low FODMAP diets. You can see a few versions of a low FODMAP diet here. Let’s look at what the research says regarding low FODMAP diets (aka SIBO diets).
I should first mention that a meta-analysis is generally agreed to be the highest level of scientific evidence. This is because a meta-analysis attempts to summarize what all the available studies have found. So, one meta-analysis may summarize the findings of 10, 30 or even 50 individual studies. With this in mind…
A meta-analysis entitled Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis recently concluded the low FODMAP diet is effective for those experiencing digestive symptoms
“The present meta-analysis supports the efficacy of a low FODMAP diet in the treatment of functional gastrointestinal symptoms.”
And two other meta-analyses have come to the same conclusion (26, 27).
And to quote another research paper (28)
“There are currently at least 10 randomized controlled trials or randomized comparative trials showing the low FODMAP diet leads to clinical response in 50%–80% of patients with IBS, in particular with improvements in bloating, flatulence, diarrhea and global symptoms.”
Remember how we discussed treating SIBO as being able to help non-digestive symptoms? Well a SIBO diet, aka low FODMAP diet was shown to improve pain and quality of life in those with fibromyalgia. Speculatively, a low FODMAP diet may even help with brain fog. A low FODMAP diet has been shown to lower histamine levels, 8-fold. Histamine can cause brain fog when levels are high. Histamine is also involved in the allergic response.
Hypnotherapy is better than a low FODMAP diet – Incorrect
An ill-informed author made a strong statement after citing one study. Citing one paper in defense of a strong statement is poor science and very misleading. Apparently, this author does not read thoroughly because the study clearly stated that at 6 months, the impact from diet was better than the impact from hypnotherapy.
This improvement relative to baseline symptoms was maintained 6 months post-treatment in 74% (hypnotherapy), 82% (diet) and 54% (hypnotherapy and diet).
I have no quarrel with hypnotherapy. Hypnotherapy did show substantial benefit in this study, which is great. However, making the statement that hypnotherapy is better than diet for SIBO, is an intellectually dishonest statement.
.
SIBO violates Koch’s postulate, therefore SIBO is not ‘real’ – Incorrect
This same author states SIBO is not valid because it violates Koch’s postulate. This concept makes sense, if we were utilizing a 1980s level of understanding… we have learned there is an important interplay between the host, one’s commensal bacteria and one’s immune system to dictate whether or not it will be problematic. This is why, for example, malaria seemed to be commensal in Sardinia, and then when it was eradicated a high level of MS ensued. Also, why H. pylori may be protective in some and we also see Prevotella copri acting differently in different hosts. Below is an excerpt regarding Prevotella from Healthy Gut, Healthy You
- Here is another example from mice studies regarding a bacteria called Prevotella copri DMS 18205 (34). I don’t like citing animal data but this study helps illustrate the point. When this bacteria was transplanted into one group of mice, it actually showed the ability to improve glucose levels. So this suggests it may help with things like diabetes. However, when transplanted into a different group of mice, it actually caused arthritis (35). Also, when this same bacteria was transferred into mice that had been previously given antibiotics, they formed colitis or inflammation in the intestines. So we see the same bacteria acting in very different ways in different contexts. Again, because your gut is a complex ecosystem.
.
Rifaximin treatment for SIBO has poor efficacy – Incorrect
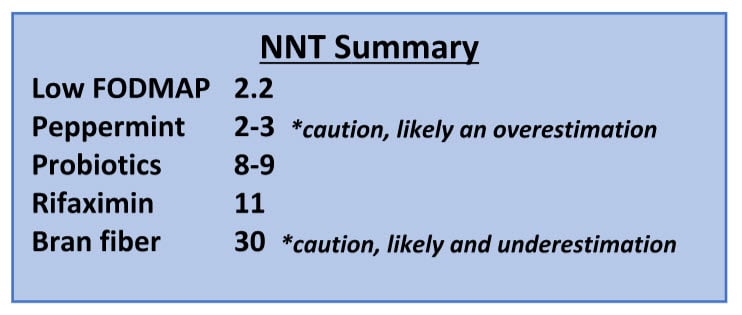
One author stated that the number needed to treat (NNT) of 11 for Rifaximin is poor. NNT simply means the number of people need to have the treatment before one will benefit. Rifaximin is the most commonly used antibiotic for SIBO and IBS. Rifaximin is FDA approved to treat diarrheal IBS. I partially agree that results obtained in Rifaximin studies could be better, but to say the treatment is ineffective is misleading.
Lets again look to what high level science reports, with another meta-analysis regarding Rifaximin, Systematic review with meta-analysis: Rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth
Here are a few direct quotes:
- “32 studies involving 1331 patients were included
- The overall eradication rate according to intention-to-treat analysis was 70.8%
- The overall rate of adverse events was 4.6%
- Improvement or resolution of symptoms in patients with eradicated SIBO was found to be 67.7%”
- “CONCLUSION: Rifaximin treatment seems to be effective and safe for the treatment of SIBO.”
Is Rifaximin the best and only option for IBS and/or SIBO? No. Should you be discouraged by criticism of Rifaximin? No. Rifaximin in these studies is used as a monotherapy, and for only 2 weeks, which may not be adequate duration for more progressed cases. These studies often leave out synergistic interventions such as diet, lifestyle and probiotics. If nothing else the antibiotic/Rifaximin studies establish the premise that antibacterial therapy, is one efficacious component of SIBO/IBS treatment.
There are better treatment options than antibiotics for SIBO and/or IBS – Key Point
Peppermint

Some cite peppermint oil (aka menthol) as the most effective treatment for IBS, having a number needed to treat of 2-3. Peppermint oil is certainly a consideration and something that I use in my clinical practice. But it’s also important we don’t paint a false picture of peppermint being more effective that it might be.
As a general rule, the smaller the sample size (aka number of people studied) the more positive the results. So the less studies on something usually equals a lower NNT (number needed to treat). The opposite is also true. The more something is studied the higher the NNT tends to become, this is known as positive publication bias. There are only a handful of studies with peppermint, about 4, whereas there are around 90 with probiotics. The NNT for peppermint is 2-3 and the NNT for probiotics is 8-9 (39). They are both effective which is why I recommend both of these (40, 41). However, thinking peppermint is more effective than probiotics for IBS or SIBO is extremely misguided.
Probiotics
It’s important to mention that the number needed to treat (NNT) for probiotics are better than most of the drug therapies (but not all) for IBS, and better than fiber. Probiotics can clean bacterial overgrowth, and other forms of dysbiosis in the gut like fungus and parasites. Probiotics have been shown as effective as anti-fungal and anti-parasitic medication. (42, 43)
One study even found that probiotics worked better for those with IBS with SIBO when compared to those who have IBS without SIBO. (44)
This is the first study that prospectively demonstrated superior clinical efficacy of probiotics in patients with IBS with SIBO.
This is likely because probiotics can reduce overgrowths of bacteria. So, it’s no surprise that the highest-level science, a meta-analysis, showed probiotics can decrease gas levels, SIBO and relieve some digestive symptoms… (46)
“the present findings indicated that probiotics supplementation could effectively decontaminate SIBO, decrease H2 concentration, and relieve abdominal pain.”
Several studies were reviewed in my book, showing that probiotics either decrease SIBO gas levels, symptoms or both. Here is an excerpt;
Probiotics for SIBO
- A symptomatic improvement of 82% was seen using a probiotic as the only treatment for SIBO patients. This improvement was 30% better than a group of patients being treated with the antibiotic metronidazole. (The probiotics contained 33 million Lactobacillus casei and L. plantarum, Streptococcus faecalis, and Bifidobacter brevis – dosed once to twice a day) (47)
- A 64% reduction of SIBO gas levels after using lactobacillus as the only treatment (6.5 billion Lactobacillus casei Shirota) (48)
- A 47 % SIBO eradication rate using a dose of 2 billion Bacillus clausii, (49) this is a soil based/spore forming probiotic as we discussed earlier.
What are the best probiotics for SIBO? Again, I detail this in Healthy Gut, Healthy You but essentially you should experiment with 1 of each of the three classes of probiotics. The three categories are;
- Lactobacillus and Bifidobacterium blend
- Saccharomyces boulardii
- Soil based organisms (select bacillus species)
The Low FODMAP Diet
The low FODMAP diet displayed a NNT of 2.2 according to a meta-analysis of clinical trials (which is pretty good for a diet that critics say doesn’t work and treats a problem that doesn’t exist). There have been roughly 12 studies on the low FODMAP diet, so there is a fair amount of evidence.
The results of a recent meta-analysis of RCT evaluating the effectiveness of low FODMAP diet in patients with IBS consistently support the utility of this dietary intervention with an estimated number needed to treat (NNT) of 2.2 (51)
Herbal Antimicrobials
There are less studies examining herbal antimicrobials, but they have been shown effective in IBS and SIBO. Herbal antimicrobials work to clean out overgrown or unwanted organisms (dysbiosis) from the gut. (52, 53)
In my clinical observation herbal antimicrobials and probiotics are more curative than peppermint oil and can alleviate symptoms AND allow people to broaden their diet. Many of these herbal medicines also have side benefits of being anti-inflammatory and perhaps even anti-depressants. (54, 55, 56)
It’s very important to mention that, speculatively, herbals can also combat imbalances we might not have caught on testing like small intestinal fungal overgrowth, candida or other bacterial overgrowths like excess hydrogen sulfide bacteria. (57, 58) A wealth of case studies from my office also support this. (59) This is because many herbal medicines act against bacteria, fungus and protozoa at the same time – whereas pharmaceuticals tend to act against just one of these.
Most people do not benefit from treatment in the long term – Incorrect
When looking at drug monotherapy, perhaps. But this paints a very misleading picture of IBS and SIBO long term. One study has shown the low FODMAP diet is helpful in the longer term.
“Follow-up of patients consuming a FODMAP-modified diet suggests clinical benefit in 57%–74% of patients at 14–16 months, although the results are likely subject to significant recall bias.” (60)
Long term success can be garnered when we discover what combination of factors best support your individual gut ecosystem. Factors like diet, lifestyle, probiotics, prebiotic and fiber intake, fasting and use of herbal antimicrobials. This often means NOT treating test results but rather treating you as an entire person, your gut as a unique ecosystem and listening to your body’s response. By combining validated treatments, via a conservative and pragmatic approach, you can obtain excellent results. No published data support this method per se, but there are data to support each of these individual components which together comprise the entire approach. Also, a wealth of happy patients have proven this concept (61). For those in need of help, the approach I use with patients is outlined in Healthy Gut, Healthy You.
No consistent standard for SIBO breath testing – Incorrect
It is true that there is debate regarding the best SIBO breath test, but attempts are currently being made to standardize and increase the accuracy of the testing. The North American Consensus (a panel of expert gastroenterologists and researchers) have laid out guidelines to standardize and prevent over diagnosis (63). The Rome Foundation has also laid out guidelines regarding SIBO breath testing (64). See details below. However, not all clinicians have adopted these updates and over diagnosis and treatment does occur. See summary of the recommendations below.
Bottom Line
If you use the SIBO breath testing the right way, conservatively and in conjunction with someone’s history and symptoms, it can be helpful. Therefore, I recommend never making treatment decisions based upon lab testing alone. This is why a SIBO breath test is not the final data point dictating treatment decisions.
Rome Foundation and North American
Consensus Statements
~Testing Interpretation~
Rome supports (65)
- Use the glucose-SIBO breath test with a recommended cut off of 10-12 ppm. Using 50g of glucose in a 120min test
- Methane testing not recommended
North American Consensus (66)
- A rise in hydrogen of ≥20 ppm by 90 min during glucose or lactulose breath test for SIBO was considered positive
- Methane levels ≥10 ppm was considered methane positive
.
SIBO testing does not quantify the amount of bacteria in SI – Incorrect
SIBO breath testing has been shown to correlate with the ‘gold standard’ of duodenal sampling directly from the small intestine. (67)
“For glucose breath test, the diagnostic yield is lower but there is adequate agreement with culture and a good specificity.”
We should never draw conclusions from just one study. Another study found similar results – SIBO testing correlated with gold standard testing, and more importantly subsequent antibiotic treatment improved symptoms which also matched the breath retesting result (68). These same findings were not seen in healthy controls.
CONCLUSION: SIBO appears to be a frequent cause of chronic digestive symptoms in children. The breath test provides a simple and noninvasive method of detecting it.
And yet another study found similar results (69). All that said, the breath test is not perfect and does have valid, published criticism. (70, 71)
SIBO tests are inconsistent & SIBO testing does not correlate with symptoms – Incorrect
The Rome Foundation, one of the largest and most well recognized gastroenterology bodies in the world, does feel SIBO testing can be accurate and clinically useful. However, they do take a conservative stance and recommend judicious use of the test. A similar panel of well recognized experts issued the North America Consensus Statement and while they also feel SIBO breath testing to be accurate and clinically useful, they advise more liberal use of the test. Here is the quick summary.
Rome Foundation and North American
Consensus Statements
~Testing Guidelines~
- Rome recommends the following: (72)
- Use the glucose SIBO breath test, which assesses hydrogen gas
- Reserve this test for populations at risk for SIBO. Specifically, those with certain conditions such as malabsorption (like hypochlorhydria), anatomical abnormalities or gastrointestinal motility failure
- Rome feels the diagnostic value of glucose breath testing is “quite good” but also that the results should be interpreted with caution and should be looked at in context of the patients’ clinical history
- Rome feels bacteria likely do play a role in IBS
- The North American Consensus recommends the following: (73)
- Use the breath test in the routine diagnosis of:
- Methane-associated constipation,
- Evaluation of bloating/gas, and
- Carbohydrate maldigestion
- Use the breath test in the routine diagnosis of:
So top authorities around the world weigh in and seem to agree that SIBO breath testing at least has a partial role when used conservatively. To come to these conclusions experts will, in part, look to high quality studies to craft their opinions. What do the high-quality studies say?
A meta-analysis of 11 studies found, “Breath testing was more often abnormal among IBS subjects than healthy controls.”
Some of the studies reviewed in this meta-analysis have documented that breath testing can predict who will respond to anti-bacterial therapy, and that test results improve as a patient’s symptoms improve.
“In one of these, normalization of the breath test with antibiotics predicted a greater proportion of subject response to treatment. In the other study, subjects responding to the antibiotic Rifaximin had a significantly greater reduction in hydrogen compared to non-responders.”
This same meta-analysis concluded,
“This study demonstrates that the breath test findings in IBS appear to be valid. While this meta-analysis does not suggest that the breath test findings imply SIBO, the abnormal fermentation timing and dynamics of the breath test findings support a role for abnormal intestinal bacterial distribution in IBS.”
Or said another way,
“The results demonstrate that a ‘‘positive’’ breath test is more common in IBS patients compared to controls, irrespective of definition.”
This not the only meta-analysis to find an association between breath testing results and digestive function. (75) I think it’s reasonable to say that a positive breath test indicates dysbiosis, or imbalance in bacteria, even if the testing does not fit the pattern of SIBO specifically.

There is high level evidence showing SIBO breath testing correlates with symptoms – Key Point
High level data has shown abnormal gas production can be elucidated by breath testing, and more importantly, treatment of this dysbiosis can lead to improvement of symptoms which correlates with retesting results. Just to clarify again – abnormal gas production occurs because of bacterial overgrowth, and bacterial overgrowth is a type of dysbiosis.
A meta-analysis of 11 studies entitled Abnormal breath testing in IBS: a meta-analysis found that SIBO breath testing was more often abnormal in those with IBS,
“breath testing was more often abnormal among IBS subjects than healthy controls.”
This held true irrespective of definition of SIBO used.
“The results demonstrate that a ‘‘positive’’ breath test is more common in IBS patients compared to controls, irrespective of definition.”
Are the data here perfect and 100% definitive? No. This paper concluded that abnormal bacteria and abnormal breath test finding are valid in IBS, however we can’t imply this in SIBO specifically. Perhaps due to inconsistency in the diagnostic criteria used in the various studies.
“This study demonstrates that the breath test findings in IBS appear to be valid. While this meta-analysis does not suggest that the breath test findings imply SIBO, the abnormal fermentation timing and dynamics of the breath test findings support a role for abnormal intestinal bacterial distribution in IBS.”

“… a significant association was found between methane on breath test.”
And the authors continued that breath testing may be useful in identifying those with constipation who should be treated with antimicrobial therapy.
We demonstrate that methane present on breath testing is significantly associated with constipation in both IBS and functional constipation. These results suggest there may be merit in using breath testing in constipation. Moreover, methane may be used to identify candidates for antibiotic treatment of constipation.
This then begs the important question, does treatment of SIBO correlate with improved breath test results and with improved symptoms. Yes, we have already covered some evidence to support this. Let’s continue.
SIBO breath retesting results correlate with response to treatment – Key Point
A clinical trial looked to assess if treating SIBO lead to improved symptoms and improved SIBO breath testing results. They found that 84% of subjects with IBS had SIBO via breath testing, while only 20% of healthy controls had SIBO. Antibiotic treatment lead to 35% improvement whereas placebo lead to 11% improvement. The best outcomes occurred in those treated who also saw a normalization of their breath test, this especially reinforces the connection between SIBO breath test results and symptoms. The authors concluded that normalization of the breath test leads to a significant reduction in symptoms.
Abnormal breath testing is common in subjects with IBS. Normalization of the breath test with antibiotic treatment leads to a significant reduction in IBS symptoms.
Another study found that SIBO breath testing correlated with symptoms and did so more accurately than the gold standard of duodenal aspirates (taking a sample directly from the small intestine). In this study of sick patients, a lactulose SIBO breath test found SIBO whereas the direct sampling did not. When the sick patients were treated with antibiotics their symptoms improved and so did their SIBO breath tests. This likely indicates that the SIBO was out of sampling reach, or said another way, the SIBO was further down the intestinal tract than could be reached by the sampling device.
Elevated bacterial counts of questionable significance were found in duodenal aspirates before and after antibiotic treatment. There was no evidence of bile salt deconjugation or structural changes in the small intestine by light or electron microscopy. This may indicate that the site of colonization is distal to the biopsy site. Breath testing indicated lactose malabsorption in all patients.
Dietary restriction alone did not cause complete cessation of symptoms, whereas all patients responded dramatically to oral antibiotic therapy. When patients were well, the lactase-sucrase ratio had returned to normal in those tested, and all nine had normal lactose and lactulose breath hydrogen tests

“Normalization of breath test after antibiotic therapy is associated with a significant improvement of symptoms.”
It is also important to keep in mind most of the data here are refer to antibiotic treatment alone. The criticism is sometimes made that the level of improvement from antibiotic treatment is not impressive. I would agree. However, this does not mean that antibiotic, or herbal antimicrobial therapy is ineffective. Rather, what is means is this is one of a few treatment modalities that can be used together to achieve optimum results.
This is nothing new in medicine. A drug, or herb, alone is usually less effective than using said treatment in conjunction with dietary and lifestyle changes. This argument would be akin to saying if adrenal supporting herbs don’t lead to a near 100% resolution of fatigue they are ineffective. It would be foolish to suggest the only intervention for someone who is tired would be Ashwagandha. Yes, it can help, but for optimum results one should also be eating enough calories, a somewhat healthy diet, exercising, obtaining adequate sleep and managing stress.
Even though we have established that post-treatment SIBO retesting results tend to match symptomatic improvements, you don’t have to test and retest SIBO when treating SIBO. It is OK to use an approach that is exclusively guided by one’s symptoms. This was concluded by a systematic review in 2008, a systematic review is very similar to a meta-analysis and reviews the available data on an issue. Keep in mind this was ten years ago and we have sharpened our understanding regarding the SIBO breath test considerably since then.
…the most practical method to evaluate SIBO in studies at this time would be a test, treat, and outcome technique. Note: so essentially they are saying test and then treat until someone feels well.
How I use SIBO breath testing- Key Point
I usually test patients to get a baseline, but only in patients who have already taken some initial steps toward improving their gut health but are not feeling better. This usually means someone has tried at least one diet and/or one type of gut healing intervention like probiotics. If someone hasn’t done this we might forgo any/all testing and simply start with these basics. But, if someone has already taken these steps and is still not feeling well, then we perform a SIBO breath test. Once the test is preformed we have two paths we may traverse:
- Path one:
- Treat until an optimal symptomatic response is achieved
- Once this is achieved there is optional confirmatory retesting
- Path two:
- If optimal symptomatic improvement is not achieved after multiple treatment attempts, we retest to see how their SIBO status correlates with their current condition to guide future treatment
This approach seems reasonable because it is as effective as a more testing heavy method (in my observation), but I would argue produces results faster (because less time is allocated for retesting) and cheaper (because less testing expense is incurred).
Rapid transit may cause a false positive SIBO test. Meaning your test says you have SIBO but you really don’t, instead you have rapid transit – Incorrect
Data clearly show transit can influence test results, this is known and ads nothing new to the discussion. There are safeguards that can be taken to minimize the impact of transit time on SIBO breath testing results – which we have already covered and any good SIBO clinician will be doing.
Interpret lactulose testing conservatively by using a 90 min cutoff.
- Use correct dose of lactulose (10g) which minimizes accelerated transit.
- As we have discussed in our clinician newsletter and as outlined by American consensus
- And as other direct examination studies have concluded (84)
- Or, use the glucose test as advised by the Rome Foundation consensus paper discussed previously.
It is important to avoid only treating the test results. False positives can occur, meaning you can have a positive test result in someone who does not require treatment – like I outline in a case study with Bob
Altered transit may be CAUSED by SIBO and transit may improve from SIBO treatment – Key Point
While abnormal transit can skew results of a breath test, we also know bacterial overgrowth and the subsequent increased production of hydrogen and methane gas can alter transit (and specifically alter small intestinal motility). This is likely part of the reason why treatment of overgrowth can normalize breath testing results, because it can normalize transit. Here is this concept summarized.
- Abnormal bacteria (SIBO) = altered transit = abnormal breath test
- Normalized bacteria (from treatment) = normalized transit = normalized breath test
But, don’t take my word for it. Let’s see what the evidence says. The paper Methanogens, methane and gastrointestinal motility provides some important insights. Preliminary data is finding that methane gas causes delayed transit.
While a causative relation (constipation + methane) is not proven yet, there is strong evidence from animal studies that methane delays intestinal transit, possibly acting as a neuromuscular transmitter.
This evidence is further supported by the universal finding that methane production (measured by breath test) is associated with delayed transit time in clinical studies.
More importantly it has been shown that treatment of the SIBO-gas leads to improvement in transit.
There is also preliminary evidence that antibiotic reduction of methanogens (as evidenced by reduced methane production) predicts the clinical response in terms of symptomatic improvement in patients with constipation predominant irritable bowel syndrome.
The above is supported by several other studies. (88, 89, 90, 91, 92, 93)
However, there is also some data showing gas does not affect motility or transit time. (94, 95, 96, 97)
One critic misquotes his references, wherein he conflates what a fructose malabsorption tests shows to be equivalent to what a SIBO breath test shows.
One study saw that 67% of people tested get different results when retested 6 weeks later even though they were given no treatment or dietary change.
In fact, what he sites isn’t even a study, it’s a commentary on a study. This same critic makes the same mistake in yet another reference in his next paragraph….. again, citing a fructose malabsorption test to mean the same thing as a SIBO breath test, which it does not.
Some studies have shown repeat SIBO testing to be consistent. (100, 101, 102)
However this point is now moot in light of the high level science overview we have performed.
Researchers have abandoned SIBO – Incorrect.
A quick search on PubMed shows 30 studies published on SIBO from Jan to March of 2018. Also, two major bodies in gastroenterology (Rome and the North American Consensus) recently went through great lengths required to generate consensus statements for the proper use of the SIBO breath test. So how someone can make this statement is beyond me.
There is no such thing as SIBO – Incorrect.
This is too strong of a statement. The more one knows, the more cautious their statements tend to be. Strong statements usually reflect a degree of ignorance. It should be clear at this point that such a statement is clearly untenable.
Yes, there is controversy regarding the testing for SIBO. This is likely because not everyone with IBS has SIBO upon breath testing, but rather a subgroup of patients with IBS have SIBO.
“Breath testing is useful to identify a subgroup of IBS-like patients, whose symptoms are owing to SIBO” (103)
But because there is controversy regarding something does not mean it doesn’t exist. Most issues in science are shrouded in controversy. This is how we learn more, resolving the controversies with additional study.
Conventional or Natural Medicine?
Should you see a conventional or alternative provider for IBS (gas, bloating, abdominal pain, constipation and/or diarrhea)?
There is a balance to be struck here. On the one hand you should keep your conventional doctor in the loop so that you can obtain the care you need in a timely fashion. On the other hand, it’s important not to overreact and prematurely seek out imaging studies, endoscopies and the like which can be costly, unpleasant and invasive.
There are some simple, safe and natural interventions that could eliminate the need for a more costly and invasive evaluation. In studies that compare natural to pharmaceutical treatments for IBS, it’s fairly clear to see that, overall, natural therapies work better than pharmaceuticals. Drugs have a place in the treatment of IBS, but this is one area where diet and natural medicine appear superior. The most comprehensive plan I am aware of for IBS is the Healthy Gut, Healthy You protocol. This provides a system to personalize the available treatment options to your individual needs. So instead of randomly trying various therapies, you can apply the right therapy at the right time.
Give this a try and see how you do. You may see all your IBS and/or SIBO symptoms disappear. If so, great. If not, get your conventional doctor involved.
Always follow through with whatever routine evaluations have been recommended by your conventional doctors. Even if you prefer natural medicine make sure not to turn a blind eye to conventional medicine.
.
Overview of the conventional medicine screening process for those with IBS.
The Up-To-Date medical guidelines database offers the following recommendations, paraphrased.
- “In all patients with suspected IBS, we perform a complete blood count” Note: this is a simple, routine blood test.
- “In patients with diarrhea, we perform the following:
- C-reactive protein and/or fecal calprotectin
- Serologic testing for celiac disease”
- Note: they comment that cytolethal distending toxin B (CdtB) and vinculin antibodies require further validation before their use.
- Age appropriate colorectal screenings
- In patients with constipation
- Imaging and motility studies may be ordered
- In those with alarm features further examination may be advised including endoscopy, colonoscopy and imaging.
- Alarm features — Alarm features include [10]:
- Age of onset after age 50 years
- Rectal bleeding or melena
- Nocturnal diarrhea
- Progressive abdominal pain
- Unexplained weight loss
- Laboratory abnormalities (iron deficiency anemia, elevated C-reactive protein or fecal calprotectin)
- Family history of IBD or colorectal cancer
- Alarm features — Alarm features include [10]:
What To Do
One of the most prevalent problems I see in healthcare is not ‘starting with the gut’ and skipping over this foundational aspect of one’s health, instead pursuing things that are better addressed after optimizing gut health. This would include areas like adrenal health, hormones, detox, Lyme and mold.
SIBO breath testing is not perfect nor are the treatment options for IBS, but when used correctly, they can be very effective. Also remember that many non-digestive symptoms like fatigue, depression, insomnia, skin issues and potentially thyroid autoimmunity and metabolism, may improve after optimizing one’s gut health.
At the end of the day if you are working with a competent clinician or through a process that is attentive, conservative and will treat your gut holistically (instead of merely treating your lab tests) you should do very well.
What you should not do:
- Obsess over SIBO and/or your breath test results
- Treat only your SIBO labs
- Be treated for SIBO if you have no symptoms
- Eat or avoid foods because you think they are good or bad for SIBO
- Sporadically try digestive health treatments or use treatments that are non-validated
- Avoid conventional medicine
What you should do:
- Understand SIBO is a lab finding, not a life sentence of suffering and worry
- Use SIBO breath results, in addition to your history and current symptoms to determine the best treatment
- Listen to your body to find the foods that work best for you
- Apply the validated treatment for digestive healthy in a logical sequence of steps
- All of the above are outlined in Healthy Gut, Healthy You.
- Keep your conventional doctor in the loop, but hopefully you will not need any treatment after using natural interventions
I hope this article helps to prevent confusion and fear and allows you to improve your health quickly. I invite you to share your thoughts below.
Important Clarifications
1. https://www.ncbi.nlm.nih.gov/pubmed/28592442
2. https://michael-ruscio.preview21.rmkr.net/practitioner-2017-dec-research/#r4 (subscription required)
3. https://www.ncbi.nlm.nih.gov/pubmed/25174455
4. https://www.ncbi.nlm.nih.gov/pubmed/26987104
5. https://www.ncbi.nlm.nih.gov/pubmed/25918524
6. https://www.ncbi.nlm.nih.gov/pubmed/27588061
7. https://www.ncbi.nlm.nih.gov/pubmed/28737477
8. https://www.ncbi.nlm.nih.gov/pubmed/28592442
Points Where I Agree with Criticisms
9. https://www.ncbi.nlm.nih.gov/pubmed/24857420
10. https://www.ncbi.nlm.nih.gov/pubmed/19344474
Improvements with SIBO Symptoms
11. https://www.ncbi.nlm.nih.gov/pubmed/18456568
12. https://www.ncbi.nlm.nih.gov/pubmed/21570907
13. https://onlinelibrary.wiley.com/doi/10.1111/j.1479-8425.2012.00537.x/abstract
14. https://www.ncbi.nlm.nih.gov/pubmed/26833719
15. https://www.diabetesforecast.org/2012/nov/certain-bacteria-might-make-type-2-more-likely.html
16. https://www.ncbi.nlm.nih.gov/pubmed/22347829
17. https://www.ncbi.nlm.nih.gov/pubmed/23533244
18. https://www.ncbi.nlm.nih.gov/pubmed/27509521
19. https://michael-ruscio.preview21.rmkr.net/gut-autoimmune-connection-sibo-ra/
20. https://www.ncbi.nlm.nih.gov/pubmed/17308218
21. https://www.ncbi.nlm.nih.gov/pubmed/12738465
22. https://www.ncbi.nlm.nih.gov/pubmed/23715643
23. https://www.ncbi.nlm.nih.gov/pubmed/18416345
24. https://www.ncbi.nlm.nih.gov/pubmed/15154971
Points Where I Disagree
Diets for SIBO
25. https://www.ncbi.nlm.nih.gov/pubmed/25982757
26. https://www.ncbi.nlm.nih.gov/pubmed/29129233
27. https://www.ncbi.nlm.nih.gov/pubmed/28846594
28. https://www.ncbi.nlm.nih.gov/pubmed/28592442
29. https://www.ncbi.nlm.nih.gov/pubmed/28850525
30. https://www.ncbi.nlm.nih.gov/pubmed/26976734
31. https://www.ncbi.nlm.nih.gov/pubmed/27397586
Koch’s Postulate
32. https://www.ncbi.nlm.nih.gov/pubmed/17889443
33. https://michael-ruscio.preview21.rmkr.net/getgutbook/
34. https://www.ncbi.nlm.nih.gov/pubmed/26828918
35. https://www.ncbi.nlm.nih.gov/pubmed/24192039
Treatment for SIBO
36. https://www.ncbi.nlm.nih.gov/pubmed/28078798
37. https://www.ncbi.nlm.nih.gov/pubmed/21389791
38. https://en.wikipedia.org/wiki/Publication_bias
39. https://www.ncbi.nlm.nih.gov/pubmed/21389791
40. https://store.michael-ruscio.preview21.rmkr.net/products/peppermint-oil
41. https://store.michael-ruscio.preview21.rmkr.net/pages/step-2
Probiotics
42. https://www.ncbi.nlm.nih.gov/pubmed/23703468
43. https://www.ncbi.nlm.nih.gov/pubmed/20922415
44. https://www.ncbi.nlm.nih.gov/pubmed/29508268
45. https://www.ncbi.nlm.nih.gov/pubmed/28267052
46. https://www.ncbi.nlm.nih.gov/pubmed/21381407
47. https://www.ncbi.nlm.nih.gov/pubmed/18763284
48. https://www.ncbi.nlm.nih.gov/pubmed/19352343
49. https://store.michael-ruscio.preview21.rmkr.net/pages/step-2
Low FODMAP Diet
50. https://michael-ruscio.preview21.rmkr.net/gutbook-resources/
51. https://www.ncbi.nlm.nih.gov/pubmed/25410635
Herbal Antimicrobials
52. https://www.ncbi.nlm.nih.gov/pubmed/26400188
53. https://www.ncbi.nlm.nih.gov/pubmed/24891990
54. https://www.ncbi.nlm.nih.gov/pubmed/29197739
55. https://www.ncbi.nlm.nih.gov/pubmed/?term=24039370
56. https://www.ncbi.nlm.nih.gov/pubmed/21205415
57. https://www.ncbi.nlm.nih.gov/pubmed/27163246
58. https://www.ncbi.nlm.nih.gov/pubmed/27163246
59. https://michael-ruscio.preview21.rmkr.net/patient-conversations/
Long Term Treatment
60. https://www.ncbi.nlm.nih.gov/pubmed/17000196
61. https://michael-ruscio.preview21.rmkr.net/patient-conversations/
62. https://michael-ruscio.preview21.rmkr.net/getgutbook/
SIBO Testing
63. https://www.ncbi.nlm.nih.gov/pubmed/28323273
64. https://www.ncbi.nlm.nih.gov/pubmed/19344474
65. https://www.ncbi.nlm.nih.gov/pubmed/19344474
66. https://www.ncbi.nlm.nih.gov/pubmed/28323273
67. https://www.ncbi.nlm.nih.gov/pubmed/25600077
68. https://www.ncbi.nlm.nih.gov/pubmed/8636812
69. https://www.ncbi.nlm.nih.gov/pubmed/3410238
70. https://www.ncbi.nlm.nih.gov/pubmed/2295385
71. https://www.ncbi.nlm.nih.gov/pubmed/8792701
72. https://www.ncbi.nlm.nih.gov/pubmed/19344474
73. https://www.ncbi.nlm.nih.gov/pubmed/28323273
74. https://www.ncbi.nlm.nih.gov/pubmed/20467896
75. https://www.ncbi.nlm.nih.gov/pubmed/21286935
76. https://www.ncbi.nlm.nih.gov/pubmed/20467896
77. https://www.ncbi.nlm.nih.gov/pubmed/21286935
78. https://www.ncbi.nlm.nih.gov/pubmed/12591062
79. https://pediatrics.aappublications.org/content/74/2/229
80. https://www.ncbi.nlm.nih.gov/pubmed/19525858
81. https://www.ncbi.nlm.nih.gov/pubmed/17990113
Rapid & Altered Transit
82. https://michael-ruscio.preview21.rmkr.net/practitioner-2017-jun-research/#r2
83. https://www.ncbi.nlm.nih.gov/pubmed/28323273
84. https://www.ncbi.nlm.nih.gov/pubmed/2377020
85. https://www.ncbi.nlm.nih.gov/pubmed/19344474
86. https://michael-ruscio.preview21.rmkr.net/living-well-sibo-cast-study-follow/
87. https://www.ncbi.nlm.nih.gov/pubmed/24466443
88. https://www.ncbi.nlm.nih.gov/pubmed/21286935
89. https://www.ncbi.nlm.nih.gov/pubmed/16293652
90. https://www.ncbi.nlm.nih.gov/pubmed/12645795
91. https://www.ncbi.nlm.nih.gov/pubmed/19830557
92. https://www.ncbi.nlm.nih.gov/pubmed/24247567
93. https://www.ncbi.nlm.nih.gov/pubmed/22097886
94. https://www.ncbi.nlm.nih.gov/pubmed/29497795
95. https://www.ncbi.nlm.nih.gov/pubmed/28417537
96. https://www.ncbi.nlm.nih.gov/pubmed/28295896
97. https://www.ncbi.nlm.nih.gov/pubmed/24503633
SIBO Breath Test
98. https://www.ncbi.nlm.nih.gov/pubmed/23855397
99. https://www.ncbi.nlm.nih.gov/pubmed/23002720
100. https://www.ncbi.nlm.nih.gov/pubmed/4096490
101. https://www.ncbi.nlm.nih.gov/pubmed/7811826
102. https://www.ncbi.nlm.nih.gov/pubmed/3197582
103. https://www.ncbi.nlm.nih.gov/pubmed/19525858
Conventional or Natural Medicine
104. https://michael-ruscio.preview21.rmkr.net/getgutbook/
105. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-irritable-bowel-syndrome-in-adults?search=ibs%20diagnosis&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H3710510959
106. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-irritable-bowel-syndrome-in-adults/abstract/10
What do you think? I would like to hear your thoughts or experience with this.
- Get help with Small Intestinal Bacterial Overgrowth (SIBO).
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.

 Interpret lactulose testing conservatively by using a 90 min cutoff.
Interpret lactulose testing conservatively by using a 90 min cutoff.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!