How to Boost Your Brain Through Neuroplasticity Healing
Rewiring Your Brain for Mind-Body Healing
- Understanding Neuroplasticity & Limbic System|
- Benefits of Neuroplasticity Healing|
- How Neuroplasticity Training Works|
- Lifestyle Changes to Boost Neuroplasticity|
- Other Healing Tips|
- Recommended Products|
- Neuroplasticity healing or limbic system retraining may help to improve pain, anxiety, stress response, and cognition.
- Neuroplasticity healing requires the right fundamentals — diet, sleep, and gut health maintenance — to allow the adult brain to form new neural pathways and learn new skills.
- Imbalances in your gut microbiome can affect cognitive, emotional, and mental health via the gut-brain axis (the millions of neurons running between your gut and brain cells).
- For those who have improved diet, lifestyle, and gut health, but still feel unwell, reprogramming nervous system responses through neuroplasticity training may be a powerful next step.
Can you change your brain in order to improve your health?
Neuroscientists and clinicians once believed that only people younger than 25 had a malleable brain, but this is now known not to be true.
In fact, the ability of the human brain and its complex neurological circuitry to make new connections and be adaptive to change can also happen in the more mature brain. This ability is called neuroplasticity or neural plasticity [1].
In a medical context, neuroplasticity shows up as the rewiring of parts of the brain to help improve chronic pain or heal brain damage. The ability of the brain to recover in stroke patients, or after traumatic brain injury is a good example of neuroplasticity healing in action.
Neuroplasticity or limbic system training may also be able to help with trauma healing, emotional regulation, and anxiety by retraining nervous system responses that have become “stuck” over time.
If you’ve been struggling with a chronic illness or symptoms for some time, neuroplasticity healing might be the missing link to bring you back to your healthiest self.
Or, if you’re generally feeling well but looking to improve your cognitive health, diet and lifestyle changes aimed at improving brain plasticity can help to sharpen your learning, memory, and focus.
What Is Neuroplasticity Healing?
Neuroplasticity healing refers to the lifestyle changes and brain exercises that can help the neural connections in your brain continue developing and changing.
Some diet and lifestyle changes can help to increase neuroplasticity along with overall health. There are also a number of programs aimed specifically at retraining the brain and nervous system, and reprogramming emotional responses.
These may be referred to as neuroplasticity training, limbic system retraining, or amygdala retraining (the latter two referring to specific components of the nervous system, which we’ll cover below).
Neuroplasticity healing programs typically involve a combination of meditation, breathwork, visualization, and behavioral exercises.
Understanding the Limbic System and the Amygdala
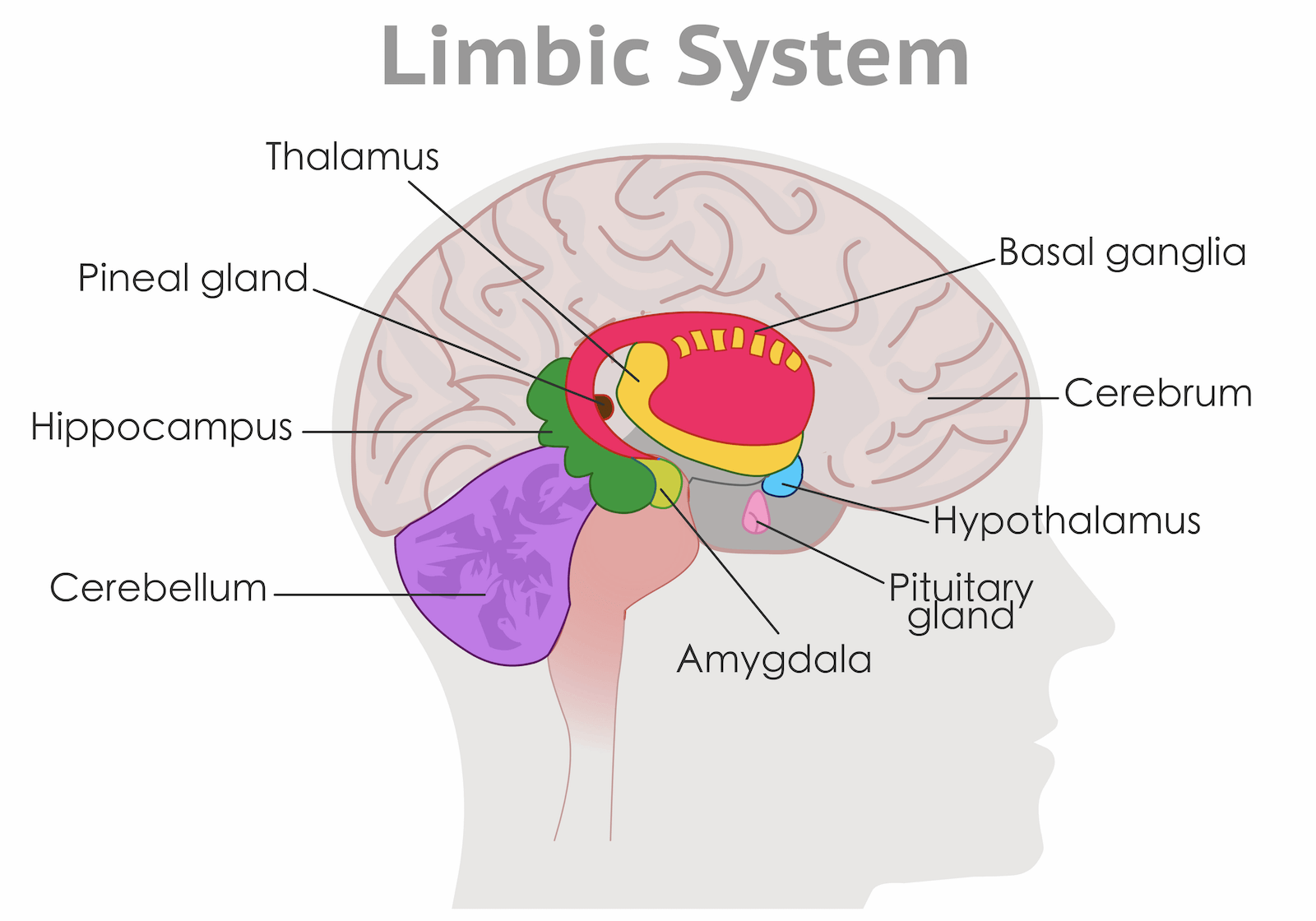
The limbic system is a group of structures in the brain that regulates behavior, emotion, and memory. The amygdala is one component of the limbic system and is connected to emotional memory and response, including the “fight or flight” response to danger or stress.
Benefits of Neuroplasticity Healing or Limbic System Retraining
Although research is still in its infancy, some studies suggest that limbic system retraining programs may lead to the following benefits [2, 3, 4, 5]:
- Pain reduction for those with fibromyalgia or chronic fatigue syndrome
- Reduced anxiety
- Improved stress response
- Increased mindfulness
- Better sleep
- Increased energy
- Reduced levels of depression
One 2020 pilot randomized controlled trial involving patients with fibromyalgia found that, compared to a relaxation therapy, an amygdala retraining program led to improvements in pain, anxiety, depression, and even mindfulness and self-compassion [1].
What’s really interesting about this study is that three months after treatment had ended, the limbic system retraining group still had not only improved pain and symptoms but significant improvements in “pain catastrophizing” and “psychological rigidity.” In other words, it wasn’t just their pain that had improved, but their response to pain, and their mental or emotional ability to cope.
Can Limbic System Retraining Help with Anxiety and Chronic Illness Healing?

The fact that our brains can create and strengthen neural pathways when we learn or are faced with something new is a good thing. But what does this mean for those who have been through a traumatic event or are dealing with a chronic illness? According to the limbic system or amygdala theory, the nervous system may have learned to become overly sensitive or responsive to certain triggers — even after they’ve stopped being harmful.
For example, if you have dealt with reactivity to food or supplements for several months or even years, paired with chronic symptoms like fatigue, brain fog, bloating, or constipation, your limbic system may have learned to associate food, supplements, or mild symptoms with danger.
Even if you’ve healed your gut, improved the health of your immune system, and resolved the majority of the underlying issues that led to your symptoms, your brain could still be responding to food or any hint of symptoms the way it’s been trained to: essentially, by making you anxious.
And that’s where neuroplasticity healing or training comes in. The goal is to rewire those neural pathways and reprogram the responses that might be keeping you “stuck” even after your body has healed.
It’s worth noting that research in this area is still quite limited. However, I’ve found with my patients that for those who have done the work when it comes to diet, lifestyle, and gut healing, and whose conditions have objectively improved but who are still feeling unwell, this type of training can be incredibly powerful and helpful.
How Neuroplasticity Training Works
What’s actually involved in a neuroplasticity or limbic system training program? There are a number of different programs available whose approaches may vary slightly. Generally, a limbic system retraining program will last for several weeks to several months, broken down into short regular sessions.
Neuroplasticity retraining typically involves specifically targeted programs that combine multiple mind-body modalities. These may include:
- Meditation or mindfulness training
- Breathwork
- Visualization
- Cognitive behavioral therapy
- Personalized coaching
- Therapies aimed at emotional restructuring
How to Encourage Neuroplasticity
Beyond limbic system or amygdala retraining programs, there are many diet and lifestyle strategies that can help to encourage neuroplasticity. Tips for boosting neuroplasticity may include:
- Improving gut health and the gut-brain connection
- Reducing brain inflammation, through:
- An anti-inflammatory diet
- Improving the health of your gut bacteria
- Getting better sleep (or improving your sleep hygiene)
- Physical activity
Let’s go through some of these areas in more detail.
Neuroplasticity, Cognition, and Your Gut
A sluggish brain and poor cognitive function might actually relate to what is going on with your gut bacteria.
The science linking the brain and gut health is far from fully developed, but it shows that:
- There is constant two-way communication from your microbiota to your brain and the other way around, via nervous and immune systems and hormonal signaling [6].
- Disruptions to your microbiome can impair these communication pathways between gut and brain [7].
- The microbiome also influences gut production of important transmitters (such as dopamine, serotonin, and GABA), which play a key role in affecting mood [8, 9].
Brain inflammation is one of the primary contributory factors to brain fog [10, 11, 12] and may also reduce neuroplasticity [13]. Unfortunately, imbalances in the gut microbiome have been shown to produce inflammation in the brain [7, 14, 15, 16, 17].
Cognitive symptoms like brain fog have also been associated with irritable bowel syndrome (IBS), Crohn’s disease, small intestinal bacterial overgrowth (SIBO), and gluten sensitivity, further reinforcing a gut/brain link [18, 19, 20, 21, 22].
Lifestyle Changes to Boost Neuroplasticity and Cognition
Before jumping into neuroplasticity training or cognitive enhancement supplements, it’s important to get the lifestyle basics (diet, sleep, exercise) right.
Brain Boost Diet
Avoiding foods that cause inflammation, such as sugar, alcohol, deep fried foods, and highly processed foods is your first step towards healthier brain function.
Most healthy diets include plenty of anti-inflammatory foods, which encourage a more neuroplastic brain.
Cutting out the junk and eating whole, unprocessed foods should bring benefits, but specifically, polyphenols, found in colorful vegetables and fruits, tea, and some herbs have been linked with improved neuroplasticity [23].

The Mediterranean diet, which is rich in polyphenols, has been the most tested for its impacts on cognitive function. For example:
- A 2016 review of 32 studies associated the Mediterranean diet with improved cognitive function, a decreased risk of cognitive impairment, and decreased risk of dementia. However, results were not consistent and some of the studies reviewed found no association between diet and improved cognitive function [24].
- A 2018 systematic review found that a Mediterranean diet improved 12.1% of outcomes on cognitive tests [25]. Overall, the researchers found the evidence was inconclusive but noted the significant cognitive improvements
I also get good reports of cognitive improvements from my patients who are following a Paleo diet. The paleo and Mediterranean diets are very similar, but paleo also cuts down on carbs [26]. Paleo also restricts gluten and dairy, which are some of the most common food intolerances.
Whichever diet you choose, aim to include plenty of oily fish as its omega-3s content has been linked with better cognition [26, 27]. If not, you may want to take a DHA/EPA supplement.
Quality Sleep

Most people need 7-8 hours of good quality sleep a night to ensure good cognitive function and maintain good neuroplasticity. Neurology research shows us that a good night’s shuteye improves learning outcomes, restores the synapses (junctions) between nerve cells, solidifies memories, and removes brain waste [28].
On the other hand a lack of sleep can lead to leaky gut, which can contribute to systemic inflammation, including brain inflammation [28, 29].
Monitoring your sleep is worth investing in. Two of my recommendations for doing this are the Oura Ring and WatchPat One — worth checking out if you wake up groggy and brain fogged and would like some feedback on how to sleep better.
Regular Exercise
Daily exercise is vital for concentration, focus, and mood. Each week, you should try to fit in 150 minutes of moderate or 75 minutes of vigorous exercise. This can be spread over several short (5-10 minute) bursts if you prefer.
Research shows that working out helps to [30]:
- Improve neuroplasticity by altering the structure and function of synapses in parts of the brain (including the hippocampus, which plays a big role in learning and memory).
- Increase the density and size of cortical neurons (never cells in the brain’s cortex), which could also positively impact memory, attention and perception.
When you raise your heart rate and get a sweat on, levels of brain-derived neurotrophic factor (BDNF) also rise. BDNF is a molecule with a key role in neuroplastic changes related to beneficial learning and memory [31].
More generally, exercise helps to decrease systemic inflammation and improve sleep quality — two factors that can directly affect cognitive function [32, 33].
In older people, research shows that exercise may improve mild cognitive impairment [34].
Probiotics for the Gut-Brain Axis

When you’ve already taken steps to eat well, sleep better and get moving, you can support these new foundations with probiotic supplements that feed your gut with healthy bacteria.
The idea that probiotics can be very helpful in promoting mental health and wellness is more than just theoretical. Scientific research shows that probiotics can:
- Help to prevent inflammatory neurodegeneration [35]
- Improve cognition in patients with IBS, fibromyalgia and Alzheimer’s [36, 37, 38, 39, 40]
- Improve moods in people with mild to moderate depression, potentially help major depressive disorder, and have an anti-anxiety effect [41, 42, 43, 44]
- Improve stress, anxiety, memory, social emotional cognition, and verbal learning for adults who have been experiencing emotional stress [45]
Other Neuroplasticity Healing Tips and Tricks
Some evidence suggests that you may also get cognitive gains through certain kinds of supplements, brain training games, and even sauna therapy.
Supplements for Cognitive Enhancement

If your diet and lifestyle foundations are in place and your cognition needs some fine tuning, supplements may be of help. A few research-backed options for improving cognitive function include lion’s mane [46], citicoline [47, 48, 49], ashwagandha [50], ginkgo biloba [51], and turmeric [52].
Brain Training
The theory behind brain training aids and apps is that they use techniques from the world of neuroscience to offer targeted mental stimulation. In turn, this reorganizes connections between brain cells, improving brain neuroplasticity.
- One study found that young adults who used brain training games had gains in brain processing speed, working memory, and executive functions like flexible thinning and self control [53].
- A 2020 systematic review and meta analysis, this time involving adults over 60 without cognitive impairment, found that computerized brain training programs also significantly improved their processing speed, working memory, executive function, and verbal memory, but not attention or visual-spatial processing [54].
Two brain training apps that I like are BrainHQ and CogniFit. But the evidence for brain training is mixed — as well as the positive studies above, other studies have failed to find a benefit [55, 56, 57].
Sauna Therapy

If you have access to a sauna, this could be another way to give yourself a brain boost. The evidence here isn’t strong, but it’s intriguing. For example, observational studies have shown that:
- Young men’s brains were more relaxed and more efficient at performing auditory and visual tasks 90 minutes after sauna bathing (at 101.3 – 103.3 F) [58].
- People who took saunas 9-12 times per month were less likely to develop dementia than those who sauna bathed 0-3 times per month [59].
Exactly why saunas are so beneficial is uncertain. However, heat therapy can cause activation of heat shock proteins, which may be part of the brain’s way of healing itself from neurodegenerative attack and benefiting muscle function and brain blood flow [60].
As well as the potential mental health benefits, saunas, and other heat and soak therapies have been shown to have physical benefits including:
- Improving cardiovascular health and reducing high blood pressure [61]
- Reducing stress and chronic pain [62]
- Improving metabolism markers, like fasting blood glucose
More research is needed, but if you have the opportunity to take a hot bath or sauna on a regular basis it’s worth doing — after all it’s a very soothing thing to do anyway.
The Bottom Line
In summary, you can encourage an adaptable, neuroplastic, healthy brain by working on your diet, sleep and exercise. And if you feel like you’ve hit a wall with your treatment for chronic illness or symptoms, a neuroplasticity or limbic system retraining program might be able to help.
Sometimes, unpacking what aspect of your diet or lifestyle might be causing your brain fog or lack of focus is hard to do without professional help. Consider making an appointment with myself or someone on my team for personalized help.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Park DC, Bischof GN. The aging mind: neuroplasticity in response to cognitive training. Dialogues Clin Neurosci. 2013 Mar;15(1):109–19. PMID: 23576894. PMCID: PMC3622463.
- Carleton RN, Asmundson GJG, Korol SL, LeBouthillier DM, Hozempa K, Katz JD, et al. Evaluating the efficacy of an attention modification program for patients with fibromyalgia: a randomized controlled trial. Pain. 2020 Mar;161(3):584–94. DOI: 10.1097/j.pain.0000000000001746. PMID: 31693540.
- Goldway N, Ablin J, Lubin O, Zamir Y, Keynan JN, Or-Borichev A, et al. Volitional limbic neuromodulation exerts a beneficial clinical effect on Fibromyalgia. Neuroimage. 2019 Feb 1;186:758–70. DOI: 10.1016/j.neuroimage.2018.11.001. PMID: 30408596.
- Sanabria-Mazo JP, Montero-Marin J, Feliu-Soler A, Gasión V, Navarro-Gil M, Morillo-Sarto H, et al. Mindfulness-Based Program Plus Amygdala and Insula Retraining (MAIR) for the Treatment of Women with Fibromyalgia: A Pilot Randomized Controlled Trial. J Clin Med. 2020 Oct 11;9(10). DOI: 10.3390/jcm9103246. PMID: 33050630. PMCID: PMC7599726.
- Toussaint LL, Whipple MO, Abboud LL, Vincent A, Wahner-Roedler DL. A mind-body technique for symptoms related to fibromyalgia and chronic fatigue. Explore (NY). 2012 Apr;8(2):92–8. DOI: 10.1016/j.explore.2011.12.003. PMID: 22385563.
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015 Jun;28(2):203–9. PMID: 25830558. PMCID: PMC4367209.
- Bravo JA, Julio-Pieper M, Forsythe P, Kunze W, Dinan TG, Bienenstock J, et al. Communication between gastrointestinal bacteria and the nervous system. Curr Opin Pharmacol. 2012 Dec;12(6):667–72. DOI: 10.1016/j.coph.2012.09.010. PMID: 23041079.
- Lyte M. Microbial endocrinology in the microbiome-gut-brain axis: how bacterial production and utilization of neurochemicals influence behavior. PLoS Pathog. 2013 Nov 14;9(11):e1003726. DOI: 10.1371/journal.ppat.1003726. PMID: 24244158. PMCID: PMC3828163.
- Tran N, Zhebrak M, Yacoub C, Pelletier J, Hawley D. The gut-brain relationship: Investigating the effect of multispecies probiotics on anxiety in a randomized placebo-controlled trial of healthy young adults. J Affect Disord. 2019 Jun 1;252:271–7. DOI: 10.1016/j.jad.2019.04.043. PMID: 30991255.
- Jones KA, Thomsen C. The role of the innate immune system in psychiatric disorders. Mol Cell Neurosci. 2013 Mar;53:52–62. DOI: 10.1016/j.mcn.2012.10.002. PMID: 23064447.
- Conti P, D’Ovidio C, Conti C, Gallenga CE, Lauritano D, Caraffa A, et al. Progression in migraine: Role of mast cells and pro-inflammatory and anti-inflammatory cytokines. Eur J Pharmacol. 2019 Feb 5;844:87–94. DOI: 10.1016/j.ejphar.2018.12.004. PMID: 30529470.
- Theoharides TC, Stewart JM, Hatziagelaki E, Kolaitis G. Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015 Jul 3;9:225. DOI: 10.3389/fnins.2015.00225. PMID: 26190965. PMCID: PMC4490655.
- Calabrese F, Rossetti AC, Racagni G, Gass P, Riva MA, Molteni R. Brain-derived neurotrophic factor: a bridge between inflammation and neuroplasticity. Front Cell Neurosci. 2014 Dec 22;8:430. DOI: 10.3389/fncel.2014.00430. PMID: 25565964. PMCID: PMC4273623.
- Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol. 2014 Oct 21;20(39):14105–25. DOI: 10.3748/wjg.v20.i39.14105. PMID: 25339800. PMCID: PMC4202342.
- Lin L, Zheng LJ, Zhang LJ. Neuroinflammation, gut microbiome, and alzheimer’s disease. Mol Neurobiol. 2018 Nov;55(11):8243–50. DOI: 10.1007/s12035-018-0983-2. PMID: 29524051.
- Sun M-F, Shen Y-Q. Dysbiosis of gut microbiota and microbial metabolites in Parkinson’s Disease. Ageing Res Rev. 2018 Aug;45:53–61. DOI: 10.1016/j.arr.2018.04.004. PMID: 29705121.
- Dopkins N, Nagarkatti PS, Nagarkatti M. The role of gut microbiome and associated metabolome in the regulation of neuroinflammation in multiple sclerosis and its implications in attenuating chronic inflammation in other inflammatory and autoimmune disorders. Immunology. 2018 Feb 27;154(2):178–85. DOI: 10.1111/imm.12903. PMID: 29392733. PMCID: PMC5980216.
- van Langenberg DR, Yelland GW, Robinson SR, Gibson PR. Cognitive impairment in Crohn’s disease is associated with systemic inflammation, symptom burden and sleep disturbance. United European Gastroenterol J. 2017 Jun;5(4):579–87. DOI: 10.1177/2050640616663397. PMID: 28588890. PMCID: PMC5446137.
- Isasi C, Tejerina E, Morán LM. Non-celiac gluten sensitivity and rheumatic diseases. Reumatol Clin. 2016 Feb;12(1):4–10. DOI: 10.1016/j.reuma.2015.03.001. PMID: 25956352.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR, Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12(1):85. DOI: 10.1186/1741-7015-12-85. PMID: 24885375. PMCID: PMC4053283.
- Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020 Jul 10;11:664. DOI: 10.3389/fpsyt.2020.00664. PMID: 32754068. PMCID: PMC7366247.
- Rao SSC, Rehman A, Yu S, Andino NM de. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018 Jun 19;9(6):162. DOI: 10.1038/s41424-018-0030-7. PMID: 29915215. PMCID: PMC6006167.
- Murphy T, Dias GP, Thuret S. Effects of diet on brain plasticity in animal and human studies: mind the gap. Neural Plast. 2014 May 12;2014:563160. DOI: 10.1155/2014/563160. PMID: 24900924. PMCID: PMC4037119.
- Petersson SD, Philippou E. Mediterranean diet, cognitive function, and dementia: A systematic review of the evidence. Adv Nutr. 2016 Sep 15;7(5):889–904. DOI: 10.3945/an.116.012138. PMID: 27633105. PMCID: PMC5015034.
- Radd-Vagenas S, Duffy SL, Naismith SL, Brew BJ, Flood VM, Fiatarone Singh MA. Effect of the Mediterranean diet on cognition and brain morphology and function: a systematic review of randomized controlled trials. Am J Clin Nutr. 2018 Mar 1;107(3):389–404. DOI: 10.1093/ajcn/nqx070. PMID: 29566197.
- Jönsson T, Granfeldt Y, Ahrén B, Branell U-C, Pålsson G, Hansson A, et al. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: a randomized cross-over pilot study. Cardiovasc Diabetol. 2009 Jul 16;8:35. DOI: 10.1186/1475-2840-8-35. PMID: 19604407. PMCID: PMC2724493.
- Masharani U, Sherchan P, Schloetter M, Stratford S, Xiao A, Sebastian A, et al. Metabolic and physiologic effects from consuming a hunter-gatherer (Paleolithic)-type diet in type 2 diabetes. Eur J Clin Nutr. 2015 Aug;69(8):944–8. DOI: 10.1038/ejcn.2015.39. PMID: 25828624.
- Wigren H-K, Stenberg T. [How does sleeping restore our brain?]. Duodecim. 2015;131(2):151–6. PMID: 26237917.
- Swanson GR, Burgess HJ. Sleep and circadian hygiene and inflammatory bowel disease. Gastroenterol Clin North Am. 2017 Dec;46(4):881–93. DOI: 10.1016/j.gtc.2017.08.014. PMID: 29173529.
- Lin T-W, Tsai S-F, Kuo Y-M. Physical exercise enhances neuroplasticity and delays alzheimer’s disease. Brain Plast. 2018 Dec 12;4(1):95–110. DOI: 10.3233/BPL-180073. PMID: 30564549. PMCID: PMC6296269.
- Miranda M, Morici JF, Zanoni MB, Bekinschtein P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front Cell Neurosci. 2019 Aug 7;13:363. DOI: 10.3389/fncel.2019.00363. PMID: 31440144. PMCID: PMC6692714.
- Kelley GA, Kelley KS. Exercise and sleep: a systematic review of previous meta-analyses. J Evid Based Med. 2017 Feb;10(1):26–36. DOI: 10.1111/jebm.12236. PMID: 28276627. PMCID: PMC5527334.
- Petersen AMW. The anti-inflammatory effect of exercise. J Appl Physiol. 2005 Apr 1;98(4):1154–62. DOI: 10.1152/japplphysiol.00164.2004. PMID: 15772055.
- Biazus-Sehn LF, Schuch FB, Firth J, Stigger F de S. Effects of physical exercise on cognitive function of older adults with mild cognitive impairment: A systematic review and meta-analysis. Arch Gerontol Geriatr. 2020 May 12;89:104048. DOI: 10.1016/j.archger.2020.104048. PMID: 32460123.
- Alexandrov P, Zhai Y, Li W, Lukiw W. Lipopolysaccharide-stimulated, NF-kB-, miRNA-146a- and miRNA-155-mediated molecular-genetic communication between the human gastrointestinal tract microbiome and the brain. Folia Neuropathol. 2019;57(3):211–9. DOI: 10.5114/fn.2019.88449. PMID: 31588707.
- Roman P, Estévez AF, Miras A, Sánchez-Labraca N, Cañadas F, Vivas AB, et al. A pilot randomized controlled trial to explore cognitive and emotional effects of probiotics in fibromyalgia. Sci Rep. 2018 Jul 19;8(1):10965. DOI: 10.1038/s41598-018-29388-5. PMID: 30026567. PMCID: PMC6053373.
- Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014 May 28;20(20):6024–30. DOI: 10.3748/wjg.v20.i20.6024. PMID: 24876725. PMCID: PMC4033442.
- Frändemark Å, Jakobsson Ung E, Törnblom H, Simrén M, Jakobsson S. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil. 2017 Jan;29(1). DOI: 10.1111/nmo.12898. PMID: 27401139.
- Akbari E, Asemi Z, Daneshvar Kakhaki R, Bahmani F, Kouchaki E, Tamtaji OR, et al. Effect of Probiotic Supplementation on Cognitive Function and Metabolic Status in Alzheimer’s Disease: A Randomized, Double-Blind and Controlled Trial. Front Aging Neurosci. 2016 Nov 10;8:256. DOI: 10.3389/fnagi.2016.00256. PMID: 27891089. PMCID: PMC5105117.
- Tamtaji OR, Heidari-Soureshjani R, Mirhosseini N, Kouchaki E, Bahmani F, Aghadavod E, et al. Probiotic and selenium co-supplementation, and the effects on clinical, metabolic and genetic status in Alzheimer’s disease: A randomized, double-blind, controlled trial. Clin Nutr. 2019 Dec;38(6):2569–75. DOI: 10.1016/j.clnu.2018.11.034. PMID: 30642737.
- Ng QX, Peters C, Ho CYX, Lim DY, Yeo W-S. A meta-analysis of the use of probiotics to alleviate depressive symptoms. J Affect Disord. 2018 Mar 1;228:13–9. DOI: 10.1016/j.jad.2017.11.063. PMID: 29197739.
- Akkasheh G, Kashani-Poor Z, Tajabadi-Ebrahimi M, Jafari P, Akbari H, Taghizadeh M, et al. Clinical and metabolic response to probiotic administration in patients with major depressive disorder: A randomized, double-blind, placebo-controlled trial. Nutrition. 2016 Mar;32(3):315–20. DOI: 10.1016/j.nut.2015.09.003. PMID: 26706022.
- Yang B, Wei J, Ju P, Chen J. Effects of regulating intestinal microbiota on anxiety symptoms: A systematic review. Gen Psych. 2019 May 17;32(2):e100056. DOI: 10.1136/gpsych-2019-100056. PMID: 31179435. PMCID: PMC6551444.
- Rao AV, Bested AC, Beaulne TM, Katzman MA, Iorio C, Berardi JM, et al. A randomized, double-blind, placebo-controlled pilot study of a probiotic in emotional symptoms of chronic fatigue syndrome. Gut Pathog. 2009 Mar 19;1(1):6. DOI: 10.1186/1757-4749-1-6. PMID: 19338686. PMCID: PMC2664325.
- Lew L-C, Hor Y-Y, Yusoff NAA, Choi S-B, Yusoff MSB, Roslan NS, et al. Probiotic Lactobacillus plantarum P8 alleviated stress and anxiety while enhancing memory and cognition in stressed adults: A randomised, double-blind, placebo-controlled study. Clin Nutr. 2019;38(5):2053–64. DOI: 10.1016/j.clnu.2018.09.010. PMID: 30266270.
- Saitsu Y, Nishide A, Kikushima K, Shimizu K, Ohnuki K. Improvement of cognitive functions by oral intake of Hericium erinaceus. Biomed Res. 2019;40(4):125–31. DOI: 10.2220/biomedres.40.125. PMID: 31413233.
- Que D-LS, Jamora RDG. Citicoline as adjuvant therapy in parkinson’s disease: A systematic review. Clin Ther. 2021;43(1):e19–31. DOI: 10.1016/j.clinthera.2020.11.009. PMID: 33279231.
- Jasielski P, Piędel F, Piwek M, Rocka A, Petit V, Rejdak K. Application of citicoline in neurological disorders: A systematic review. Nutrients. 2020 Oct 12;12(10). DOI: 10.3390/nu12103113. PMID: 33053828. PMCID: PMC7601330.
- Fioravanti M, Buckley AE. Citicoline (Cognizin) in the treatment of cognitive impairment. Clin Interv Aging. 2006;1(3):247–51. DOI: 10.2147/ciia.2006.1.3.247. PMID: 18046877. PMCID: PMC2695184.
- Ng QX, Loke W, Foo NX, Tan WJ, Chan HW, Lim DY, et al. A systematic review of the clinical use of Withania somnifera (Ashwagandha) to ameliorate cognitive dysfunction. Phytother Res. 2020 Mar;34(3):583–90. DOI: 10.1002/ptr.6552. PMID: 31742775.
- Liao Z, Cheng L, Li X, Zhang M, Wang S, Huo R. Meta-analysis of Ginkgo biloba Preparation for the Treatment of Alzheimer’s Disease. Clin Neuropharmacol. 2020;43(4):93–9. DOI: 10.1097/WNF.0000000000000394. PMID: 32658034.
- Small GW, Siddarth P, Li Z, Miller KJ, Ercoli L, Emerson ND, et al. Memory and Brain Amyloid and Tau Effects of a Bioavailable Form of Curcumin in Non-Demented Adults: A Double-Blind, Placebo-Controlled 18-Month Trial. Am J Geriatr Psychiatry. 2018 Mar;26(3):266–77. DOI: 10.1016/j.jagp.2017.10.010. PMID: 29246725.
- Wang G, Zhao M, Yang F, Cheng LJ, Lau Y. Game-based brain training for improving cognitive function in community-dwelling older adults: A systematic review and meta-regression. Arch Gerontol Geriatr. 2021;92:104260. DOI: 10.1016/j.archger.2020.104260. PMID: 32980574.
- Bonnechère B, Langley C, Sahakian BJ. The use of commercial computerised cognitive games in older adults: a meta-analysis. Sci Rep. 2020 Sep 17;10(1):15276. DOI: 10.1038/s41598-020-72281-3. PMID: 32943742. PMCID: PMC7498601.
- Simons DJ, Boot WR, Charness N, Gathercole SE, Chabris CF, Hambrick DZ, et al. Do “Brain-Training” Programs Work? Psychol Sci Public Interest. 2016 Oct;17(3):103–86. DOI: 10.1177/1529100616661983. PMID: 27697851.
- Sala G, Tatlidil KS, Gobet F. Video game training does not enhance cognitive ability: A comprehensive meta-analytic investigation. Psychol Bull. 2018;144(2):111–39. DOI: 10.1037/bul0000139. PMID: 29239631.
- Melby-Lervåg M, Redick TS, Hulme C. Working Memory Training Does Not Improve Performance on Measures of Intelligence or Other Measures of “Far Transfer”: Evidence From a Meta-Analytic Review. Perspect Psychol Sci. 2016 Jul;11(4):512–34. DOI: 10.1177/1745691616635612. PMID: 27474138. PMCID: PMC4968033.
- Cernych M, Satas A, Brazaitis M. Post-sauna recovery enhances brain neural network relaxation and improves cognitive economy in oddball tasks. Int J Hyperthermia. 2018 Oct 9;35(1):375–82. DOI: 10.1080/02656736.2018.1504992. PMID: 30300030.
- Knekt P, Järvinen R, Rissanen H, Heliövaara M, Aromaa A. Does sauna bathing protect against dementia? Prev Med Rep. 2020 Dec;20:101221. DOI: 10.1016/j.pmedr.2020.101221. PMID: 33088678. PMCID: PMC7560162.
- Hunt AP, Minett GM, Gibson OR, Kerr GK, Stewart IB. Could heat therapy be an effective treatment for alzheimer’s and parkinson’s diseases? A narrative review. Front Physiol. 2019;10:1556. DOI: 10.3389/fphys.2019.01556. PMID: 31998141. PMCID: PMC6965159.
- Tei C, Imamura T, Kinugawa K, Inoue T, Masuyama T, Inoue H, et al. Waon Therapy for Managing Chronic Heart Failure - Results From a Multicenter Prospective Randomized WAON-CHF Study. Circ J. 2016 Mar 18;80(4):827–34. DOI: 10.1253/circj.CJ-16-0051. PMID: 27001189.
- Hussain J, Cohen M. Clinical effects of regular dry sauna bathing: A systematic review. Evid Based Complement Alternat Med. 2018 Apr 24;2018:1857413. DOI: 10.1155/2018/1857413. PMID: 29849692. PMCID: PMC5941775.


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!