An LPR Treatment Strategy for Stubborn Silent Reflux
- What Is LPR?|
- Symptoms|
- LPR Treatment Strategy|
- Diet for LPR|
- Gut Microbiome Support for LPR|
- Stomach Acid Support for LPR|
- Supplements for LPR|
- Other Treatments|
- The Bottom Line|
- Recommended Products|
LPR (laryngopharyngeal reflux) is a reflux disease that mostly affects your voice, throat, and sinuses. Also called “silent reflux,” LPR often doesn’t cause heartburn like regular reflux. Signs you may have LPR are hoarseness, a chronic cough, throat clearing, or other throat symptoms. Getting LPR treatment can help ensure these symptoms don’t progress to more serious conditions.
Most LPR treatment is prescription or over-the-counter proton pump inhibitors or H2 blocker medications. But these often don’t provide relief for patients, leaving them frustrated and wondering what to do next. And even if this prescription works, it does little to address the root causes of your symptoms.
Whether you have a new diagnosis of LPR or you’re still seeking answers, let’s talk about what you can do.

What Is LPR (Silent Reflux)?
Reflux is when the contents of the stomach come back up into the esophagus or throat. LPR (laryngopharyngeal reflux disease) is one type of reflux that primarily affects the voice box (larynx), the back of the throat (pharynx), or the sinuses.
“Silent” refers to the fact that LPR often doesn’t cause the heartburn associated with acid reflux, though it sometimes does.
It’s important to get treatment if you think you may have silent reflux. Left untreated, it can lead to the more advanced esophagus and throat damage of GERD (gastroesophageal reflux disease) [1, 2, 3].
Symptoms of LPR (Laryngopharyngeal Reflux)
You may want to be evaluated for silent reflux if you have many of the following reflux symptoms [4]:
- Hoarseness, vocal cord inflammation, or frequent laryngitis
- Chronic cough or frequent bronchitis
- Regurgitation
- Sore throat
- Throat clearing or tickling in the throat
- Difficulty swallowing (dysphagia)
- The sensation of a lump in the back of the throat (globus)
- Heartburn
- Postnasal drip
- Sleep disturbance
- Shortness of breath
Silent reflux may be diagnosed by your gastroenterologist or ear, nose, and throat specialist (otolaryngologist). Diagnosis may be based on:
- Medical history
- Endoscopy or laryngoscopy (using a camera (laryngoscope) to look at your esophagus and larynx)
- Manometry (a test to measure your esophagus’s motility)
- pH monitoring with a pH probe
A Hierarchical LPR Treatment Strategy
Similar to other gut conditions like IBS or SIBO, LPR may have many possible root causes. In this situation, we recommend using a hierarchical approach.
This means applying foundational diet and lifestyle changes first, continuing therapies that give you improvement, and only then moving toward more specific and targeted therapies. (You can learn all about this approach to improving your gut health in my book Healthy Gut, Healthy You.)
In simplest terms, a hierarchical approach to LPR treatment includes these steps:
1. Modify your diet and eating habits to remove reflux triggers.
2. Improve your gut microbiome with probiotics. Address gut infections with antimicrobials if necessary.
3. Support your stomach acid with betaine HCL if needed.
4. Add additional therapies only if the first three don’t provide relief.
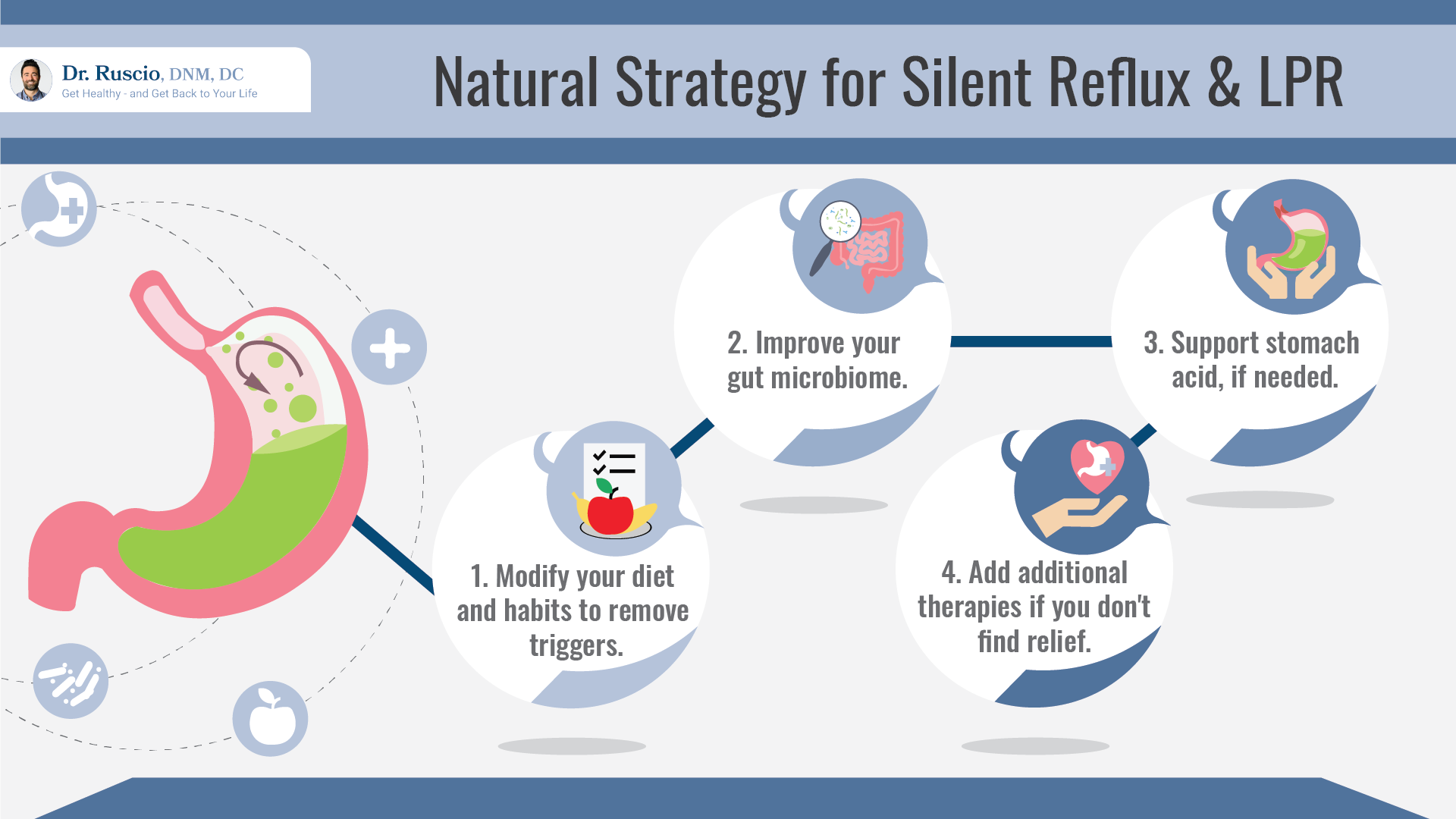
Let’s explore how to use these steps to approach your ideal LPR treatment.
Diet and Eating Habits for LPR
Diet and eating habits are the first place to start addressing LPR.
There isn’t one particular diet that’s been shown to work for all LPR patients. However, as with other digestive conditions, an elimination diet can help you to determine which foods are contributing to your LPR symptoms.
During an elimination diet, you remove foods that may be triggering your symptoms for about three weeks. Then you reintroduce foods to check for reactions. You only need to continue to avoid foods that clearly make your symptoms worse.
Studies suggest that the following elimination diets may help LPR symptoms:
- A low-carb diet [5, 6] like the Paleo diet
- A low FODMAP diet [7]
- Specifically reducing acidic foods (like citrus fruits), [8] fatty or spicy foods, chocolate, alcohol, and coffee [9]
Many of the specific foods that have been shown to aggravate reflux are foods high in histamine. There’s no direct research recommending it, but a low histamine diet may be useful if the Paleo or low FODMAP diet doesn’t give you any relief.
Additionally, a systematic review showed some specific eating habits can improve LPR [10]:
- Drinking alkaline water [8]
- Waiting 2-3 hours after eating to go to bed
- Avoiding fasting
- Eating smaller meals to avoid overeating
Once you’ve figured out your dietary reflux triggers, move on to the next step.
Support Your Gut Microbiome to Improve LPR
Imbalances in your gut microbiome or gut infections may underlie many gut challenges, including IBS (irritable bowel syndrome) and SIBO (small intestinal bacterial overgrowth). Early research suggests this is true for LPR too.
For example, a systematic review of 13 studies found that probiotics improved several LPR symptoms, including regurgitation, reflux, heartburn, and indigestion [11].
Other high-level research found that H. pylori, a bacterial infection of the stomach, was present in about half of patients with LPR [4]. And bacterial overgrowths like SIBO are often associated with slow gut motility, which early research suggests may also be a cause of LPR [12].
The simplest strategy for improving your gut microbiome is to use triple probiotic therapy. Probiotics are a low-risk approach that can heal your gut lining, reduce inflammation, and help crowd out pathogenic gut infections. To learn more about how to use probiotics, see our Probiotics Starter Guide.
If you don’t see LPR relief with probiotics, you may need to be evaluated by a practitioner for any underlying infections like H. pylori or SIBO, and treated with antimicrobial therapy. If you need help with this, consider reaching out to our center for functional medicine to become a patient.
Support Stomach Acid for LPR
Most people with reflux or heartburn imagine that it would be a good idea to reduce stomach acid with PPI medication. But many patients with LPR symptoms don’t experience relief with this therapy [13].
The evidence for using PPIs to reduce stomach acid for reflux is mixed. Some high-level research suggests PPIs provide mild improvement [14] or significant improvement [15] for LPR, while other studies suggest they provide no improvement compared to a placebo [4].
Despite this disagreement, research suggests that low stomach acid can contribute to many gut problems, including heartburn, regurgitation, reflux, and fullness after meals [16].
Ironically, for many patients who don’t feel better on PPIs, increasing stomach acid improves reflux. Using a betaine HCL supplement to increase stomach acid just before meals may help.
Not everyone needs stomach acid, but we’ve seen it make a big difference for some reflux patients at our center for functional medicine. Supplemental stomach acid should lead to noticeable change, if it’s right for you. If it doesn’t, supplementation should be discontinued.
You may be more likely to benefit from stomach acid support if you are:
- Over 65 years old [17]
- Have an autoimmune condition, like Hashimoto’s thyroiditis or rheumatoid arthritis
- Are anemic [18]
- Have been diagnosed with H. pylori
- Have chronically used antacids or proton pump inhibitors (PPIs)

Supplements for LPR
If you still haven’t found relief for your LPR symptoms even after you found your best diet, and supported your gut microbiome and stomach acid, you can try other more specific strategies. Several supplements have been demonstrated to improve LPR or reflux.
Melatonin
Melatonin, the hormone your body produces at night to help you fall asleep, has been shown to improve the function of the lower esophageal sphincter (the muscle that opens at the top of the stomach to allow food to enter) in GERD and reflux patients [19, 20, 21].
It’s also been suggested that melatonin supplementation can protect your esophagus from stomach acid [22, 23]. Including melatonin supplements at bedtime may help reduce reflux and protect your esophagus from the negative effects of reflux.
Motility Supports and Prokinetics for Reflux
Some studies suggest that slow gut motility (the movement of food through the digestive tract) may be an underlying cause of reflux [12]. Research suggests this may be true, as blends of prokinetic herbs, like Iberogast or RKT (a Japanese herbal blend including ginger and ginseng), have been shown to improve reflux, heartburn, and lower esophageal sphincter function [8, 24, 25, 26, 27, 28, 29].
Supporting your gut motility with such herbal products may improve your LPR symptoms.
And don’t forget the eating behaviors that improve motility as well:
- Avoid snacking between meals.
- Don’t eat 2-3 hours before bed.
- Avoid late-night snacking to ensure a long overnight fast. This allows your “migrating motor complex” to perform its daily cleaning cycle on your intestines.
Alginate Therapy for LPR
Sodium alginate is an over-the-counter supplement derived from brown kelp. It prevents reflux by forming a foam barrier between your esophagus and stomach by floating on top of your food.
A systematic review found alginate therapy highly effective in mild GERD [8]. Alginate is the active ingredient in a liquid over-the-counter medication available in the UK called Gaviscon Advance, and a relatively new product called Reflux Gourmet.
Using alginate supplements immediately after meals may help reduce reflux so that your esophagus can heal.
Other LPR Treatments That May Help
In one study, hiatal hernia was found in 53% of reflux patients [4], which suggests that hiatal hernia may be one underlying cause of reflux.
If you have a hiatal hernia, some naturopaths and chiropractors can adjust it manually by maneuvering the part of the stomach that’s poking through the diaphragm down, which can sometimes provide some temporary reflux relief.
An at-home device called IQoro can also help to treat reflux symptoms caused by hiatal hernias. This device works by training and strengthening weakened muscles through brief daily exercises.
One more option is fundoplication, a surgery to attach the upper part of the stomach to the esophagus for GERD patients. In one study, fundoplication surgery was found to be more effective for improving LPR symptoms like cough, throat clearing, and quality of life for patients compared to PPI therapy [30]. Most patients in the study were able to stop PPI therapy after surgery.
If you think you may have a hiatal hernia, be sure to discuss this with your doctor.
The Bottom Line
If simple, conventional LPR treatment with PPIs or H2 blockers hasn’t helped you, don’t despair. Making some simple changes to your diet and lifestyle and investigating your root causes may provide you with solutions that resolve your symptoms.
Focus on identifying your reflux food triggers, rebalancing your gut microbiome, supporting stomach acid if appropriate, and bringing in research-supported supplements.
And if you find you need more help, don’t hesitate to reach out to the Ruscio Institute for Functional Health to learn more about becoming a patient.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- https://www.niddk.nih.gov/health-information/digestive-diseases/barretts-esophagus
- https://www.hopkinsmedicine.org/otolaryngology/specialty_areas/complex_airway/conditions/subglottic_stenosis.html
- Spechler SJ. Gastroesophageal Reflux Disease and Eosinophilic Esophagitis. Gastroenterol Hepatol (N Y). 2019 Feb;15(2):111-113. PMID: 31011306; PMCID: PMC6469260.
- Brown J, Shermetaro C. Laryngopharyngeal Reflux. [Updated 2021 Mar 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519548/
- Austin GL, Thiny MT, Westman EC, Yancy WS Jr, Shaheen NJ. A very low-carbohydrate diet improves gastroesophageal reflux and its symptoms. Dig Dis Sci. 2006 Aug;51(8):1307-12. doi: 10.1007/s10620-005-9027-7. Epub 2006 Jul 27. PMID: 16871438.
- Yancy WS Jr, Provenzale D, Westman EC. Improvement of gastroesophageal reflux disease after initiation of a low-carbohydrate diet: five brief case reports. Altern Ther Health Med. 2001 Nov-Dec;7(6):120, 116-9. PMID: 11712463.
- Piche T, des Varannes SB, Sacher-Huvelin S, Holst JJ, Cuber JC, Galmiche JP. Colonic fermentation influences lower esophageal sphincter function in gastroesophageal reflux disease. Gastroenterology. 2003 Apr;124(4):894-902. doi: 10.1053/gast.2003.50159. PMID: 12671885.
- Huestis MJ, Keefe KR, Kahn CI, Tracy LF, Levi JR. Alternatives to Acid Suppression Treatment for Laryngopharyngeal Reflux. Ann Otol Rhinol Laryngol. 2020 Oct;129(10):1030-1039. doi: 10.1177/0003489420922870. Epub 2020 May 25. PMID: 32449369.
- Nanda MS. Role of Adjuvant Lifestyle Modifications in Patients with Laryngopharyngeal Reflux Disease in Hilly Areas. Int J Sci Stud 2016;3(10):114-118.
- Min C, Park B, Sim S, Choi HG. Dietary modification for laryngopharyngeal reflux: systematic review. J Laryngol Otol. 2019 Feb;133(2):80-86. doi: 10.1017/S0022215118002256. Epub 2019 Jan 16. PMID: 30646967.
- Cheng J, Ouwehand AC. Gastroesophageal Reflux Disease and Probiotics: A Systematic Review. Nutrients. 2020 Jan 2;12(1):132. doi: 10.3390/nu12010132. PMID: 31906573; PMCID: PMC7019778.
- Passaretti S, Mazzoleni G, Vailati C, Testoni PA. Oropharyngeal acid reflux and motility abnormalities of the proximal esophagus. World J Gastroenterol. 2016 Oct 28;22(40):8991-8998. doi: 10.3748/wjg.v22.i40.8991. PMID: 27833390; PMCID: PMC5083804.
- Lechien JR, Akst LM, Hamdan AL, Schindler A, Karkos PD, Barillari MR, Calvo-Henriquez C, Crevier-Buchman L, Finck C, Eun YG, Saussez S, Vaezi MF. Evaluation and Management of Laryngopharyngeal Reflux Disease: State of the Art Review. Otolaryngol Head Neck Surg. 2019 May;160(5):762-782. doi: 10.1177/0194599819827488. Epub 2019 Feb 12. PMID: 30744489.
- Lechien, J.R., Saussez, S., Schindler, A., Karkos, P.D., Hamdan, A.L., Harmegnies, B., De Marrez, L.G., Finck, C., Journe, F., Paesmans, M. and Vaezi, M.F. (2019), Clinical outcomes of laryngopharyngeal reflux treatment: A systematic review and meta-analysis. The Laryngoscope, 129: 1174-1187. https://doi.org/10.1002/lary.27591
- Wei C. A meta-analysis for the role of proton pump inhibitor therapy in patients with laryngopharyngeal reflux. Eur Arch Otorhinolaryngol. 2016 Nov;273(11):3795-3801. doi: 10.1007/s00405-016-4142-y. Epub 2016 Jun 16. PMID: 27312992.
- Rodriguez-Castro KI, Franceschi M, Noto A, Miraglia C, Nouvenne A, Leandro G, Meschi T, De’ Angelis GL, Di Mario F. Clinical manifestations of chronic atrophic gastritis. Acta Biomed. 2018 Dec 17;89(8-S):88-92. doi: 10.23750/abm.v89i8-S.7921. PMID: 30561424; PMCID: PMC6502219.
- Thomas G. Guilliams, PhD; Lindsey E. Drake, MS. Meal-Time Supplementation with Betaine HCl for Functional Hypochlorhydria: What is the Evidence? Integrative Medicine. Volume 19, No. 1. February 2020.
- Andrea L Betesh, Carol A Santa Ana, Jason A Cole, John S Fordtran, Is achlorhydria a cause of iron deficiency anemia?, The American Journal of Clinical Nutrition, Volume 102, Issue 1, July 2015, Pages 9–19, https://doi.org/10.3945/ajcn.114.097394
- Kow CS, Hasan SS. Could melatonin be used in COVID-19 patients with laryngopharyngeal reflux disease? J Med Virol. 2021 Jan;93(1):92-93. doi: 10.1002/jmv.26150. Epub 2020 Jun 24. PMID: 32519764; PMCID: PMC7300529.
- Kandil TS, Mousa AA, El-Gendy AA, Abbas AM. The potential therapeutic effect of melatonin in Gastro-Esophageal Reflux Disease. BMC Gastroenterol. 2010 Jan 18;10:7. doi: 10.1186/1471-230X-10-7. PMID: 20082715; PMCID: PMC2821302.
- Pereira Rde S. Regression of gastroesophageal reflux disease symptoms using dietary supplementation with melatonin, vitamins and aminoacids: comparison with omeprazole. J Pineal Res. 2006 Oct;41(3):195-200. doi: 10.1111/j.1600-079X.2006.00359.x. PMID: 16948779.
- Klupińska G, Wiśniewska-Jarosińska M, Harasiuk A, Chojnacki C, Stec-Michalska K, Błasiak J, Reiter RJ, Chojnacki J. Nocturnal secretion of melatonin in patients with upper digestive tract disorders. J Physiol Pharmacol. 2006 Nov;57 Suppl 5:41-50. PMID: 17218759.
- Bang CS, Yang YJ, Baik GH. Melatonin for the treatment of gastroesophageal reflux disease; protocol for a systematic review and meta-analysis. Medicine (Baltimore). 2019 Jan;98(4):e14241. doi: 10.1097/MD.0000000000014241. PMID: 30681611; PMCID: PMC6358381.
- Rösch W, Vinson B, Sassin I. A randomised clinical trial comparing the efficacy of a herbal preparation STW 5 with the prokinetic drug cisapride in patients with dysmotility type of functional dyspepsia. Z Gastroenterol. 2002 Jun;40(6):401-8. doi: 10.1055/s-2002-32130. PMID: 12055663.
- Madisch A, Melderis H, Mayr G, Sassin I, Hotz J. Ein Phytotherapeutikum und seine modifizierte Rezeptur bei funktioneller Dyspepsie. Ergebnisse einer doppelblinden plazebokontrollierten Vergleichsstudie [A plant extract and its modified preparation in functional dyspepsia. Results of a double-blind placebo controlled comparative study]. Z Gastroenterol. 2001 Jul;39(7):511-7. German. doi: 10.1055/s-2001-16142. PMID: 11505331.
- von Arnim U, Peitz U, Vinson B, Gundermann KJ, Malfertheiner P. STW 5, a phytopharmacon for patients with functional dyspepsia: results of a multicenter, placebo-controlled double-blind study. Am J Gastroenterol. 2007 Jun;102(6):1268-75. doi: 10.1111/j.1572-0241.2006.01183.x. PMID: 17531013.
- Melzer J, Iten F, Reichling J, Saller R. Iberis amara L. and Iberogast–results of a systematic review concerning functional dyspepsia. J Herb Pharmacother. 2004;4(4):51-9. PMID: 15927925.
- Saller R, Pfister-Hotz G, Iten F, Melzer J, Reichling J: Iberogast(r): Eine moderne phytotherapeutische Arzneimittelkombination zur Behandlung funktioneller Erkrankungen des Magen-Darm-Trakts (Dyspepsie, Colon irritabile) – von der Pflanzenheilkunde zur «Evidence Based Phytotherapy».Eine systematische Übersicht. 2002;9(suppl 1):1-20. doi: 10.1159/000068645
- Melzer J, Rösch W, Reichling J, Brignoli R, Saller R. Meta-analysis: phytotherapy of functional dyspepsia with the herbal drug preparation STW 5 (Iberogast). Aliment Pharmacol Ther. 2004 Dec;20(11-12):1279-87. doi: 10.1111/j.1365-2036.2004.02275.x. PMID: 15606389.
- Zhang C, Hu ZW, Yan C, Wu Q, Wu JM, Du X, Liu DG, Luo T, Li F, Wang ZG. Nissen fundoplication vs proton pump inhibitors for laryngopharyngeal reflux based on pH-monitoring and symptom-scale. World J Gastroenterol. 2017 May 21;23(19):3546-3555. doi: 10.3748/wjg.v23.i19.3546. PMID: 28596691; PMCID: PMC5442091.


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!