Listener Questions – Misdiagnosis of Hypothyroidism Is Rampant, Thyroid Hormone Absorption, Probiotics For SIBO
Subheading in sentence case.
Today we will cover listener questions, including…
- Nigella Sativa for Hashimoto’s
- Can inflammation interfere with synthetic hormone absorption
- Can eliminating reactive foods cause withdrawal symptoms
- Alkalized water
- Is there a correlation between diet and predominant microbes
- Probiotics for SIBO
Hypothyroid Misdiagnosis
- Misdiagnosis is rampant
- Especially among alternative or integrative medicine practitioners
- If you are flagged low T4 paired with not flagged high TSH, that does not diagnose you with hypothyroidism
Natural Treatments for Hashimoto’s
- Supplements: Vitamin D, magnesium, COQ10, selenium (open to Nigella Sativa but there are other therapies that get the job done)
- Diet: paleo diet, potentially a low FODMAP diet
- Exercise
- If those fail… treating any underlying problem in the gut helps this autoimmunity
Gut Inflammation Impacts Thyroid Medication Absorption
- Treat the gut to improve absorption
- SIBO and H. pylori can interfere with absorption
- Go through the Healthy Gut, Healthy You protocol
- Could try gel tabs
Can You Have Withdrawal Symptoms from Foods You Eliminate from Your Diet?
- One can have a gluteomorphic or casomorphic response
- Causes you to release some of your own endogenous pain-killing chemicals, like endorphins, a type of endogenous morphine-like compound
- Consider that by eliminating certain foods you might not be eating enough carbs which can cause various symptoms
- Consider that by eliminating certain foods and adding in others, you may have started eating foods that do not agree with you
- High FODMAP foods for instance
Effects of Alkaline Water
- The research in this area is lacking
- Study: pH of drinking water influences the composition of gut microbiome and type 1 diabetes incidence
- Acidified water increased type 1 diabetes in mice
- Study: Consumption of acidic water alters the gut microbiome and decreases the risk of diabetes in NOD mice.
- Acidifed water decreased type 1 diabetes in mice
Analyzing Microbiome Results to Determine a Diet for Weight Loss
- Modulating the microbiota with special diets or prebiotics has not shown to be a favorable thing for weight loss
- The best thing to focus on is outcome data. Try different diets and see what is working for you
Why Do Some Practitioners Discourage Probiotics for SIBO
- The medical doctor/medical establishment community may not be that comfortable with using non-prescription drugs
- Not a lot of drug company reps going to doctors’ offices, are sharing literature on probiotics
- It is not because probiotics are dangerous or that they have terrible side effects
- Side effects from most good probiotics are close to zero
- There are dozens and dozens of studies and handfuls of meta-analyses showing that probiotics can improve IBS and SIBO
In this episode…
Episode Intro … 00:00:40
Hypothyroidism Misdiagnosis … 00:01:52
Nigella Sativa and Hashimoto’s Thyroiditis … 00:10:12
Inflammation & Thyroid Med Absorption … 00:10:59
Withdrawal Symptoms From Food? … 00:19:14
Effects of Alkaline Water … 00:23:56
Analyzing Microbiome Results … 00:30:25
Probiotics Recommendations for SIBO … 00:38:52
Episode Wrap-Up … 00:49:03

Download this Episode (right click link and ‘Save As’)
Episode Intro
Dr. Michael Ruscio, DC: Hey everyone, welcome to Dr. Ruscio Radio. This is Dr. Ruscio. Today, I am here with Erin and we are going to be jumping into another edition of listener questions. Erin, are you ready to rock and roll?
Erin Ryan: I’m ready.
DrMR: As a quick reminder, I’ve decided to change the format of our listener questions. I used to look at all the questions and think through a robust answer to each. And I just wasn’t able to match the pace of questions coming in. So this is a way for me to be a little more concise with the answers.
I haven’t seen these questions before. So I’m going to try to give a concise answer, again, but with this caveat: Don’t look at this as every potential treatment option and contingency. While I’d like to be able to do that, I’m trying to go with an answer that will give you the main strokes. I won’t be able to include every possible detail. Again, I think it will be enough to get you pointed in the right direction.
Hypothyroidism Misdiagnosis
But before we jump into that, I wanted to half vent and half share something that will be very helpful for people struggling with the question: Do I have a thyroid problem or not? You’ve likely heard my opinion on thyroid care, which I think is progressive. At the same time, I’m circumspect and cautious with how quickly we label someone as hypothyroid. Perhaps you’ve also heard me discuss how I’ve caught a number of cases who were told they were hypothyroid but they actually weren’t. And I’ve made criticisms of the functional medicine community on the podcast about that.

And you know, whenever I criticize, I always try to catch myself. I don’t make these criticisms because I enjoy being a contrarian. Unfortunately, I think there is a large enough degree of irresponsible actions that it makes me look, relatively speaking, like a contrarian or a whistleblower, even though I have no desire to be that way. And I’ve recently been monitoring myself and saying, am I being too critical here of the community? Is there more of a case for this liberal diagnosis of hypothyroidism than I’m giving credit for? Honestly, I don’t think that is the case.
I was reaffirmed in this conclusion, when looking at a study that was recently published in Greece. I’m just going to give you the quick take on this. But I will do a more formal synopsis of this study that will go out in our Monday video newsletter/podcast. Essentially, 291 patients in Greece who had a non-firm hypothyroid diagnosis were rechecked and the researchers had them go off thyroid hormone. First, they did a TSH and T4 test, and then had them go off thyroid hormone for six to eight weeks. After those six to eight weeks, they retested. And they found that 60% of the patients did not require thyroid medication. They were not hypothyroid. That is huge.
I have to admit, I am not surprised. Just last Friday in the office, someone came to see me after seeing a top-notch thyroid guru who lectures all over the country, has a couple books out there, and is very well known. I now check new patients who present with this diagnosis to see if they are truly hypothyroid (unless it’s been a super conventional doctor who has made a diagnosis). I check because I find that the incidence of false diagnoses in the alternative community is alarmingly high. Yet again, this patient had normal TSH, normal T4, and normal T3. Now, her T3 was in the lower end of the normal range, but that does not, by any stretch of the imagination, mean someone is hypothyroid.

In this doctor’s defense, perhaps she gave the patient a more nuanced diagnosis. Maybe she said, you’re not truly hypothyroid, but you have poor conversion and you may benefit from medication. But it doesn’t change the fact that this patient thought she was hypothyroid, felt worse on medication, and struggled for months trying different medications. All this only to say I’m done, I don’t want to take this medicine anymore. Then, years later, she ends up in my office. She gets reaffirmation that she was never hypothyroid. In only two months, with some gut work, I believe her symptoms are 75% improved.
So this problem is getting out of hand. There’s another study that went in our December Future of Functional Medicine Review clinicians’ newsletter. It was a systematic review and meta-analysis looking at 21 studies. They looked at over 3,000 studies and selected for only studies that were high-quality, didn’t have a risk of bias, and adequate controls, and consolidated down to 21 of the most high-quality studies. This gave the researchers a sample of about 2,100 people who had subclinical hypothyroid. So this means that you have high TSH according to the conventional ranges. On your lab report, you’ll see “high,” and it will be in bold or in red. And that’s paired with normal T4. They were looking to see, maybe this group of people who are subclinical hypothyroid would benefit from thyroid medication. You have to have high TSH and low T4 to diagnose hypothyroid, but these people only had high TSH, kind of inching their way toward hypothyroidism.
So in over 2,100 people, they found no effect on quality of life, no effect on thyroid-related symptoms. But it did normalize their TSH. So that’s even more evidence showing we shouldn’t be so liberal with our use of the diagnosis of hypothyroidism, or even the potential experimentation with thyroid hormone replacement medication if someone is looking non-optimal. I’m open to the exceptional case where someone feels better on a little support with thyroid hormone. But I think all too often, what is likely happening, and what this growing body of evidence is supporting, is that people are given thyroid hormone when they don’t need it. I would venture a guess that for many of the people that feel better on it, it’s either the placebo effect or the other interventions they’re undergoing at the same time, paleo diet, gluten-free, vitamin D, fish oils, adrenal support, whatever it is.
And I think there are probably far more people who are on thyroid medication unnecessarily than there should be. This will be the next book that I write. It will not be for a little while because it’s quite the undertaking, but this is an area that is getting out of control. The take-home is, if you’ve been diagnosed with hypothyroidism by anyone other than a conventionally-practicing doctor—and I don’t mean just if they’re an MD or a DO—get a second opinion on what your labs showed at the time of diagnosis. If you are flagged low T4 paired with not flagged high TSH, that does not diagnose you with hypothyroidism. So you really may want to get a second opinion, because you may not need the medication.
And I don’t mean any disparagement against alternative or integrative medicine, even though it may sound like it. I just think some of the education in this space has gotten a bit too far away from what the science says. I think, in this liberal use of thyroid hormone, people are trying to find a therapy that can help. But in my opinion—and I think this is what the totality of the data supports—for most people, unfortunately that does not produce any symptomatic improvement. It may actually lead to symptomatic detriment reactions. And for most people who are experiencing clinical improvements symptomatically, it may either be the placebo effect or attributed to other interventions they are undergoing at the same time, like dietary changes, nutritional support, adrenal support, and so on.
So it’s an important issue. Feel free to leave your feedback on this post. I’m curious where people are at in grappling with this. And Erin, we can now go to questions, unless you have anything you wanted to touch on.
ER: No, I think you got it.
DrMR: Thanks.
Nigella Sativa and Hashimoto’s Thyroiditis
ER: That was very well said. So let’s move into our first question from Maria. She says, “Can you talk about the herb nigella sativa and the effects on Hashimoto’s based on studies or clinical practice?”
DrMR: No, I can’t say I’ve used that herb in clinical practice. I think I’ve seen one study. There might be others. And here’s my take: usually, it’s either improved thyroid autoimmunity or improved thyroid hormone conversion. For thyroid autoimmunity, we already have a handful of things that work well in terms of supplements: vitamin D, magnesium, COQ10, selenium. And diets: a paleo diet, potentially a low FODMAP diet. And if those fail, then treating any underlying problem in the gut helps this autoimmunity. Some problems could be small intestinal bacterial overgrowth, which has been highly associated with hypothyroidism and thyroid autoimmunity, or H. pylori. We have at least one study (not all the data here support this) showing that the treatment and clearance of H. pylori can lead to an improvement in thyroid autoimmunity.
We already have stuff there that works well. The other component is to improve your conversion. I think you could make a case for a partial benefit from some of the agents known to improve thyroid conversion. I believe ashwagandha is one, selenium is also one. But in my experience, the improvement someone’s going to get from those symptomatically is really minimal in comparison to a fundamental cause, like their diet, their exercise, their caloric intake, and any lingering inflammatory or irritating problem in the gut.
In short, my answer is: I think it’s one of a handful of new things popping up that are supposed to either help with thyroid autoimmunity, conversion, or both. But nothing has looked as attractive or better than some of the other therapies that are more well-studied, to make me think it really needs to be utilized. And that is a really important concept, not getting caught up in trying the newest stuff. This is the whole premise of Healthy Gut, Healthy You. It’s not about having this magical herb or vitamin that no one else has. Rather you need a solid program or system to use the available therapies that have been studied, to help people improve their health. So I’m open to it but I think there are a lot of other things available that can get the job done. This may more be a bell and whistle than anything else.
Gut Inflammation Impacts Thyroid Medication Absorption
ER: Okay, cool. The next question is from Kathleen. Another thyroid question: “Can inflammation still interfere with synthetic hormone absorption in a person without a thyroid gland? My thyroid was removed due to thyroid cancer. If so, can you recommend a treatment? I’m still experiencing crippling fatigue. Currently on 42.5 total mcg of Cytomel T3 broken up into three doses during the day, and no T4.”
DrMR: Okay. First of all, can inflammation—I’m assuming she means inflammation in the gut—interfere with the absorption of even the synthetic? And yes, absolutely. This is one of the reasons why I think we, in our office, see patients be able to measurably decrease their thyroid medication and see an improvement in all their thyroid symptoms. This is because we improved the health of their gut and the absorption of their thyroid hormone. And that is not a conjecture.
We’re starting to see evidence published on certain models of malabsorption like chronic ulcer and chronic H. pylori. Potentially also in short bowel syndrome, although I’m not positive. But in people with a condition that leads to malabsorption, studies are now showing that using a liquid gel capsule, Tirosint (which we’ve talked about in the past), leads to much better outcomes. These patients have a poor rate of absorption, which is likely due to H. pylori or ulcer, leading to damage of the gut. So these gel tabs are easier to absorb, are better absorbed, and they lead to better outcomes in the patients.

Another way of getting around this, instead of taking a liquid gel tab, is to just fix someone’s gut. I would argue that that would lead to the greatest overall symptomatic improvement. But some people, even at their best—if we’re going to be real in this conversation—will never have fully optimal absorption. So they may need some support with an easier-to-absorb form of the medication. I did lay out an algorithm for navigating this in our clinician’s newsletter. But one of the first things you want to do is optimize your gut health, because then you will do better on any medication that you take.
So yes, inflammation can interfere with absorption of any kind of thyroid medication. The type that would be least prone to that would be Tirosint, or other liquid gel tabs of thyroid hormone. And a way to get around that— that would probably lead to you feeling your best—would be making sure you optimize your gut health. Again, the protocol in Healthy Gut, Healthy You is the best thing that I can offer you. So I would 1000% start there.
The other interesting thing about what you said is that you’re only on Cytomel. That runs counter to what the majority of the literature says about what medications someone might feel best on. To bottom line it for you (and this is counter to what much of the functional and integrative community will tell you), when you look at research evidence, you don’t see a supported philosophy that everyone needs to be on T3.
Do you see support for the position that people may do better on more than just T4? Yes. And that conventional medicine should be open to more than just using T4? Yes. There is support for this. But we don’t go from one extreme all the way to the other and now say, everyone should be on T4 plus T3.
What the evidence shows is most people will do okay on T4 alone. But a subset of people—and I don’t know the exact percentage off the top of my head, maybe we could say 15-30%, I could be a little off—are genetically poor at conversion of T4 to T3. And they may do better with the addition now of T3.

But what I would do first after trying this with T4 would be upping the dose of the T4. One of the problems some people have when they go on T3 is side effects. Insomnia, loss of hair, racing heart, anxiety, palpitations. How else can we get more hormone in the system without causing those reactions? What the literature supports is: Try a higher dose of T4, getting TSH in the lowest fourth of the acceptable range, and see how the patient responds. That seems to work well, according to what the literature shows, for a good number of people.
If that still doesn’t work, then consider the T4 plus T3. If none of that works, potentially consider the liquid T4, plus or minus a T3. I’m open to T3 alone. But—and maybe there’s some evidence I haven’t seen supporting that approach—that approach seems a little tenuous. I’m not sure how you’ve arrived at that conclusion to use that. I don’t know if I feel that to be a great strategy. Again, there may be something that I’m missing. But I would work through the outline that I just laid out. I think you have a good probability of seeing the dramatic resolution that you’re looking for if you do so.
ER: Great. And I think we did a video recently on that piece of research that you’re talking about. So I’ll try to find that for the show notes. Next, we have an audio question from Ben.
Withdrawal Symptoms from Food?
Ben: Hi, Dr. Michael. Thank you very much for all the information you gave. My name is Ben from Israel. My question is, is it possible that elimination of food that spikes antibodies in the body can cause withdrawal symptoms like depression and anxiety? Thank you very much.
DrMR: Okay. I believe he’s saying, if I get rid of foods I’m having an immunogenic response to and that are causing a measurable antibody response, can that lead to withdrawal-type symptoms? Yes. I can’t say I see a lot of this, maybe any of this, where you take someone off gluten or dairy and they feel worse. I suppose it is possible. This has been published.
Some people are known to have a gluteomorphic or casomorphic (gluten-derived or casein-derived) response. As I understand it, it is so painful to the body that it causes you to release some of your own endogenous pain-killing chemicals, like endorphins, a type of endogenous morphine-like compound. So when you take someone off these foods, they’re no longer getting the stimulus that causes the body to release its own pain-suppressing compounds. Therefore, it can lead to a withdrawal reaction. I’ve heard about that. I’ve never thoroughly checked the science behind it. I’ve seen one or two papers that talked about this. One or two papers doesn’t mean it’s clinically meaningful or fairly prevalent, but there is something there.

What do you do about that? Well, you may want to slowly wean off, just like someone who’s coming off cigarettes. I can’t say I’ve read anything that supports this, but logic may be a way to navigate this. The other thing—that I think has a higher likelihood—is that you may inadvertently be changing your diet in a way that doesn’t work well for your body.
You may be doing one of two things. One, you may be eating too low-carb. Or two, you may be eating more of certain foods that don’t work well for your body. For some people, they first go paleo and they may not process certain fruits and vegetables that are high in FODMAPs very well. And they inadvertently go onto a high-FODMAP diet when they decide to try paleo, or something similar. They’re getting off grains or getting off dairy, so now what do they eat? A lot of vegetables and fruits and meats and nuts and seeds. But they may be eating more of the fruits and vegetables that are high in FODMAPs than their gut can process. And now they’re experiencing negative side effects because of that.
So I would circle back to your diet and check to see that you haven’t dramatically decreased your carb intake or dramatically increased other food groups, like FODMAPs, that could be problematic. And again, Healthy Gut, Healthy You walks you through a way of navigating this.
Again, it could be you’re changing your diet in a unbeneficial but unintentional way. Or there may be something to gluteo- or casomorphines, leading to this internal pain response. In that situation, you may need to do a slow wean-off rather than a cold turkey. Although that’s just my opinion and I haven’t read anything to support it.
ER: Okay. That’s certainly interesting.
Sponsored Resources
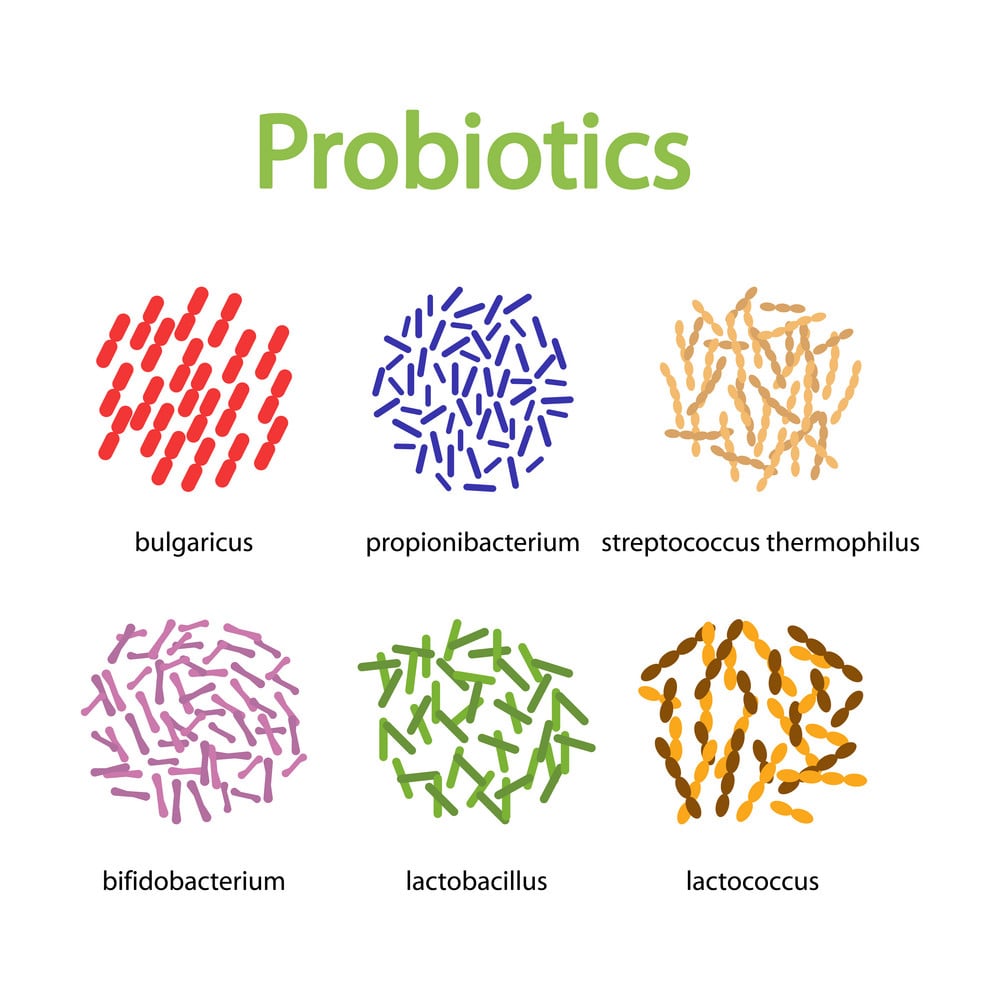
DrMR: Hey, everyone I’d like to tell you about BIOHM, who helped to make this podcast possible. Now, BIOHM offers a line of gut-healing products, including a probiotic, a prebiotic, and a green powder. Now, their probiotic is interesting in the sense that it combines strains from both category 1 and category 2.
So from category 1, you have lactobacillus, acidophilus, lactobacillus rhamnosus, and Bifidobacterium breve. And from category 2, you have S. boulardii, so a nice combination of category 1 and category 2.
And if you go over to BIOHMHealth.com/Ruscio and use the code RUSCIO at checkout, you’ll get 15% off your first order. So BIOHM, they’ve got a good line of probiotic and prebiotic and the greens powder, all to help you improve your gut health, which we know has such massive and far-reaching impacts. So check them out over at BIOHMHealth.com/Ruscio.
Effects of Alkaline Water
ER: So the next question is an audio question about alkalized water.
Faye: Hi, Dr. Ruscio. My name is Faye from Hong Kong. I’ve been listening to your podcast for a few months. I’ve really enjoyed it and I’ve learned lots. I have a question regarding electrolyzed reduced water. A salesperson told me tons of benefits that the alkaline water ionized system can offer. I did some searches on the internet and did find some scientific articles about the benefit of such water, especially its antioxidant capability. But this type of water has quite a high pH, 8.5 to 9.5. I wonder how long-term use of this water would affect stomach acid and overall gut health. I would appreciate if you could share some of your thoughts on this. Thank you.
DrMR: Okay, this is an old question. I remember this came in awhile back and I didn’t have the time to really dig into the literature, and I still haven’t. But I will share with you what I found when I did a quick search and pulled up a couple papers. There are two papers on animals. We have to be really careful what we conclude from animal data. One showed that acidified water may increase Type I diabetes. But another study showed that acidified water decreased diabetes. So kind of a wash there on the outcomes, from a quick poke into animal literature.
I also found one study, entitled “Correlation between water hardness and cardiovascular disease in Mostar City, Bosnia, and Herzegovina.” They concluded that the results might indicate a correlation between the prevalence of cardiovascular disease in a population and those who drink soft water.
I believe that hard water is more mineralized, so it’s more alkalinized. And soft water has less minerals and therefore is less alkalinized. Although, I could be wrong in that assumption. So I honestly don’t know what the body of literature there fully says.
We have wheels in motion to interview someone. We don’t have a guest yet, but we’re trying to find someone who knows this body of evidence and can speak to it objectively. The challenge we’ve run into is that most people who know something about this own companies that sell devices. That doesn’t preclude someone from having an objective opinion. I technically own a company that sells probiotics and antimicrobials, and I like to think I’m not biased in the use of those. I like to think I’m pretty objective. But it does make it harder to get a read, because now we have to evaluate someone on the merits of their argument and whether they’re objective or not.
My guesstimation would be, there’s probably some evidence that shows an association. Whether there are any clinical trials is probably harder to pin down. I think it’s a good idea to drink the healthiest water that you can. One issue we bump into is, how much hoop-jumping do you have to proceed through to get healthy water? And is it worthwhile buying this filter that does 10 functions, rather than just basic removal of toxins? So I don’t know what the answer to that question is. Again, I would shoot for a good water filter.

Now, what does that give you on what to go out and buy? We’re looking into that issue now. There are filters that are somewhat reasonably priced, which reionize and remineralize your water. I think that is probably worthwhile, especially if you’re using reverse osmosis. Though I’ve heard criticisms of reverse osmosis water, because it strips many of the minerals and, I’m assuming (along with the minerals), any ionizing charge. So I think there is something there. I just don’t know if it’s a huge issue. I’m open to it.
I think it’s reasonable to conclude that it’s not necessarily a fundamental pillar. Like, if you could put effort into improving your gut health, your sleep, your exercise, and your diet, I would do that way before I worry about the particulars of your water. If you’ve done those things, and now you’re at the stage where you’re at this cherry-on-top fine-tuning, we will hopefully have a future episode to speak to how much benefit you can get from this and the best cost-benefit.
Another thing we have to be careful of is, if there is a benefit, but the benefit is so infinitesimally small that it’s near negligible. It may not be worth it. Sometimes what you see in various research analyses is something that is statistically significant, but you wouldn’t call it meaningful in the real world. The example I always use here is prebiotics for weight loss. You’re looking at a couple pounds at best, in those who are already obese. For someone who was obese at 225 pounds, losing two to three pounds from a prebiotic was found to be significant mathematically. But clinically meaningful? I’d say it’s certainly shy of that.
So a lot of hot air here to give you a non-definitive answer on the question. But hopefully we’ll have that coming for you soon.
ER: Okay. We’re really working our way around the globe here. We had Israel and Hong Kong. It’s crazy.
DrMR: I know. We’re international.
Analyzing Microbiome Results
ER: So, this question is from Tammy. Tammy is a microbiologist curious about some self-experimentation. She consumes tons of homemade probiotic foods like yogurt, kefir, sauerkraut, and kimchi, but her uBiome results show very low numbers of bifidobacteria and lactobacilli. She also finds it interesting that even though she has lost weight and feels great on a typical high-fat, low-carb diet, she tilts toward firmicutes, which is typical of obese people. Her predominant organisms are the clostridia. She finds the gut microbiome vastly interesting and wanted to get your thoughts on this. P.S. she loves the podcast and can’t wait to read the book.
DrMR: Great. Well, gosh. There’s a lot here to pick into. The thing I’ve found challenging when you look at the research literature is—and I expand upon this in the book—the diets that are best for producing the gut bacteria theoretically most conducive to weight loss don’t lead to the best weight loss. In fact, it’s the diets that theoretically skew the microbiota in an unfavorable way for weight loss that actually lead to the best weight loss.

This is a shining example of why I emphasize looking at outcome data. When you look at outcome data, you’re not going to be misled. What you’re after as a healthcare consumer is doing something to produce the result that you’re looking for. So you’re looking to make an intervention, experience an outcome. The outcome data, the clinical-trial-type data, tells you the answer to the question of: if I do X, Y, or Z, will it produce the weight loss that I’m looking for? Or whatever it is.
So there’s conjecture from looking at mechanisms and other observational data trying to say, if we eat this way, it influences the bugs in that way. And then this leads to a change in metabolism in the other way, and that should lead to a change in weight gain or loss in this way. But along that road of inferences, there are a lot of things we may not yet fully understand, that trump the effect of whatever inference we can actually see.
This is a problem with drawing inferences when looking at mechanisms: you assume that you know everything. Then, we may find a few years later that there’s a whole other pathway or line of pathways we didn’t even know about. And this is why, for example, we see more of a favorable trend in weight loss with diets that reduce the carbohydrate intake, than those that are liberal with the use of carbohydrate intake, including fiber. So meaning, the lower-fiber, lower-carb diets tend to be better for weight and metabolism than do the higher-carb, higher-fiber diets.
Although the effect size, the difference between these, is small. There doesn’t seem to be a huge difference in terms of eating a high-fiber, high-carb diet versus a lower-carb, lower-fiber diet. The lower-carb, lower-fiber diets show more favorability in terms of weight loss, but it’s not a huge difference. It’s maybe anywhere from three to 10 pounds in the study. But one of the problems is that some studies trying to study a low-carb diet are pitting a healthy low-carb diet against a not-very-healthy high-carb diet. So this is an area where we have to be careful. If we’re more on the paleo, low-carb end of the spectrum in what we “agree with,” we have to be careful not to cherry-pick data that supports what we want to think.
I think Christopher Gardner has done a fantastic job with his DIETFITS study. And we’ll have him on the podcast soon to be discussing this. But he compared a healthy, low-fat to a healthy, high-fat diet and he found the outcomes were pretty negligible between the groups. All that is to say, listen to your body. There are even some attempts to use the microbiome—this is a lab known as DayTwo—to predict your glycemic response to food to predict the best diet for you. There does seem to be something there. And they do seem to have a model that works, at least according to the one paper of theirs I read. I didn’t realize that DayTwo had their testing ready for commercial use until we had Professor Rob Knight on the podcast to discuss this.
That would be the best game in town, in my opinion, if you wanted to try to figure out the best diet for a glycemic response. Presumably, that could lead to the best impact on your body composition. I don’t know that the impact on body composition has been fully borne out or if it would be significant, but that’s something to consider.
So there’s a lot to this question and little details that people will get wrapped into. I would make the first barometer your response to a given diet. And it sounds like you’ve already figured out that you seem to do better metabolically, and I’m assuming symptomatically, on a lower-carb, higher-fat diet. So I would, quite simply, continue to do that. The reason why you’re improving from that is probably yet to be fully elucidated via the underlying mechanism, especially in the microbiota. If you wanted to go a little bit further, consider the lab at DayTwo. Something to consider if you want to go further to dial into what you’re eating and optimize your glycemic response.
But at the end of the day, I don’t think modulating the microbiota with special diets or prebiotics is shown to be a really favorable thing for weight loss. My thinking is, if you improve your gut health, you may see a reduction in your weight. But trying to say, “This population is high or low, so I’m going to eat to feed this population of bacteria,” is kind of arrogant on behalf of the scientific community. Thinking we know so much about human metabolism that we can boil it down to a grouping of bacteria, and that is going to have a measurable impact on someone’s metabolism. It assumes that those bacteria are having too much of an impact on someone’s metabolism. The better strategy would be, again, experimenting with a few different dietary modifications or camps, and continuing with the one that you’ve noticed you have the best outcomes on.
View Dr. Ruscio’s Additional Resources
Probiotics Recommendations for SIBO
ER: So we’re at our last question from Kip. He says, “Why do MDs tend to dislike the use of probiotics for SIBO and natural doctors strongly recommend them?”
DrMR: Great question. This is one I’ve spoken to a few times in the past. I should say, you are correct that most MDs dissuade against the use of probiotics. But there are also a fair amount of natural doctors who don’t like using probiotics in SIBO. I think there are two different reasons for this in each respective camp.
I think the medical doctor/medical establishment community are not that comfortable with using non-prescription drugs. And while there are a handful of prescription probiotics, there’s much less in terms of formulations available out there. I think it’s because they’re more used to a drug model and they’re not used to using things like living organisms. I think they’re more used to a model of suppression and blockage, rather than support. Although you could make a counter-argument for hormones (a hormone being a support or replacement).
I think it boils down to the fact that there are probably not a lot of drug company reps going to doctors’ offices, sharing literature with on probiotics. So that combined with the fact that there are only a handful of prescriptions probably has something to do with it. Unfortunately, there is probably a financial incentive behind how quickly information on a given therapy permeates into our profession.
I don’t want to paint that because I’m not a conspiracy theorist. I don’t think there’s a group of guys in some conference room somewhere cackling, saying, “Haha. Everyone’s IBS will be there forever because we’re not allowing them information on the probiotics.” I think it’s more that the more profit these companies make on a product, the more expensive salespeople they can hire to go out and tout their product. And unfortunately, I’m assuming the profit margin on a prescription probiotic like VSL3 is probably not nearly as good as it is for another similar antispasmodic medication for IBS.
So it is a problem, because there is evidence on benefits. But it is ignored. And you see a number of meta-analyses and numbers of clinical trials. I think there have been at least 100 clinical trials using probiotics. It’s a different practice model. That is likely the predominant constellation of factors leading to conventional doctors not using probiotics more. I certainly do not think it’s because there’s any danger or negative side effects, because the dangers are really close to zero (except for soil-based probiotics in severely immunocompromised patients). And the side effects are also close to zero. So it’s not because they’re adhering to “first do no harm.”
I think, rather, it’s just a combination of comfort zone and financial incentives. Again, it’s not the financial incentives of the doctor. I find it distasteful when people criticize the way a doctor practices because they’re making less money. I think most doctors of any stripe chiefly want to help people. But sometimes they are unaware of the biases and the educational system they are in, and they are a pawn in a larger game they may not fully be aware of. Or they may be helpless to do anything about it. There are some doctors that are really overworked, struggling to get by financially, and I include conventional doctors in there. That’s becoming an increasing problem in the conventional medicine community. So they may be slaving away and they don’t have the luxury of taking additional time to do the reading. They’re relying more on the community that they’re in. And unfortunately, there’s a bias selecting out the lower profit-margin probiotics that are pushed into their sphere of sight by sales representatives.
In brief, on the natural side of doctors who sometimes don’t recommend probiotics, there are a couple very—I would consider very—knowledgeable thought leaders in IBS and SIBO who, for reasons I struggle with understanding, are uncomfortable with the use of probiotics. I think there have been two studies to date showing a negative outcome from probiotics. That is what I hear referenced. Just giving it to you straight here, it really irritates me when there has been one meta-analysis of four clinical trials showing that probiotics are an efficacious treatment against SIBO, and dozens and dozens of studies and handfuls of meta-analyses showing that probiotics can improve IBS (just treating IBS symptoms and not SIBO).
To me, that is really disheartening. You would expect experts in this niche area to be familiar with both the pro and con information on a given therapy rather than just citing two studies. Both small. Neither one I would consider very well done. One was with Satish Rao, showing probiotic overuse may cause brain fog in a small number of people. And the other shows that use of probiotics may actually lead to SIBO. But there was no correlation to symptoms. So we don’t even know if the SIBO that was found on the lab testing—on this one small study—correlated to symptoms, or if it was mostly white noise that was meaningless.
Whereas, we have at least four clinical trials showing the ability to lead to an improvement in SIBO and symptoms. And we have a number of clinical trials showing the ability to ameliorate symptoms or at least improve symptoms of IBS when using probiotics. So why that happens, I don’t know. In the clinic, we see some patients only need a good well-rounded probiotic protocol, just like we recommend in Healthy Gut, Healthy You, to see all their symptoms go away.
So while it’s disheartening, I guess it’s job security for me. When doctors keep missing this, these patients end up in our office, we go through some basic therapies, and they end up feeling a lot better. But it’s an unfortunate problem that this simple, safe therapy—that has also been shown to have side benefits like a marginal decrease in cholesterol, blood pressure, and improvement in mood, just to name a few, and improvements in any type of dermatitis and skin conditions—is somehow being eschewed because, who knows, there are two small studies that are a contradiction of the behemoth of positive studies. Yeah, that’s my rant on probiotics.
ER: Good rant. I have a question. Could it also be—and I guess this goes along with lack of education—just lack of understanding of the different categories of probiotics? When you did the podcast breaking down soil-based probiotics and the categories for all probiotics, that really opened my eyes. I can attest 100% to the efficacy of soil-based probiotics on improving my SIBO. So that was a game changer for me. It seemed like everyone before had tried a probiotic with me (I couldn’t tell you which one), and when I said I wasn’t feeling well, they just said, “Okay, then we’re writing off probiotics.” It was tried on me in some sense, but it didn’t seem like they went through the process of trying different kinds.
DrMR: Yeah, and you make a great point. It falls into the lack of, or minimal amount of, prescription options. The only prescription probiotic I know of is VSL3, which is a category one lactobacillus-bifidobacterium blend. But as I understand it, there is no prescription Saccharomyces boulardii, and there is no prescription soil-based probiotic. So that makes it even more challenging for a conventional doctor. They may recommend what I think is called Florastor, which is a popular over-the-counter Saccharomyces boulardii. Again, there’s lack of education and also lack of the clinical drug to use.
And I understand why a conventional doctor would want to lean more towards drugs. Because they live in the space of: here are all these nutritional companies, coming at me with different claims. They’re all telling me how great theirs are. How do I know who’s good? Who’s bad? Who can I trust? Who can I not trust? If I were not in the position of knowing how to vet this stuff, I’d want to go with what’s been FDA-approved. What’s gone through the rigors that the drugs usually have to go through. Not to say that’s always fail-proof, but at least they’re used to that system bringing them stuff that’s supposed to be safe and that they won’t get into legal trouble for using. So I get it.
But with a little bit of education, like, I don’t know, reading a book called Healthy Gut, Healthy You, you could get a good purview of the literature on this, the clinical trials, the different categories, and bring that into your practice. So we’re not far from remedying that situation. I just think we need to get more of these docs to understand that it’s not this boogeyman of ambiguity. And with a little bit of attention, they could probably have a decent protocol to navigate the effective use of probiotics.
Episode Wrap-Up
ER: All right. That was our last question.
DrMR: Sweet. Well, time flies when you’re having fun, huh?
ER: Mm-hmm.
DrMR: All right, guys. Hopefully you got a lot out of that. Keep the questions coming and we will talk to you next time.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ Resources & Links
- Sofi MH, Gudi R, Karumuthil-Melethil S, Perez N, Johnson BM, Vasu C. pH of drinking water influences the composition of gut microbiome and type 1 diabetes incidence. Diabetes. 2014 Feb;63(2):632-44. doi: 10.2337/db13-0981. Epub 2013 Nov 5. PMID: 24194504; PMCID: PMC3900548.
- Wolf KJ, Daft JG, Tanner SM, Hartmann R, Khafipour E, Lorenz RG. Consumption of acidic water alters the gut microbiome and decreases the risk of diabetes in NOD mice. J Histochem Cytochem. 2014 Apr;62(4):237-50. doi: 10.1369/0022155413519650. Epub 2014 Jan 22. PMID: 24453191; PMCID: PMC3966285.
- Gardner CD, Trepanowski JF, Del Gobbo LC, Hauser ME, Rigdon J, Ioannidis JPA, Desai M, King AC. Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association With Genotype Pattern or Insulin Secretion: The DIETFITS Randomized Clinical Trial. JAMA. 2018 Feb 20;319(7):667-679. doi: 10.1001/jama.2018.0245. Erratum in: JAMA. 2018 Apr 3;319(13):1386. Erratum in: JAMA. 2018 Apr 24;319(16):1728. PMID: 29466592; PMCID: PMC5839290.
- DayTwo
- Professor Rob Knight post
- BiohmHealth.com
- Dr. Ruscio’s Additional Resources




Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!