Reading the Symptoms: A 71yo Male Who Responded Extremely Well to HCl - Don’t Miss This Symptomatic Clue
TREATING CLINICIAN: DR. MICHAEL RUSCIO
Patient Info:
- Nathan, 71 year old, male
- Previous Dx
- n/a
- Rx
- n/a
- Chief Complaints
- Bloating – 7-INT
- Gas – 7-INT
- Skin rashes (lichen planus) – 9-CO
- Arthritis in fingers – 1-CO
- Other Symptoms
- Acid reflux (nocturnal)
- Belching
Initial Impression:
- Nathan is a 71yo male, on a vegetarian low FODMAP diet, with a healthy lifestyle, demeanor, and outlook.
- Dx/Rx
- Esophagitis
- Previous Testing
- Endoscopy (esophagitis)
- Onset
- Began experiencing acid reflux while sleeping about 7 years ago. “I was also experiencing frequent belching and passing gas – heartburn was not one of my symptoms. It seems that I am not digesting my food properly.”
- Family History
- Both parents suffered from digestive issues and severe arthritis.
- Prior Treatments
- Enzymes and probiotics have helped. PPIs cause rashes.
- Notes/DDX
- Likely has low HCl, which might have caused reflux, SIBO, and reactivity to FODMAPs.
- Prognosis
- Good to excellent.
- Previous Diets
- Vegetarian low FODMAP diet has been helpful.
Testing:
- Tests ordered
- CMP, CBC w/ diff
- Iron panel, Lipids, Vitamin D
- TSH, Free T4
- H. pylori Breath Test
- Optional:
- Doctors Data Para 3x
- Aerodiagnostics Lactulose SIBO breath test
- Rationale
- GI testing is an option, SIBO, dysbiosis and/or H. pylori could be present. However, there is much that can be done to address these which does not require testing.
- I’d like to assess for anemia, given his age, he is at higher risk for hypochlorhydria-driven anemia. While he is at the lab, we can perform the HP breath test.
- We will also order basic blood work
Recommendations:
- Diet
- Continue Vegetarian Low FODMAP Diet. Do your best to be compliant, but you do not need to be perfect.
- Consider a couple days a week off green tea.
- Lifestyle
- Continue using elevation pillows
- Incorporate weight training, namely squat and deadlifts, into your exercise routine
- NRT
- Vitamin D/K
- GI
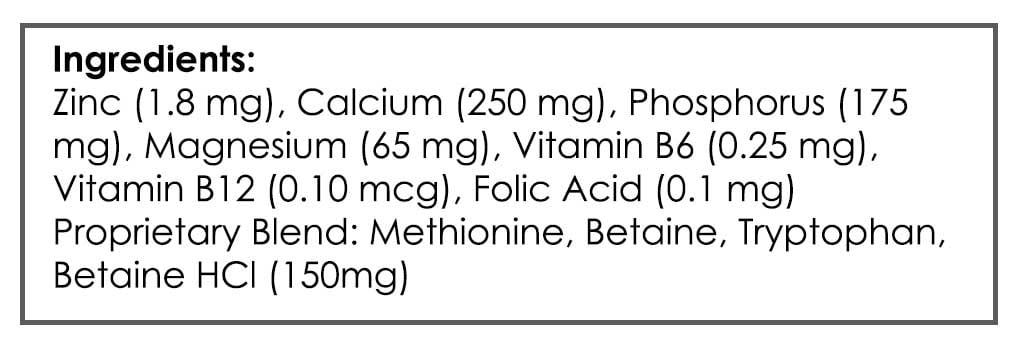
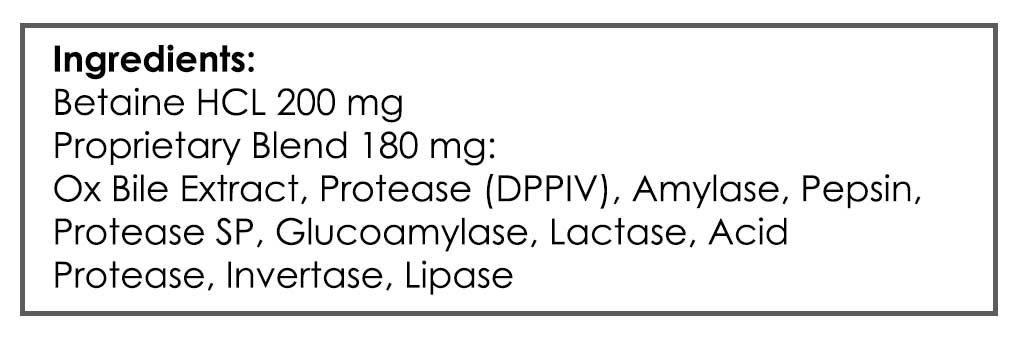
- Digestive Acid HCl + Digestive Enzymes w/ HCl
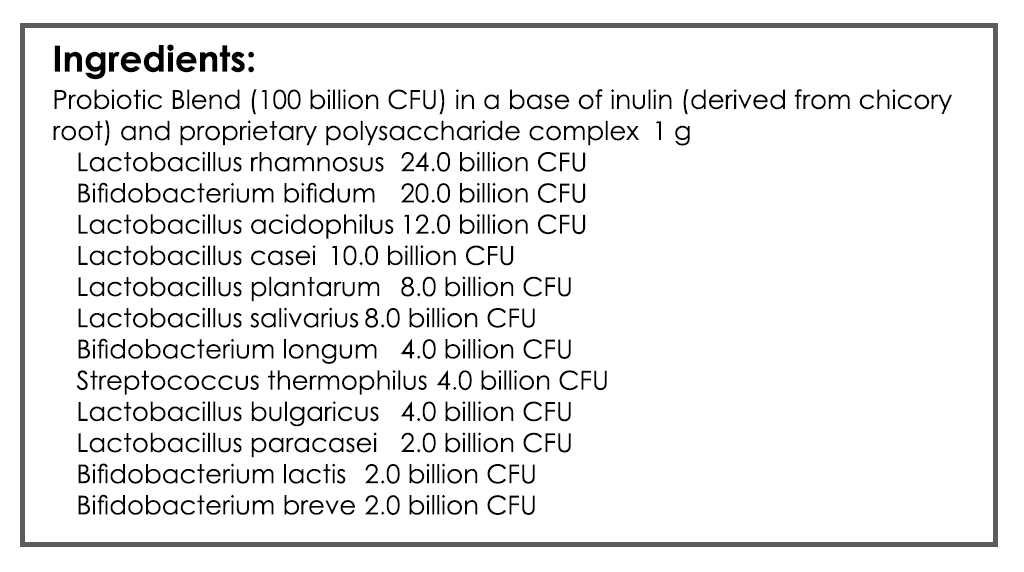
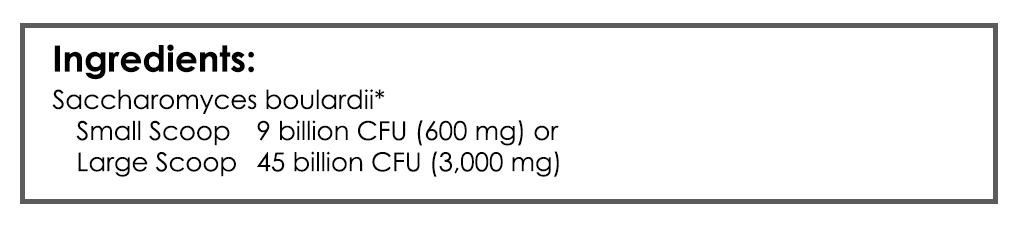
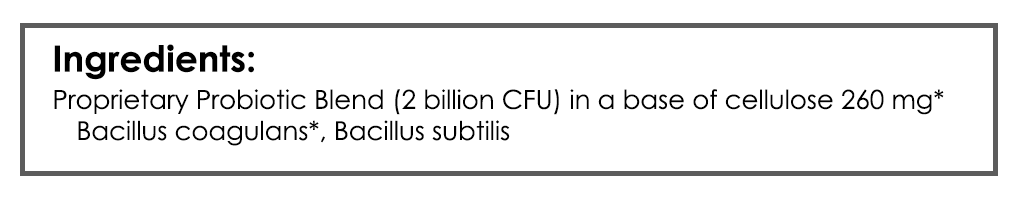
- Lacto-Biff, S. boulardii (take low end of dose range), Soil-Based probiotics
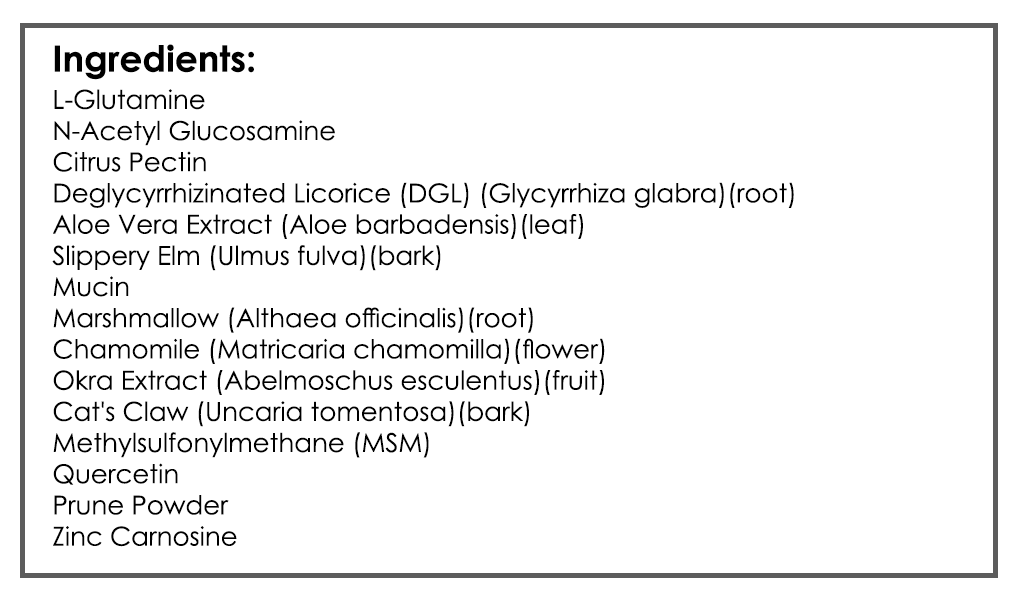
- GI-Revive
- Notes
- Be on the supplements for 3 weeks before following up. Please make a note of the change you noticed from diet versus supplements
- Rationale
- Low FODMAP diet has already been working, so we’ll keep that constant.
- We will encourage continuation of health lifestyle practices.
- We will add an HCl supplement plus a separate HCl-enzyme combo supplement for likely hypochlorhydria. We will also support suspected dysbiosis, overgrowth and/or HP with probiotics. In case there is GI lining irritation, we will add supportive nutrients.
- If I were seeing this patient today, I would stagger the start of HCl/enzyme versus probiotics so as to capture a clearer signal of response to each.
Subjective Assessment:
- Digestive Acid HCl + Digestive Enzymes w/ HCl (3 weeks) – very helpful for bloating, gas, GI upset
- Probiotics + Gut-Healing Nutrients – helpful
- Improved
- Bloating, Gas, Skin Rashes
- Acid Reflux, Belching
- Same
- n/a
- Worse
- n/a
Lab Interpretation:
- CBC w/ diff: Platelets 96-L
- Iron panel: Ferritin 111-WNL
- Lipids: LDL 124-H
- Vitamin D: 50.1-WNL
- Aero SIBO
- Did not perform
- Doctors Data
- Did not perform
Impression:
- Today has done great from HCl/enzymes and from probiotics. All CCs improved and he was able to expand his diet. Will maintain the current plan today then follow up in 2-3 months.
Recommendations:
Starting
- We will review your pending stool test results at your next visit.
- Look up deadlift videos and incorporate into your exercise.
- Continue to expand your diet
- Follow up: 2-3 months
Subjective Assessment:
- Improved
- Bloating, gas, skin rashes.
- Acid reflux, belching.
- Same
- n/a
- Worse
- n/a
Impression:
- Went from 100% to 95%, gurgling, and reflux at night. Has stopped GI nutrients and is taking probiotics every 3 days, so will go back on and dial in dose. Otherwise is done and has responded nicely. Doctor’s Data results came in today and were unremarked.
Recommendations:
- Go back on full program, then experiment one at a time to determine a minimal effective dose of supports.
- Follow up: once yearly or as needed.
Clinician’s Comments
This case provides a good example of what a likely responder to HCl presents as. However, remember how crucial the therapeutic hierarchy is. In this case, yes, a likely HCl responder, but that response is not complete unless we address the more foundational issues of diet, probiotics, and repair.
Clinical Rule: Dysbiosis should be addressed before secretions.
This case study also showcases where the line is for the minimal effective dose. This does not indicate ‘we need to do testing,’ so be careful not to fall into that trap. Clinical observations provided all the data needed here.
If you are seeing clinical response with empiric treatment, then see a regression, learn from that response and be cautious not to rush into testing.
Clinical Rule: Exhaust empiricism before testing (in most cases)
Older version of algorithm here
Hi Everyone,
Below I have updated & better summarized:
- The thyroid hierarchy regarding thyroid hormone replacement therapy, and
- Integrated testing and antibody treatment data.
There is still some work to be done here, but this should do a far better job in putting most everything in one place and with supporting references.
Dr. Ruscio
Thyroid Algorithm
Hypothyroidism
Level 1
- Stand/tablet LT4, with dose adjustments
- Note: Don’t forget to check compliance (is the patient missing doses?) and that the medication is being taken on an empty stomach
- Diet & Lifestyle Foundations
Level 2
- Optimize Gut Health
- Gut tailored diet (ex. low FODMAP), probiotics, elemental reset, etc.
- Treatment of SIBO (if symptoms persist & if electing to test)
Level 3
- Consider higher than normal LT4 dose, perhaps guided by dialysis/LC-MS, targeting TSH in lowest ½ of the reference range
- Consider screening for and treating low ferritin (low=below 100)
- Note: Our experience has been the lower the ferritin the higher the likelihood of subjective improvement upon iron supplements.
Level 4
- Liquid LT4 (Tirosint)
- Consider if TSH and fT4 levels are not fully or consistently responding.
- Combination T4/T3 formula (Nature, WP, etc.) or addition of T3 (Cytomel) to current LT4.
- Hypoallergenic tablet LT4+LT3 (Nature Thyroid, WP Thyroid).
- Consider if levels are responding but symptoms are not, and/or if clear reactions to medication are suspected.
Hashimoto’s & Thyroid Autoimmunity
Testing
Elevated TPO antibodies may pose a 9-19% risk of hypothyroid
- Elevated TPO (here defined as TPO >40) may predict a 9-19% risk of progression to hypothyroidism. Prospective, 5,783 subjects, average 9.1 years follow-up window.
- However, they did not quantify how the degree of TPO elevation tracks the magnitude of risk of developing hypothyroidism. The study below did and provides another point
TPO >500 may be cut off for when clinical intervention is required & risk is present.
TPO most successfully predicts outcomes, data for TG not as strong
- TPO levels of >500 indicate a moderate risk of progression to hypothyroid. TG levels were not predictive. 335 patients, tracked for 6.2 years on average, retrospective (strongest data for this question).
- TPO of >250 had a 16.5% chance of conversion to overt hypothyroidism, over a 2-year follow-up. TPO is also elevated before TSH, so TPO may be an acceptable screening test. Retrospective, 4,581 subjects, 2 years follow-up.
- This study had a larger sample size, but I believe they also used the TPO >250 cutoff for those who become SCH AND those who become true hypothyroid, which may falsely skew this cutoff.
- We are currently doubling checking this, which may require correspondence with study authors. I will update the Thyroid Algorithm based on our findings. More to follow.
- May 2020 FFMR
- This study had a larger sample size, but I believe they also used the TPO >250 cutoff for those who become SCH AND those who become true hypothyroid, which may falsely skew this cutoff.
Thyroid antibodies may track with quality of life and other subjective measures, but a recent meta-analysis may challenge this association.
- TPO was inversely associated with quality of life and maintained even after adjustment for comorbidities. TPO on average was 287. 84 patients assessed via SF-36, mixed group of those on meds and those euthyroid.
- However, a recent 2021 MA of 13 studies found the majority of studies found no association between thyroid antibodies and qualify of life.
- Analysis coming in subsequent FFMR, study link.
Treatment
Selenium (200 mcg/day) reduces TPO antibodies and likely has benefits on quality of life. Use for up to one year, use beyond that should be discouraged.
- 3 meta-analyses have found Se reduces antibodies. 2 of these found improvements in mood, well-being, or quality of life. However, the other MA found increased adverse events in the Se users.
- July 2018 FFMR; MAs 1, 2, 3.
- 16 control trials summarized in a systematic review
Other treatments: Vitamin D, Mg, and CoQ10
- Updates to follow and will be posted here
Can J Gastroenterol. 2005 Apr;19(4):231-4. doi: 10.1155/2005/978794.
Study Purpose
- Assess non-GI symptoms associated with IBS.
Intervention
- Two hundred consecutive patients with IBS (based on the Rome criteria) and 200 patients with documented Crohn’s disease were included in the present study
Main Results
- IBS patients were more likely to complain of headache, urinary dysfunction, chronic fatigue syndrome (CFS), fibromyalgia, or mood disturbance.
- Subjects in both groups frequently reported sleep disturbance.
- Slightly more patients with IBS than IBD described menstrual difficulties, but the difference did not appear to be significant.
- Anxiety and depression were severe enough to warrant specific psychotropic therapy.
Additional Results
- The impact of IBS on sleep is underappreciated in my opinion, when considering how impactful sleep is on overall health.
- It has been estimated that 28% to 74% of IBS patients describe significant difficulties with sleep
- Important female health issues may be caused by IBS, important not to overlook these.
Limitations
- A single-center study, referral bias.
Authors Conclusion
- Aside from the Rome criteria, there are many complaints unrelated to the gastrointestinal tract that characterize patients with IBS. It would appear, therefore, that IBS is a systemic disorder involving many non-gastrointestinal symptoms that are usually labeled ‘functional’.
Clinical Takeaways:
- Problems in the gut (IBS), can cause many non-GI symptoms like fatigue, depression, anxiety, menstrual irregularity, and sleep disturbances.
- What to tell your patients:
- We must start with the health of your gut because problems in the gut can cause many non-gut symptoms like insomnia, fatigue, depression, and menstrual irregularity.
Dr. Ruscio Comments
Great study. Reinforces what many of us probably already know, but it is nice to see published evidence for this clinical observation.
Short-course Rifaximin therapy efficacy and lactulose hydrogen breath test in Chinese patients with diarrhea-predominant irritable bowel syndrome
BMC Gastroenterol 2020 Jun 12;20(1):187. doi: 10.1186/s12876-020-01336-6.
- The non-randomized clinical trial, 78 IBS-D via Rome IV, given 400 mg Rifaximin BID x 2 wks
- LHBT and QOL questionnaire assessed at week 0 and 4
- All participants showed significant improvements in GI symptom subdomains after rifaximin treatment
- QoL scores (SF-36) also improved
- No GI symptoms were associated with SIBO (corroborates findings of other studies)
- LHBT normalization after rifaximin treatment was found in 44.4%
- Conclusion:
- A short course (2 weeks) of rifaximin improved GI symptoms and QoL in Chinese IBS-D patients whether they had SIBO or not. However, the efficacy of rifaximin could not be explained by the successful eradication of SIBO.
Insufficient evidence to support the clinical efficacy of selenium supplementation for patients with chronic autoimmune thyroiditis
Endocrine 2021 Mar 27. doi: 10.1007/s12020-021-02642-z. Online ahead of print.
- A systematic review of 23 trials examining the use of selenium in AITD
- In LT4-treated populations, patients receiving selenium demonstrated lower thyroid peroxidase antibody (TPOAb) levels at 3 months (mean difference [MD], -237), 6 mo (MD, ‑407), and 12 months (MD, -327)
- In the non-LT4-treated population, the selenium group demonstrated significantly lower TPOAb levels after 3 months, 6 months, but not 12 months
- Selenium not needed FOREVER
- There was no significant change in thyroid-stimulating hormone (TSH) levels in either group
- Lower thyroid echogenicity was observed in all patients receiving selenium at 3, 6, and 12 months.
- Se supplemented participants had a significantly higher risk of reported adverse effects.
- Conclusions:
- Current evidence does not justify the emerging use of selenium supplementation in the treatment of AIT, despite it resulting in a decrease in autoantibody levels.
- Note: Not sure I agree