Practitioner Research Review – July 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- Dr. Ruscio’s Thyroid Medication Review: T4 Versus Combination Therapy (T4+T3)
- The Gut-Thyroid Connection, Profound but Underappreciated: Dr. Ruscio’s presentation at the LDN conference in June 2019.
- Rapid-fire Research – ultra concise summaries of noteworthy studies
- Randomized placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome
- Effect of vitamin D3 supplementation on blood pressure in adults: An updated meta-analysis
- Thyroid-stimulating hormone (TSH) serum levels and risk of spontaneous abortion: A prospective population-based cohort study.
![]()
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Dr. Ruscio’s Thyroid Medication Review: T4 Versus Combination Therapy (T4+ T3)
This was a lot of work. Painstaking evaluating the data, in a neutral fashion, while also attempting to identify any gaps in the research that are clinically relevant. Below you will see my analysis, comments, and conclusions. If this has helped you, please encourage others to join the newsletter as I feel it is vital to disseminate this information to more clinicians.
The case for combination therapy. Evidence is not a strong one as proclaimed to be but is an understandable misread of the data.
- Survey of over 12,000 individuals found an overall higher treatment satisfaction on combination therapy compared to T4 and decreased the likelihood of complaints related to weight, fatigue, mood, and memory. [1]
- In those not responding to T4 alone, evidence (South Med J) does exist documenting improvement when switching to combination therapy. However, this study is not great data, because there is no blinding nor control. Other large trials (Saravanan et al, J Clin End 2005, roughly 600 subjects) indicate placebo may drive this ‘improvement’. Saravanan et al. found patients will report benefit any time there is a change (or perceived change) in their medication, irrespective of the change. This improvement is visible at 3 months and then often disappears by 12 months. Meaning placebo effect is substantial. [2,3]
T4 Versus combination therapy – weighing the evidence
- All 4 systematic review (SR) and/or meta-analyses (MA) published to date, have concluded no difference [4]
- MA of 10 RCTs, 1153 patients.
- They analyzed biochemical variables, psychological and physical well-being, and patient preference (4 studies). “T4 alone may be beneficial in improving psychological or physical well-being.” No other measures were statistically significant.
- MA of 9 RCTs, 1141 patients [5]
- “no significant difference in treatment effect on psychiatric symptoms in the nine controlled studies to date.”
- MA of 11 RCTs, 1216 patients. [6]
- They analyzed biochemical variables, psychological and physical well-being, and did not assess patient preference. No difference between therapies.
- SR of 9 RCTs, 1082 patients. [7]
- They did not analyze anything statistically as this was only SR (no MA analysis as described in the next Table 4).
- MA of 10 RCTs, 1153 patients.
- Most up-to-date (2018) review found no difference between T4 vs combination therapy. [8]
- The above Meta-Analyses analyzed a common set of 8 RCTs. The 2018 review added 4 new RCTs. What did these 4 new RCTs find?
- A handful of smaller studies have found a preference for combination therapy
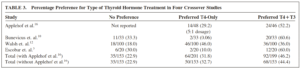
- Table 3 from Psychosomatics. 2007 Sep-Oct;48(5):379-84. 9 RCTs, 1141 patients
- Recap: The overwhelming majority of data does not support a preference for combination therapy. What happens when we look closer at the small number of studies suggesting that combination therapy is superior?
- The meta-analysis in Psychosomatics 2007 did find a slight but insignificant numeric preference for combination therapy, roughly 10% preferred combination therapy. How do we account for this? In short biased and/or placebo.
- The three SR/MAs with “No significant difference in preference” did a heterogeneity/bias analysis and the one “Preference for LT4/LT3” did not do a heterogeneity/bias analysis.
- Also, even while this fourth study found a numeric preference, it was not tested for statistical significance. So biased or placebo may be an important factor in interpreting the data.
- “But my patients report feeling better after switching to combination therapy.” Placebo effect after changing medication is significant and likely has a large effect on biasing results.
- Journal of Clinical Endocrinology and Metabolism 2005, Saravanan et al.
- 697 patients were blinded, then either put back on T4 (same medication as prior) or combination therapy (substitution of 10 µg T3).
- There was a 39% improvement in psychiatric symptoms in the placebo group! It was sustained at 12 months. The T3 group improved also, however, their improvements were lost at 12 months.
- Leading the authors to conclude
- “They [study results] also emphasize the large and sustained placebo effect that can follow changes in thyroid hormone administration.” [13]
- Other studies have also found the placebo effect to be substantial. Nygaard 2009 found that any perceived change in medication leads to a significant symptomatic improvement from baseline, even if the medication did not change. [14]
- Recap: some data do support combination therapy being better. However, as data quality improves (larger sample size, control group, reduction of placebo…) the finding of combination therapy being superior is attenuated. Thus, the best data finds no superiority of combination therapy. Reminder, this is different than say probiotics versus Rifaximin for IBS. In this situation, probiotic studies are not as large, nor as rigorous, as the drug studies, so we can’t do an apple-to-apple comparison, we don’t have the data. With thyroid hormone comparisons, we do.
Do genetics predict preference for combination therapy? Maybe. The data here are roughly split with perhaps a slight edge suggesting genes do dictate preference of medication. However, the same genes have not been tested across all studies, making exactly what to test unclear. Due to these inconsistencies, testing is unnecessary, in my opinion.
- RCT of 45 patients in Eur Thyroid Journal 2107 found that as the number of polymorphisms (SNPs) increase, so did preference for combination therapy. With no polymorphisms, 1 or 2 the preference for combination therapy was 42 vs. 63 vs. 100%. No placebo effect here (prospective, double-blind, cross-over). T3 levels correlated with a preference for combination therapy. Some genes here can be assessed by 23andMe, Ancestry, FamilyTreeDNA… [15]
- Another RCT in 552 subjects found that genetics (SNPs) predicted both poor response to T4 alone and preference for combination therapy. The effect persisted at a 12-month follow-up. A general health questionnaire was the measure. T3 levels did not differ between groups. [16]
- Not all data show genes dictate preference. RCT in 141 patients found genes did not dictate response or preference to T4 therapy or T4/T3 combination. [17]
- In an observational cohort study of 364 subjects on thyroid hormone found no association with the type of medication (T4 only) or D2-Thr92Ala polymorphism and any thyroid hormone measure (TSH, fT4, fT3), comorbidities, health-related quality of life or cognition. [18]
- Other data regarding genetics and conversion can be found here. [19]
Clinical Takeaways:
- The utility of combination therapy has been overstated, most do not require combination therapy.
- There is evidence showing that patients prefer combination therapy, however, the better the level of evidence the more diminished the preference becomes.
- Most anecdotal reports stating combination therapy to be effective/better are likely due to the placebo effect.
- Genetics (conversion) may predict who requires combination therapy, but further research is required.
- A small subset of patients (perhaps 10%) may, in fact, feel better on combination therapy, so clinicians should remain open to this and make consideration as part of a complete thyroid algorithm.
- Do not forget this as a potential cause of the non-responsive symptoms of thyroid hormone levels.
What to tell your patients:
- Combination therapy is a consideration; however, its beneficial effects have been overstated by functional/natural medicine. We will start you on T4 while working to improve your gut health which might be causing all your symptoms. In fact, improving your gut health might also lead to a reduced medication need and improvement in thyroid autoimmunity. Then, we will re-evaluate and this is when a trial on combination therapy makes sense.
Dr. Ruscio Comments
Be careful not to chase thyroid at the expense of gut health. Dr. Mather’s and Dr. Abbott’s recent case studies (May and June 2019) have reinforced this. Both are important, make sure you have the appropriate sequencing and this will improve outcomes.
The Gut-Thyroid Connection, Profound but Underappreciated
Dr. Ruscio’s presentation at the LDN conference in June 2019.
Rapid-Fire Research: Ultra-Concise Summaries of Noteworthy Studies
Randomized placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome
https://gut.bmj.com/content/early/2018/08/14/gutjnl-2017-315136
Conclusion
- “In patients with IBS-D with intestinal hyperpermeability following an enteric infection, oral dietary glutamine supplements dramatically and safely reduced all major IBS-related endpoints. Large randomized clinical trials (RCTs) should now be done to validate these findings, assess the quality of life benefits and explore pharmacological mechanisms.”
Effect of vitamin D3 supplementation on blood pressure in adults: An updated meta-analysis
Nutr Metab Cardiovasc Dis. 2016 Aug;26(8):663-73. doi: 10.1016/j.numecd.2016.04.011. Epub 2016 Apr 25.
Study purpose
- A meta-analysis of evidence regarding vitamin D supplementation’s impact on blood pressure
Findings
- A total of 30 RCTs, including 4,744 participants were included.
- The mean duration of the studies was 5.6 months, and doses of VD3S varied between 200 and 12,000 IU/day.
- “VD3S had no effect on SBP (-0.68 mmHg), and DBP (-0.57 mmHg).” Note: overall no effect found, but when subanalysis performed it was found that using higher doses (>800 IU) and in older subjects (≥50) there was an effect.
- Subgroup analysis revealed that daily vitamin D3 therapy at a dose of >800 IU/day for <6 months in subjects ≥50 years old reduced both SBP and DBP (p < 0.001).
- The effect of vitamin D appears to depend on age, dose, and other comorbidities.
- “In addition, VD3S showed hypotensive effects in healthy subjects and hypertensive patients, but a hypertensive effect in overweight and obese subjects. However, after excluding overweight and obese subjects, VD3S significantly reduced SBP and DBP.”
- Vitamin D with calcium might pose a risk.
- VD3S in combination with calcium supplementation significantly elevated SBP (3.64 mmHg,) and DBP (1.71 mmHg).
- No evidence of publication bias was found.
Conclusion
- The effects of VD3S on blood pressure depends on the dose of supplementation, treatment regimens, trial duration, and population subgroup.
- Supplementation may be beneficial at daily doses >800 IU/day for <6 months in subjects ≥50 years old.
What to tell your patients:
- Vitamin D may help reduce blood pressure. However, the effect is small, might only occur in older individuals (over 50) and may not occur if you are taking calcium or overweight.
- The dose contained in a multivitamin may not be enough to create benefit, over 800 IUs per day is needed.
- Remember that sun exposure is important and vitamin D is not a substitute for the healthy lifestyle practice of regular exposure to the sun. Also, remember never to burn and be cautious when obtaining sun exposure that you do not overdo it. You’re better off getting 15 minutes on most days than getting 2 hours once per week.
Thyroid-stimulating hormone (TSH) serum levels and risk of spontaneous abortion: A prospective population-based cohort study.
Clin Endocrinol (Oxf). 2019 Jul;91(1):163-169. doi: 10.1111/cen.13979. Epub 2019 Apr 15.
Conclusion
- “Our finding suggests that the upper limit for the TSH normal range should be redefined to <2.5 mIU/L during the first trimester of gestation.”
- Note: pregnancy is a time when we should be meticulous with thyroid assessment and is one of the few exceptions when normal range perturbations in TSH can be consequential.
If you have found this information helpful please share with a friend using this link: https://drruscio.com/review/
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!