Inflammation – The Silent Thyroid Disruptor
“All steps of thyroid hormone synthesis, from iodide uptake to thyroid hormone secretion, may be affected by cytokines (aka inflammation), the effects of which are generally inhibitory.” 1
Inflammation is a big deal. The more we research the effects of inflammation the more we realize how inflammation is one of the main unifying commonalities in most chronic disease; thyroid disease is certainly no exception. In the short term the inflammatory response is beneficial, it helps us deal with injury and infection. However, when inflammation becomes chronic it becomes a problem. The textbook characteristics of inflammation are redness, swelling, pain, heat and altered function. This list is great for medical students trying to prep for an exam, but this classical definition is slightly misleading. This is misleading because often times people are inflamed and have to idea, hidden inflammation. People usually recognize the symptoms that are a by-product of the inflammation, but fail to connect the fact that this hidden inflammation is causing their symptoms. The percentage of people who are inflamed can range from 12% in healthy to 80% in those considered ‘not healthy’ (overweight or have high blood pressure, etc…) It seems safe to say that 1 in 3 people are inflamed in the US population. 2 Inflammation has been correlated with a myriad of diseases and symptoms, but we will stay focused on thyroid. Before we dive into the red, hot, swollen world of inflammation and thyroid one quick thought.
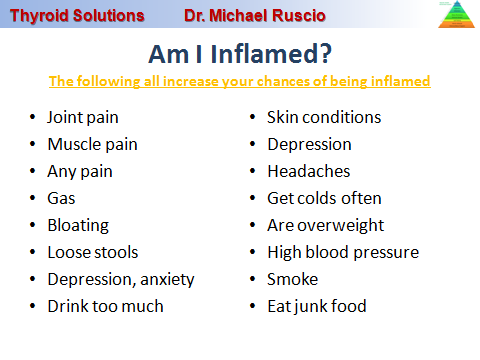
How do you know if you are inflamed? If you have any of the following it is highly likely you are inflamed; joint pain, muscle pain, any pain, gas, bloating, loose stools, depression, skin conditions, depression, headaches, get colds often, are overweight, have high blood pressure, smoke, eat junk food, drink excessively, there are more but this will give you an idea.
|
Did you know? In experiments where people are injected with inflammatory compounds, near immediate changes in thyroid function are observed… |
It is great to want to ‘treat’ or lower your inflammation, but don’t forget to ask the question, “why am I inflamed”? The three main factors implicated in the chronic inflammatory process are diet, gut health and chronic infections, although stress and toxins can play a role also. No, it’s not a deficiency of some miracle berry that grows in the rain forest of Peru that you can but for 89.99 a bottle. Diet, gut health and infections will produce inflammation which will; age you faster, rob you of energy, derange your thyroid function and make you feel ill. We discussed the infection piece already in the infection section and we have also discussed some key dietary concepts, but as a quick refresher remember to do the following; avoid over indulgence in high carb. foods, identify and avoid foods you’re allergic to, ensure you are consuming adequate omega 3s, avoiding excess omega 6s and make sure you are eating fresh vegetables for their anti-oxidant content.
If you are inflamed, Euthyroid Sick Syndrome is the most common manifestation of thyroid problems. Euthyroid sick syndrome (EST) basically means your lab work looks normal but you have symptoms of thyroid disease. Sound like you? Well you are certainly not alone because this is a common complaint.
This all sounds good Dr. Ruscio, but I have been to the best endocrinologist in my area and they have never mentioned I am inflamed. This means I can skip this chapter right? Wrong, you cannot make this assumption. Why? Without going too far down the rabbit whole, this is again because you cannot assume a conventional screening will pick up all cases of inflammation. The standard marker for inflammation, CRP (C-reactive protein), is not always elevated in patients with inflammation. 3
Additionally some medications can mask inflammation, causing whats known as a false negative; meaning you tested negative for inflammation but it was actually present. Statins, a family of cholesterol lowering drugs, are one example of this.
There are numerous way in which inflammation can interfere with your thyroid; the peer reviewed medical literature suggest at least 7 pathways through which inflammation can inhibit your thyroid; lets look at a few. 1
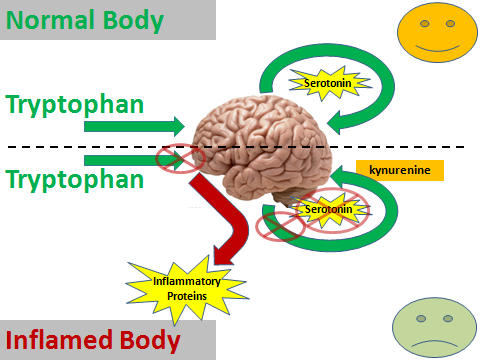
Inflammation can interfere with neurotransmitters (your happy mood & focus brain hormones) and properly levels of neurotransmitters are needed to stimulate TSH. This is likely one reason why thyroid patients have a higher incidence of depression. Said again simply, when the happy mood chemicals in your brain are off, your brain doesn’t make as much TSH and you can then become hypothyroid.
Hopefully this makes sense. If not there is another pathway that is slightly easier to understand. Inflammation will directly interfere with TSH secretion and can hence throw off your thyroid. Remember that TSH is secreted by the brain and tells your thyroid to work, so if this is off your thyroid function will certainly suffer. 6, 7, 8, 9, 10, 11
One of the most popular nutrients you will hear about regarding thyroid is iodine. Some say you need iodine or will become hypothyroid, others say iodine can make your thyroid worse. We will discuss this further in later sections, but for now all you need to know is iodine can be helpful or hurtful depending on your situation. So you need to have iodine in the right balance. How does inflammation tie in? Inflammation can interfere with proper transportation of iodine into your thyroid gland. Inflammation interferes with the door needed for iodine to get into your thyroid known as the sodium-iodine symporter. When the function of this door is altered, it can make iodine damaging to your thyroid. 12
Before anyone with thyroid autoimmunity supplements with iodine they need to make sure this door is working or they risk damaging their thyroid.
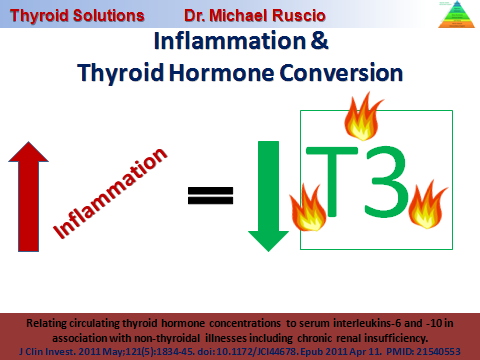
Inflammation can inhibit conversion of T4 to T3, 13, 14, 15, 16 and inflammation can
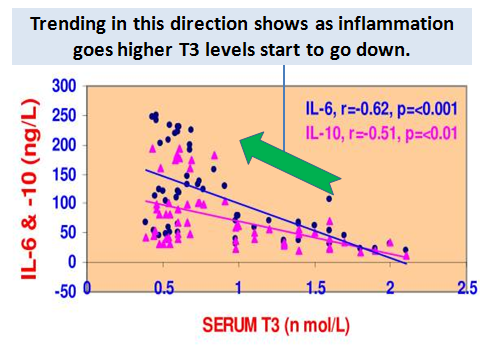
Here is the real world proof that inflammation is bad news for your thyroid. A study was published in the BMC of Endocrine Disorders medical journal in 2008. This study looked at 60 patients that had disorders that caused high levels of inflammation compared to 20 healthy controls. What they found was the higher inflammation was in these patients blood, they lower their T3 levels were. This is a graph from the study, IL-6 and IL-10 are two inflammatory proteins and of course on the other axis you will see our beloved T3. Each dot on the graph represents a patient and the lines show the trends between all the patients’ levels of inflammation (IL-6 & 10) and their T3 levels. Again the trend line shows that as inflammation goes up T3 levels go down. 14Interestingly some studies have shown that antioxidants can undo some of the thyroid problems caused by inflammation. 12
Are you sure Dr. Ruscio? Maybe people who have autoimmunity are ill and that is what’s inhibiting their thyroid function and the inflammation is just an innocent bystander? That is a fair question. Three studies have been done in which healthy patients were injected with inflammatory compounds, all of these studies showed various forms of thyroid inhibition after injection of inflammatory compounds. 19, 20, 21, 22
Whew, OK Dr. Ruscio you are making a strong case for the negative effects inflammation on my thyroid. Great, but hang in there we are not done yet. As if all this wasn’t enough, inflammation can directly provoke thyroid autoimmunity (hashimoto’s, Graves). 23
We have already discussed how certain factors that cause inflammation are known to also provoke autoimmunity; food allergies, intestinal inflammation and infections. It has also been documented that deficiencies in certain anti-inflammatory nutrients like vitamin D and fish oil are correlated with increased risk for autoimmunity. We also know that supplementing with certain anti-inflammatory nutrients (vitamin D, fish oil, antioxidant) and taking certain anti-inflammatory drugs are helpful with autoimmunity. What is the connection? In the chapter on autoimmunity we discussed the concept of the immune system being over stimulated to ‘attack’ and how this is a major factor in autoimmunity. Well, inflammation is the attack signal for your immune system. Specifically things known as cytokines, like the IL-6 and 10 we discussed earlier, tell your immune system to attack in a variety of ways.
We just covered a lot. To bring us back to the big picture remember one thing; decreasing levels of inflammation in your body will be helpful in managing almost any thyroid condition. Also remember inflammation and the immune system are intimately linked. And one final reminder, while yes in some cases thyroid medications will be needed, thyroid medication will not treat the causes of inflammation; the source of the inflammation must be determined and address for you to regain optimal thyroid function.
Please note the next section is available through the sample chapter request box at
- Eur J Endocrinol. 1998 Jun;138(6):603-14. PMID: 9678522
http://www.ncbi.nlm.nih.gov/pubmed/9678522 - Brain Behav Immun. 2006 Sep;20(5):498-504. PMID: 16330181
http://www.ncbi.nlm.nih.gov/pubmed/?term=16330181 - http://www.2healthandwellness.org/uploads/9/4/3/5/9435545/895790_orig.gif?177
- Neuro Endocrinol Lett. 2007 Dec;28(6):826-31. PMID: 18063923
http://www.ncbi.nlm.nih.gov/pubmed/?term=18063923 - Brain. 1992 Oct;115 ( Pt 5):1249-73. PMID: 1422788
http://www.ncbi.nlm.nih.gov/pubmed/?term=1422788 - Metabolism. 1998 Oct;47(10):1289-93. PMID: 9781636
http://www.ncbi.nlm.nih.gov/pubmed/?term=9781636 - Endocrinology. 1996 May;137(5):1591-8. PMID: 8612490
http://www.ncbi.nlm.nih.gov/pubmed/?term=8612490 - J Clin Endocrinol Metab. 1990 Oct;71(4):817-24. PMID: 2169479
http://www.ncbi.nlm.nih.gov/pubmed/?term=2169479 - J Clin Endocrinol Metab. 1990 Jun;70(6):1735-43. PMID: 2112152
http://www.ncbi.nlm.nih.gov/pubmed/?term=2112152 - J Clin Endocrinol Metab. 1990 Dec;71(6):1567-72. PMID: 2229314
http://www.ncbi.nlm.nih.gov/pubmed/?term=2229314 - J Clin Endocrinol Metab. 1995 Nov;80(11):3140-4. PMID: 7593416
http://www.ncbi.nlm.nih.gov/pubmed/?term=7593416 - J Clin Invest. 2011 May;121(5):1834-45. doi: 10.1172/JCI44678. Epub 2011 Apr 11. PMID: 21540553
http://www.ncbi.nlm.nih.gov/pubmed/?term=21540553 - J Clin Endocrinol Metab. 1993 Dec;77(6):1695-9. PMID: 8263160
http://www.ncbi.nlm.nih.gov/pubmed/?term=8263160 - BMC Endocr Disord. 2008 Jan 22;8:1. doi: 10.1186/1472-6823-8-1. PMID: 18211669
http://www.ncbi.nlm.nih.gov/pubmed/?term=18211669 - J Endocrinol Invest. 1994 Apr;17(4):269-74. PMID: 7930379
http://www.ncbi.nlm.nih.gov/pubmed/?term=7930379 - Metabolism. 1998 Oct;47(10):1289-93. PMID: 9781636
http://www.ncbi.nlm.nih.gov/pubmed/?term=9781636 - J Endocrinol Invest. 1994 Apr;17(4):269-74. PMID: 7930379
http://www.ncbi.nlm.nih.gov/pubmed/?term=7930379 - Metabolism. 1998 Oct;47(10):1289-93. PMID: 9781636
http://www.ncbi.nlm.nih.gov/pubmed/?term=9781636 - J Clin Endocrinol Metab. 1990 Dec;71(6):1567-72. PMID: 2229314
http://www.ncbi.nlm.nih.gov/pubmed/?term=2229314 - J Clin Endocrinol Metab. 1995 Nov;80(11):3140-4. PMID: 7593416
http://www.ncbi.nlm.nih.gov/pubmed/7593416 - J Clin Endocrinol Metab. 1994 Nov;79(5):1342-6. PMID: 7962327
http://www.ncbi.nlm.nih.gov/pubmed/?term=7962327 - Q J Med. 1992 Jan;82(297):33-42. PMID: 1332102
http://www.ncbi.nlm.nih.gov/pubmed/1332102 - Eur J Endocrinol. 1998 Jun;138(6):603-14. PMID: 9678522
http://www.ncbi.nlm.nih.gov/pubmed/9678522
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!