How Natural Menorrhagia Treatments Can Improve Heavy Periods
How To Balance Your Hormones to Improve Heavy Menstrual Bleeding
- What Is Menorrhagia?|
- Symptoms|
- Causes|
- Diagnosis and Treatment|
- Conventional Treatment|
- Balancing Hormones for Treatment|
- Gut-Hormone Connection|
- Diet and Probiotics|
- Herbs|
- The Bottom Line|
- Recommended Products|
Menorrhagia — pronounced men-or-raj-ee-a — simply means heavy menstrual bleeding. Menorrhagia can affect women of any age, and is often due to hormonal imbalances. Treatments must address hormones or other root causes.
Improving gut health with diet and probiotics and relying on gentle and proven herbs for heavy menstrual bleeding and the fatigue that can come with it are the best natural menorrhagia treatment strategies.
In this article, we’ll discuss what menorrhagia is, potential causes of menorrhagia, and how you can work on naturally bringing heavy menstrual bleeding back into balance.

What Is Menorrhagia (Heavy Menstrual Bleeding)?
Menorrhagia is heavy menstrual bleeding, usually during a menstrual period. Menorrhagia is one of the most common gynecological problems for women of reproductive age 1. In the US, 20-30% of women who seek gynecological care will present with menorrhagia each year 2.
During your monthly period, your endometrium (uterine lining) normally sheds the tissue that has built up to support a potential embryo.
However, women with menorrhagia experience abnormal uterine bleeding or very heavy menstrual flow during their periods.
During a normal menstrual period, typical blood loss is 10 to 80 mL, with 35 mL being average. Women with menorrhagia and heavy periods may have menstrual blood loss of more than 80 mL per menstrual period 1. Menorrhagia can also happen during or after menopause, at which time it is a serious concern warranting immediate medical attention.
Symptoms of Menorrhagia
There are a few simple signs and symptoms of menorrhagia. The defining symptom is heavy bleeding during the menstrual period, which can lead to anemia. Here is a summary of symptoms:
- Heavy periods or menstrual flow of 80 mL or more per menstrual cycle, or the perception of heavy blood loss 1. This includes:
- Soaking tampons or pads within two hours
- Finding blood clots larger than a quarter 3
- Bleeding for longer than a week 3
- Needing to double up on pads or tampons to control menstrual flow 3
- Needing to change sanitary protection at night 3
- Missing school, work, or other important activities because of heavy menstrual flow 3
- Symptoms of anemia, such as fatigue or heaviness from frequent, heavy blood loss
- Vaginal bleeding after menopause
- May co-present with dysmenorrhea (painful periods)
These symptoms often translate to a reduced quality of life for women with menorrhagia, especially during their periods.
Causes of Menorrhagia
Many causes of menorrhagia are hormonal. This includes estrogen dominance conditions like polyps, adenomyosis and endometriosis, uterine fibroids, endometrial cancer, and other hormonal conditions, like polycystic ovaries, or thyroid imbalances.
The American College of Obstetricians and Gynecologists (ACOG) consider bleeding disorders like Von Willebrand disease as other potential causes of heavy menstrual bleeding 4.
Some of these causes absolutely require conventional medical treatment, but the underlying hormonal imbalances that can cause heavy menstrual bleeding can be easily influenced by diet and lifestyle interventions such as diet, stress reduction, and hormone balancing herbs.
Natural Menorrhagia Treatment
If you present with abnormal uterine bleeding, your doctor will consider your medical history and might order a procedure called intrauterine hysteroscopy, which uses a scope to view the inside of the uterus. If something doesn’t look right, they may take a biopsy after dilation of the cervix, to check for cancer or other abnormalities.
Once serious concerns are ruled out, you can turn your attention to balancing your hormones naturally. Let’s discuss.
The Gut-Hormone Connection in Menorrhagia
Improving your gut health may be a viable strategy for menorrhagia treatment.
Gut imbalances, such as bacterial dysbiosis or inflammation from eating processed foods, are seen as stress by your body. This low-level, underlying stress can deplete your sex hormones to produce stress hormones instead. High stress levels have also been shown to increase leaky gut 5 6.
Other research indicates that your hormones are also affected by these gut-related issues:
- Poor fat digestion 7 8
- The diversity and balance of gut bacteria 9 10 11
- The female reproductive tract microbiome 12 13
This means that supporting your gut health can likely help rebalance any hormonal causes of menorrhagia.
All of this evidence suggests that a healthy gut microbiome improves hormone levels and reduces your susceptibility to hormone-related disorders, including some causes of menorrhagia.
Diet for Menorrhagia: Eat to Balance Blood Sugar
Blood sugar imbalance is associated with an increase in hormonal symptoms like PMS 14, and painful periods 15. This likely because frequently fluctuating blood sugar is interpreted by your body as stress. What you eat also affects your level of gut inflammation, which is also considered stress by your body.
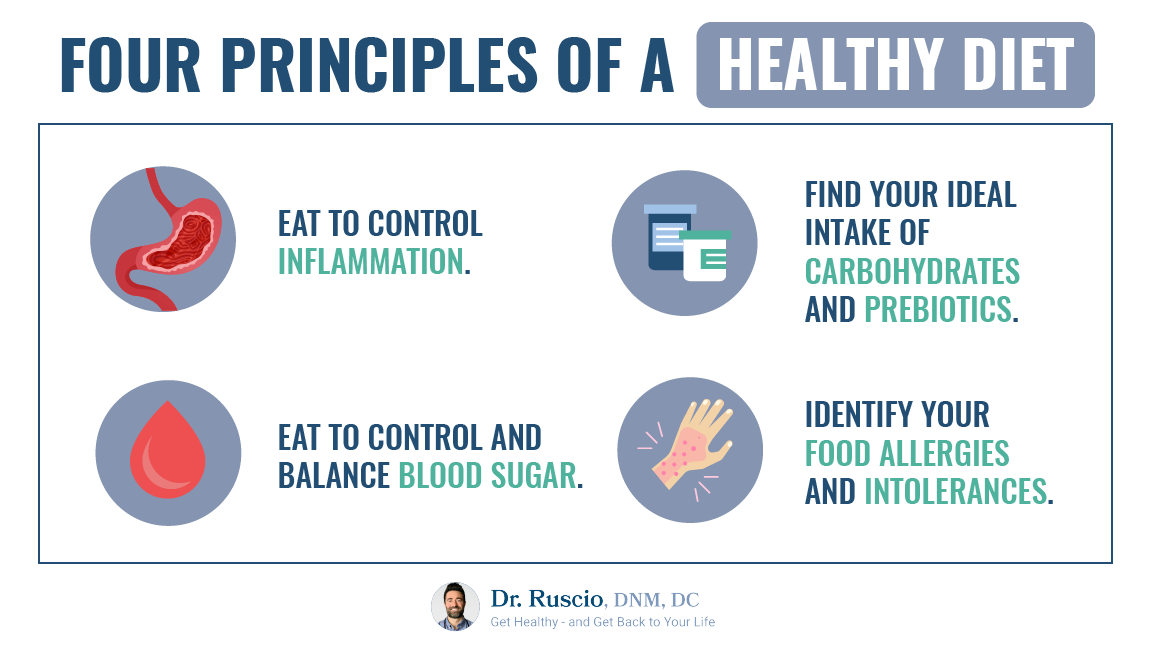
A simple, whole-foods diet template free of inflammatory or processed foods, like the paleo diet, may help improve your heavy menstrual bleeding. That’s because the paleo diet follows the four principles of a healthy diet.
Eating a real-food, anti-inflammatory diet reduces the causes of many hormonal disorders by improving your gut health, reducing inflammation, and keeping your blood sugar stable.
Probiotics for Menorrhagia
Probiotics can further improve your diet gains by crowding out bad bacteria 16 17 18, reducing gut inflammation 19, improving digestive symptoms (which often co-occur with hormone symptoms) 20 21, and reducing leaky gut 22 23 24.
We don’t have data that specifically show that using probiotics improves menorrhagia, but there is some evidence that probiotics can improve hormonal conditions in women. For example, a systematic review and meta-analysis of 855 women with PCOS found that probiotic supplements improved inflammatory and hormonal markers 25.
Another study showed that women with more fecal microbiome diversity had more estrogen metabolites in the urine, suggesting that they had better estrogen detoxification 13.
Triple probiotic therapy (incorporating one high-quality product from each of the three main types of probiotics) is a simple, easy way to make progress on both your gut and hormone symptoms. (See the Probiotic Starter Guide for more information.)
Herbs To Improve Hormones
Along with simple dietary changes and probiotics to support gut health, a few simple herbs help gently and naturally balance female hormones. Complex protocols generally aren’t necessary.

If we presume that some cases of menorrhagia are due to hormone imbalances, a simple trial of herbs that have been shown to balance estrogen and progesterone levels is worth a test, especially considering the potential side effects of oral contraceptives and other pharmaceutical treatments.
For example, the herb chaste tree berry (Vitex) was shown in a clinical trial to reduce heavy menstrual bleeding almost as much as pharmaceutical treatment 26. Additionally, a systematic review of three clinical trials found that ginger capsules and myrtle fruit syrup significantly reduced menstrual duration and blood loss compared to a placebo 4. Pomegranate flower capsules were also as good as tranexamic acid at reducing blood loss 4.
But often, simple blends of herbs — such as gamma oryzanol, black cohosh, dong quai, licorice root, and trans-resveratrol to balance estrogen levels 27 28 29 30, or a blend of licorice root, white peony, and chaste tree berry (vitex) to balance progesterone — has been shown to improve menstrual symptoms 31 32 33.
Keeping it simple is likely to resolve your heavy bleeding symptoms.
What to Do When Natural Menorrhagia Treatments Don’t Work
Medical treatment with a qualified doctor is necessary and important for some cases of menorrhagia, including cancers, blood clotting disorders, and sometimes for more advanced hormonally related conditions.
Standard menorrhagia treatment options include:
- Endometrial ablation (spot burning of problem areas) or curettage (a procedure to scrape away the uterine lining) for uterine abnormalities
- Hysterectomy (removal of the uterus) or uterine resection for fibroids, adenomyosis, or endometrial cancer
- Antifibrinolytic (blood clotting) medications like tranexamic acid to reduce blood flow and promote blood clotting 34
- NSAIDs (non-steroidal anti-inflammatory drugs) like Ibuprofen to reduce bleeding by inhibiting prostaglandins (hormone-like compounds) that affect uterine contractions and blood flow 34
- Birth control pills or hormonal IUDs (intrauterine devices) like the Mirena with progesterone (levonorgestrel or progestin).
The Bottom Line
If you struggle with heavy and excessive bleeding during your menstrual period, seek medical advice immediately to help you determine the causes.
If your menorrhagia is determined to be due to hormone imbalances, consider improving your gut health with a clean, anti-inflammatory diet and probiotics. In addition, consider using herbs to help balance your hormones.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Davies J, Kadir RA. Heavy menstrual bleeding: An update on management. Thromb Res. 2017 Mar;151 Suppl 1:S70-S77. doi: 10.1016/S0049-3848(17)30072-5. PMID: 28262240.
- Walker MH, Coffey W, Borger J. Menorrhagia. [Updated 2020 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536910/
- https://www.mayoclinic.org/diseases-conditions/menorrhagia/symptoms-causes/syc-20352829
- Javan R, Yousefi M, Nazari SM, Amiri P, Mosavi-Jarrahi A, Modiramani P, Naghedi-Baghdar H. Herbal Medicines in Idiopathic Heavy Menstrual Bleeding: A Systematic Review. Phytother Res. 2016 Oct;30(10):1584-1591. doi: 10.1002/ptr.5675. Epub 2016 Jul 10. PMID: 27397554.
- Vanuytsel T, van Wanrooy S, Vanheel H, Vanormelingen C, Verschueren S, Houben E, Salim Rasoel S, Tόth J, Holvoet L, Farré R, Van Oudenhove L, Boeckxstaens G, Verbeke K, Tack J. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut. 2014 Aug;63(8):1293-9. doi: 10.1136/gutjnl-2013-305690. Epub 2013 Oct 23. PMID: 24153250.
- Karl JP, Margolis LM, Madslien EH, Murphy NE, Castellani JW, Gundersen Y, Hoke AV, Levangie MW, Kumar R, Chakraborty N, Gautam A, Hammamieh R, Martini S, Montain SJ, Pasiakos SM. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am J Physiol Gastrointest Liver Physiol. 2017 Jun 1;312(6):G559-G571. doi: 10.1152/ajpgi.00066.2017. Epub 2017 Mar 23. PMID: 28336545.
- Delgado BJ, Lopez-Ojeda W. Estrogen. [Updated 2020 Aug 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538260/
- Cable JK, Grider MH. Physiology, Progesterone. [Updated 2020 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558960/
- Goedert JJ, Jones G, Hua X, Xu X, Yu G, Flores R, Falk RT, Gail MH, Shi J, Ravel J, Feigelson HS. Investigation of the association between the fecal microbiota and breast cancer in postmenopausal women: a population-based case-control pilot study. J Natl Cancer Inst. 2015 Jun 1;107(8):djv147. doi: 10.1093/jnci/djv147. PMID: 26032724; PMCID: PMC4554191.
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas. 2017 Sep;103:45-53. doi: 10.1016/j.maturitas.2017.06.025. Epub 2017 Jun 23. PMID: 28778332.
- Fuhrman BJ, Feigelson HS, Flores R, Gail MH, Xu X, Ravel J, Goedert JJ. Associations of the fecal microbiome with urinary estrogens and estrogen metabolites in postmenopausal women. J Clin Endocrinol Metab. 2014 Dec;99(12):4632-40. doi: 10.1210/jc.2014-2222. PMID: 25211668; PMCID: PMC4255131.
- Chen C, Song X, Wei W, Zhong H, Dai J, Lan Z, Li F, Yu X, Feng Q, Wang Z, Xie H, Chen X, Zeng C, Wen B, Zeng L, Du H, Tang H, Xu C, Xia Y, Xia H, Yang H, Wang J, Wang J, Madsen L, Brix S, Kristiansen K, Xu X, Li J, Wu R, Jia H. The microbiota continuum along the female reproductive tract and its relation to uterine-related diseases. Nat Commun. 2017 Oct 17;8(1):875. doi: 10.1038/s41467-017-00901-0. PMID: 29042534; PMCID: PMC5645390.
- Łaniewski P, Ilhan ZE, Herbst-Kralovetz MM. The microbiome and gynaecological cancer development, prevention and therapy. Nat Rev Urol. 2020 Apr;17(4):232-250. doi: 10.1038/s41585-020-0286-z. Epub 2020 Feb 18. PMID: 32071434.
- Vaghela N, Mishra D, Sheth M, Dani VB. To compare the effects of aerobic exercise and yoga on Premenstrual syndrome. J Educ Health Promot. 2019 Oct 24;8:199. doi: 10.4103/jehp.jehp_50_19. PMID: 31867375; PMCID: PMC6852652.
- Bajalan Z, Alimoradi Z, Moafi F. Nutrition as a Potential Factor of Primary Dysmenorrhea: A Systematic Review of Observational Studies. Gynecol Obstet Invest. 2019;84(3):209-224. doi: 10.1159/000495408. Epub 2019 Jan 10. PMID: 30630172.
- Wang F, Feng J, Chen P, Liu X, Ma M, Zhou R, Chang Y, Liu J, Li J, Zhao Q. Probiotics in Helicobacter pylori eradication therapy: Systematic review and network meta-analysis. Clin Res Hepatol Gastroenterol. 2017 Sep;41(4):466-475. doi: 10.1016/j.clinre.2017.04.004. Epub 2017 May 25. PMID: 28552432.
- García-Collinot G, Madrigal-Santillán EO, Martínez-Bencomo MA, Carranza-Muleiro RA, Jara LJ, Vera-Lastra O, Montes-Cortes DH, Medina G, Cruz-Domínguez MP. Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020 Apr;65(4):1134-1143. doi: 10.1007/s10620-019-05830-0. Epub 2019 Sep 23. PMID: 31549334.
- Greco A, Caviglia GP, Brignolo P, Ribaldone DG, Reggiani S, Sguazzini C, Smedile A, Pellicano R, Resegotti A, Astegiano M, Bresso F. Glucose breath test and Crohn’s disease: Diagnosis of small intestinal bacterial overgrowth and evaluation of therapeutic response. Scand J Gastroenterol. 2015;50(11):1376-81. doi: 10.3109/00365521.2015.1050691. Epub 2015 May 19. PMID: 25990116.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106-1113. doi: 10.2174/1389200219666180813144834. PMID: 30101706; PMCID: PMC6340155.
- Yuan F, Ni H, Asche CV, Kim M, Walayat S, Ren J. Efficacy of Bifidobacterium infantis 35624 in patients with irritable bowel syndrome: a meta-analysis. Curr Med Res Opin. 2017 Jul;33(7):1191-1197. doi: 10.1080/03007995.2017.1292230. Epub 2017 Mar 7. PMID: 28166427.
- Tiequn B, Guanqun C, Shuo Z. Therapeutic effects of Lactobacillus in treating irritable bowel syndrome: a meta-analysis. Intern Med. 2015;54(3):243-9. doi: 10.2169/internalmedicine.54.2710. PMID: 25748731.
- Mujagic Z, de Vos P, Boekschoten MV, Govers C, Pieters HH, de Wit NJ, Bron PA, Masclee AA, Troost FJ. The effects of Lactobacillus plantarum on small intestinal barrier function and mucosal gene transcription; a randomized double-blind placebo controlled trial. Sci Rep. 2017 Jan 3;7:40128. doi: 10.1038/srep40128. PMID: 28045137; PMCID: PMC5206730.
- Sindhu KN, Sowmyanarayanan TV, Paul A, Babji S, Ajjampur SS, Priyadarshini S, Sarkar R, Balasubramanian KA, Wanke CA, Ward HD, Kang G. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014 Apr;58(8):1107-15. doi: 10.1093/cid/ciu065. Epub 2014 Feb 5. PMID: 24501384; PMCID: PMC3967829.
- Lamprecht M, Bogner S, Schippinger G, Steinbauer K, Fankhauser F, Hallstroem S, Schuetz B, Greilberger JF. Probiotic supplementation affects markers of intestinal barrier, oxidation, and inflammation in trained men; a randomized, double-blinded, placebo-controlled trial. J Int Soc Sports Nutr. 2012 Sep 20;9(1):45. doi: 10.1186/1550-2783-9-45. PMID: 22992437; PMCID: PMC3465223.
- Shamasbi SG, Ghanbari-Homayi S, Mirghafourvand M. The effect of probiotics, prebiotics, and synbiotics on hormonal and inflammatory indices in women with polycystic ovary syndrome: a systematic review and meta-analysis. Eur J Nutr. 2020 Mar;59(2):433-450. doi: 10.1007/s00394-019-02033-1. Epub 2019 Jun 29. PMID: 31256251.
- Yavarikia P, Shahnazi M, Hadavand Mirzaie S, Javadzadeh Y, Lutfi R. Comparing the effect of mefenamic Acid and vitex agnus on intrauterine device induced bleeding. J Caring Sci. 2013 Aug 31;2(3):245-54. doi: 10.5681/jcs.2013.030. PMID: 25276733; PMCID: PMC4134154.
- Dietz BM, Hajirahimkhan A, Dunlap TL, Bolton JL. Botanicals and Their Bioactive Phytochemicals for Women’s Health. Pharmacol Rev. 2016 Oct;68(4):1026-1073. doi: 10.1124/pr.115.010843. PMID: 27677719; PMCID: PMC5050441.
- Ghazanfarpour M, Sadeghi R, Abdolahian S, Latifnejad Roudsari R. The efficacy of Iranian herbal medicines in alleviating hot flashes: A systematic review. Int J Reprod Biomed. 2016 Mar;14(3):155-66. PMID: 27294213; PMCID: PMC4899762.
- Kupfersztain C, Rotem C, Fagot R, Kaplan B. The immediate effect of natural plant extract, Angelica sinensis and Matricaria chamomilla (Climex) for the treatment of hot flushes during menopause. A preliminary report. Clin Exp Obstet Gynecol. 2003;30(4):203-6. PMID: 14664413.
- Jiang K, Jin Y, Huang L, Feng S, Hou X, Du B, Zheng J, Li L. Black cohosh improves objective sleep in postmenopausal women with sleep disturbance. Climacteric. 2015;18(4):559-67. doi: 10.3109/13697137.2015.1042450. Epub 2015 May 22. PMID: 26000551.
- Maleki-Saghooni N, Karimi FZ, Behboodi Moghadam Z, Mirzaii Najmabadi K. The effectiveness and safety of Iranian herbal medicines for treatment of premenstrual syndrome: A systematic review. Avicenna J Phytomed. 2018 Mar-Apr;8(2):96-113. PMID: 29632841; PMCID: PMC5885324.
- Verkaik S, Kamperman AM, van Westrhenen R, Schulte PFJ. The treatment of premenstrual syndrome with preparations of Vitex agnus castus: a systematic review and meta-analysis. Am J Obstet Gynecol. 2017 Aug;217(2):150-166. doi: 10.1016/j.ajog.2017.02.028. Epub 2017 Feb 22. PMID: 28237870.
- Cerqueira RO, Frey BN, Leclerc E, Brietzke E. Vitex agnus castus for premenstrual syndrome and premenstrual dysphoric disorder: a systematic review. Arch Womens Ment Health. 2017 Dec;20(6):713-719. doi: 10.1007/s00737-017-0791-0. Epub 2017 Oct 23. PMID: 29063202.
- Bradley LD, Gueye NA. The medical management of abnormal uterine bleeding in reproductive-aged women. Am J Obstet Gynecol. 2016 Jan;214(1):31-44. doi: 10.1016/j.ajog.2015.07.044. Epub 2015 Aug 5. PMID: 26254516.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!