Effective, Natural IBS Pain Management and Treatment Options
Research-Backed Ideas for Reducing IBS Pain
- IBS|
- IBS Pain|
- Cause of IBS Pain|
- Manage IBS Pain|
- Diet|
- Probiotics|
- Digestive Support|
- Fiber|
- Enzymes|
Abdominal pain is one of the defining (and least comfortable) symptoms of IBS. Most IBS patients report some form of abdominal pain, including bloating, distention, cramping, or stomach pain. Let’s explore what causes IBS pain and how you can manage and prevent it.

Irritable Bowel Syndrome (IBS)
On average, 10-15% of American adults have irritable bowel syndrome [1], making it one of the most common digestive system problems.
IBS is not a specific disease with a clear mechanism — it’s a group of digestive symptoms [2]. Recurrent abdominal pain and changes in bowel habits are the hallmark symptoms of IBS [3]. IBS-C patients tend to have constipation, while IBS patients with IBS-D more often have diarrhea.
IBS may co-occur with other digestive medical conditions, such as inflammatory bowel diseases [4] (including Crohn’s disease and ulcerative colitis), celiac disease [5], and SIBO [6, 7, 8]. A family history of IBD or colorectal cancer may also increase your risk of developing IBS [9]. IBS patients tend to go through periods of symptom flare-ups, followed by periods of relative calm.
Common Symptoms of IBS That Can Cause Pain
Abdominal pain, stomach pain, and bloating are obvious sources of IBS pain. Digestive IBS symptoms that may cause IBS pain include:
- Frequent bowel movements or diarrhea
- Constipation
- Cramping or a spastic colon
- Flatulence or gas
IBS can also cause non-digestive pain symptoms by affecting the central nervous system [10], or the immune system [11, 12]. Symptoms such as joint pain [13] and headaches [14, 15] are surprisingly common for IBS patients. Additionally, one interesting study suggested up to 49% of fibromyalgia patients also have IBS as well [16].
What Is the Cause of IBS Pain?
Because IBS is a syndrome made up of a collection of digestive system symptoms, there are many potential underlying causes of IBS pain for individual patients.
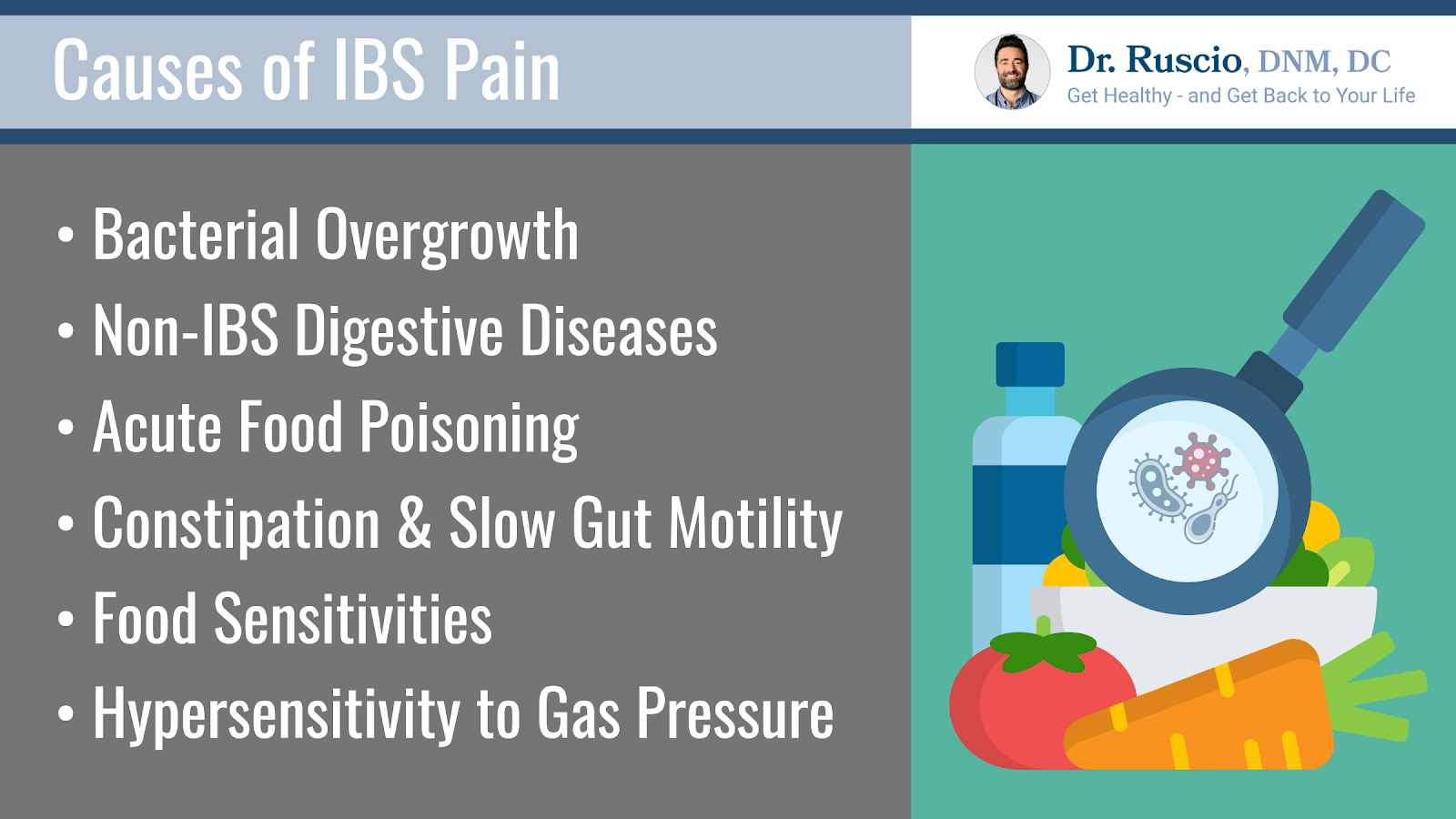
Bacterial Overgrowth
Several studies suggest a significant portion of IBS patients have small intestine bacterial overgrowth (SIBO) or other types of bacterial imbalance [17, 18, 19]. Bacterial overgrowth can irritate the lining of the small intestine or large intestine, causing IBS pain or a change in bowel habits. Excess bacteria can also overproduce gas that leads to bloating and distention.

Other Digestive Diseases
Many IBD [20] and celiac disease [21] patients also have IBS symptoms, including pain. This may be due to intestinal inflammation or irritation. Your doctor may try to rule out these other potential causes of pain before diagnosing you with IBS.
Acute Gastroenteritis
Acute gastroenteritis, also known as food poisoning, can also certainly cause stomach and intestinal pain. It’s estimated that between 5%-32% of IBS is caused by gastroenteritis [22]. A meta-analysis and systematic review found that gastroenteritis increased the risk of developing IBS four-fold compared to people who never had gastroenteritis [23].
Some preliminary animal model research indicates that gastroenteritis can cause increased anti-cytolethal distending toxin B (CdtB) and anti-vinculin antibodies in the small intestine [24]. This can lead to an autoimmune reaction in the small intestine, which can lead to chronic IBS symptoms [25].
A subsequent study compared levels of these antibodies in patients with IBS-D and controls. The study found that “Anti-CdtB titers were significantly higher in D-IBS subjects compared to IBD, healthy controls and celiac disease…Anti-vinculin titers were also significantly higher in IBS compared to the other groups.” In other words, food-poisoning-triggered antibodies may be a cause of some cases of IBS-D and chronic IBS pain.
Constipation and Gut Motility
Constipation is one of the hallmark symptoms of IBS. It may also be a cause of IBS [26]. Slow gut motility increases the likelihood of small intestinal bacterial overgrowth (SIBO) or other dysbiosis, which can lead to chronic IBS symptoms [27]. Gut motility can also be slowed down by medications like opioids [28], abdominal scar tissue or adhesions, or lack of physical activity [29].
Food Sensitivities or Intolerances
Food sensitivities may also aggravate or cause IBS symptoms, including pain [30]. Intolerance to particular groups of FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) can increase bloating and abdominal pain and distention when those foods are consumed [31]. Other potential food triggers of IBS pain include gluten [32], dairy products [33], high histamine foods [34], or artificial additives or ingredients [35].
Hypersensitivity to Gas Pressure
Many IBS patients report that no matter what they eat, they are extremely sensitive to bloating and gas pressure, even normal levels. Inflammation [36] or altered serotonin metabolism [37] may play a role in this hypersensitivity. Some preliminary research suggests that certain types of foods, such as fats [38], or high FODMAP foods [39] may influence digestive hormones and trigger hypersensitivity.
Regardless of the underlying causes of your IBS pain, general gut support resolves many cases of IBS pain. This can often easily be done by making proactive diet and lifestyle changes to identify and resolve the worst triggers of your IBS symptoms. Let’s discuss how to help you reduce your IBS pain.
How to Manage and Treat IBS Pain
A gastroenterologist might order blood tests or a colonoscopy to rule out other possible diagnoses. They may then prescribe laxatives, antispasmodic medications, or prescription medications like loperamide to manage and treat IBS pain.
However, many of these approaches have unwanted side effects and don’t get at the root cause of your IBS pain or symptoms. There are many proactive steps you can take in your day-to-day life to manage and treat your IBS and IBS pain.
Using Diet To Prevent IBS Pain
Eating an anti-inflammatory diet is the first step to addressing your IBS pain.
Particular food sensitivities or intolerances may very closely relate to your IBS symptoms like pain, or your foods may be encouraging bacterial overgrowth.
A simple 3-4 day gut reset with an elemental diet is an effective and easy way to start. An elemental diet reduces IBS pain and other symptoms by starving bacterial overgrowths, which reduces exposure to food irritants and allows your digestive system to rest temporarily. In one study, 86% of SIBO patients on a two-week elemental diet saw their breath tests normalize, and 65% of IBS patients saw an improvement in their IBS symptoms [40].
Once you’ve completed a gut reset, consider adopting a low FODMAP diet.
FODMAPs are Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, which are all simply natural, fermentable sugars and starches that occur in plant foods.
The low FODMAP diet is the most researched diet for IBS. It has been shown in two meta-analyses (the highest quality evidence) and several smaller studies to improve IBS symptoms like bloating and abdominal pain and to improve quality of life for IBS patients [41, 42, 43]. The low FODMAP diet has also been shown in research to improve the function of gut endocrine cells, which can normalize bowel habits [44, 45, 46].
The low FODMAP diet temporarily eliminates high FODMAP foods, such as foods high in lactose, like dairy products, and foods high in fructose, like mangoes, to reduce food with bad bacteria that may be overgrown in the intestines.
Once your inflammation has calmed down, you reintroduce foods to see which ones you truly need to keep avoiding. For help eating a low FODMAP diet, see our guide to the low FODMAP diet.

Probiotics To Reduce IBS Pain
Many cases of IBS are caused by dysbiosis, or an imbalance of your good and bad bacteria, and the inflammation this can trigger in your digestive system [47]. Probiotics have been shown in several meta-analyses and smaller studies to improve IBS symptoms, including bloating, abdominal pain, and gas [48, 49, 50, 51, 52, 53].
Probiotics have also been shown to improve outcomes of antibiotic or antimicrobial herb treatment for infections like H. pylori and SIBO [54, 55, 56].
Probiotics don’t work like medications to reduce IBS pain and symptoms. Instead, they work to generally reduce inflammation and help balance your gut microbiome and environment [57].
There are three main categories of probiotics. Using probiotics for IBS pain is as simple as using one probiotic from each of the three main categories together:
- A Lactobacillus-Bifidobacteria blend, containing mainly Lactobacillus and Bifidobacteria species.
- Saccharomyces boulardii, a beneficial yeast
- A soil-Based probiotic, usually containing Bacillus species
The three categories work together to restore balance in your gut environment.

Meta-analyses and systematic reviews suggest that a diversity of probiotic species improves IBS symptoms more than single strains or species [58, 59]. Many people try a single probiotic product and give up when they don’t see results. By using a diverse complement of probiotics, IBS patients often see a positive shift in their IBS symptoms. My clinical experience mirrors this research.
Other Digestive Support for IBS Pain
Consider trying these additional digestive supports if they are appropriate for you to help reduce your IBS pain.
Fiber Supplements
Research suggests fiber supplements are helpful for people with IBS-C [60]. A meta-analysis concluded that soluble fiber improved IBS symptoms, including IBS pain [61]. Several individual studies support this conclusion [62, 63]. However, fiber supplements may trigger an increase in bloating, gas, and abdominal pain for a significant portion of IBS patients [64], so they should be used with caution.
If you’re interested in trying fiber supplements, start low and slowly increase your intake. If you notice negative side effects, discontinue use immediately and try again when your gut has done some healing.
Digestive Enzymes
Some IBS patients get IBS pain flares because they have trouble digesting certain foods, such as FODMAPs or dietary fats. A meta-analysis showed that pancreatic enzyme replacement therapy improved IBS symptoms compared to a placebo [65]. One additional small study found that digestive enzymes improved symptoms for IBS and IBD patients [66]. Digestive enzymes are worth a trial for managing your IBS pain.
Lifestyle Changes for IBS Pain
Stress is a common trigger for IBS pain and other IBS symptoms [67]. Getting your stress under control can make a huge difference in your experience of IBS pain.
Research shows that treatment options like cognitive behavioral therapy [68, 69] and relaxation techniques such as hypnotherapy [70, 71] and meditation [72] can improve IBS pain from 20% to 65% percent. Regular exercise was also shown in one small study to improve bloating and IBS patient quality of life [73].
Say Goodbye to IBS Pain
Though pain is one of the more common IBS symptoms, you need not be a prisoner to your IBS pain. Diet and lifestyle changes such as eating a low FODMAP diet, including probiotics, fiber, and enzymes may improve symptoms, while relaxation techniques can help improve your gut-brain-stress related symptoms.
For more detail about how to properly use these options, see my book Healthy Gut, Healthy You.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- https://gi.org/topics/irritable-bowel-syndrome/
- Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015 Mar 3;313(9):949-58. doi: 10.1001/jama.2015.0954. PMID: 25734736.
- Lacy BE, Patel NK. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017 Oct 26;6(11):99. doi: 10.3390/jcm6110099. PMID: 29072609; PMCID: PMC5704116.
- Halpin SJ, Ford AC. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2012 Oct;107(10):1474-82. doi: 10.1038/ajg.2012.260. Epub 2012 Aug 28. PMID: 22929759.
- Sainsbury A, Sanders DS, Ford AC. Prevalence of irritable bowel syndrome-type symptoms in patients with celiac disease: a meta-analysis. Clin Gastroenterol Hepatol. 2013 Apr;11(4):359-65.e1. doi: 10.1016/j.cgh.2012.11.033. Epub 2012 Dec 13. PMID: 23246645.
- Schmulson M, Bielsa MV, Carmona-Sánchez R, Hernández A, López-Colombo A, López Vidal Y, Peláez-Luna M, Remes-Troche JM, Tamayo JL, Valdovinos MA. Microbiota, gastrointestinal infections, low-grade inflammation, and antibiotic therapy in irritable bowel syndrome: an evidence-based review. Rev Gastroenterol Mex. 2014 Apr-Jun;79(2):96-134. English, Spanish. doi: 10.1016/j.rgmx.2014.01.004. Epub 2014 May 23. PMID: 24857420.
- Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020 Jul 10;11:664. doi: 10.3389/fpsyt.2020.00664. PMID: 32754068; PMCID: PMC7366247.
- Saffouri GB, Shields-Cutler RR, Chen J, Yang Y, Lekatz HR, Hale VL, Cho JM, Battaglioli EJ, Bhattarai Y, Thompson KJ, Kalari KK, Behera G, Berry JC, Peters SA, Patel R, Schuetz AN, Faith JJ, Camilleri M, Sonnenburg JL, Farrugia G, Swann JR, Grover M, Knights D, Kashyap PC. Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders. Nat Commun. 2019 May 1;10(1):2012. doi: 10.1038/s41467-019-09964-7. PMID: 31043597; PMCID: PMC6494866.
- Lacy BE, Patel NK. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017 Oct 26;6(11):99. doi: 10.3390/jcm6110099. PMID: 29072609; PMCID: PMC5704116.
- Ohman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. 2010 Mar;7(3):163-73. doi: 10.1038/nrgastro.2010.4. Epub 2010 Jan 26. PMID: 20101257.
- Ohman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. 2010 Mar;7(3):163-73. doi: 10.1038/nrgastro.2010.4. Epub 2010 Jan 26. PMID: 20101257.
- Ford AC, Talley NJ. Mucosal inflammation as a potential etiological factor in irritable bowel syndrome: a systematic review. J Gastroenterol. 2011 Apr;46(4):421-31. doi: 10.1007/s00535-011-0379-9. Epub 2011 Feb 18. PMID: 21331765.
- Kamp KJ, Weaver KR, Sherwin LB, Barney P, Hwang SK, Yang PL, Burr RL, Cain KC, Heitkemper MM. Effects of a comprehensive self-management intervention on extraintestinal symptoms among patients with IBS. J Psychosom Res. 2019 Nov;126:109821. doi: 10.1016/j.jpsychores.2019.109821. Epub 2019 Aug 29. PMID: 31499231; PMCID: PMC6842704.
- Cámara-Lemarroy CR, Rodriguez-Gutierrez R, Monreal-Robles R, Marfil-Rivera A. Gastrointestinal disorders associated with migraine: A comprehensive review. World J Gastroenterol. 2016 Sep 28;22(36):8149-60. doi: 10.3748/wjg.v22.i36.8149. PMID: 27688656; PMCID: PMC5037083.
- Arzani M, Jahromi SR, Ghorbani Z, Vahabizad F, Martelletti P, Ghaemi A, Sacco S, Togha M; School of Advanced Studies of the European Headache Federation (EHF-SAS). Gut-brain Axis and migraine headache: a comprehensive review. J Headache Pain. 2020 Feb 13;21(1):15. doi: 10.1186/s10194-020-1078-9. PMID: 32054443; PMCID: PMC7020496.
- Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002 Apr;122(4):1140-56. doi: 10.1053/gast.2002.32392. PMID: 11910364.
- Chen B, Kim JJ, Zhang Y, Du L, Dai N. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis. J Gastroenterol. 2018 Jul;53(7):807-818. doi: 10.1007/s00535-018-1476-9. Epub 2018 May 14. PMID: 29761234.
- Schmulson M, Bielsa MV, Carmona-Sánchez R, Hernández A, López-Colombo A, López Vidal Y, Peláez-Luna M, Remes-Troche JM, Tamayo JL, Valdovinos MA. Microbiota, gastrointestinal infections, low-grade inflammation, and antibiotic therapy in irritable bowel syndrome: an evidence-based review. Rev Gastroenterol Mex. 2014 Apr-Jun;79(2):96-134. English, Spanish. doi: 10.1016/j.rgmx.2014.01.004. Epub 2014 May 23. PMID: 24857420.
- Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020 Jul 10;11:664. doi: 10.3389/fpsyt.2020.00664. PMID: 32754068; PMCID: PMC7366247.
- Halpin SJ, Ford AC. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2012 Oct;107(10):1474-82. doi: 10.1038/ajg.2012.260. Epub 2012 Aug 28. PMID: 22929759.
- Sainsbury A, Sanders DS, Ford AC. Prevalence of irritable bowel syndrome-type symptoms in patients with celiac disease: a meta-analysis. Clin Gastroenterol Hepatol. 2013 Apr;11(4):359-65.e1. doi: 10.1016/j.cgh.2012.11.033. Epub 2012 Dec 13. PMID: 23246645.
- Thabane M, Marshall JK. Post-infectious irritable bowel syndrome. World J Gastroenterol. 2009 Aug 7;15(29):3591-6. doi: 10.3748/wjg.15.3591. PMID: 19653335; PMCID: PMC2721231.
- Klem F, Wadhwa A, Prokop LJ, Sundt WJ, Farrugia G, Camilleri M, Singh S, Grover M. Prevalence, Risk Factors, and Outcomes of Irritable Bowel Syndrome After Infectious Enteritis: A Systematic Review and Meta-analysis. Gastroenterology. 2017 Apr;152(5):1042-1054.e1. doi: 10.1053/j.gastro.2016.12.039. Epub 2017 Jan 6. PMID: 28069350; PMCID: PMC5367939.
- Pimentel M, Morales W, Pokkunuri V, Brikos C, Kim SM, Kim SE, Triantafyllou K, Weitsman S, Marsh Z, Marsh E, Chua KS, Srinivasan S, Barlow GM, Chang C. Autoimmunity Links Vinculin to the Pathophysiology of Chronic Functional Bowel Changes Following Campylobacter jejuni Infection in a Rat Model. Dig Dis Sci. 2015 May;60(5):1195-205. doi: 10.1007/s10620-014-3435-5. Epub 2014 Nov 26. PMID: 25424202.
- Pimentel M, Morales W, Pokkunuri V, Brikos C, Kim SM, Kim SE, Triantafyllou K, Weitsman S, Marsh Z, Marsh E, Chua KS, Srinivasan S, Barlow GM, Chang C. Autoimmunity Links Vinculin to the Pathophysiology of Chronic Functional Bowel Changes Following Campylobacter jejuni Infection in a Rat Model. Dig Dis Sci. 2015 May;60(5):1195-205. doi: 10.1007/s10620-014-3435-5. Epub 2014 Nov 26. PMID: 25424202.
- Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015 Mar 3;313(9):949-58. doi: 10.1001/jama.2015.0954. PMID: 25734736.
- Pimentel M, Soffer EE, Chow EJ, Kong Y, Lin HC. Lower frequency of MMC is found in IBS subjects with abnormal lactulose breath test, suggesting bacterial overgrowth. Dig Dis Sci. 2002 Dec;47(12):2639-43. doi: 10.1023/a:1021039032413. PMID: 12498278.
- Prichard D, Norton C, Bharucha AE. Management of opioid-induced constipation. Br J Nurs. 2016 May 26-Jun 8;25(10):S4-5, S8-11. doi: 10.12968/bjon.2016.25.10.S4. PMID: 27231750.
- Gao R, Tao Y, Zhou C, Li J, Wang X, Chen L, Li F, Guo L. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scand J Gastroenterol. 2019 Feb;54(2):169-177. doi: 10.1080/00365521.2019.1568544. Epub 2019 Mar 7. PMID: 30843436.
- Cuomo R, Andreozzi P, Zito FP, Passananti V, De Carlo G, Sarnelli G. Irritable bowel syndrome and food interaction. World J Gastroenterol. 2014 Jul 21;20(27):8837-45. doi: 10.3748/wjg.v20.i27.8837. PMID: 25083057; PMCID: PMC4112903.
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2):252-8. doi: 10.1111/j.1440-1746.2009.06149.x. PMID: 20136989.
- Catassi C, Alaedini A, Bojarski C, Bonaz B, Bouma G, Carroccio A, Castillejo G, De Magistris L, Dieterich W, Di Liberto D, Elli L, Fasano A, Hadjivassiliou M, Kurien M, Lionetti E, Mulder CJ, Rostami K, Sapone A, Scherf K, Schuppan D, Trott N, Volta U, Zevallos V, Zopf Y, Sanders DS. The Overlapping Area of Non-Celiac Gluten Sensitivity (NCGS) and Wheat-Sensitive Irritable Bowel Syndrome (IBS): An Update. Nutrients. 2017 Nov 21;9(11):1268. doi: 10.3390/nu9111268. PMID: 29160841; PMCID: PMC5707740.
- Deng Y, Misselwitz B, Dai N, Fox M. Lactose Intolerance in Adults: Biological Mechanism and Dietary Management. Nutrients. 2015 Sep 18;7(9):8020-35. doi: 10.3390/nu7095380. PMID: 26393648; PMCID: PMC4586575.
- Schnedl WJ, Lackner S, Enko D, Schenk M, Holasek SJ, Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intest Res. 2019 Jul;17(3):427-433. doi: 10.5217/ir.2018.00152. Epub 2019 Mar 7. PMID: 30836736; PMCID: PMC6667364.
- Schnabel L, Buscail C, Sabate JM, Bouchoucha M, Kesse-Guyot E, Allès B, Touvier M, Monteiro CA, Hercberg S, Benamouzig R, Julia C. Association Between Ultra-Processed Food Consumption and Functional Gastrointestinal Disorders: Results From the French NutriNet-Santé Cohort. Am J Gastroenterol. 2018 Aug;113(8):1217-1228. doi: 10.1038/s41395-018-0137-1. Epub 2018 Jun 15. PMID: 29904158.
- Liu L, Liu BN, Chen S, Wang M, Liu Y, Zhang YL, Yao SK. Visceral and somatic hypersensitivity, autonomic cardiovascular dysfunction and low-grade inflammation in a subset of irritable bowel syndrome patients. J Zhejiang Univ Sci B. 2014 Oct;15(10):907-14. doi: 10.1631/jzus.B1400143. PMID: 25294380; PMCID: PMC4201319.
- Keszthelyi D, Troost FJ, Jonkers DM, van Eijk HM, Dekker J, Buurman WA, Masclee AA. Visceral hypersensitivity in irritable bowel syndrome: evidence for involvement of serotonin metabolism–a preliminary study. Neurogastroenterol Motil. 2015 Aug;27(8):1127-37. doi: 10.1111/nmo.12600. Epub 2015 May 31. PMID: 26031193.
- Simrén M, Abrahamsson H, Björnsson ES. An exaggerated sensory component of the gastrocolonic response in patients with irritable bowel syndrome. Gut. 2001 Jan;48(1):20-7. doi: 10.1136/gut.48.1.20. PMID: 11115818; PMCID: PMC1728182.
- Mazzawi T, El-Salhy M. Effect of diet and individual dietary guidance on gastrointestinal endocrine cells in patients with irritable bowel syndrome (Review). Int J Mol Med. 2017 Oct;40(4):943-952. doi: 10.3892/ijmm.2017.3096. Epub 2017 Aug 11. PMID: 28849091; PMCID: PMC5593462.
- Pimentel M, Constantino T, Kong Y, Bajwa M, Rezaei A, Park S. A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Dig Dis Sci. 2004 Jan;49(1):73-7. doi: 10.1023/b:ddas.0000011605.43979.e1. PMID: 14992438.
- Lacy BE, Patel NK. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017 Oct 26;6(11):99. doi: 10.3390/jcm6110099. PMID: 29072609; PMCID: PMC5704116.
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2):252-8. doi: 10.1111/j.1440-1746.2009.06149.x. PMID: 20136989.
- Gibson PR, Shepherd SJ. Food choice as a key management strategy for functional gastrointestinal symptoms. Am J Gastroenterol. 2012 May;107(5):657-66; quiz 667. doi: 10.1038/ajg.2012.49. Epub 2012 Apr 10. PMID: 22488077.
- Mazzawi T, El-Salhy M. Changes in duodenal enteroendocrine cells in patients with irritable bowel syndrome following dietary guidance. Exp Biol Med (Maywood). 2017 Jul;242(13):1355-1362. doi: 10.1177/1535370217699537. Epub 2017 Mar 17. PMID: 28737477; PMCID: PMC5528200.
- Mazzawi T, Hausken T, Gundersen D, El-Salhy M. Dietary guidance normalizes large intestinal endocrine cell densities in patients with irritable bowel syndrome. Eur J Clin Nutr. 2016 Feb;70(2):175-81. doi: 10.1038/ejcn.2015.191. Epub 2015 Nov 25. PMID: 26603880; PMCID: PMC4744244.
- Mazzawi T, El-Salhy M. Effect of diet and individual dietary guidance on gastrointestinal endocrine cells in patients with irritable bowel syndrome (Review). Int J Mol Med. 2017 Oct;40(4):943-952. doi: 10.3892/ijmm.2017.3096. Epub 2017 Aug 11. PMID: 28849091; PMCID: PMC5593462.
- Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015 Mar 3;313(9):949-58. doi: 10.1001/jama.2015.0954. PMID: 25734736.
- McFarland LV, Dublin S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J Gastroenterol. 2008 May 7;14(17):2650-61. doi: 10.3748/wjg.14.2650. PMID: 18461650; PMCID: PMC2709042.
- Martoni CJ, Srivastava S, Leyer GJ. Lactobacillus acidophilus DDS-1 and Bifidobacterium lactis UABla-12 Improve Abdominal Pain Severity and Symptomology in Irritable Bowel Syndrome: Randomized Controlled Trial. Nutrients. 2020 Jan 30;12(2):363. doi: 10.3390/nu12020363. PMID: 32019158; PMCID: PMC7071206.
- Whelan K. Probiotics and prebiotics in the management of irritable bowel syndrome: a review of recent clinical trials and systematic reviews. Curr Opin Clin Nutr Metab Care. 2011 Nov;14(6):581-7. doi: 10.1097/MCO.0b013e32834b8082. PMID: 21892075.
- Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014 Oct;109(10):1547-61; quiz 1546, 1562. doi: 10.1038/ajg.2014.202. Epub 2014 Jul 29. PMID: 25070051.
- Rogha M, Esfahani MZ, Zargarzadeh AH. The efficacy of a synbiotic containing Bacillus Coagulans in treatment of irritable bowel syndrome: a randomized placebo-controlled trial. Gastroenterol Hepatol Bed Bench. 2014 Summer;7(3):156-63. PMID: 25120896; PMCID: PMC4129566.
- Khalighi AR, Khalighi MR, Behdani R, Jamali J, Khosravi A, Kouhestani Sh, Radmanesh H, Esmaeelzadeh S, Khalighi N. Evaluating the efficacy of probiotic on treatment in patients with small intestinal bacterial overgrowth (SIBO)–a pilot study. Indian J Med Res. 2014 Nov;140(5):604-8. PMID: 25579140; PMCID: PMC4311312.
- Wang F, Feng J, Chen P, Liu X, Ma M, Zhou R, Chang Y, Liu J, Li J, Zhao Q. Probiotics in Helicobacter pylori eradication therapy: Systematic review and network meta-analysis. Clin Res Hepatol Gastroenterol. 2017 Sep;41(4):466-475. doi: 10.1016/j.clinre.2017.04.004. Epub 2017 May 25. PMID: 28552432.
- García-Collinot G, Madrigal-Santillán EO, Martínez-Bencomo MA, Carranza-Muleiro RA, Jara LJ, Vera-Lastra O, Montes-Cortes DH, Medina G, Cruz-Domínguez MP. Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020 Apr;65(4):1134-1143. doi: 10.1007/s10620-019-05830-0. Epub 2019 Sep 23. PMID: 31549334.
- Greco A, Caviglia GP, Brignolo P, Ribaldone DG, Reggiani S, Sguazzini C, Smedile A, Pellicano R, Resegotti A, Astegiano M, Bresso F. Glucose breath test and Crohn’s disease: Diagnosis of small intestinal bacterial overgrowth and evaluation of therapeutic response. Scand J Gastroenterol. 2015;50(11):1376-81. doi: 10.3109/00365521.2015.1050691. Epub 2015 May 19. PMID: 25990116.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106-1113. doi: 10.2174/1389200219666180813144834. PMID: 30101706; PMCID: PMC6340155.
- American College of Gastroenterology Task Force on Irritable Bowel Syndrome, Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2009 Jan;104 Suppl 1:S1-35. doi: 10.1038/ajg.2008.122. PMID: 19521341.
- Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014 Oct;109(10):1547-61; quiz 1546, 1562. doi: 10.1038/ajg.2014.202. Epub 2014 Jul 29. PMID: 25070051.
- El-Salhy M, Ystad SO, Mazzawi T, Gundersen D. Dietary fiber in irritable bowel syndrome (Review). Int J Mol Med. 2017 Sep;40(3):607-613. doi: 10.3892/ijmm.2017.3072. Epub 2017 Jul 19. PMID: 28731144; PMCID: PMC5548066.
- Moayyedi P, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Ford AC. The effect of fiber supplementation on irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2014 Sep;109(9):1367-74. doi: 10.1038/ajg.2014.195. Epub 2014 Jul 29. PMID: 25070054.
- Furnari M, de Bortoli N, Martinucci I, Bodini G, Revelli M, Marabotto E, Moscatelli A, Del Nero L, Savarino E, Giannini EG, Savarino V. Optimal management of constipation associated with irritable bowel syndrome. Ther Clin Risk Manag. 2015 May 30;11:691-703. doi: 10.2147/TCRM.S54298. PMID: 26028974; PMCID: PMC4425337.
- Bellini M, Gambaccini D, Salvadori S, Tosetti C, Urbano MT, Costa F, Monicelli P, Mumolo MG, Ricchiuti A, De Bortoli N, Marchi S. Management of chronic constipation in general practice. Tech Coloproctol. 2014 Jun;18(6):543-9. doi: 10.1007/s10151-013-1093-9. Epub 2013 Nov 22. PMID: 24272606.
- El-Salhy M, Ystad SO, Mazzawi T, Gundersen D. Dietary fiber in irritable bowel syndrome (Review). Int J Mol Med. 2017 Sep;40(3):607-613. doi: 10.3892/ijmm.2017.3072. Epub 2017 Jul 19. PMID: 28731144; PMCID: PMC5548066.
- Alkaade S, Vareedayah AA. A primer on exocrine pancreatic insufficiency, fat malabsorption, and fatty acid abnormalities. Am J Manag Care. 2017 Jul;23(12 Suppl):S203-S209. PMID: 28727474.
- Spagnuolo R, Cosco C, Mancina RM, Ruggiero G, Garieri P, Cosco V, Doldo P. Beta-glucan, inositol and digestive enzymes improve quality of life of patients with inflammatory bowel disease and irritable bowel syndrome. Eur Rev Med Pharmacol Sci. 2017 Jun;21(2 Suppl):102-107. PMID: 28724171.
- Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014 Oct 21;20(39):14126-31. doi: 10.3748/wjg.v20.i39.14126. PMID: 25339801; PMCID: PMC4202343.
- Zhao SR, Ni XM, Zhang XA, Tian H. Effect of cognitive behavior therapy combined with exercise intervention on the cognitive bias and coping styles of diarrhea-predominant irritable bowel syndrome patients. World J Clin Cases. 2019 Nov 6;7(21):3446-3462. doi: 10.12998/wjcc.v7.i21.3446. PMID: 31750328; PMCID: PMC6854400.
- Lackner JM, Jaccard J, Keefer L, Brenner DM, Firth RS, Gudleski GD, Hamilton FA, Katz LA, Krasner SS, Ma CX, Radziwon CD, Sitrin MD. Improvement in Gastrointestinal Symptoms After Cognitive Behavior Therapy for Refractory Irritable Bowel Syndrome. Gastroenterology. 2018 Jul;155(1):47-57. doi: 10.1053/j.gastro.2018.03.063. Epub 2018 Apr 25. Erratum in: Gastroenterology. 2018 Oct;155(4):1281. PMID: 29702118; PMCID: PMC6035059.
- Peters SL, Muir JG, Gibson PR. Review article: gut-directed hypnotherapy in the management of irritable bowel syndrome and inflammatory bowel disease. Aliment Pharmacol Ther. 2015 Jun;41(11):1104-15. doi: 10.1111/apt.13202. Epub 2015 Apr 10. PMID: 25858661.
- Miller V, Carruthers HR, Morris J, Hasan SS, Archbold S, Whorwell PJ. Hypnotherapy for irritable bowel syndrome: an audit of one thousand adult patients. Aliment Pharmacol Ther. 2015 May;41(9):844-55. doi: 10.1111/apt.13145. Epub 2015 Mar 4. PMID: 25736234.
- Shah K, Ramos-Garcia M, Bhavsar J, Lehrer P. Mind-body treatments of irritable bowel syndrome symptoms: An updated meta-analysis. Behav Res Ther. 2020 May;128:103462. doi: 10.1016/j.brat.2019.103462. Epub 2019 Nov 12. PMID: 32229334.
- Zhou C, Zhao E, Li Y, Jia Y, Li F. Exercise therapy of patients with irritable bowel syndrome: A systematic review of randomized controlled trials. Neurogastroenterol Motil. 2019 Feb;31(2):e13461. doi: 10.1111/nmo.13461. Epub 2018 Sep 19. PMID: 30232834.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!