How to Relieve Bloating: An Expert Shares Surprising Facts
Overcoming bloating & distention with clinician & researcher Dr. Peter Whorwell.
Bloating may be largely ignored by most doctors, but this uncomfortable symptom is common and deserves more attention. Dr. Peter Whorwell, a specialist clinician and researcher, shares his insights into bloating and reveals some surprising facts. Why do only half of the patients with bloating pain show signs of abdominal swelling? What is a bloatometer? How is bloating with constipation different from bloating with diarrhea? When is bloating a sign of a more serious disease? What are the most current treatments? Join us for a detailed look at this important topic.
What is bloating?
- Bloating is the term that patients often use to describe a feeling of fullness or gas
- 50% of patients who experience bloating also have distension
- Men do not distend as much as women
Visceral hypersensitivity
- When a patient is hyper sensitive to a normal amount of gas pressure even if they don’t look very bloated, they feel a lot of discomfort
- Inflammation can lead to hypersensitivity
- Laxatives and antibiotics can make someone sensitive
Distenders tend to be constipated and not hypersensitive
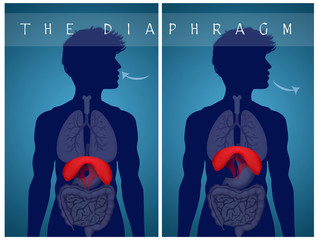
- Accommodation reflex – when the diaphragm goes up, so the belly doesn’t get bigger
- Distenders tend to experience the diaphragm going down
- Distension is also caused by stool backing up in the intestines
- Diaphragmatic biofeedback or hypnosis can be useful
- 80% response rate (50% improvement)
- 12 sessions – once per week – can be done via Skype
- Study: A randomised controlled trial on hypnotherapy for irritable bowel syndrome: design and methodological challenges
- 80% response rate (50% improvement)
Diet & treatment for distended-constipated patients
- 1st use laxatives – Miralax, Bisacodyl AND Hypnosis
- Miralax risks are low/none according to Whorwell
- Hypnosis – helps bloating, but is better for bloating but non-constipated types
- 2nd remove all fiber and potentially increase laxative support
- Low FODMAP or no fiber diet
- Elemental diet – can also be helpful for all types
Diet & treatment for bloated but non-distenders & non-constipated patients (aka Diarrhea)
- 1st Low FODMAP Diet & Hypnosis
- 2nd consider low-dose tricyclic antidepressant (only as needed)
- Continual dosing of Imodium could make bloating worse
Foods to avoid
- FODMAPS, Fiber
- Fat can be problematic for some
- Gluten can also be problematic
Probiotics
- A trial of probiotics can help
- If probiotics are causing symptoms after about a 2 week trial, discontinue
Red Flag Bloating/Distension
- If bloating is not worse as the day goes on, or does not vary, see your doctor – this could indicate a more serious condition
Where to learn more?
- Book: Take Control Of Your IBS
- Find Dr. Peter Whorwell on Pubmed.
In This Episode
Episode Intro …00:00:40
Bloating and Distension … 00:02:55
Diets to Relieve Bloating and IBS … 00:11:15
Biofeedback and Hypnosis … 00:15:28
Low FODMAP Diet … 00:26:00
Laxatives for Constipation … 00:29:23
Elemental Diet … 00:35:02
Treating Bloating and Diarrhoea … 00:41:25
Additional Dietary Advice … 00:46:56
SIBO and Bloating … 00:50:14
The Case for Probiotics in IBS … 00:55:46
Immune Activation in the Gut … 01:01:01
See Your Doctor Right Away if … 01:09:25
Episode Wrap Up … 01:11:13

Download this Episode (right click link and ‘Save As’)
Episode Intro
Dr. Michael Ruscio, DC: Hey everyone, welcome to Dr. Ruscio Radio. This is Dr. Ruscio. Today I’m here with Dr. Peter Whorwell, who is a specialist clinician/researcher in bloating. I’m very interested to have this conversation to dig into his brain a little bit about what bloating is all about, what’s new and exciting and what are some of the best tests and treatments.
Peter, thanks and welcome to the show.
Dr. Peter Whorwell, MD PhD: Pleasure.
DrMR: Can you tell people a little bit about your background?
DrPW: Yes. I’m a gastroenterologist who works in Manchester, in the U.K. and I’ve been doing this for quite a long time now. I specialize now entirely in irritable bowel and related conditions, the so-called functional gastrointestinal disorders. I still see 600 new patients a year. They’re all what are called tertiary care patients. They’re the ones who have seen a primary-care doctor, seen a secondary-care hospital doctor and are still in trouble. So, I see that sort of tip-of-the-iceberg patient.
DrMR: Is bloating something that you have a particular interest in? You came referred through a friend of mine, Dr. Allison Siebecker, as the guy to talk to for an expanded narrative on bloating. How does the bloating piece fit in here?
DrPW: Well, irritable bowel is my main interest. One of the symptoms of irritable bowel is bloating. When I first started on this many, many years ago, I used to think that bloating doesn’t sound like too much of a big deal. I’m sure patients are more worried about their pain and they’re worried about their bowel dysfunction. But actually, a lot of patients find the bloating as intrusive as the other symptoms.
Gradually, I got more and more interested in this problem. It is a very complex problem. We don’t quite understand it and it’s very intrusive. The women with bloating will complain bitterly about it.
Bloating and Distension: An Important Distinction
DRPW: As people interested in this, we see bloating as a thing the patient complains of. But, as doctors, it’s a little bit more confusing than that. Because there’s bloating, which is the feeling of pressure inside your tummy, and then there is where you can actually see the bloating, in medical parlance we call that distension.
So, there’s bloating, and distension, although a patient never comes in complaining of distension. They complain of bloating. That’s the word the patients use. As doctors we see it as two components. That feeling that your tummy’s swollen, and it isn’t necessarily. In about half those patients it’s actually swollen. Some people can look pregnant, you know, full-term pregnancy.
DrMR: I’m glad that you made that delineation because that’s one of the first questions I wanted to ask you. That’s something I struggle with as a clinician. When someone says, “I’m bloated,” do they mean they feel bloated? That gas pressure type of feeling. Or is it that they appear, visually to be distended? Is there a technical definition here that clinicians should be trying to identify one versus the other? Does it not really matter? How do you parse this on the clinical side of things?
DrPW: I think so few people are interested in irritable bowel and even less are interested in bloating, that clinicians just talk about bloating in a very glib way. There’s only us purists who go into this distention thing. Because we’re so interested in it, we developed a bloatometer, which is a belt which you can wear for 24 hours, and it records your girth.
With this bloatometer, we then realized that all the patients, everybody with bloating has complaints of that feeling. But, if you put the bloatometer on them, only half of them, 50%, will actually distend. We’ve got a problem here. Why do half of them distend, and the other half just feel bloated? I can go into that, if you want, it’s a little bit complicated, but that’s the problem that half of them distend. With the bloatometer, some of them can distend up to 20 centimeters. Quite often they have to change their clothing by the end of the day. The women will say, “It’s easier for me just to put on a dressing gown, or pajamas, because I’m so swollen.” A lot of the youngsters, you know, the early 20s get fed up with being asked, “Are you pregnant?”
DrMR: Yeah. I’ve had some patients who have made that same remark and they’ve sent in photos. Certainly, I’m sure that this is not pleasant, whether or not you’re actually distended. Even the feeling of distension is a very unpleasant sensation. Do you feel there is a difference in the underlying mechanism of those who are distended versus those who aren’t distended?

Pardon my rambling here, but there’s quite a few things that I’m trying to organize for the audience, as we weigh into this. One would be: Are there different mechanisms at play when someone is feeling bloated versus being actually distended? I wonder, as one component here to put on the table as we launch in… I know that hypersensitivity to gas pressure has been shown to be one of the mechanisms for why people feel bloated. So, it would seem plausible that some of the people that feel bloated but are not bloated, they are hypersensitive to normal gas pressure. So perhaps there’s not enough gas pressure to actually distend them. But, because they are hypersensitive, they feel bloated. How do you start trying to organize some of this in your mind?
DrPW: You’re right, actually. With the bloatometer, obviously, we can try and sort this out. As you well know, nothing in human physiology is perfect, so there’s never a binary difference between the two. With the bloatometer we have shown precisely what you’ve said. The ones that feel distended, or feel a pressure are…
I should just mention, in case I forget to say it again, the men don’t distend as much as women. That’s quite interesting, because women’s tummies are designed to accommodate pregnancy, whereas men’s aren’t. We can come back to that.
With the bloatometer, we’ve shown that the ones who don’t distend are hypersensitive. As you may know, the best way to test for this is to put a balloon up somebody’s tail-end and blow it up. Normal people feel pain as you blow up the balloon at a certain pressure. People with IBS feel pain at a much lower pressure. That’s called hypersensitivity, visceral hypersensitivity. Visceral meaning internal.
If you do this with the bloatometer patients, pick out the ones who are not actually distending and put a balloon up their tail-end and blow it up, they will be much more sensitive. Whereas the distenders tend to not be viscerally sensitive so much and tend to be constipated. There are two features: The distenders tend to be more constipated and not quite so sensitive. The bloaters without distension tend to have a loose bowel and be viscerally hypersensitive. Hypersensitive to the gut, for want of a better word.
Just recently, we published a paper showing that if you distend the bladder by making people drink a lot of water and hang onto it, that makes them distend. Suggesting that this initiates some sort of reflex, which I can talk about, if you wish a little later.
DrMR: Do you feel there to be a reason why some people are hypersensitive? Some of what I’ve read suggests that if there’s inflammation, that can lead to visceral hypersensitivity. Then, of course, inflammation has a litany of potential causes. Are you looking at or are you finding that there are a few keystone causes that underlie the hypersensitivity?
DrPW: Yeah. I think most people, as you’ve just said, it can follow inflammation. If people have gastroenteritis, they can be viscerally sensitive. We’ve shown that if you give people a laxative, it can make them sensitive. Antibiotics, if you get antibiotic diarrhea, you can become sensitive afterwards. Certain drugs, like the anti-inflammatory group of drugs… In other words, anything that can inflame the gut, can then make it sensitive. Even people with colitis and Crohn’s disease, when they’re in remission, because they’ve had an inflammation, can get this visceral hypersensitivity.
We showed many, many years ago that colitis in remission have a high prevalence of IBS and the bloating that goes with the IBS. Yes, you’re right. Any inflammatory process can make the gut more sensitive.
DrMR: Gotcha. For the audience, at least in my mind, that’s kind of good news. Because we know that there are a number of things that can be anti-inflammatory. Things like certain dietary changes, avoiding certain foods that can be noxious, potentially probiotics, as just a couple. Would you agree with that? Modify that?
Diets to Relieve Bloating and IBS
DrPW: Yeah. You’re right. Whenever we do anything with IBS and bloating in all these patients, we always start off with diet. We have this strange problem that an unhealthy diet is more suitable than a healthy diet. I don’t know what it’s like in the USA, but we’re all told to eat five a day, lots of broccoli and cabbage and things. Actually, if you’re a bloater, especially if you’re a loose bowel bloater, you can almost guarantee you’ll help them by cutting back on all that fiber. Because it’s all fermented inside you and makes a lot of gas and, if you’re sensitive, you don’t cope with the gas so well.
I should possibly point out that there isn’t excessive gas. People think I must have a massive gas inside me with all this distension. It isn’t excessive gas, it’s hypersensitivity to normal amounts of gas, as you said a while back.
DrMR: Yeah, I think that’s an important point. One of the things that may underline why the low FODMAP diet is helpful… I should definitely say that you’re preaching to the choir here. One of the things that I’ve been saying for years now, is that even though high prebiotic, high FODMAP foods, like broccoli and asparagus are stereotyped as being healthy and they feed gut bacteria; that doesn’t mean that they’re going to be helpful for every population. And the population that they pose the highest potential for detriment to are your IBS and IBD patient groups.

There may be some nuance there, when we look at IBS constipation versus IBS diarrhea, but we at least can somewhat confidently establish the premise that the “healthy” foods may not be great for people with this visceral hypersensitivity. This may be one of the reasons why the low FODMAP diet is helpful. Even though people don’t see a drop to abnormally-low amounts of gas, that subtle variation on gas pressure may be enough to alleviate the gas pressure that is enough to tip a hypersensitive person into reaction.
DrPW: That’s right. It’s bizarre because we tell patients routinely to eat an unhealthy diet for a while and see how they go. Then they get an improvement. They often say, “I didn’t believe you, but I thought I better do it.” Then they say, because we’re so bombarded with this healthy eating stuff at the moment… They then say, “can I now go back on my healthy eating?” Of course, as soon as they do that, they start getting problems again.
DrMR: Mm-hmm (affirmative). I think that’s one of the most demoralizing observations for someone who is taking steps to improve their health. Let’s say they are going on a raw vegetarian diet, or a paleo diet that’s going to be higher in fruits and vegetables. Then, they say, “Ugh, I’m feeling worse! I went to the supermarket and I bought all this food and I checked off my dietary list and really made an effort. Now, I’m feeling worse.” Which is why, I think, we should all be open-minded to the fact that no one diet is going to be best for everyone.
This was such a clear illustration of that concept for me. As someone who was very in favor of the paleo diet early on in my career, there were some people who clearly we had to make modifications for, because they had a tough time with these foods.
That leads me to a follow-up from this discussion of this point, which is: Is there any reason why the distenders tend to be constipated? Obviously the stool could be building up and that increases mass in the gut. Is there anything else there that you’ve been able to uncover?
Biofeedback and Hypnosis for Bloating and IBS
DrPW: This is complicated, I’ll try to explain it briefly and as simply as I can. If you think when you’re swallowing a meal, you’re swallowing quite a big volume of food and liquid. That goes into your tummy and the average person, like me, you don’t change shape. What’s happened, why haven’t you changed shape? Why hasn’t your tummy started bulging? That’s called the accommodation reflex. The accommodation reflex means that when you swallow this volume, the diaphragm goes up. So, because the diaphragm goes up, your belly doesn’t get bigger.
For some reason, in patients with IBS and distention, their diaphragm goes down when they eat a meal. Therefore, the only other bit that can give… Your pelvis can’t give, your back can’t give, and your diaphragm has gone down. So your tummy relaxes a bit and expands. That’s called the accommodation reflex. If you think about it, if you are constipated, your colon is going to get distended with stool or feces.
So, that sends messages to your brain saying that I’m expanding, so it kicks in the accommodation reflex. That’s what led us to the hypothesis… I wonder if a bladder, as it gets bigger, will do the same? That’s why we did that experiment. It seems that anything that’s getting bigger inside your abdomen is going to kick off your accommodation reflex. In a normal person, the diaphragm just relaxes and goes up a bit and you don’t change shape. But, in these people, you get this accommodation reflex being reversed.
There is another condition called anismus, which is called obstructive defecation, where when you open your bowels your bottom relaxes, for want of a better word. In these people the reflex is reversed and your bottom contracts. There is a precedent for these reversed reflexes. That’s what happens in these distenders.
DrMR: Now, we’ve had a discussion previously on the show with Satish Rao who has pioneered some work in biofeedback therapy. I believe what he’s describing is the same thing here, which is the analogy for passing stool of getting toothpaste out of a toothpaste tube. You take off the cap, that’s relaxation of the anal sphincter, and you squeeze the tube, that’s contraction of the stomach musculature. In people with this dyssynergic constipation, the cap stays on and you don’t squeeze the tube. The reflex is, kind of, inverted.
Are you finding that biofeedback therapy is something that can help to retrain the musculature to resurrect this aberrant accommodation response?
DrPW: Yeah, we don’t do it. We use hypnosis. But a chap called Fernando Azpiroz in Spain, in Barcelona, who we’ve worked closely with over the years; he does diaphragmatic biofeedback. It’s a bit complicated because you have to put a tube down the esophagus, the gullet, to the level of the diaphragm and record the activity of the diaphragm. Then teach the patients to relax their diaphragm. He gets very good results. Yes, that’s one way of tackling it.
DrMR: This is different than the biofeedback that’s used for dyssynergic constipation, is that correct? It sounds correct.
DrPW: They’re the same principle. As you know, biofeedback is just giving you a signal. Either a tone, or some other visual signal to try and teach you to do something with an organ. It’s exactly the same. Fernando puts this probe into the esophagus, at the level of the diaphragm, and teaches them to relax it that way. The principle is identical to…
DrMR: Right. Principle identical, but some of the finer points of the application… As I understand the Rao protocol, I believe you sit on the toilet and there’s certain biofeedback. Perhaps he is using some sort of diaphragmatic signaling device. He didn’t mention that in our conversation, but perhaps he omitted that detail. Your point is taken, which is that the underlying principle is the same. Perhaps, some of the nuances are a little different.
DrPW: Just in case I forget about it, some people’s diaphragm must go up so much that breathlessness is sometimes quite a problem featured in some of these really big distended patients. Presumably, their diaphragm has gone up so much that, it’s sort of so splinted, I should say, rather than gone up. It’s splinted, they actually feel breathless. Probably, as you know the majority of us breathe diaphragmatically at rest, we don’t breathe with our ribs and intercostal muscles. If that diaphragm’s activity is being interfered with, then you can actually feel breathless.
DrMR: Mm-hmm (affirmative). I’m assuming you probably see a higher predilection of upper back and neck tightness and trigger points.
DrPW: Yeah.
DrMR: The hypnosis… let’s try to look at this through the consumer lens. It sounds like a much more attractive proposition than having some sensor hooked up to your diaphragm. I’m not sure how invasive that is, but just at first shake here, my inclination would be to steer towards hypnosis. In brief, what does that therapy look like? Is it one session a week? How many weeks? How long until you start seeing some effect?
DrPW: We’ve been doing that. Well, I started it 30 years ago. Now I have people doing it for me. At the moment, we do 12 sessions once a week. In the IBS population, we get, I’ll have to be a little bit careful… We get an 80% response rate. Now, response rate is not cure. We get a responder, is simply get a 50% improvement in their symptoms, or more. Fifty percent or more. It’s worthwhile to get 50% improvement when you haven’t responded to anything else.
If they are particularly bloated or distended, then we give them visualization about the diaphragm and relaxing the diaphragm. Teaching it to, sort of, behave normally. I’ve been doing hypnosis for over 30 years, I still don’t quite understand how it works. We’ve just published a big review which is open access, actually. It came out two days ago, on Friday. A complete review of hypnosis for IBS and related conditions. It contains one of our little scripts for people who want to understand more about it. We’ve never published scripts before. We’ve published just a short script.
DrMR: When you say script, do you mean the protocol for exactly how you administer it?
DrPW: We published our protocol as an additive to the paper. Yeah.
Just also published, at almost the same time. We’re now do Skyping with that as well.
DrMR: That was a question I just wanted to ask you. Let’s say there’s someone listening to this, who’s not in your area. Do they have to see a hypnotherapist in person? Is some of this able to be done over the phone or via tape or some sort of multimedia platform? Tell us about that.
DrPW: We see people from all over the U.K. and Ireland and, occasionally, Europe. Obviously that’s a pain if they’re coming in for hypnotherapy, to see me for hypnotherapy, 12 sessions. We started doing Skype hypnotherapy and we get nearly as good results. It’s not quite as good, but we still get… I’ve forgotten what it is now. It’s about 70% response rate, versus 80% response rate. It’s still very good. The whole point is, if they hadn’t had it by Skype, they wouldn’t have been able to have it, because either they live right down the other end of the U.K. or the diarrhea… It’s an awful problem traveling anyway.
We do like to see them the first time face-to-face, so they get to know the therapists a little bit more. Then, the rest of it can be done by Skype. If we do them from abroad, we just sometimes do them by Skype right from the beginning. It’s very helpful.
DrMR: If someone listening to this wanted to get started, if we put a link to your website there, will it be easy for them to send an email or what have you? To get the ball rolling on this? Or, is there somewhere else you’d like to direct them?
DrPW: We haven’t got a website, because our hospital is sort of funny about all sorts of things to do with IT. The NHS… we didn’t even have Doodle Polls until recently. They are very risk averse. If you go into PubMed… Most people, I think, know PubMed. My name is unique on PubMed. If you put my name into PubMed, you’ll get all our publications, and that gets you a lot of information.
DrMR: Gotcha. Okay, I’ll talk with you offline about potentially finding a way to streamline the referral process for people, if that’s at all possible. We’ll handle that after, just so we don’t burn up too much time here with logistics.
Sponsored Resources
Hey, everyone. I’d like to thank one of my favorite probiotic companies for making this podcast possible, Klaire Labs. Again, Klaire is one of my favorite probiotic companies, which I have used personally and in the clinic. They offer a quality formula in each of the three categories of probiotics, most namely their Ther-Biotic Complete, their Saccharomyces boulardii, and their BioSpora.
They even offer specific blends, for example, a post antibiotic formula, a woman’s probiotic, and even an infant-focused formula. You’ve likely heard me discuss recent findings showing that probiotics can improve mood. One study, a high-quality randomized control trial, was using a Klaire Labs formula, Target gb-X, as in gut brain access. Klaire Labs, I highly recommend their probiotic line.
Does a Low FODMAP Diet Relieve Bloating and IBS?
Another question I wanted to ask you: What do you feel to be the best diet for distenders? One of the things I’m wondering about specifically, knowing that the IBS subgroup that seems to do the best with fiber supplementation is the constipated group. Does this group maybe do better with some FODMAPs or at least some minimally fermentable fibers to help keep things moving? Or maybe using something like a magnesium citrate as a laxative? What are you finding helpful there?
DrPW: You’re absolutely right. If you give a FODMAP diet… By the time people come to us, they’ve had the FODMAP diet. So, we don’t…
DrMR: I’m sorry, you mean the low FODMAPs diet?
DrPW: Low FODMAPs diet. By the time they come to us, they’ve tried that, so we’ve got to pull something else out of the bag. We take all fiber out of the diet and really, it’s a very restrictive diet. Yes, if you do the FODMAP diet, it tends to constipate. Our diet definitely constipates. So what we do, as I said already, the diarrheas do really well with the low FODMAP diet. The constipation, you’re going to make them worse.
So, what we do first is we get their constipation sorted out with a laxative and then say to them, “Once you’ve got your constipation sorted out, then you can try the low fiber diet and/or the FODMAP diet.” We warn them that they may then have to increase their laxative even further, because the diet is constipating. If you just stick people on these diets and don’t tell them that there is this problem of constipation, they’re going to find out in a flash and stop doing it. It is a bit strange when you give them one treatment and then have to give them a treatment to treat the side effects of the first treatment.
Safe and Effective Laxatives for Constipation
DRPW: With the sort of constipations we see in our clinic, which are pretty severe, they’re very bloated and distended, really, you’ve got to do that, you’ve got to clear their bowels out. Just clearing their bowels out will help a lot, if you really purge them properly. Some of our patients only go once every couple of weeks. We’ll say, look, we want to get you down to preferably once a day, once alternate days. So, you’re having to give them hefty doses of laxatives.
I don’t know how much the myth of laxatives damaging the bowel exists in the U.S., but just about every U.K. doctor has been taught that laxatives damage the bowel. And the public think that laxatives damage the bowel. So, you have to do a hard sell on these laxatives. Say, look, it’s nonsense that laxatives damage the bowel. Some of the older fashioned ones, like liquid paraffin weren’t good. But, the modern laxatives don’t damage the bowel. You can take them for the rest of your life and, actually, you’ll be a lot better with an empty bowel than a bowel that’s half-full of feces all the time.
DrMR: Mm-hmm (affirmative). You have a good point there. Are there some laxatives that you like more than others? I’ve heard that long-term use of Senna, which is a natural laxative, can cause, I believe it’s increased melanin. So, a darkening of tissue in the gut. Although Leonard Weinstock, a United States based gastroenterologist, doesn’t feel, at least in personal communication, that to be an issue that he’s really concerned with.
I’m wondering about Senna, MiraLAX, do you go all the way to things like your Amitizas, or… What are you liking there?
DrPW: Senna, it can make the lining of the colon go almost black. And so it’s always spooked people that this must be damaging the bowel in some way, but actually there’s just been another publication come out recently claiming that it doesn’t damage the bowel in any way. It’s quite difficult when you see a black lining to the bowel to think, gosh, what’s this doing. We don’t use Senna, we use Movicol, which is your MiraLAX. That’s the one that’s most used these days.

I think, the commonest laxative when I was a young doctor was Lactulose and that’s a FODMAP and god knows what else. That is really bad news for any IBS. It just creates a huge amount of wind. It’s still widely used in the U.K., so we banned Lactulose. We don’t use Senna because I’m just not too keen on it. We use Bisacodyl, which I think is available over your side of the Atlantic, and MiraLAX, or in this country it’s called Movicol or Laxido. They’re the main ones.
In the tertiary care group, for these really bad constipators, we use something called sodium picosulfate.
DrMR: I’m glad to hear your comments on MiraLAX. I’ve had a few patients where at least a small doses of MiraLAX, in some cases, using it every other day was enough to just tip the balance to keeping them at a level of regularity that they felt good about. In my mind, if we’ve done everything that we can to mitigate the need for medication, and then there is still a small need for medication, I’m much less in opposition to that, when we’ve made a case for minimal reliance on a medication.
I also performed a very cursory review of the literature on MiraLAX. There may be something here that I’m missing, in terms of side effects, but from that very cursory review, nothing significant jumped out at me in terms of a risk. It seems like you’re corroborating that there’s really little to no side effects or long-term negative impacts from the use of MiraLAX. Is that correct, or is there something there that people should be on the lookout for?
DrPW: No. Obviously a lot of my clientele is young females who want to get pregnant, they say, “Can I carry on taking this?” If they’re going to get pregnant, we usually stick to MiraLAX. No pharma company is ever going to reassure a woman that it’s safe to take anything in pregnancy. That’s the counsel of perfection. But we live in the real world and if somebody’s on laxatives, it’s going well and they know if they stop the laxative they’re going to go back to once every two to three weeks, that’s not a good thing to happen in pregnancy.
It’s the worst thing to be doing, is to stop the laxative when you get pregnant and then bung up. Then you have to take big does to clear them out. That could, in the early stages of pregnancy, actually, perhaps risk a miscarriage. We just say, look, just press on. There’s no evidence that this laxative causes problems in pregnancy. Obviously, we would prefer you not to take anything in pregnancy, but we live in a real world. If suddenly your bowels are going to stop working, that’s going to be more of a risk.
Does an Elemental Diet Relieve Bloating and IBS?
DrMR: Mm-hmm (affirmative). What about the use of an elemental diet? Are you using that at all as a form of bringing the fiber down? Obviously, that’s one way of bringing the fiber content down to zero. With some of the newer versions that are also palatable, I’ve seen those be very effective for select cases. Are you incorporating that, at all, into your model?
DrPW: Yeah. I should preface everything I say that I’m tertiary care, so I see the really, really bad patients. A third of my patients are suicidal. That’s the sort of level of the patients I see. Yes, we will resort to these various elemental diets and things to help the patients. Probably, one in three of patients will say to you, “If I didn’t have to eat, I’d be fine.” They have a strange relationship with food. When you see an anorexic with IBS and bloating and things, it’s a disaster, because obviously, it’s a good excuse not to eat if you’ve got bloating and irritable bowel. Even non-anorexic patients will say, food just doesn’t seem to settle well with me.
DrMR: Are you seeing that with time… let’s say as an example, take the distender/constipated type of a patient. You have them using some type of laxative. Your preference, of course, is potentially MiraLAX. That gets you moving forward. Then you perhaps had them using low FODMAP or maybe an elemental diet or maybe even both, which is something that I do. Do you notice with time, they’re able to expand their diet?
Yes, maybe they’re not able to go off the rails and eat whatever they want. But are you seeing ability to expand their diet, at least to some type of appreciable degree?
DrPW: Yes. I think that’s because they’ve got a handle on the problem. Then the stress level will go down. I don’t think IBS and all these conditions I see is caused by stress. I think you have to have the underlying propensity for the condition, probably genetic. Then, stress is one of the factors that makes it worse. One of many factors.
Hopefully when they come to us and they understand their condition, we’ve endorsed their symptoms, we’ve taken them seriously and then given them something that helps. The background stress levels go down. Then they do, you could say they experiment. We say it may not be an all or none, it may be a dose of that. The patient will say I love apples. I don’t know why, because I hate apples. They’ll say I love apples, but I can eat half an apple, but I can’t eat a whole apple. Or, I can eat an apple once a week, but not every day. So, yes, they gradually work up. It’s a dose effect. It’s not necessarily all or none.
Like females, their guts are very much more sensitive during menstruation, so you warn them. Say, “You may be able to eat things between your periods that you can’t eat during your periods.” It’s gradually getting a handle on your condition, so you’re not at the mercy of your condition. Rather than the other way around. You’re in control of it.
DrMR: Coming back for just one moment… By the way, I think that’s a fantastic perspective. I think it’s important for people to keep in mind it’s not like a light switch where you do some therapy and then, all of a sudden, everything’s fixed. It’s a gradual progression of your ability to tolerate foods and there will likely be a few speed bumps along the way. I think it’s important to also mention that for patients because, sometimes, when they’re feeling better and they try to expand their diet and they hit some turbulence, they freak out. As if they’ve broke something.
Sometimes just assuring them that, hey, we’re going to hit a few snags and that’s part of the process and that’s okay. That seems to provide a lot of solace for patients who are working through this.
DrPW: I couldn’t agree with you more. You need to warn them. They’re going to get complacent and then when they hit a bump, as you called it, they really lose the plot.

DrMR: Exactly. I just wanted to ask you, if I could paint this loose subgroup of the distender/constipated subgroup, where does hypnosis fit into the… first laxatives, then removing fiber? Where does this interface into the hierarchy or outlook?
DrPW: The one symptom that hypnosis doesn’t seem to help a lot is constipation. We can control the pain, we can control the bloating quite a bit. The loose ones do firm up nicely with hypnosis. A few patients do well, the constipated ones. We’re not shy in the constipation group. You don’t necessarily have to stop your laxatives, if you feel better on the laxatives, we’ll stick with them. Yes, treating the constipation/distender, you use the laxative and hypnosis to help with the diaphragmatic side of it. You’re sort of tackling it… You’re emptying the colon, because that’s the stimulus to this reversed reflex. You’re also, hopefully, normalizing the response of any distention of the colon with the hypnosis on the diaphragm.
DrMR: Gotcha. You would say, on the whole, does it tend to look better for the non-constipated, non-distended, bloating types?
DrPW: Sorry, I missed that question.
DrMR: Would you say, on average, hypnosis works better for the bloating, more diarrheal type and not quite as well for the constipated and distending type?
DrPW: Yes. I would say it’s minimal, but there is definitely a slightly better chance of responding in the loose group.
Treating Bloating/Diarrhea
DrMR: Gotcha. Okay. Now, coming to the other group here, that we haven’t really gone into much detail on, which is the non-distended, non-constipated, more so bloating without distension, who are more likely to be toward the diarrheal end of things. You mentioned low FODMAP. Are there any other nuances, in terms of the therapies that you’re using? And how you might lay out a one-two-three treatment hierarchy for this group?
DrPW: Yeah. Certainly I would go straight to the diet. We give the diet to everybody. The low fiber, low FODMAP diet to everybody, really. Obviously, as I’ve already said, most of them have tried the low FODMAP diet. They certainly get our diet. Then most of them we’d probably, if we didn’t have such a long waiting list, we’d probably go straight to hypnotherapy second.
The top two treatments for this group of patients would be diet and hypnotherapy. But, as I say, we do have a long waiting list for this. If they didn’t respond very well to the diet and we’re still waiting for the hypnotherapy, we would probably then give them a medication in the form of a tricyclic antidepressant. We prefer nortriptyline to amitriptyline because it’s a low dose. As you know, we used only use 10 or 20 mg with an antidepressant dose being 100 mg. The patients are usually happy to take that. And we say, “Why don’t you see if it works?” If it doesn’t work, we won’t continue with it. If it does work, then when the hypnotherapy comes round, we probably withdraw it and then give you the hypnotherapy.
It’s useful, then you know you’ve got another backup if ever you’re in a really difficult place. Or, the hypnotherapy doesn’t work quite as well or something. It’s quite nice to have a backup. If somebody’s got loose bowels and is taking loperamide (Imodium) then you do have to warn them that loperamide can actually make your bloating worse. It’ll stop your bowels going, but if you overdo it, it can make the pain and bloating worse. Certainly, loperamide is really good stuff for getting from A to B, if you’ve got a very loose bowel. But continuous loperamide, yes some people respond quite well to it, but there is a significant risk of making your bloating and pain or discomfort worse if you overdo loperamide.

Whereas, with the tricyclics, you get the anti-diarrheal effect like loperamide, but you get the pain effect, the bloating effect and everything, because it’s hitting on the visceral hypersensitivity.
DrMR: Gotcha. Just for people in the U.S., that’s an aka for Imodium. A simple, over the counter…
DrPW: Loperamide is American. Interestingly with the hypnosis, we’ve shown that if you put the old balloon up your bottom and do the visceral hypersensitivity test, we can restore visceral hypersensitivity to normal sensitivity. Quite consistently.
DrMR: Hmm. There was one study I know of that showed, I believe it was a reduction of leaky gut with loperamide, aka Imodium. There is some evidence, I think, to show benefit there, even thought I would assume a fair number of people in our audience are probably somewhat resistant to medications. I would just offer people the thinking of it doesn’t have to be an either or venture. If you prefer natural, that’s totally fine, and I think a great place to start. But we shouldn’t be dichotomous where if we like natural, we’re going to be anti-medicine. We should be open minded and think about these things in the hierarchical fashion, as you’re alluding to, Peter.
We start them off with diet and hypnosis, natural therapies. Then, we can potentially get some more gain, if needed with a medication.
DrPW: Yeah. We’re not afraid of… we always say, because we’re rather well-known for our hypnosis… we say, look, this is not a stand-alone treatment. We’ll add things in and maximize the benefit. All these things are add ons, so you get more benefit with the diet and hypnosis and perhaps the tricyclic. We’re not afraid. But we have to say to a 20-year-old who’s in trouble, you’ve got this problem for the rest of your life, so we want to try and keep drugs out of it as long as we can. Then, we would like to use tried and tested drugs like amitriptyline, nortriptyline and the laxatives which we know are safe.
The newer things like Linaclotide and Prucalopride, we will use those, and they are very useful. They have a useful place. Linaclotide can have a significant effect on bloating and we shouldn’t really ignore that one because it does work for bloating. As does Prucalopride.
Additional Dietary Advice for Bloating
DrMR: Back to the topic of food… Are there any other highly impactful, important dietary modifications that you think are important to incorporate? I know that there has been some evidence showing that fat can potentiate visceral hypersensitivity. This is where I think of the LOFFLEX diet, which is a low fiber and fat diet, which has mainly been applied in inflammatory bowel disease. I’ve had a handful of patients, where being mindful of fiber and fat has been helpful, just as one example. Are there any other food changes that are fairly impactful that you think we should make sure to include here?
DrPW: Yep. I could point out fat on our little diet sheet we give patients. It says fat can upset you. It’s important to sort of take that a little further with patients. It’s fat irrespective of the source. The fat in the full-fat milk could upset you just as much as the fat on a rather fatty piece of lamb or something like that. We say it’s fat, in general, that upsets you. For instance, people will often say, I go out for an Indian meal and it upsets me. They immediately think it’s the spices, but the Indian meal you have at an Indian restaurant in this country will have a huge amount of fat and ghee in it. Whereas, if you make it at home, and I quite often say to patients, “You try making a curry at home and don’t put much fat in it, you’ll probably be okay because spices don’t always cause trouble.”
Yes, fat is certainly something that they need to think about. And gluten, of course, is the other chestnut that everybody’s talking about. Yes, some people do seem to be intolerant to gluten when they don’t have celiac disease. It’s called non-celiac gluten sensitivity these days. I sometimes wonder whether it’s due to the fiber, because people still insist on eating brown bread and thinking gluten, and it’s probably just the fiber in it.
DrMR: There’s some research that attempted to parse that. There have been some studies that have done both a gluten withdrawal and a FODMAP withdrawal, and then they’ve given either a placebo, a gluten capsule, or a FODMAP capsule. From my read of the literature here, the last one on this was about a year ago. It seemed that about 80% of the studies showed that gluten was a problem. But, there was maybe 20% showed that it was FODMAP being the problem.
I wouldn’t take that quote too literally, because I don’t think the studies were designed to all parse that equally. I think we could probably say that you could go either way. For some people who think they have a problem with gluten, this is the key take home. They may not actually have a problem with gluten, they may have a problem with FODMAPs, and as they heal their gut, they’ll be less FODMAP sensitive. It’s important not to just fall into the hysteria of gluten free, as helpful as it can be for some people. Yes, I absolutely agree. We want to make sure we personalize this to the individual, not avoid it blindly due to fear.
SIBO and Bloating
Okay, now, what about bacterial overgrowth? SIBO, dysbiosis, small intestinal fungal overgrowth is another thing. There’s some interesting research being published on it. Are you evaluating this? Treating this at all?
DrPW: Yeah, certainly it’s a very big thing in the U.K. at the moment. Everybody comes in saying, I’m sure I’ve got SIBO. There is definitely some evidence that people have dysbiosis of the gut. I suppose that’s not surprising. At least a third of the patients we see have had antibiotics on a long-term basis. Usually in childhood, for either tonsils or sinuses. Or in adolescence for acne, where you often get antibiotics for a couple of years. It’s not surprising that that group of patients or people who have had long-term antibiotics for other things, they almost all have dysbiosis.
So, whether that’s SIBO or not… Because SIBO is small bowel bacterial overgrowth, whereas dysbiosis is thought to be more colonic bacterial imbalance.
My problem with SIBO, even though we test in my lab we do the test for SIBO, is it cause or effect? We know that irritable bowel is a bit of a motility problem and we know if the motility of the gut isn’t quite right there is a tendency for bacteria to multiply. It’s like a stagnant drain, you’ll get more bacteria.
So, my problem is, is the SIBO the cause of the IBS? Or is it the IBS that’s leading to the SIBO? I feel that sometimes it’s more likely to be due to the IBS. Because you treat the SIBO, they get a bit better for a while, then it comes back again. I am a little bit concerned about giving repetitive courses of antibiotics. So, we do the test for patients and we’ll give them a couple of treatments if they’ve got a high breath hydrogen indicating SIBO. But, I’m not very keen on giving people antibiotics for the rest of their lives, every so often, if they’re in their 20s or 30s.
Patients are very keen to have it treated and of course patients with these conditions are keen to have abnormal test. So, when you come up with an abnormal test, they always want to be treating. I’m very much sitting on the fence about SIBO. If you go to meetings, you’ll get about 50% of people hotly saying that SIBO is really, really important and the other half saying it’s a load of nonsense. I’m merrily sitting on the fence, at the moment. I’m sure when the final chapter is written on these conditions, bloating and IBS and things, I’m sure there’s something going on with the bacteria.

You get a patient sometimes who will take an antibiotic for a cold or chest infection, and they say my bowels became normal. There’s something going on in there, but I just really don’t think we know what’s going on yet. Then, of course, fecal transplantation is all the rage now. We’re just about to start looking at that. So, yes, a lot to be learned. And, as you say, that’s called the microbiome, and now everybody’s getting interested in the fungizome. The fungus in the gut, we’ve got lots of funguses. One of my predictions is that we are ignoring at our peril, at the moment, the virome, the virology going on in the gut. There are tons of viruses in our gut.
I did work in the States many years ago, on Crohn’s disease, actually. I was amazed when I looked at stool under the electron microscope. It’s teeming with viruses.
DrMR: Mm-hmm (affirmative). One of the causes, although as I understand it, very rare, of highly recalcitrant or non-responsive inflammatory bowel disease can be cytomegalovirus. There is something interesting there and this is why my belief has been not to lead with the hubris that we know more than we do, and humble myself to the fact that the gut is really like an ecosystem. We want to look at all the inputs that we can use to improve the health of the host because, arguably, if the practices of the host create a healthier internal environment, then we have healthier soil for the bacteria, fungi, viruses all to live in.
So, I do think there’s a degree of this that’s very much dependent upon making the host as healthy as you can and not getting too wrapped up into what one lab says. Per your SIBO example, I think it’s a fool’s errand to treat someone exclusively based upon their SIBO results. Because then you miss the forest for the trees. I agree, there’s much more here to learn, which is why I think all practitioners should be a bit humble and not prone to extrapolate from lab work.
DrPW: Yeah. And stop nuking it with antibiotics.
The Case for Probiotics in IBS
DrMR: Right. Agreed. What about probiotics? One could make the case… There have been a handful of clinical trials showing that probiotics can actually decontaminate SIBO out of the small bowel. There have been, I believe, at least 99. That was about six months ago. So at this point, there’s probably well over 99 clinical trials in IBS showing benefit with probiotics.
I feel that they sometimes don’t get the attention they deserve. Possibly because there’s many different formulas and quality regulation could be a concern. What are your thoughts on probiotics?
DrPW: I am positive about probiotics. I’m not sure if they’re suitable for the sort of patients we see in the tertiary care… Suicidal group, we’ve got pain like labor pains, they look pregnant all the time and terrible bowels. I see probiotics as modulators of the gut. I say to patients, “I think these things sort of harmonize the activity of the gut.” We did a study some years ago with a probiotic. It’s always difficult to think you’re giving a little tiny probiotic, a few million into an ecosystem that’s got trillions. How can it change it?
The study we did showed… Sponsored by Danone. They would look to the stools of these patients after they’d been treated with the probiotic. It showed that this probiotic was there, but it had also encouraged new probiotic organisms to multiply as well. So, it could be that just giving a probiotic doesn’t just put good germs into you, it encourages other good germs to take up residence and multiply. And, that makes sense to me.
We know that probiotics can modulate your immune system. Some probiotics can actually kill other bacteria. Salmonella can be killed by some probiotics. I think the big problem is it’s so woolly. Just because one lactobacillus does you good doesn’t mean to say a different lactobacillus does you good. As you rightly say, very few probiotic preparations have actually been submitted to clinical trial. The majority, 99% of probiotic preparations are just out there untested. But they may be better than the ones that have been tested.
It’s a really difficult field. So, what I say to patients is we’ve done a clinical trial with these two probiotics, try these first. If they don’t work, just go to the health food shop and try a few off the shelf. See whether you find one that helps. The majority of the clinical trials have shown a signal… that is they help. But they’re not like a proton pump inhibitor which reduces acid 90%. It’s not that sort of massive effect. It’s sort of modulating the gut and gradually normalizing the bacteria. That’s what I tell them. Don’t expect to swallow the probiotic and within two days you’re going to start feeling better.
That’s the placebo bit. I take a probiotic every day because it can’t do me any harm. The one I take has been shown to boost your immune system a bit, so I take that. People always come out with stories of the two trials that have shown that they can cause problems. But for those two trials, there have been millions that show no effect. No detrimental effect. I say to patients, “By all means take them.” If I saw milder patients, I would be peddling them more frequently.
DrMR: Gotcha. I think that’s well said. I appreciate you pointing out that there have been, literally, only two studies showing negative effects. One, in particular, showing an increase in SIBO gas levels. Yet, the thing that was left out of that criticism was there was no change in symptoms. At that point, it may have just been a nominal change on a lab test that wasn’t tied to any clinically meaningful change in how someone was feeling. We should juxtapose that with the overwhelming body of evidence showing benefits.
I also understand your concern about working with a highly sensitive patient group. That kind of bridling your enthusiasm or vigor for which you would use probiotics. One of the ways I’ve circumvented that is having patients perform only one probiotic at a time. Letting them know that this may be prone to cause a reaction. If it does, give yourself a few days, because sometimes there’s a little bit of adjusting turbulence, but after a few days, if you’re not feeling at least at your baseline, if you’re feeling any worse than baseline, we can discontinue. That way they don’t come back three weeks later and say, “Boy, I’ve had diarrhea the whole time I was on this probiotic.” Sometimes, if you’re a really diligent patient, you will keep doing something, even if it’s clearly not working.
View Dr. Ruscio’s Additional Resources
Immune Activation in the Gut
A final kind of clinical question here… then we can move to a few closing bits. Immune activation in the gut is something that I think thwarts some patients from seeing the level of improvement they would like. I guess another way of describing inflammation is immune activation, they’re kind of the same thing. What I’m meaning, more specifically, when I say immune activation is how that label could pertain to some of the corresponding treatments. Histamine has been shown to be an issue for a subgroup of IBS patients. We know that a low FODMAP diet can lead to an appreciable decrease in histamine levels. A low histamine diet can improve symptoms and also increase the amount of histamine digesting enzymes, specifically DAO, that the patient releases. There may even be some type of healing impact that can be imparted by a low histamine diet.
Then, we have certain immunoglobulin formulas, like ImmunoLin, that are showing the ability to bind toxins in the gut and, theoretically, they help to improve symptoms by reducing immune activation. If you bind to the irritant, then the irritant can’t trigger the immune system to cause this whole cascade of inflammation and leaky gut and what have you. Is there anything here that you think is interesting, or that you’re experimenting with?
DrPW: This is a very tricky area. When I was in the States, I was an immunologist. I’ve been various things in my long career. Immunology was the answer to everything when I was a young doctor in the 70s. Then, it went into abeyance. Now, of course, we’ve got all of these monoclonal antibodies and things. Yes, I think the immune system in the gut is so complicated. The interaction with mast cells… You know, mast cells release so many active amines that it’s very bewildering, at the moment, to know what’s going on.
Food antibodies is another one. IgG food antibodies. That’s incredibly controversial. We did a trial with that and got an effect with IgG food antibodies, taking the foods out to which we have antibodies. So many normal people have antibodies that everybody’s rubbished that. But, we got an effect. Then there’s of course dietary allergy. We published showing in the IBS population, bloating, functional bowel disorder population have a higher incidence of atopy.
There’s a new treatment for asthma with anti-IgE monoclonal. I’ve had a few patients with severe asthma who have been given this anti-IgE monoclonal, and their IBS has just disappeared. We’re seeing all these signals that the immune system is wonky in some of these patients. I think the trouble is, because we have no biomarkers for functional disorders, it’s the clinical diagnosis. I’m always saying when the final chapter is written on IBS, there will probably be ten subtypes of it. Some of them will be driven by immunology. Some of them by enzyme deficiencies. There’s this isomaltase deficiency they’re talking about now.

I think we’re calling it one condition, something that is probably ten interrelated conditions. I think you’re right, the immune side of things is unraveling. Where does inflammatory bowel disease end and irritable bowel start? Or the other way around? Are they part of a spectrum? Or are they completely different? I think genetics will help sort this out. We’re doing quite a lot of gene stuff, at the moment. If we can pinpoint different subtypes of IBS. Does the bloater have a different genetic makeup to the diarrhea?
It seems bizarre to me that you’re calling a patient who has abdominal pain and not opening their bowels for a month the same as a patient with abdominal pain that’s opening their bowels 20 times a day. We’re calling that the same condition, at the moment. And that seems a little odd, when we look back on it, I suspect.
DrMR: At least we have the IBS-C versus IBS-D, but your point is taken. They’re still subtypes of the same condition and we may learn that there is quite a bit of difference as we increase our diagnostic yield. Just to get nerdy here, for one quick second. Dectin-1 or CARD9… are those either of the gene markers that you’ve been looking at?
DrPW: Were looking at the U.K. Biobank. We’re looking at just about everything. Looking at a couple hundred thousand people and seeing if we can pick out something. I think it will be a sort of fishing expedition. I suspect it will be a very muddy response. It’s a bit like Crohn’s disease, it started off with one gene, this NOD gene. Now they’re up to 100 genes in Crohn’s disease. I suspect it’s going to be very muddy.
DrMR: That’s one of my fears with the gene testing. This is known as the Dunning–Kruger effect. The less you know about something the more confident you are about it. I think with the genes, there were a handful of genes that were correlated to a few different things. The more and more we learn, like you said, it’s going to be very muddy, most likely. There will be so many potential ways to go based upon a gene test that you end right back where we are today. Which is good clinical horse sense; looking at a person and trying to figure out what sort of treatment hierarchy you should construct for them based upon their signs or symptoms or history. The gene testing, hopefully will have a few things that are helpful. But, I don’t anticipate it to be this huge cathartic change in how we practice.
DrPW: I think that’s why this area is so interesting as a clinician. In the U.K., we’re getting all these blunt pathways now, where you just have to tick a box. You go through an algorithm. Whereas, with these patients, it’s all seat of the pants stuff. Every patient is different. We’re giving them some of the treatment pathways but you can’t really have an algorithm for these conditions. You have to use clinical judgment, as you rightly imply.
DrMR: Sure. You have maybe a loose algorithm. But then you have to personalize how that’s applied based upon the individual.
DrPW: Absolutely.
DrMR: Well, as we move to a close, is there anything that you want to leave people with that we haven’t touched on, that you think is important?
See Your Doctor Right Away if You Have This Type of Bloating
DrPW: I ought to just raise one negative point. It’s a cautionary point. The important feature of bloating and distension is it’s diurnal, which means it varies. The typical pattern is that they’re not too bad in the morning, then it gradually gets worse during the day. Or, it fluctuates during the course of the day. That’s absolutely crucial. If I see a bloater or distender who doesn’t change slightly over the course of 24 hours, that’s a red flag for me. We have to think of other things.
There are two things… The one thing that women are worried about is ovarian cancer. So, when they start distending, it’s in all the women’s magazines, they start worrying. I think any patient who has got bloating or distension and it doesn’t vary, they probably ought to be seeing a doctor sooner rather than later.
The other cause of distension that doesn’t vary is accumulation of fluid in your abdomen. Ascites, as it’s called. Again, that’s a red flag that it might mean something different than IBS or functional bloating or something like that. It’s so easy. As long as the bloating or distension varies a bit, it can’t have a sinister cause and its part of the spectrum that we’ve been talking about today.
DrMR:That’s fantastic. I’m very appreciative of that note, because certainly we don’t want people chasing down the gut link when it may not be something in the gut. Or, something more serious. That’s a fantastic point.
Episode Wrap Up
DrMR: Hey guys, just one quick note… Dr. Whorwell forgot to mention during the interview that he has a book out, called Take Control of Your IBS. We’ll put the link in the transcript and it’s also available on Amazon. Take Control of Your IBS, the book by Dr. Whorwell.
Peter, thank you so much for taking the time to speak with us today. This was a fantastic conversation. Very insightful. I know you don’t have a website, but you mentioned PubMed earlier. Is that where you’d like to direct people if they’re interested and want to learn more about you and your work?
DrPW: Unfortunately, if you Google my name, my surname, everything about me is sort of at the top. It comes up as the university website where I’m based at Manchester. Then, it has a profile about me and e-mail address and everything.
DrMR: Gotcha. It’s just Peter Whorwell.
DrPW: Just Peter Whorwell in Google, and you’ll find it.
DrMR: Alrighty, sir. Thank you, I appreciate the time.
DrPW: Good, thanks for having me on.
DrMR: It’s been a pleasure.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.






Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!