Steps to Lower your Alzheimer’s Risk, with Dr. Dale Bredesen
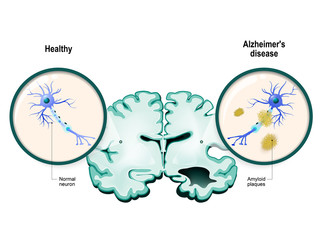
A diagnosis of Alzheimer’s disease (or similar degenerative neurological conditions) is devastating, as, so far, no cure exists. However, recent studies into the condition show that the amyloid plaque responsible for Alzheimer’s symptoms may form as a protective mechanism against other threats to the body. Promising research into the disease shows the possibility of prevention and even reversal of cognitive decline. There may be multiple risk factors for Alzheimer’s, such as chronic inflammation, chronic infections, tick-borne illnesses, the presence of the ApoE4 gene, mold or heavy metal toxicity, hormone changes, and others. Getting a “cognoscopy” at age 45 could give early warning indicators. Prevention protocols may vary widely among individuals. Some foundational tips include inducing mild ketosis, sleeping well, reducing stress, exercising, and treating underlying conditions.
What can cause a change in your cognition?
- Chronic inflammation (for example, leaky gut)
- Undiagnosed chronic infections (very common)
- Tick-borne illnesses – Babesia, Bartonella, Borrelia, Anaplasma, Ehrlichia
- Living with mold in your immediate environment (home or workplace)
- Mercury from dental amalgams, or from eating swordfish, shark, tuna
- Various organic toxins, like toluene, benzene, formaldehyde
- Biotoxins, like trichothecenes, ochratoxin A, gliotoxin
What can you do?
- There is about a 20-year period between when the underlying process actually starts in your brain and when you receive a diagnosis of Alzheimer’s
- Diet, fasting, exercise, sleep, stress, brain training
- Diet – remove processed foods and address insulin sensitivity, try keto diet
- Optimizing Vitamin D and zinc
- Hormone balancing
- Mitochondrial support
- Paper showing 100 people with documented Alzheimer’s or pre-Alzheimer’s, who had documented improvement in their cognition.
What is a “Cognoscopy” and when should you get one?
- Cognoscopy is a term coined by Dr. Dale Bredesen and refers to a thorough screening, recommended at age 45, to see what your risk of developing Alzheimer’s Disease
- It is recommended for age 45 or over (you can get it done sooner if you like)
Testing for ApoE4
- Can be done at any major lab
- Great resource www.apoE4.info
Lyme testing
- PCR urine tests
- Can give false-positives, still needs work but may be a promising test for the future
- IGeneX has a very good panel
Hormones and Alzheimer’s
- Female hormone issues can affect cognition
- Surgical or hysterectomy-induced menopause
- Estrogen and progesterone both affect various neurotransmitters
- Hormone therapy and herbal therapy can be helpful tools
- Males in the lowest quintile of testosterone levels have a much higher likelihood of developing cognitive decline and Alzheimer’s
- Suboptimal testosterone would be around 250
Where to learn more
In This Episode
Episode Intro … 00:00:40
The Surprising Origins of Alzheimer’s … 00:03:25
Early Alzheimer’s Warning Signs… 00:07:44
Varying Contributors to Alzheimer’s … 00:11:19
Habits for Brain Health … 00:13:51
Mast Cell Activation Disorder & Alzheimer’s … 00:21:55
ApoE4: a Risk Factor … 00:24:25
The Microbiome and Alzheimer’s … 00:30:37
Defining Protocols for SIBO and Lyme … 00:34:50
Female Hormones and Alzheimer’s … 00:37:48
Male Hormones and Alzheimer’s … 00:43:54
Is Mercury a Common Cause? … 00:46:12
Episode Wrap-Up … 00:52:57

Download this Episode (right click link and ‘Save As’)
Episode Intro
Dr. Michael Ruscio, DC: Hey, everyone. Welcome to Dr. Ruscio Radio. This is Dr. Ruscio. Today I’m here with Dr. Dale Bredesen and we are talking about cognition, which, of course, is really important. If anyone listening has ever had brain fog, which I have, it’s a very unpleasant and debilitating symptom.
So I’m really looking forward to having the conversation with Dale, and drilling down into some of these details. So thanks for being here and welcome.
Dr. Dale Bredesen: Absolutely. Thanks for having me.

DrMR: You’ve done a lot of great work in this space. I hear your name repeatedly when it comes to cognition. This is a conversation I’ve been wanting to have for a while. I have to apologize, I haven’t done a deep dive into your work, so a lot of what I’ve picked up has just been bits and bytes, and things through the grapevine, all good. I do know you have this web, I think it’s 33 or 31 factors of causality for cognition. Is that correct?
DrDB: Yeah, 36. So this is just looking at why people get Alzheimer’s, why it’s so common, and what does it actually represent. That’s how we came up with that.
DrMR: Gotcha. And I’d like to give the audience an overview of that. If we can’t get through all 36, that’s fine. I’m sure there are some that may be highly relevant and affect a lot of people, and some that may be a little more nuanced. But how do you launch into this conversation on cognition and the model that you’ve developed?
DrDB: All right, so let me give you 30 seconds of background here. I’m a research neurologist. We spent 30 years in the lab looking at: Why is Alzheimer’s so common, what is the problem? Why have we been so unsuccessful about treating it? As you know, you can argue that this is the area of greatest biomedical therapeutic failure. As they say, everybody knows a cancer survivor, nobody knows an Alzheimer’s survivor.
Whether you’re talking about Alzheimer’s, ALS, frontotemporal dementia, Lewy body disease, there just haven’t been any advances. These are death sentences. So, of course, we were desperate. And we were going to look at what is actually going on here. If you look at how the treatments are set up, they’re trying to do something without knowing what’s causing the disease. It actually makes no sense.
As we tell people, when someone tells you you have Alzheimer’s, it’s like taking your car in and they say, “Oh yeah, you have car-not-working syndrome.” It really doesn’t mean anything, and they don’t tell you why. They say, “Okay, things are going to fall apart.”
So we wanted to understand. We spent years looking at what molecularly drives the degenerative process. Why does it happen? I agree with your point, that this is all about cognition. And what we found really impacts cognition for everyone.
The Surprising Origins of Alzheimer’s
What we found is that Alzheimer’s disease is a protective response, just 180 degrees the opposite of what we’ve been told. It’s a protective response against a series of insults that we suffer as we age. In fact, we can suffer them early on and we handle them for a while.
Whether you have chronic inflammation, which can be due to things like leaky gut (very common), undiagnosed chronic infections (incredibly common), tick-borne illnesses, Babesia, Bartonella, Borrelia, Anaplasma, Ehrlichia—it’s shocking how many of these different things can go undiagnosed—this is essentially the neuro-syphilis of the 21st century. And as you know, the Lyme organism, Borrelia, is a spirochete, just like the syphilis organism, Treponema.
So whether you have those, whether it’s specific toxins or whether you’re living in a moldy home and you don’t even realize it, it’s causing a change in your cognition. I was shocked when—as someone trained in classical medicine and basic science—I first understood that living in a moldy home can be a critical contributor to cognitive decline. I was really surprised.
Then, there are various toxins. Whether you’re talking about mercury that you may be picking up from dental amalgams, or from eating swordfish, shark, tuna and things like that, or whether you’re talking about various organic toxins, like toluene, benzene, formaldehyde; or whether you’re talking about biotoxins, like trichothecenes, ochratoxin A, gliotoxin, these are all contributors. You are literally protecting yourself when you produce the amyloid that we associate with Alzheimer’s.
And as it’s been shown, in very nice studies by Professor Robert Moyer and Rudy Tanzi at Harvard, this amyloid that we make, that we associate with the Alzheimer’s (that we say is the bad guy) is actually an antimicrobial. It’s quite a good endogenous antimicrobial. It also, by the way, binds metals quite nicely.
So you are literally trying to protect yourself. If you can imagine having a country where you’ve got the bad guys coming across the border, you’re now going to put down napalm to try to kill the bad guys. But of course in so doing, you are retreating, you’re pulling back. You’ve got less arable soil. That’s exactly what’s happening in Alzheimer’s. It is a protective downsizing program.
Okay, so we’ve got to now look at this in a completely different way and say, “To optimize our cognition, we want to look at all the factors that are creating problems.” Why do we have to protect ourselves against these insults? We want to remove those. Then of course, we want to optimize all the pro-cognitive factors. And I’m sure you’ve talked about nootropics and things like that.
But there’s lots that can be done in terms of insulin sensitivity. It’s essentially all the anti-Alzheimer’s things: including increasing your BDNF, making sure you have appropriate cholinergic tone, making sure you have appropriate building blocks for synapses. There’s a tremendous amount that can be done. In fact, most of us don’t have the optimal cognition that we could have.
When we’re going toward Alzheimer’s, there is about a 20-year period between when the underlying process actually starts in your brain and when you receive a diagnosis of Alzheimer’s. So, you have a tremendous window of opportunity there. And we’ve now seen unprecedented improvements. We’ve published a paper just two months ago, showing 100 people with documented Alzheimer’s or pre-Alzheimer’s, who had documented improvement in their cognition.
DrMR: Awesome. That’s a fascinating way of looking at this and it’s a terrific thing to uncover, that there’s this pyrrhic victory, if you will. You’re winning the battle, but it’s such a devastating cost to your own side.
Early Alzheimer’s Warning Signs
So I’m assuming there are certain early indicators? A decent amount of our audience has probably suffered with brain fog, loosely termed, or some feeling of cognitive impairment. Is that something that’s suggested? Let’s say somebody has really impaired gut health; they eat a certain food and then they get brain fog.
DrDB: Yes.

DrMR: Is that one of a number of symptomatic early indicators?
DrDB: Absolutely. In fact, what you indicated is really important here, that everything now has got to be reconsidered. When there was nothing to do about this, people kept saying, “Well, don’t worry because there’s nothing you can do about it anyway. So don’t get checked, don’t evaluate your genetic status, don’t look at these other things, because there’s nothing that you can do about it. It’s probably not Alzheimer’s.”
Really, you should be doing the opposite of that. We want to look f. So what we recommend is that everybody who’s 45 or over get a cognoscopy (and it’s fine to do it before that, but you want to get a colonoscopy when you hit 50).
That is to say, you want to know, what’s my status with insulin resistance? If you have insulin resistance, which about 80 million Americans do, then you want to make your insulin sensitivity return. If you have chronic inflammation, if you have suboptimal nutrients, the critical point here is that there is a supply and a demand for making and keeping your synapses. And a mismatch between what is supply and what is demand, is what underlies neurodegenerative processes.
Whether you’re talking about Alzheimer’s, whether you’re talking about macular degeneration, whether you’re talking about ALS, what have you, there is a chronic mismatch. So you need to measure that.
Now as you indicated, when you get symptoms—that actually takes a while, your body is set up to deal with these things for some period of time, it may be a few years in some people, a few decades in others—absolutely, when you have a change in your cognition, you need to get evaluated. At the very least, get some basic blood tests. I outline these in the book. Also, get some online cognitive assessment.
Now, the good news is, you don’t have to go through four hours of neuropsychological quantitative testing. You can go online and within 20 or 30 minutes for either nothing or next to nothing, you can see where you stand cognitively. Often, we find out that people who come in for “prevention,” when we actually test them, are already into the mild cognitive impairment which is the pre-Alzheimer’s condition. That means the underlying process in the brain has been going on for several years already.
So absolutely, if you have brain fog, please get it checked out.
DrMR: Okay, so here’s a question I ask, admittedly with my own bias imparted into it. But I think back to this case study we published on our website a few months ago. I’m not sure if people in the audience have caught it yet. If not, I’d recommend checking it out. It was a moving case study with Harmanjeet, who is a young woman working in San Francisco. Came into our clinic because she had such debilitating brain fog, she was worried she was going to get fired.
And it turns out the two big things for her were: low FODMAP diet, partially helpful, and then she did have small intestinal bacterial overgrowth. Treatment of those two things combined led to a complete resolution of her brain fog.
Varying Contributors to Alzheimer’s
So the question I ask in that context is, before going to quantifying the cognitive impact, do you think it’s a good practice to look directly to some of the underlying factors, like someone’s gut health?
DrDB: Yeah. So I think that the two go together. In other words, you want to know, am I going in the right direction when I have the low FODMAP diet, for example? When I change one thing or another? Am I going in the right direction? Now, you will obviously have subjective changes. I’m more alert, I can follow directions better, I can remember things better. And we hear this all the time. But of course, people will say, “Oh, this is placebo effect.” So you want to document where you stand both before and after.

But what you indicated is so critical, because I keep getting the comments, “Oh well, this alone doesn’t do it. Diet isn’t important.” Well, each of these things has a role. And again, we have to reconsider medicine.
When I trained in medicine, this was the late 1970’s and early 1980’s, a long time ago. What we were taught is that you look at what it is, you make a diagnosis, and then you write a prescription. The fact of the matter is, that’s 20th century medicine. 21st century medicine is not about monotherapies. It’s about programmatics.
So you want to look at all the things that are contributing. Obviously in the case that you just talked about, the gut was contributing importantly. In some people, it turns out that leaky gut or SIBO or things like this are absolutely important. In other people, it turns out that they have critical pathogens. In others, it turns out that there are critical toxins.
We had one interesting guy that came in and had already had a PET scan, had already been told he had early Alzheimer’s, and they said, “Come back in a year. You’re not doing that badly yet.” Luckily, he didn’t wait and called me up. I said, “Look, you have Type 3 Alzheimer’s, which is Toxic Alzheimer’s, and you’ve got some toxins there based on your presentation.” He said, “No, no, I live a very clean life, etc.” Well, the long and short of it was, he had the highest mercury content that had been seen for multiple years in the laboratory which did his testing. And he got that treated and he’s doing much better now.
So you have to look. Each person is different. All these things can contribute ultimately, but as you indicated, it’s basically a combination. For some people it’s going to be a change in their diet, for other people it’s going to be detoxification, for other people it’s going to be hormonal changes. You’ve got to look. It’s different for each person.
DrMR: Sure, that’s fair.
Habits for Brain Health
Just to make sure we don’t gloss over some of the foundation for people, I’m assuming that we’ll get a large subset of the population responding pretty favorably if we get them on a diet, at the very least, that limits processed foods and blood sugar spikes (there are nuances, I’m sure). In addition, I assume some intermittent fasting and some exercising, maybe some sauna therapy. You’re going to get a lot of yardage. Are there any other really big, simple, foundational lifestyle or dietary pillars?

DrDB: So for the diet, definitely we want to get people into mild ketosis. We’ve looked and compared the ones that got into ketosis with the ones that didn’t, and definitely they do better if they do. We recommend 1.5 millimolar to 4.0 millimolar beta hydroxybutyrate. So, good idea. You can get a very inexpensive ketone meter and check things out. That’s very helpful.
So as you indicated, diet, exercise, sleep, stress, brain training, some basic synaptic support, and various supplements can be very helpful, including some herbs. They may need hormone balancing. Those are the basics. And you’re right, many people will respond very nicely. No surprise, the earlier you are in the process, the better and the more complete the responses are. So at this point, prevention is relatively straightforward, when you optimize these various parameters.
However, there are other people, who with all those things, will not maintain their improvement. You need to look at the pathogens, the toxins, whether there’s underlying vascular disease, autoimmunity, and things like that.
DrMR: Yep, makes complete sense. Regarding supplements, are there are a handful that you find to be particularly helpful? I’m sure there’s supplements, obviously if there’s a certain condition that you’re trying to treat that are case-specific, but are there some foundational brain support supplements that you find to be helpful?
DrDB: Again, it’s personal. We have a computer-based algorithm that we use when we evaluate all these different things, and to see who needs what, who is subtyped. We identified and published about subtypes a few years ago. There are people who are more on the inflammatory side, more on the atrophic side, more on the toxic side, more on the glycotoxic side, etc.
In general, number one, ketosis turns out to be helpful for your brain and for the brains of these patients. So, MCT oil, things like that can be very helpful, or even exogenous ketones, depending on whether you’re able to generate ketones or not.
Secondly, things like magnesium threonate can be helpful for some people. Again, it’s on a personal basis. Things that support the immune system. In fact, the old approach of using amalaki, tinospora, and ashwagandha is very helpful. Ashwagandha actually does help you to clear amyloid from your brain.
Now, you don’t want to clear the amyloid without taking away what’s causing it. You have to link those two things up. This idea that we’re just gonna get rid of amyloid and everything’s gonna be fine, that has not worked. You’re putting it there for a reason.
Curcumin has turned out to be very helpful for many people. Optimizing vitamin D. Many people, as you know, are suboptimal in their vitamin D. Zinc is another one. There are about one billion people on Earth, as you know, who are zinc-deficient.

So all of these things have turned out to be helpful. Again, different people, different things, but it depends on where you are lacking. Many people are high in homocysteine, as you know. There’s very nice work out of the UK showing that as your homocysteine rises linearly above six, you have an increase in the rapidity with which you have atrophy of your cerebrum.
DrMR: Now, we recently had Jon Kaiser on the podcast, who does some research in mitochondrial dysfunction. And with age-associated mitochondrial dysfunction, the two biggest things he saw were immunosuppression and cognitive decline.
DrDB: Yeah.
DrMR: So… NAC, alpha-lipoic acid, CoQ10, acetyl l-carnitine. Are you finding these to be pretty helpful also?
DrDB: Absolutely. Mitochondrial support is part of this. If you remember, go back to: this is a fundamentally a mismatch between what is supplied and what is demanded. In this case, for making synapses. In the other diseases, for motor control or for your macular support, on and on and on.
So in this case, you’re talking about a trophic mismatch. Of course, if you don’t have mitochondrial support, it’s literally: you don’t have the batteries to make this go. You’re not going to the have optimal ability to make and maintain synapses. I should add, by the way, the people who respond with this approach—when you’re actually addressing the underlying causes of the problem—sustain their improvement. Whereas when you use a monotherapy, you may get a little bump and go right back to declining again.
DrMR: Interesting. And with the assessment that you’re doing, are you doing some type of mitochondrial testing? Are you doing this more subjectively, based upon symptoms?
DrDB: Great point. As you know, there’s no perfect way to assess mitochondria right now, so people look at things like organic acids. Most of us don’t want to have a muscle biopsy to evaluate our mitochondria.
We’re just starting to interact with a metabolomics group that is specialized in that and can give us a much better look at what’s going on with mitochondrial support. There are all sorts of indirect ways to get at that, but there hasn’t been a simple clinical test where you can check off, “Hey, while you’re checking the sodium and potassium, please check the mitochondria.”
DrMR: Sure. Is the mito swab test something that’s come across your radar screen?
DrDB: Yeah, it has, and we’ll see if that turns out to be the best thing or not. I think at this point, it still needs more support to determine whether it’s going to be the right way to go or not. I certainly hope it does, because I think the potential is tremendous.
DrMR: I share your hope there.
Sponsored Resources
DrMR:Hi, everyone. Let’s talk about bone broth and probiotics, both of which helped to make this podcast possible. Functional Medicine Formulations contains a line of probiotics that I personally developed, and I’m super excited to be able to offer you the same probiotics that I’ve been using in the clinic for years and are a byproduct of an extensive review of the literature plus my own clinical experience.
In this line, you will find my favorite three probiotics in all three of the main categories that work synergistically to help you fight biosis, like SIBO, candida yeast, and H. pylori, help to eradicate parasites, help to reduce leaky gut and repair the gut barrier, and can improve gas, bloating, diarrhea, constipation, and may even improve mood, skin, sleep, and thyroid function because of the far-reaching impact of the gut. You can learn more about these at drruscio.com/probiotics.
I’d also like to thank Kettle & Fire, who makes one of my favorite bone broths. Now, you’ve probably heard that bone broth can help via a variety of mechanisms, by helping to repair your gut, by soothing inflammation and repairing joints, by nourishing your hair, skin, and nails and having this almost anti-aging effect, and this is in part because bone broth is very nutrient rich, and especially Kettle & Fire bone broth, which uses non-GMO, organic, and free-range ingredients, and they really do have an excellent product.
Now, if you go to kettleandfire.com/drruscio, they are going to offer our audience 15% off and free shipping on any orders of six cartons or more, so definitely check them out at kettleandfire.com/drruscio.
Mast Cell Activation Disorder and Alzheimer’s
DrMR:Coming back to something gut-related for a minute—I’m not sure if you’ve seen much of this—but in my realm, where I look at a lot of gut disorders, histamine intolerance has been shown to increase in prevalence when people have IBS. And one of the manifestations of histamine intolerance is this foggy cognition. Is this something that you’ve seen much in your work?
DrDB: Yes. Not only that, but as you know, when you look at people with cognitive decline, it is really surprising how many people have Mast Cell Activation Disorder (MCAD). There’s a wonderful website started by Julie G. and her colleagues, that’s called ApoE4.Info. As you probably know, if you have zero copies of ApoE4, which is about 240 million Americans, your chance of getting Alzheimer’s during your lifetime is about 9%. If you have a single copy, it’s about 30% (about 80 million Americans). If you have two copies, and that’s over seven million Americans, you’ve got over a 50% chance. Most likely you will develop Alzheimer’s during your lifetime.

It’s very high-risk and important. So they started a website. These people are doing protocols that we’ve discussed. In fact, a surprising number of them turn out to have MCAD. There is something about the alteration, whether it is gut-related, primarily histamine-related, more related to immune changes. This seems to be a part of the overall phenomenon that we call Alzheimer’s, where you have a chronic activation of your innate immune system. And really, the amyloid that is made is simply part of the innate immune system response.
DrMR: Just for our audience, quick side note here, (I’m not sure if we’ve discussed this study previously yet) there was one study looking at histamine-intolerant individuals. They found that you only need to be histamine-avoidant about 70% of the time to see the benefits of a low histamine diet. So you don’t have to be totally perfect. And they did document an increased ability to secrete the diamine oxidase enzyme that breaks down histamine after adhering to a low histamine diet for a few months.
So there may be this ability to repair the gut enzyme secretion that can help with this. Some good news there. It’s not, apparently, a life sentence.
DrDB: Yeah, fantastic.
ApoE4: a Risk Factor
DrMR: You mentioned ApoE. I’ve been watching some of the gene research and it seems that there’s a lot here, at least from my vantage point, that needs to be sorted out. With ApoE, there seems to be the one camp that thinks you should really avoid fat. Then another camp would purport that you should be more ketogenic. Those seem to be, obviously, contradictory to one another. Is there a nuance here that I’m missing? Or how do you navigate this?
DrDB: There is some controversy. So to set the stage here, there are over 100 different genes that have relation to your risk for Alzheimer’s. However, the dominant one, the most common one, is ApoE4. ApoE is a really interesting gene. It appears with hominids. So the simians have a different ApoE… essentially a chimp ApoE.
If you look at all the changes that were made between the simians and the hominids, it’s actually, as you know, a relatively small number. When I told my wife, who’s an integrative practitioner, that, “Hey, my DNA as a whole is more similar to a male chimp’s than it is to yours,” she said, “Well, duh.”

The bottom line is, we’re very similar to the simians. Of those few changes that occur, the surprise is that many of them were related to a pro-inflammatory status. Why would that be? It’s been suggested by Tuck Finch from USC (and I think he’s absolutely on the right track) that what it took to come down out of the trees and walk the savannah, where you’re puncturing your feet, you’re fighting for your food and with your brethren, you’re eating raw meat and digesting all these microbes, is a proinflammatory state. It helps you in that scenario where you are changing niches.
So initially, and for 96% of hominid evolution, we’ve all been ApoE4 homozygous. It’s just been in the last 220,000 years that ApoE3 appeared, which is now the most common one. I’m a 33 and most people in this country are 33s. About three-quarters of us are ApoE4 negative.
ApoE4 has a pro-inflammatory effect. Literally, you are protecting yourself. But over time, because of this pro-inflammatory effect, you also have increased risk for cardiovascular disease and increased risk for cognitive decline, for Alzheimer’s disease. So it’s a trade-off. You do better with ApoE4 if you’re living in the Third World with squalid conditions, because you are protecting yourself.
Here’s the thing with the fat. You also absorb fat better when you have ApoE4. You can go longer without food. So, we usually recommend 12 to 14 hours fasting after dinner for ApoE4 negatives, and 14 to 16 hours for ApoE positives. When you eat, yes, if you’re eating a lot of saturated fat and also eating simple carbs, you’re really putting yourself at risk. But if you have good fats and if you keep the carbs to a minimum, you actually do quite well.
So what we recommend is a plant-rich, high fat, low-carbohydrate, medium protein diet. We call this Ketoflex 12/3, and it has the fasting periods with it. As you know, following total cholesterol is not very helpful. You want to follow either your sdLDL, your oxidized LDL, or your LDL particle number. When you first start out, you can use things like MCT oil. But after a few months, you get your insulin sensitivity back. Now you want to switch over to more polyunsaturated, to extra virgin olive oil, etc. This is discussed, by the way, both in the book and extensively on the website, ApoE4.Info.
With that, you can have a plant-based, plant-rich, high-fat diet without getting yourself into problems with lipidology, basically.
DrMR: And so, you are recommending a limitation on saturated fat in this group?

DrDB: What we’re recommending is: follow your numbers. You want to get the best of both worlds. You want to be able to get into ketosis, but once you’re able to do that, you want to then follow your LDL particle number and keep it below a thousand. Therefore, if you’re at 700, fine, you can have MCT oil. If you’re too high, you want to use things like ketone salts or ketone esters. Or hopefully you’re able to generate it endogenously. In other words, you want to balance these and get the best of both worlds.
DrMR: Gotcha. And it’s interesting: I talk about this in my book regarding autoimmunity, where the genes that were more befitting to help you fight infection a long time ago are likely now a liability. So for some people who have autoimmune conditions, who have this strong inflammatory response, you may have had better genes that would have kept you alive if we were alive 400, 500, or more years ago. But nowadays, in our environment, they may be a liability.
DrDB: Absolutely. And by the way, that’s exactly what’s seen with ApoE4. You have a stronger and quicker inflammatory response, which can help you under one set of circumstances but can harm you under another set of circumstances. If you’re ApoE4 negative, you tend to be less hyperreactive in general. So it may help you, but it also may hurt you if you’re in a scenario where you’re trying to deal with pathogens.
DrMR: Has it been examined if there’s a higher incidence of autoimmunity in the ApoE4 genotype?
DrDB: Yes. Again, there’s a little difference in terms of the adaptive versus innate. But in general, there is a stronger and more lasting pro-inflammatory response in the ApoE4 positives.
DrMR: Interesting, okay.
The Microbiome and Alzheimer’s
So you talked about infection. I’m assuming you are delineating between gut infection and other blood-borne infections, or Lyme and Lyme co-infection. Can you give us the high-level overview in terms of how you’re looking at gut infections (if you’re looking at them), compared to these other infections? And then some details in terms of how you’re handling those?
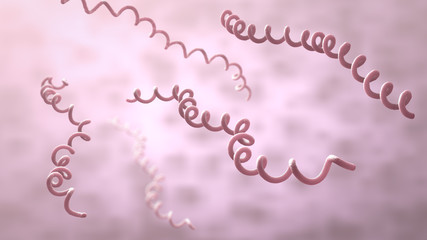
DrDB: Absolutely. First, one of the interesting findings is: numerous labs have published that if you look in the brains of patients with Alzheimer’s disease, you find microbes. That’s been P. gingivalis from the mouth, it’s been HSV-1, HHV, candida, and other fungi. There are all sorts of different things. And of course, Borrelia. All of these things.
If you look at where these things come from, many are coming from the oral cavity, from the lips, from the sinuses. So there’s that proximity. But there are also, as you indicated, blood-borne infections, such as Borrelia and other tick-borne illnesses, which can be seen in the brain. So there is this response.
The gut is a different scenario to some extent, as you know. You’re not talking so much about an infection as you are about a microbiome change and about a structural change (if you’ve got leaky gut or not). You’re now talking not just about organisms, but things like LPS, food particles, food sensitivities, fragments, and all these sorts of things you have to deal with. Barriers turn out to be absolutely critical. Again, this goes back to the idea that what Alzheimer’s is all about is about a protection against onslaught from all these various insults.
No question, the gut is an important site, not only for Alzheimer’s, but for things like Parkinson’s. Excellent data on that point as well. Having a gut that is not leaky, having an optimal microbiome, is really critical. There are some very nice studies published on the difference in microbiomes between patients with Alzheimer’s and patients without Alzheimer’s, and also the effect on optimizing the microbiome.
So these are all critical players in this response we call Alzheimer’s disease.
DrMR: And coming back to Lyme for a minute, one of the things that’s challenging is getting a definitive diagnosis. I understand that in a fairer aspect of medicine, black and white diagnoses are very hard to come by. You have to look at the patient, their family history, their history, their symptoms, all the relevant context, weigh that against the lab results and make the best-informed decision that you can. But have you found any testing to be particularly helpful for Lyme and the Lyme co-infections?
DrDB: That’s a great point. And this is an area of controversy. There are people who just focus on that one issue and treating Lyme disease and its other co-infections.

Some of the PCR urine tests I think are ultimately going to be helpful. There have been complaints recently that they have been perhaps giving too many false-positives. So I don’t know that currently they’re the best way to go, but I think, theoretically, they look like they should be the best way to go. No surprise, you’re going to find that a lot of people have these things and they’re doing just fine. Again, our concept of what an infection is has changed so much in the last couple of decades.
The second thing is, IGeneX has a very good panel. It’s a good panel, not only for Borrelia, but for other co-infections like Bartonella, Babesia, etc. That may be the best thing going currently. Then, of course, there are all sorts of other tests that can be used for Borrelia.
And you’re right, it is tough to know. Again, this is not like the old idea, do you have pneumococcus or do you not have pneumococcus? These are things that are chronically present, can be there for years, can be sequestered. You’re literally fighting a cold war with these things. So you’ve got to decide, is this the thing that is contributing importantly to the chronic illness I’m trying to improve?
Defining Protocols for SIBO and Lyme
DrMR: Right. That’s actually a nice transition into a thought I wanted to add for the audience here. And this is by no way definitive. This is my best proposal based upon what we know: sometimes it’s helpful to proceed via a process of elimination. Because there may not be any way, as we’re suggesting, to really definitively say yes or no, you have Lyme or you have a Lyme co-infection. Rather, we can work through this in a hierarchical fashion. This was posed by Farshid Rahbar, who was a gastroenterologist focusing on SIBO, but also looking at the SIBO-Lyme connection. If you’re suspecting both, start with the gut and then reevaluate, because your patient may have a more robust immune response if you optimize gut health before you go to the Lyme treatments. Any thoughts on that?

DrDB: Absolutely, and I agree. One of the ideas here is, with programs, we’re now getting to a situation where the treatment is relatively complex. So you can’t do everything at once and you really don’t want to do everything at once. For example, we often see people who will have very low hormone, of one or another kind. As you begin to treat them, as they begin to become healthier, on their own they will optimize their hormones. You don’t need to give them hormones. And this has certainly been pointed out by Ritchie Shoemaker in CIRS patients as well, for example.
So I agree with you. This is part of the whole idea of removal, resilience, and rebuilding. You want to remove what’s causing the problem and then you want to make people resilient. And you could argue that the most important thing for resilience is gut health.
DrMR: Yeah, I would certainly agree with you there. I always try to paint a kind of hierarchy for the patient. I think the challenge on the patient end is, you see a Lyme guy, a mold guy, and a gut guy and they’re all going to tell you, “Yeah, that’s the thing.”
DrDB: Yep.
DrMR: So if you have a hierarchy, you can say, “I’ll listen to the gut guy first and then maybe the Lyme guy second and then the mold guy third,” or whatever. Some process of elimination that patients can use to codify these things.
DrDB: Absolutely. In the recent book by Neil Nathan, Toxic: Heal Your Body (which I thought was a very good book), he talks about biotoxins. He talks about this issue of having multiple problems, and how you decide the most important one to go after.
Of course in a practical sense, it’s the thing that’s going to make the patient better. How can you get at the right thing? His point was, look, if they’ve got three different organisms, but one of them is the dominant problem, you need to go after that one.
DrMR: Right. And sometimes the hardest thing is figuring out which one that is.
DrDB: Absolutely.
DrMR: It’s trying to organize these things in the most efficient manner so you can try to get your dominoes falling in the right order.
Female Hormones and Alzheimer’s
I remember seeing some research about hormones years ago: that women who were not put on hormone replacement therapy when they had a surgically or hysterectomy-induced menopause had this cascade of brain inflammation which was bad for their cognition.
I’m curious on that. Also, just applying some of my clinical experience, I have seen very nice results in women who have gut imbalances—because that’s predominantly who I see—but who are also exhibiting subjective symptoms of female hormone imbalances, when I give them herbs like dong quai and black cohosh. I’ve seen very nice improvements in their cognition, premenstrual irritability, anger, brain fog, and what have you. And we know that estrogen and progesterone both affect various neurotransmitters.
So I’m curious here to know what you think about the female hormone piece and how this interfaces in what you do therapeutically.
DrDB: Yeah, absolutely. It’s a very, very important area. The work that you alluded to… very nice work out of the Mayo Clinic showing that people who basically had TAH-BSOs, or who had oophorectomies at the age of 40 or younger without hormone replacement, doubled their risk for Alzheimer’s. Even though the Alzheimer’s was coming on years later, they actually doubled their risk.

Again, this fits perfectly with what we found in the lab. You have a system that is looking at the support, and you’ve got to support it with appropriate trophic factors, BDNF, NGF, nutrients and hormones. You need all of the above.
You remove that and you’re literally changing that switch. You’re changing the likelihood of developing cognitive decline. You could interestingly trace from estradiol to its receptor. It turns on hundreds of different genes. And it actually increases the gene that takes your APP and prevents you from making amyloid out of it, which is the alpha secretase.
You can trace a direct path from estradiol to an anti-Alzheimer’s effect. So, no big surprise that if you provide this—if you’ve got enough of it and you don’t have a sudden drop in it—you’re going to do much better.
Now unfortunately, the WHI study that came out about 15 years ago really changed the landscape. Everybody was very afraid to give these things, like: “Oh, my gosh, we’ve got to get away from these.” I think it really muddied the waters. The reality is—we’ve had a lot of interaction with Dr. Anne Hathaway who’s a real expert in the area of BHRT—there’s no question that support for your neural system, done in the right way at the right time, is very helpful.
DrMR: Now, does she have any experience or thoughts on some of these herbs that work to help to increase or decrease your estrogen receptor sensitivity, instead of modulating your hormone levels, like the dong quai and black cohosh?
DrDB: Yeah, and I know certainly Sara Gottfried has written extensively about this… that there’s a lot you can do without actually providing the hormones. Again, it depends on where you stand. Are you able to make them endogenously with some help from these various approaches (the chaste berry and so on, for progesterone)? There are all sorts of ways you can go.
I always think it’s better to start that way. If you can get away without writing prescriptions for hormones, you’re probably going to be better off. For one thing, you may not suffer some of the negative effects. On the other hand, you have to remember, when someone comes in with cognitive decline and you determine that they are either at pre-Alzheimer’s or early Alzheimer’s, either you’re going to help them or they’re going to die.
So this is a really important time, and you really need to pull out all the stops. If it requires giving and including BHRT, then we think, “Okay, it’s better than a nursing home.”
DrMR: Completely agreed. And at least in my experience, I think the good news here is—and I modeled this from some of the research looking at estrogen receptors and receptor modulating herbs—you only need two to three cycles or months in a cycling female for these to take full effect. So you don’t need months and months. You need a couple cycles. Then usually what I do in the clinic is, if we’re not seeing marked improvements in these symptoms after a few months, we’ll go to something like a cream that has the actual hormones in them.
DrDB: Yeah, that’s a great way to do it.
DrMR: And I’ll mention for women who are not cycling, (at least in my opinion) based upon the mechanism of the chaste tree, you’re not going to get the progesterone response. The chaste tree helps to facilitate the action of dopamine in the brain, and that helps signal the LH that leads to the progesterone production. So for postmenopausal women, in my opinion, the chaste tree is probably not a viable option.
View Dr. Ruscio’s Additional Resources
Male Hormones and Alzheimer’s
What about men? One of the things that you see a lot more now on these commercials is, “Are you a guy who is unhappy? Could just be a number. Could just be low T.”
DrDB: Right.
DrMR: I do think there is something to that. But unfortunately I think it’s now a scapegoat for men who aren’t eating well, aren’t taking care of themselves, and they think they can just pave over that with testosterone. So I do think there’s something there, but I want to be careful not to lean on that too strongly.

Do you have a certain age gradient for what a healthy testosterone level should be? And how are you grappling with this one?
DrDB: Yeah, really good point. Again, this is the difference between 20th century medicine, which says, “What prescription can I write to avoid nature and try to make you able to continue doing all the wrong things and not get at what’s causing the disease?” and 21st century medicine, which says, “Why do you have this problem?”
If you are in the lowest quintile of testosterone levels, you have a much higher likelihood of developing cognitive decline and Alzheimer’s than if you’re in the highest quintile. There’s no question there’s a relation and no question that testosterone supports that neural network.
We do like to see testosterone levels up around 500 or more. If a person’s got early Alzheimer’s and their testosterone is 250, we are concerned about that. That is a suboptimal testosterone. We’re not trying to make you go out and get into fights, but we’d like to give you enough to support your neural network and an optimal neural network.
So we like to look at that, but we like to understand why. Is this because, as you indicated, you’re doing all the wrong things? As Dr. Shoemaker pointed out, if you are exposed chronically to mycotoxins, you are going to have HPA axis dysfunction, which will often include low testosterone.
We like to understand first what’s creating the problem. It can be, as you say, very poor lifestyle. You can fix all those things. Beyond that though, if you need some support, fine. The goal here, again, is to prevent you from dying of Alzheimer’s, to keep you out of a nursing home and to keep your cognition optimal.
Is Mercury a Common Cause?
DrMR: Yep, well said. Coming to mercury… this is one of many controversial issues.
DrDB: Yeah.

DrMR: I do think there’s a challenging balance here to be struck. When I spent some time going through the evidence on mercury—only mercury, I can’t say I looked at other of the heavy metals—it did seem that the majority of the evidence did not correlate mercury exposure.
There have been some fairly elegant studies done trying to correlate for every filling that you have: if you have two compared to four, six, eight, did that correlate in any way, in a dose response, to any morbidity or mortality endpoint? Really, in many of these large population-based studies, there did not seem to be this correlation. However, there does seem to be a smaller subset of people who may have an immune response to mercury, where they may be what we could loosely term a hyper-responder.
Firstly, would you agree with that posit? And do you think we need to be cautious not to say mercury is a problem for everyone, but there’s a nuance in terms of a smaller subset this may be a problem for? Or how do you navigate this? Because this is another challenging thing. I’m sure if many people in the audience did the right kind of provoked urine test, they’d all come back high. But who out of those people actually would have a problem?
DrDB: Yeah, that’s a really good point. And you said the most important words, which are smaller subset. So when you do these big population-based studies, you have an underlying assumption there which is incorrect. Which is that this is one disease and it’s all being caused by the same thing. So you’re looking for an effect on the group.
If 1% of the group has a mercury problem, another percent of the group has a Vitamin D problem, and another percent of the group has a mycotoxin problem, you’re not going to see any of them in this large population study. So you’re going to conclude that none of these things causes the problem, when in fact they all can contribute.
The acid test with mercury (and for all of these things) is, when you change that parameter, do people get better? There are a number of people that do clearly get better when you reduce their mercury levels. On the other hand, as you indicated, you can find mercury in all of us if you provoke it. We’ve got it in our bones, we’ve got it in our brains. It is being sequestered, as so many of these toxins are, until you begin to lose this and then essentially re-secrete it. This is the concern at the time of menopause: you’re now changing your osteoclastic to osteoblastic signaling and you’re re-releasing these sequestered toxins like mercury.

I find it helpful to understand whether someone has a high inorganic versus organic, and then to look and see what is actually causing this. It may be fish consumption. With the amalgams, you’re right: there are a lot of us who can have dental amalgams and never leak much of that into our blood. There are others who will get a chipped tooth or something they don’t even know about, and they’re now a bigger releaser. And as you indicated, there are people who are quite insensitive to this and people who are quite sensitive to it.
Unfortunately, I think it is a fundamental problem to say this is or isn’t a problem. For certain individuals, it’s clearly a problem and dealing with it makes them better. For others, it doesn’t seem to be a problem.
DrMR: Is it fair to say that if we’re building this loose hierarchy for people, we would put this a little bit lower in the hierarchy than some other things, like gut health, diets, exercise?
DrDB: Yes. Again, unless you find in the analysis, in the evaluation, that they have very little else that’s abnormal and they have a very high mercury. Then you want to focus in on that. Otherwise, you wouldn’t worry about it as much. You also, of course, want to know about their detox ability. Where do they stand with their liver/kidney function? Where do they stand with the various markers from GGT to glutathione, to ALT, AST, and all these things? Are you set up to be a good detoxifier, or not?
DrMR: Okay. And then one devil’s advocate question, because I know people in the audience will probably be asking some of our sharper clinicians. There was one study that was essentially a placebo versus control, a sham detox versus an actual detox of mercury. All patients reported benefit in the symptoms that were assessed. Sometimes this can be challenging to adjudicate an actual response to a placebo. When you say people respond, have you tracked this in some non-subjective way that can show benefit, like in the inflammatory markers?
DrDB: Yeah. The main thing is just ability to go back to work. You’re right, if you can get away with that as a placebo effect, hallelujah. But people improve their MoCA scores, they can interact better. You’re right, we need to have a study with all of the people who have responded in this way, to say, “Okay, was the response five points on average on the MoCA score? Was it something else?”
So yes, you could play devil’s advocate and say, “Well, could this be a placebo response?” It’s possible. I think you can’t exclude it without further studies. But to get those studies done is challenging. I know firsthand because since 2011 we’ve been trying to do a programmatic approach to cognitive decline. And the response from the IRBs has been, “We’re not going to let you do this, because we want you to do a single variable study.” The problem is, that assumes that physiology works in a way that it does not. We know that multiple things contribute to these chronic illnesses.
DrMR: Yeah, I’m learning your pain there, because we’ve been having a heck of a time with just a natural count that we’re trying to get through IRB approval. In this case, similar but different: the IRB board is not very up to speed with herbal medicine. So they’re having a very hard time approving almost anything, even though it’s a fairly innocuous compound, because it’s different than what they’re used to.
DrDB: There really does need to be a functional medicine IRB. And to my knowledge, there isn’t one in existence yet.
DrMR: That would be fantastic if there was one. It would make both of our lives a lot easier.
Episode Wrap-Up
All right, Dale. I want to be respectful of your time here. We went a little longer than we planned, but it was a fantastically rich conversation and I really appreciate it. Are there any closing thoughts that you have for people? And where would you like to point them in terms of a website, a book, or a program, or anything like that?
DrDB: Sure. So I think the closing here is, working together, we can reduce the global burden of cognitive decline, the global burden of dementia. The reality is, this should be a rare disease. Please get things checked out as early as possible. Don’t wait, because: better results earlier on.
As far as more information, you can look at The End of Alzheimer’s, which was published last year. That’s available from Random House. You can go on Facebook to Dr. Dale Bredesen and drbredesen.com, any of those will give you more information. Also there is a course for practitioners on our protocol for reversing cognitive decline, which is available through Institute for Functional Medicine.
DrMR: Awesome. I’ve heard great things about that program, by the way. Dale, I love what you’re doing. Thank you again for taking the time. I really appreciate it.
DrDB: Thanks so much, Michael. Take care.
DrMR: You too.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.




Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!