Debate: Should You Test For SIBO with Gastroenterologist Leonard Weinstock
Some debates about small intestine bacterial overgrowth (SIBO) can take information out of context. A nuanced examination of relapse rates after Rifaximin, or breath test intervals, may spur a conclusion that SIBO treatments and tests just don’t work. Research disagrees over the extent to which antibiotics, herbal antimicrobials, probiotics, the low FODMAP diet, and other treatments impact SIBO. SIBO is a complex condition, and treating for the root cause is important. We discuss our clinical perspectives and the latest research on SIBO testing and treatment.
SIBO Testing
- SIBO testing can result in false positives
- Does not truly assess the condition of the small intestine
- Does not consistently correlate with symptoms
- Isn’t needed to guide treatment
- One could get the same results if a patient could not perform testing
SIBO & IBS
- SIBO is more common in those with IBS according to numerous studies and 2 meta-analyses
SIBO Diagnosis
- Is given readily and is often shrouded in fear
- Not everyone with SIBO positive testing will have symptoms or require treatment
- It is important to take notice of symptoms that are taking place outside of the gut
- Skin rashes, achy joints, hair loss, hives, weight loss
- It is important to take notice of symptoms that are taking place outside of the gut
SIBO Treatment
- 42-44% of patients will respond well to rifaximin (antibiotic approved for SIBO treatment)
- Of that percentage, a third of patients will stay in remission for over 18 weeks
- The underlying condition that is causing SIBO must be addressed or else relapse will be inevitable
- Studies have shown that a low FODMAP diet does improve symptoms of SIBO and IBS.
- There is little evidence that a low FODMAP diet decreases the diversity of microorganisms in the gut
- Probiotics can have an antimicrobial effect and can help to heal the gut lining
- Probiotics may not be for everyone
Where to learn more
In This Episode
Episode Intro … 00:00:40
SIBO Breath Test Accuracy … 00:03:22
Is SIBO Over-Diagnosed? … 00:13:22
Should the SIBO Breath Test Be Optional? … 00:22:33
Effectiveness of SIBO Treatments … 00:28:25
Treating the Causes of IBS … 00:40:40
Episode Wrap Up … 00:45:13

Download this Episode (right click link and ‘Save As’)
Episode Intro
Dr. Michael Ruscio, DC: Hey, everyone. Welcome to Dr. Ruscio Radio. This is Dr. Ruscio today with Dr. Leonard Weinstock, who has now been on the podcast three times. We are going to be talking about SIBO. What I would like to do is argue both sides of some contentious points in SIBO. Welcome to the show!
Dr. Leonard Weinstock: Thank you so much, Michael.
DrMR: It’s great to have you back. I’ve got to say that I’ve been continually impressed with the work that you do. You seem to be pushing hard, not only in your clinical practice, but also in publishing. I know you said before we got on the line here, it’s always a delicate balance maintaining your sanity, not being overworked, and still doing all that. But I want to say it’s definitely appreciated. I’m very impressed with some of the papers you published.
DrLW: Well, thank you very much. Appreciate it. The whole spectrum of interpreting, testing, and new ways of looking at irritable bowel syndrome has brought so many interesting facets to my practice. And the change in FDA drugs for irritable bowel syndrome with diarrhea since 2015 also makes it interesting, and makes us more effective. We just need an open mind out there—”we” meaning doctors, and in particular, medical doctors—and I know we’re going to be talking about some of these aspects. So, let’s talk about these things.
DrMR: Okay. I should mention for the audience, in case you haven’t heard from previous episodes: Leonard Weinstock is a conventional gastroenterologist, that’s his background and his training. Now he operates in what I would consider a really optimal blend of conventional training and holistic, or functional, medicine training.
We’ve always seen eye-to-eye, not being dogmatic or overzealous, so I thought we’d have a nice conversation. The inception of the idea was that I wanted to find someone to debate on SIBO. But the challenge was that I couldn’t find anyone to debate SIBO who actually knew the SIBO literature! So I figured, rather than debate, Leonard and I could have a friendly conversation doing point/counterpoint. We’ll probably flop back and forth on who’s talking about the pro-SIBO side and who’s arguing the anti-SIBO side.
SIBO Breath Test Accuracy
One of the things I wanted to start us off with was SIBO testing. There’s been criticism that the testing is inaccurate, perhaps due to false positives. Perhaps those false positives are due to rapid transient, among other things. What would you say to someone who says, “I don’t want to do a SIBO breath test because I’ve heard they’re inaccurate”?
DrLW: I’d say, realize that there is limitation to the sensitivity and the specificity. But if the test is strongly positive, it’s helpful. And it’s strongly positive, namely, with a very early peak and a steady rise over the 90 minutes (as opposed to the testing we see occasionally, where the numbers will be low and at the very end it’ll pop up and be positive… the suggestion is that it gets into the colon at that point). If you see the former results where the numbers show zero, 10, 40, 70, 90, that’s going to be a strongly positive test. And you can feel more confident to label someone as having SIBO.

DrMR: Yeah. I think that’s a really great point, and I want to reiterate that for our audience. I have noticed that looking at these tests too literally can be problematic. Allison Siebecker and I have discussed this previously also: a positive is not a positive is not a positive, especially if you’re looking at the machine printout. The machine printouts don’t seem to have caught up with the more contemporary time interval. They don’t clarify the interval you would use to say: “If you see a spike in gases within this time, I think 90 to 100 minutes is reasonable,” so that you can rest assured it’s positive. And as you’re alluding to, Lenny, if you see just a little bit of positivity at the end, that’s probably not SIBO.
DrLW: Correct.
DrMR: Or it’s unlikely. And this isn’t a black and white issue. I think for patients to know that detail can be very helpful, especially for the subgroup of people who only have this mild elevation at the very end of the test. But if you’re seeing high elevations in the early or mid time interval, and that persists, that tells you these results are more significant and more meaningful.
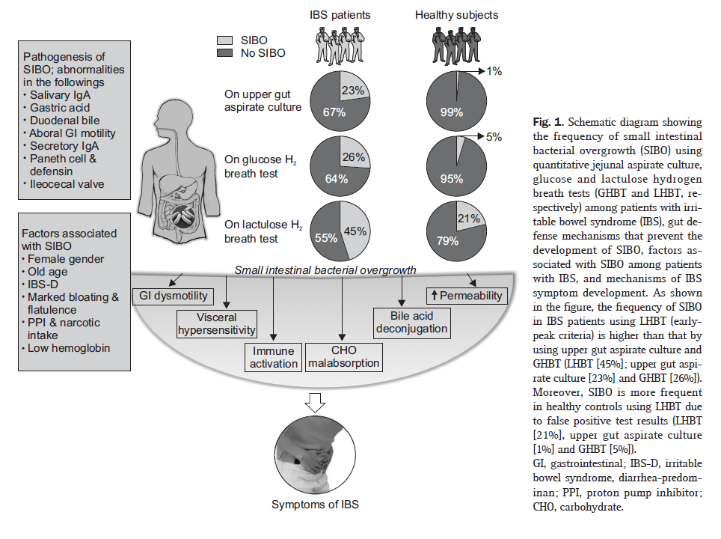
DrLW: Correct. Now, the breath test we talked about would use lactulose. There is a well-recognized IBS doctor in a university in a different state who only does glucose breath-testing. He knows that a positive test with glucose will be very specific. But it’s not sensitive. The problem with glucose is that when it’s done, it’s absorbed in the first three feet of the small intestine. So it only tests those first three feet (as opposed to all fifteen feet). With the glucose breath test, the likelihood that you’ll pick up a positive is less. But when it is positive, it’s definitely positive. So that’s yet another possibility.
And in the academic world, some of the testing is just wrong. They did a study that was bound to be abnormal, or different than the normal testing. They gave the lactulose with solid food, and looked at when that food got down to the colon. Well, the standard test is done fasting. So it’s a totally different test than the one that was used to show that testing with lactulose was a bad test. That was just wrong.
DrMR: This is a good point. Again, this is something that we’ve covered many times on the podcast. We want to make our decisions not based upon one test, but the total breadth of the evidence, and then look for what the totality of the evidence suggests.
Just one other point for anyone who may be newer to SIBO. There are essentially two breath tests that you can use: a lactulose test or a glucose test. You have to be more careful with the time interval that you interpret with the lactulose test because it has a higher incidence of false positives. But as Lenny was saying, with the glucose test, if you see a positive, you can rest much more assured that that positive is actually positive. These nuances are sometimes where people get really confused. I think it’s understandable, especially if people argue the merits of a test while cherry-picking one or two studies, rather than looking at the totality of the data.
What about the question, or the criticism, that SIBO breath-test results don’t correlate with symptoms?
DrLW: Well, I think the data at UCLA Cedars-Sinai show that they probably do. So if there’s methane, you’re going to have a component of constipation, whereas hydrogen only gives more bloating and diarrhea.
There’s another issue that’s coming up now: the ability to tag to hydrogen sulfide. Those patients with a rotten egg smell to their gas or urine or stool or breath can show up with positivity on hydrogen sulfide, on a new machine. Whereas before, we only guessed that it was abnormal if it was a total flat-line test, and patients recognized what a bad odor like rotten egg smelled like.
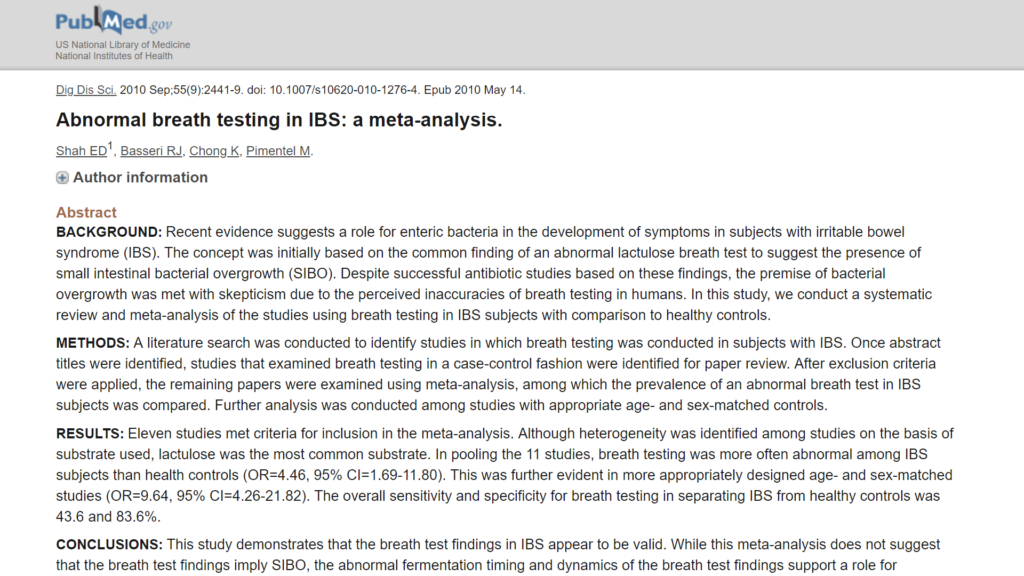
DrMR: There was a meta-analysis of 11 studies that found that breath testing was more often abnormal in IBS subjects than it was in healthy controls. Again, the same theme. You can find one study that shows a high false positive rate in healthy controls, so there are healthy controls that have nearly the same level of positivity as those with irritable bowel syndrome on the breath test. But if you look at what most of the data show, there seems to be the trend that, overall, patients with irritable bowel syndrome—with abdominal pain and altered bowel function, constipation, diarrhea, and oscillation between the two—seem to significantly more often be positive for SIBO than healthy controls.
DrLW: Right.
DrMR: What about the criticism of repeat SIBO breath-testing, saying it’s not needed to guide ongoing SIBO treatment?
DrLW: So, this is interesting. In preliminary work in Italy on breath-testing and efficacy of different antibiotics, they repeated the test. They showed good correlation with reversing the breath test and, let’s say, treating somebody who had irritable bowel. In another study, rosacea, when they reversed the breath test, it really made a difference.
In my own studies on restless leg syndrome, rosacea, and interstitial cystitis, I found that it just wasn’t very accurate. There were a lot of inconsistencies on that second test. So a lot of my patients ask, “Should I repeat the test as soon as I’m done?” And in my hands, it’s just not accurate, which makes you worry that the whole thing is inaccurate. You’re working on the basis of the first test, and if they get better, their test should get better. So I’m a little concerned and/or confused about these confounding results in my own work, versus the Italians.
DrMR: I would very strongly agree with that. There do seem to be some data showing that treatment does tend to correlate—I’m assuming it was from the Italian group, but I never checked the source—and the lab re-testing results tend to correlate with symptoms. So if someone’s feeling better symptomatically, it tends to correlate with the way their labs look. But I can’t say that’s an airtight case.
One systematic review posed the following on how to use the testing: use it at baseline to understand if you are dealing with SIBO. From there, proceed empirically. In other words, use the patient’s response to treatment to guide whether you continue treating, or stop treating. And that’s essentially what I’ve been doing in the clinic. Occasionally, we’ll do some re-testing. But I found once we have established the players on the board—maybe you find H. pylori, maybe SIBO— I tend to treat until we see a symptomatic resolution. Then potentially we do confirmatory re-testing. For H. pylori, I probably would be more prone to retest due to the potential detriment that it can pose. For SIBO, if someone is no longer symptomatic, I likely won’t re-test. It sounds, Lenny, like we’re doing a very similar algorithm there.
DrLW: Right. And for Helicobacter, you really have to confirm the eradication.
DrMR: Yeah.
DrLW: There’s too much resistance and, as you say, the risk of ulcer, cancer, or possibly extraintestinal manifestations of Helicobacter. You have to look.
Is SIBO Over-Diagnosed?
DrMR: Speaking of extraintestinal, I want to come to that relating to SIBO in a moment. But I wanted to first touch on SIBO diagnosis. We alluded to this earlier. I think it’s a valid criticism when people say that the SIBO diagnosis is handed out too readily and often with too much fear. I have some thoughts on this, but what’s your take here?

DrLW: Well, first of all, let’s just talk about SIBO as a diagnosis. It’s a condition. It’s not a be-all, end-all diagnosis. There are doctors who come back and tell the patients, “Well, I don’t know anything about SIBO,” or “Irritable bowel is not SIBO.” Let’s go back a couple of steps. Number one, there’s a chapter in every GI textbook about small intestinal bacterial overgrowth. Although in one of them it’s called small intestinal bacterial overgrowth syndrome. Basically, it’s a set of symptoms that could be caused by jejunal diverticulosis, blind loop, untreated celiac disease, chronic pancreatitis, altered immunity, altered neurological or muscular function of the gut, and newer explanations such as mast cell disease, that I’m finding. I’m working towards a publication on that.
But small intestinal bacterial overgrowth is simply a set of symptoms associated with a very black-and-white definition, with nutritional deficiencies. Conventional doctors have the problem that—though maybe they remember reading that chapter for their boards or reading for education—when it comes to irritable bowel, it’s just too fuzzy and gray. It really strikes at their training that irritable bowel could be hypersensitivity and stress, an abnormal brain-gut disorder, but not an infection, for instance. So, that’s where people who are trained in a very rigid way, who never wanted a change from the textbook, and/or never read newer material, are the naysayers. Those are the people who, if you really wanted a pro and con conversation, you should have gotten on the other side of this telephone.
DrMR: I’m not sure.
DrLW: But always I try to tell my physicians’ assistants, who are working with me, to look at SIBO as an explanation for symptoms. But when it comes to irritable bowel syndrome, the symptoms can be due to many different things. And vice versa, SIBO can be due to many different things. I think we should talk about: “What is a treatable cause for underlying disease states that cause SIBO?”
DrMR: Right, and IBS is probably the most common symptomatic manifestation associated with small intestinal bacterial overgrowth.
Now, there are data showing that even in healthy subjects, you will see positive findings for SIBO in some cases. So, I think we can make a case that not everyone who is positive for SIBO needs to be treated for SIBO.
But I think there’s a shade of gray here that should be colored in. And I’m curious about your thoughts on this, Lenny. If someone does not have IBS, if someone has no digestive symptoms and they test positive for SIBO, then I don’t think they would need to necessarily treat them. But we should also be considering, “Do they have other extraintestinal symptoms?” Joint pain, skin lesions of some sort, depression, brain fog? Because we do know, and you published some of this research, that treatment of SIBO can clear some of these extraintestinal symptomatic manifestations.
Maybe the best way to articulate this would be: if you find positive SIBO results in a totally healthy patient, then they probably don’t need to be treated. But if the patient has almost any type of symptom that has no other known cause, then at least a cautious trial of SIBO treatment seems warranted. Would you agree with that, modify that?

DrLW: Let me just modify it slightly. For our restless legs syndrome study, we looked at restless leg syndrome versus control. We also got a control group of 30 people who said they were completely healthy, they had no symptoms, they were not taking any medications. That’s hard to do, to find a totally healthy group. And 10%, 3 out of 30, had an abnormal breath test.
Now, maybe those were the three where they had just had a powerful wave, and the lactulose shot down to the colon and they were then positive. Every test you do in medicine is bound to have false positives and false negatives. It’s not like turning a coin over and having it be heads, or turning it over and it’s tails. You can’t just trust it because you can see it’s a head or a tail. No. Because medical testing is fraught with a variety of errors and changes, because of the test or the person.
Certainly, if the patient has no symptoms, why would they be breath-tested in the first place, unless they were seeking evaluation in a control group? But I agree with you: you wouldn’t treat them. But I do have patients with restless leg syndrome who have no GI symptoms, have a positive test, and their disease gets better with antibiotic therapy.
DrMR: I’ve seen a number of cases now with joint pain. Sometimes it’s idiopathic and undiagnosed joint pain, and sometimes it’s been diagnosed as rheumatoid arthritis, and where there’s not really much in the way of GI symptomatology. Their joint pain does respond quite nicely to herbal antimicrobial treatment.
Sponsored Resources
Hey, everyone. I’d like to thank two companies that can improve your health and have made this podcast possible.
Firstly, Platinum LED who sells perhaps the best red light therapy units on the market. Now, red light therapy can improve your health by stimulating mitochondria so you actually help to stimulate cellular energy, and the research here, while preliminary, has shown encouraging results for an array of applications, including thyroid, one very exciting study there; skin health; anti-aging; joint pain; and body composition.
Now, I’ve been doing an experiment with a Platinum LED unit at home for a few weeks now, and I have to say, so far, I am really liking it. I do feel like it is helping my skin look healthier and younger, which has been corroborated by a handful of clinical trials.
Now, importantly, in a direct side-by-side comparison, Platinum LED lights have produced the highest irradiance of any LED lights on the market. And this is the best part, all of their lights come with a 60-day trial period, so the risk is pretty much zero, and a full three-year warranty worldwide. Now, they are offering anyone from our audience a $50 off for select panels if you visit PlatinumTherapyLights.com, that’s PlatinumTherapyLights.com, and use the coupon code Ruscio50. So definitely check out Platinum LED.
Also, a thank you to GAINSwave, which this therapy can enhance sexual function. GAINSwave uses sound waves similar to ultrasound to stimulate angiogenesis or the growth of blood vessels and to break down plaques in existing blood vessels.
Now, GAINSwave has been shown to improve erectile function in men, according to med analyses. There have also been about 40 clinical trials looking at the efficacy of GAINSwave. I have done one full round with Dr. Judson Brandeis, who’s been on the podcast before, and I have been very happy with the results.
So if you’re a man wanting to enhance or improve your sexual function, I would definitely recommend checking out GAINSwave, and you can take advantage of one free GAINSwave therapy session if you go to GAINSwave.com/patient. And for medical professionals, you can learn more at joinGAINSwave.com/provider. GAINSwave, I would definitely check them out and also Platinum LED.
Should the SIBO Breath Test Be Optional?
Do you think you could do an equivalent job treating a patient with no SIBO breath testing, if you just had to do it empirically, compared to if you had the SIBO breath test?
DrLW: First of all, if you just go by the guidelines that the FDA approved, Xifaxan for IBS—of course, we suspect that 60% or so are going to be positive for SIBO—it’s totally legit to treat and observe for a response. If they fit the criteria for IBS-D, then it’s fine to treat empirically. Whether you want to do it with herbs or with an antibiotic, you have your choices. A small study is suggesting that one works as well as another, but herbs double the length. It’s certainly less than double the cost. Herbs can be used. I don’t have a wide follow-up data perspective on this. I’ll be interested if you have kept track. So, you don’t have to have the breath test.
But when we first looked at our numbers in 2006 (we first started doing breath testing in 2005), we predicted who would have an abnormal breath test on the basis of symptoms of bloating and flatulence. That was not good enough. It didn’t really delineate who was positive and who was negative. So although I’ll ask those questions, it’s not always going to be right. Definitely not.
DrMR: Agreed. And for our clinicians who subscribe to our clinicians’ newsletter, you’ll eventually see, peppered into the case studies that I publish monthly, that I’m now, in many cases, listing the SIBO breath test as optional. The reason I’m listing it as optional—especially if the patient is not going to have insurance coverage—is because I have a certain treatment algorithm I’ll run through in my head, and I would end up escalating to antimicrobial therapy even if they didn’t have SIBO, at some point. If they were otherwise not responsive or only partially responsive, I’m more concerned with continuing them through the treatment algorithm than I am with next treating their lab results.
There are a few simple justifications I use: they may be SIBO breath-test negative, but if we had the ability to test for small intestinal fungal overgrowth, they may have that. If we had the ability to test for hydrogen sulfide SIBO, they may have that. We don’t really know what the best treatments for those are, but I’m strongly suspicious that we’ll see a broad-spectrum herbal cocktail work well. Gastroenterologist Gerry Mullin published that an herbal antimicrobial cocktail could work as well as Rifaximin. Although that study wasn’t perfect, it established the precedent that they may have comparable effectiveness.
The other reason why I do it this way is—and I suspect for many integrative practitioners this is a problem that they’re not even aware of, and it could be quite pernicious—if you’re asking for a re-test of the breath test at the end of every round of treatment, I think that can cause a major problem with compliance. Patients don’t like doing the task. It’s not to say that they hate it, but certainly it’s a little bit of a pain. Especially if there’s not full insurance coverage. My suspicion is that the number of patients who vanish on you, for no known reason, would go down significantly if testing was less pervasive in your treatment algorithm. So that’s why I’ve been using the testing a little bit less.
Again, if you have a good algorithm in your mind that you proceed through and you’re listening to the patient, I’m fairly confident you can get there with or without the testing. But without the testing I think it’s a little bit more attractive for the patients.

DrLW: Some of my patients still really want the answer: “Do I have it or don’t I?” If they’re going to do a co-pay of $500, they especially want to know, “Do I have it? What are the odds that it’s going to help?” Now, a negative test is still not going to be saying no. I think the TARGET-3 study looked at a selected group of patients who did breath tests. Getting a positive response occurred in 20% of the negative patients on the breath test, and around 50-60% on the positive. So, if you don’t have the positive on the test, it doesn’t mean that you don’t have SIBO.
DrMR: Precisely, and that’s exactly the dialogue I have with my patients. When I list the test as optional for them, I’ll say, “If you’re very curious to know then we, by all means, can use the test. If you don’t really care, or if you don’t have insurance coverage and you’re trying to save the money, then we don’t need it.” I find that when you leave the decision partially open to the patient, it really helps keep the patient and the clinician on the same page.
Effectiveness of SIBO Treatments
What about the criticism that SIBO treatments don’t work? This has been levied, I think, most strongly against Rifaximin because of the relapse rates. Some have also criticized the low-FODMAP diet as potentially damaging the microbiota. So, why don’t we start with the Rifaximin and with the low-FODMAP diet and criticize?
DrLW: If you use Rifaximin just on the basis of symptoms, 42-44% of patients will respond well. Of that, a third will stay in remission of symptoms for over 18 weeks. If you don’t understand why somebody is antibiotic-responsive and why they relapse, then you’re just not getting it. It’s the chicken and the egg. The fact is—if you have a motility disorder, or a nutritional disorder, or stasis, or one of the 30 different causes for SIBO that’s causing IBS symptoms—if you don’t correct the underlying problem, you’re not gonna resolve the disorder and it’s gonna relapse. That’s fine, if you at least take away the idea, “Okay, I’m relapsing because I’m not treating the underlying disorder.”
So, are there disorders that are treatable, not only by the antibiotic to get rid of the excess bacteria, but with underlying therapy? And that would be, just offhand, pancreatic insufficiency, celiac disease, perhaps gluten sensitivity non-celiac disorder, wheat-sensitive gluten enteropathy.

What about the idea that probably the most common cause of IBS-D is an autoantibody condition with anti-vinculin that damages the nerves? If you can treat the motility disturbance with pro-motility medication, such as erythromycin, low-dose prucalopride, or maybe even naltrexone, you’re gonna get better results because you’re treating the underlying conditions.
These are the things that you have to be saying to a naysayer, who says, “Oh, they relapsed after two months, therefore, it’s not good therapy.” It’s just like treating somebody who’s got bronchiectasis of the bronchioles: if you can’t fix the abnormal bronchi of the lungs, you’re gonna get recurrent infections. You’ll do well with each treatment for a while until you get drug resistance (luckily with Rifaximin, you generally don’t get drug resistance), but you also have to think about treatment of the underlying condition, and that’s the success and that’s how people get better.
DrMR: Agreed. How do you feel about the extent of prolonging the response to, let’s say, Rifaximin, if someone is also addressing dietary and lifestyle factors? I don’t know of any data in this precise of a context, but say someone’s not exercising, and eating an unhealthy diet. There is evidence to show exercise can help with IBS, I just don’t know if it’s been used to potentiate the effects of Rifaximin. But it would seem pretty reasonable to posit that if someone started exercising, getting enough sleep if they weren’t previously, and cleaning up their diet, we’d increase the probability of remaining in remission for a longer period.
DrLW: Diet makes a big difference. Let’s say your own natural clearance of bacteria is 10% of what it should be. And you’re going wild at 7-11, and getting Slurpees and fructose loads. You’re making your bacteria grow, and they’re not going to get out, so you’re gonna relapse faster, even in the setting of having good effects from, let’s say, low-dose erythromycin. At least in my own work, that’s gonna keep you in remission for an average of a year and three months. As long as you’re not feeding the bacteria, your likelihood of staying in remission is longer. You’ll have a longer period of time without being affected by the infection. So I think diet does make a difference. We don’t know about exercise. Yes, exercise has been helpful, but maybe those are people for whom it’s the relaxation, it’s the positive mental attitude, that makes a difference.

DrMR: This is definitely a bit more speculative, but from this mechanism, I’m curious to see if any outcome data surface eventually. We do know, from Tarek Mazzawi’s group out in Norway, that the low-FODMAP diet seems to have the ability to increase serotonin cell density. And if you understand that serotonin both has a role in pain signaling, and also in motility regulation, it’s exciting to ponder what potential motility-healing impact a low-FODMAP diet may have. And potential to prolong time in remission. Any thoughts on that one?
DrLW: Not directly to that, but on the FODMAP diet: there was a study that showed improvement in diversity, and reduction in total histamine levels, which I think can play a big role in irritable bowel symptoms.
DrMR: Yeah. So definitely a theme here: if you’re using Rifaximin as a mono-therapeutic, it’s probably not going to be as strong of a treatment as if you were to use it in a more holistic manner, including, at the very least, diet.
Now, what about probiotics? This is a contentious issue regarding small intestinal bacterial overgrowth. Some will say you should not use probiotics, because they will make SIBO worse. I think the audience here has heard my thoughts, but how would you respond to that remark?
DrLW: There was a recent study for brain fog patients, that suggested they did worse on probiotics versus not. And these patients were doing worse because they had SIBO. It was a study by Satish Rao.
People always ask me, “Should I take probiotics before or while I’m taking Rifaximin for bacterial overgrowth.” And I say, “No. You may take it afterwards. It may or may not help. It may help the gut repair.” But while you’re taking the antibiotic, if anything, you want to cut down on the bacteria going into the small intestine.
View Dr. Ruscio’s Additional Resources
DrMR: What would your response be to the fact that probiotics have antimicrobial activity? I think the model that we have the best data for is really for H. Pylori. There’s been at least one meta-analysis showing that the co-administration of probiotics along with, I believe, triple therapy—or at very least antibiotic therapy for H. pylori—has shown a significant synergistic benefit.
I should also put a recent study on the board that probiotics to treat IBS showed better results in IBS patients with SIBO than in IBS patients without SIBO. Have you come across any of this?
DrLW: No, I haven’t seen that…

DrMR: My two cents. I thought that study was remarkable. We have also published three case studies of patients. They weren’t all with SIBO: I believe two of them were, included in our clinicians newsletter. We had them perform a SIBO breath test, and while they were waiting for the results to come in, we had them tweak their diet, and start on a probiotic. In all three of these cases, they were totally asymptomatic by the time they reported for their follow-up. So I think that the probiotics have a fairly potent antimicrobial stimulus that we don’t give enough appreciation to. That being said, I’m happy to change my mind on this.
I do think there’s not enough data to make a decision strongly one way or the other. So you can do it either way, but I’ve seen a number of lab findings. SIBO and candida are probably the most common that you’ll see: the patient reports back and the testers are interpreting the lab findings from four weeks ago. And the patient’s been on a probiotic cocktail for that three weeks post-collecting the testing, and now all of their symptoms are gone.
DrLW: Interesting. Well, it goes against some data. So you feel that the probiotics can kill some of the bad bacteria on the small intestine lining?
DrMR: Precisely.
DrLW: Or change the motility? Or help repair the gut to decrease the gut permeability problems?
DrMR: I’m thinking it’s a multi-fold mechanism, because we do know that probiotics are antibacterial, antifungal, and antiparasitic. Those data have been published. I wouldn’t say we have meta-analyses on a number of different bacteria. But there’s at least enough evidence to show that you can use something like an anti-worm agent next to a probiotic and show equivalent results. So there are some data that at least suggest this.
There’re also data showing the motility simulation in the reduction of leaky gut, using probiotics. So I’m thinking it’s probably multi-fold in terms of the mechanism that it propagates. But again, one of the things that I think is easy to forget about with probiotics (because it’s so counter-intuitive) is that probiotics actually do secrete antimicrobial peptides.
DrLW: Interesting. Okay, great.
DrMR: Maybe eventually I’ll pull you over to the dark side here, Lenny!
Treating the Causes of IBS
One or two final questions here. Do you think we’re better off treating IBS than treating SIBO? I know that may be a narrow question, but it’s been asked by some of the critics. Should focus on treating IBS—which could include something like Rifaximin, which is approved to treat IBS—rather than treating SIBO? Do you draw any kind of line there?
DrLW: Wow. That’s an interesting question. Just so I’m not confused: do you say, “Let’s treat the pain or the symptoms of the disorder,” or try to treat the underlying disorder of irritable bowel syndrome?

DrMR: I don’t know, when that question’s been put forward, that there’s been a specific kind of treatment protocol attached to it. I’m assuming that what the questioners mean is, do you focus on using the established treatment for IBS—your antispasmodics, your antibiotics, any of your foundational and established treatments for IBS—rather than treating the SIBO? I suppose motility agents wouldn’t really fall in there unless they have constipation. So I’m giving you a bit of a vague answer.
DrLW: Okay, here’s a parable. If you want to hit the nail into the wood, you’re going to use a hammer. You’re not going to use the back of a screwdriver. I think if you’ve got a specific therapy for a problem, use the specific therapy. Treating symptomatically only gets you so far, and patients are not happy with it. Most patients who are treated in this manner have gone through 4.7 treatments and are unsatisfied 90% of the time. Those are the statistics. When Imodium or Lomotil, Bentyl, or other anticholinergic, but not really anti-spasm, medications were used, in four double-blind studies, it was only positive in one (at very high doses where you’re bound to get side effects). So always if possible, treat with the underlying problem treatment approach.
I think, whether you use a breath test or not, you’re looking for the antibiotic-responsive patient that suggests that SIBO is the underlying cause of irritable bowel syndrome. If that’s the case, go for it and go aggressively. If they’re not antibiotic-responsive, maybe that’s when you should use your breath test to say, “Okay, their breath test is definitely negative, so I’m gonna leave that scenario.” Or worry about other things like biofilm, or tougher treatment scenarios like small intestinal pseudo-obstruction or scleroderma, where it’s very hard to treat the patients with antibiotics. I think that’s the way you should frame it, rather than treat irritable bowel non-specifically. I think we should treat it specifically whenever possible.
DrMR: I agree with you. I think if one gives the research literature on IBS an honest look, there’ve been some great studies that have given number-needed-to-treat tables. You see that, oftentimes, the natural treatments for IBS work better than the pharmaceutical. And I think it’s because some of them are broad-spectrum in their effect. I’ll use probiotics as an example again. It has a number needed to treat of eight to nine, compared to Rifaximin which has a a number needed to treat of eleven. Now, it’s not always an apples-to-apples comparison when you’re using different studies and you’re comparing their number-needed-to-treat scores side by side.
This is a little bit different than the question I asked you and the answer that you gave, but I think many of the natural therapies are really well-positioned for IBS. I think that’s exciting, especially when we have conventional doctors like yourself, Lenny, who are willing to be open-minded and pull from both camps, with the goal of what’s best for the patient.
DrLW: Thank you.
Episode Wrap Up
DrMR: All right. That takes me through most of what I wanted to ask. Was there anything, as we move to a close here, that you feel is important to mention?
DrLW: Boy, I think of the scenario, your gastroenterologist just did your colonoscopy and said you’re normal, and there’s no treatment available. You have IBS-D. You can come back to the doctor and say, “Well, there are three FDA-approved drugs for irritable bowel syndrome. Can we go through them?” And it’s appropriate that you ask that question. The drugs that are thrown out at people are actually not FDA-approved. The Imodium, Lomotil, Bentyl, Levsin, and so forth: those are not FDA-approved.

FDA approval should mean something to physicians if they’re going to take a syndrome or a disease seriously, because the drug company has presented data, often at great expense, that proves that it’s better than placebo, and safe. And that means a lot when you’re treating patients. So rather than fly with something that they were taught in med school and residency years ago, and just are comfortable with the idea of handing out, it’s time to change. The patient can change doctors, or request specific things that are FDA-approved.
DrMR: Is there a certain order that you think is most logical to run through those in?
DrLW: Yeah, I do. I think doctors should find out who is antibiotic-responsive. Treatment with Rifaximin, and/or intermittent treatment with the antibiotic followed by pro-motility medication, makes the most sense to me to find out who’s going to be responsive to that. If they’re not responsive, in pain, and significant diarrhea is a problem, then eluxadoline is another reasonable option. If there’s very severe diarrhea, I reserve Lotronex for patients like that. If there’s an overlay, a big stress component, then relaxation therapy, yoga, hypnotherapy, and tricyclic antidepressants are all important things.
DrMR: Would you modify that if someone had predominantly constipation IBS?
DrLW: Sure. I wish there were more home runs with respect to Linzess, Trulance, and Amitiza, but those are FDA-approved drugs that can be very helpful. Certainly, if there’s a methane signal on the breath test, and bloating— especially bloating after meals and not just as the constipation gets worse—then I’d be willing to treat the methane, even though it’s tough to do.
DrMR: Well, Lenny, thank you for taking the time to speak to this. I hope, for the audience, this helps you navigate some of the nuances. Is there anywhere you’d want to point people to on the Internet, Lenny?
DrLW: I think Allison Siebecker’s sibo.info is great. That’s where we go.
DrMR: And you have your own website too?
DrLW: Yeah, I do: gidoctor.net.
DrMR: Okay. Cool. Well, thank you, sir. I appreciate you taking the time.
DrLW: You bet.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.




Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!