Stop the Struggle: How to Relieve the Symptoms of IBS Attacks
Treatment Options to Relieve and Prevent Symptoms of IBS Attacks
- Symptoms of IBS Attacks|
- Relieving Attacks|
- Preventing Attacks|
- Long-Term Treatment|
- Get a Handle on IBS|
If you have irritable bowel syndrome, you’ve likely experienced the symptoms of IBS attacks: stomach pain, bloating, extreme diarrhea or constipation. And that’s not all — fatigue [1, 2], depression and anxiety [3, 4, 5, 6], headaches [7, 8], and more can all be part of an IBS flare-up.
IBS is a common condition that can negatively affect one’s quality of life [9]. For many IBS patients, symptoms arrive in well-defined episodes, lasting, 2-5 days on average [10]. These episodes, or IBS attacks, interfere with work, family life, friends, and self-confidence.
The good news is there’s lots to be learned from recent IBS research, including strategies that can help you to reduce and even avoid symptoms of IBS attack. Read on to learn more about how to ease these symptoms and get your life back on track.

What Are the Symptoms of IBS Attacks?
Abdominal pain and altered bowel movements are the defining symptoms of an IBS attack. However, there are many other common symptoms that you may also experience during an IBS attack, including:
- Bloating [11]
- Cramping [12]
- Indigestion [13]
- Heartburn [13]
- Acid reflux [13]
- Flatulence (gas) [12]
- Rectal bleeding caused by altered bowel habits
IBS Affects More Than Just Your Digestive Tract

What’s not often discussed is that IBS symptoms can affect more than just your digestive system. For example:
- At least 50% of IBS patients struggle with fatigue [1].
- More than half of chronic fatigue patients also have IBS [2].
- Depression and/or anxiety is very common in IBS patients [3, 4, 5, 6, 14].
- Many IBS patients have pain symptoms, including migraine headaches , fibromyalgia pain, pelvic pain, and TMJ (lockjaw) jaw pain [2, 7].
How to Relieve the Symptoms of IBS Attacks
No matter which symptoms you experience during an IBS flare-up, you want to find relief quickly. There are a number of things you can do to relieve symptoms of IBS attack.
Keep in mind that every IBS patient is different, and what works for you may not work for someone else. Experiment with these approaches to find the combination of treatment options that brings you the most relief:
Treatments to Calm a Gut Flare Up
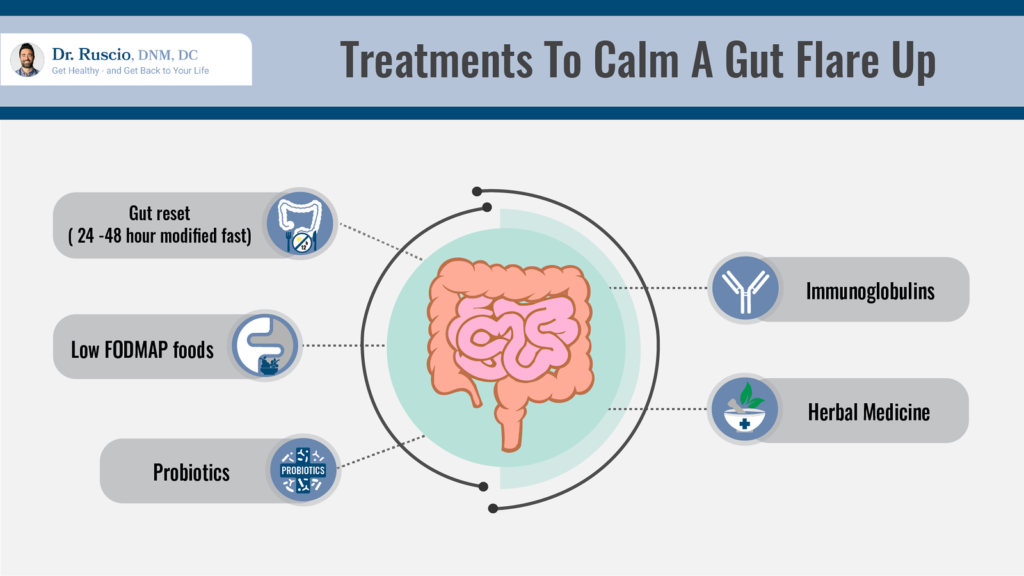
IBS flare-ups start in the gut, so it makes sense to treat the root cause of the problem. These treatment options are highly recommended for bringing the gut back into balance:
- Gut reset: A gut reset is a modified fast that allows your entire digestive tract to rest and repair. Just 24-48 hours of replacing meals with an elemental diet shake can significantly calm an IBS flare. Preliminary research suggests that fasting and eating elemental diets are effective treatments for IBS [15, 16].
- Low FODMAP foods: If you can’t do a gut reset, the next best choice is eating easy-to-digest meals that are low in fermentable carbohydrates, or low FODMAPs. Keep a few portions of low FODMAP soups in your freezer and have a few simple low FODMAP recipes that you can prepare if you’re not feeling well. This is a great way to be prepared for an IBS flare-up.
- Stress Reduction and Relaxation Techniques: stress and lack of sleep can be a common trigger for IBS symptoms. Research suggests that stress management techniques, including yoga [17], meditation [18], exercise [19], cognitive behavioral therapy [20, 21], and hypnotherapy [22, 23] can be helpful for IBS patients.
- Probiotics: Significant research evidence, including five meta-analyses (highest quality research evidence) [24, 25, 26, 27, 28], supports the use of probiotics for reducing IBS symptoms.
- Immunoglobulins: A relatively new supplement, immunoglobulins support the immune system by binding to and neutralizing bad bacteria in the gut. Clinical trials have shown that immunoglobulins improve IBS symptoms [29, 30, 31, 32, 33, 34, 35] and can be effective, even for IBS patients that don’t respond to other therapies [31].
- Herbal remedies: A number of herbal remedies can help with bloating and other digestive symptoms. Peppermint oil supplements, peppermint tea, or the herbal supplement Atrantil can help to soothe digestive symptoms.
Medication
Medication can be part of your plan for treating symptoms of IBS attack. However, most IBS medications simply provide symptom relief for digestive problems and do not address the cause of IBS flare-ups.
- For IBS with diarrhea, Imodium (loperamide) is an over-the-counter medication that relaxes the smooth muscles of the digestive system and can help to improve stool consistency and reduce the frequency of bowel movements. Prescription antidiarrheal medications for IBS include Viberzi (eluxadoline) and Lotronex (alosetron).
- For IBS with constipation, over-the-counter laxatives such as Glycolax, Miralax, or magnesium citrate can be very helpful. Fiber supplements may also be effective but can worsen symptoms for some. Choose low FODMAP sources of fiber such as ground flaxseeds or chia seeds.
- For headaches and body pain associated with an IBS attack, over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs) such as ibuprofen can provide relief. Long-term use of NSAIDs is not recommended due to side effects that can damage the gut, potentially worsening IBS symptoms.
Can IBS Attacks Be Prevented?

IBS is a set of symptoms rather than a disease. For decades, health care professionals did not know the cause of symptoms of irritable bowel syndrome. However, research is now shedding light on the many factors that can lead to IBS [36]. These include:
- Gut dysbiosis: Imbalances in the microorganisms of the gut [37], also known as gut dysbiosis, can be a result of poor diet, stress, antibiotic use, and other lifestyle factors [38].
- Post-infectious IBS: One study suggests that food poisoning (also known as gastroenteritis) may cause between 5% and 32% of IBS cases [39].
- SIBO: A meta-analysis of 50 clinical trials found SIBO (bacterial overgrowth in the small intestine) in more than one-third of the studied IBS patients [40].
- Leaky gut: Leaky gut has also been found in IBS patients [41, 42] and may be the reason for some IBS symptoms [43].
- Food intolerances: Non-celiac gluten intolerance [44], lactose intolerance [45], or intolerance to artificial additives or ingredients [46] can trigger IBS symptoms in some. Intolerance to high FODMAPs foods may increase bloating and abdominal pain [47].
- Brain-gut dysregulation: Another potential cause of IBS symptoms is alterations in normal brain-gut communications [48]. Low levels of serotonin, a chemical messenger involved in digestion, brain, and nervous system functions can affect bowel function and also may cause pain and mood disorders in IBS [49].
- Hypersensitivity to gas pressure: Many IBS patients are extremely sensitive to gas pressure. These patients feel the sensation of bloating even with normal levels of gas. Inflammation [50] or altered serotonin levels [51] may play a role in this hypersensitivity.
All of this research gives us much more insight into managing IBS symptoms. If you suffer from frequent IBS attacks, there are steps you can take to prevent IBS flare-ups and improve your quality of life.
Long-Term Treatment of IBS
There are a number of treatment options for IBS that can help you to improve your overall digestive health. Treatments for IBS may differ from other gastrointestinal disorders, so a clear diagnosis is important.
Confirm Your Diagnosis
IBS shares symptoms with other digestive conditions, including celiac disease and inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis.
Traditionally, invasive procedures such as colonoscopy and biopsy have been used to rule out IBD and celiac disease in IBS patients. Thankfully, a simple IBS blood test can now identify many IBS patients and can be used to distinguish IBS-D (IBS with diarrhea) and IBS-M (IBS with mixed diarrhea and constipation) from these other conditions.
Treatment Options
Long-term treatment of IBS is a step-by-step approach that should start with the most fundamental approaches.
For some patients, an anti-inflammatory diet, probiotics, and lifestyle changes are all that’s needed to get control of IBS symptoms. For patients who don’t respond fully to these fundamental steps, more targeted approaches are available, including a low FODMAP diet and antimicrobial treatments. Research shows that herbal antimicrobial treatments are as effective as standard antibiotic treatment with Rifaximin [52].
My book, Healthy Gut, Healthy You, provides an in-depth guide to better gut health. If you want personal guidance for your IBS treatment plan, consider making an appointment with a health coach or functional medicine practitioner at our clinic.
Get a Handle on IBS
There is much you can do to relieve symptoms of IBS attack.
While medication can be helpful for specific symptoms of an IBS flare-up, modified fasting or dietary changes, probiotics, targeted supplements, and stress reduction are more effective for bringing the gut back into balance.
If you experience frequent IBS attacks, getting on a path to better gut health can help you to prevent flare-ups and improve your quality of life.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Han CJ, Yang GS. Fatigue in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis of Pooled Frequency and Severity of Fatigue. Asian Nurs Res (Korean Soc Nurs Sci). 2016 Mar;10(1):1-10. doi: 10.1016/j.anr.2016.01.003. Epub 2016 Feb 1. PMID: 27021828.
- Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002 Apr;122(4):1140-56. doi: 10.1053/gast.2002.32392. PMID: 11910364.
- Tang YR, Yang WW, Liang ML, Xu XY, Wang MF, Lin L. Age-related symptom and life quality changes in women with irritable bowel syndrome. World J Gastroenterol. 2012 Dec 28;18(48):7175-83. doi: 10.3748/wjg.v18.i48.7175. PMID: 23326122; PMCID: PMC3544019.
- Sperber AD, Atzmon Y, Neumann L, Weisberg I, Shalit Y, Abu-Shakrah M, Fich A, Buskila D. Fibromyalgia in the irritable bowel syndrome: studies of prevalence and clinical implications. Am J Gastroenterol. 1999 Dec;94(12):3541-6. doi: 10.1111/j.1572-0241.1999.01643.x. PMID: 10606316.
- Hamilton WT, Gallagher AM, Thomas JM, White PD. Risk markers for both chronic fatigue and irritable bowel syndromes: a prospective case-control study in primary care. Psychol Med. 2009 Nov;39(11):1913-21. doi: 10.1017/S0033291709005601. Epub 2009 Apr 15. PMID: 19366500.
- Przekop P, Haviland MG, Zhao Y, Oda K, Morton KR, Fraser GE. Self-reported physical health, mental health, and comorbid diseases among women with irritable bowel syndrome, fibromyalgia, or both compared with healthy control respondents. J Am Osteopath Assoc. 2012 Nov;112(11):726-35. Erratum in: J Am Osteopath Assoc. 2013 Jan;113(1):15. PMID: 23139343; PMCID: PMC3542981.
- Cámara-Lemarroy CR, Rodriguez-Gutierrez R, Monreal-Robles R, Marfil-Rivera A. Gastrointestinal disorders associated with migraine: A comprehensive review. World J Gastroenterol. 2016 Sep 28;22(36):8149-60. doi: 10.3748/wjg.v22.i36.8149. PMID: 27688656; PMCID: PMC5037083.
- Arzani M, Jahromi SR, Ghorbani Z, Vahabizad F, Martelletti P, Ghaemi A, Sacco S, Togha M; School of Advanced Studies of the European Headache Federation (EHF-SAS). Gut-brain Axis and migraine headache: a comprehensive review. J Headache Pain. 2020 Feb 13;21(1):15. doi: 10.1186/s10194-020-1078-9. PMID: 32054443; PMCID: PMC7020496.
- Mönnikes H. Quality of life in patients with irritable bowel syndrome. J Clin Gastroenterol. 2011 Aug;45 Suppl:S98-101. doi: 10.1097/MCG.0b013e31821fbf44. PMID: 21666428.
- Palsson OS, Baggish J, Whitehead WE. Episodic nature of symptoms in irritable bowel syndrome. Am J Gastroenterol. 2014 Sep;109(9):1450-60. doi: 10.1038/ajg.2014.181. Epub 2014 Jul 1. PMID: 24980882.
- Enck P, Aziz Q, Barbara G, Farmer AD, Fukudo S, Mayer EA, Niesler B, Quigley EM, Rajilić-Stojanović M, Schemann M, Schwille-Kiuntke J, Simren M, Zipfel S, Spiller RC. Irritable bowel syndrome. Nat Rev Dis Primers. 2016 Mar 24;2:16014. doi: 10.1038/nrdp.2016.14. PMID: 27159638; PMCID: PMC5001845.
- Masuy I, Van Oudenhove L, Tack J, Biesiekierski JR. Effect of intragastric FODMAP infusion on upper gastrointestinal motility, gastrointestinal, and psychological symptoms in irritable bowel syndrome vs healthy controls. Neurogastroenterol Motil. 2018 Jan;30(1). doi: 10.1111/nmo.13167. Epub 2017 Aug 1. PMID: 28762592.
- de Bortoli N, Tolone S, Frazzoni M, Martinucci I, Sgherri G, Albano E, Ceccarelli L, Stasi C, Bellini M, Savarino V, Savarino EV, Marchi S. Gastroesophageal reflux disease, functional dyspepsia and irritable bowel syndrome: common overlapping gastrointestinal disorders. Ann Gastroenterol. 2018 Nov-Dec;31(6):639-648. doi: 10.20524/aog.2018.0314. Epub 2018 Sep 26. PMID: 30386113; PMCID: PMC6191868.
- Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016 Sep;44(6):592-600. doi: 10.1111/apt.13738. Epub 2016 Jul 22. PMID: 27444264.
- Kanazawa M, Fukudo S. Effects of fasting therapy on irritable bowel syndrome. Int J Behav Med. 2006;13(3):214-20. doi: 10.1207/s15327558ijbm1303_4. PMID: 17078771.
- Pimentel M, Constantino T, Kong Y, Bajwa M, Rezaei A, Park S. A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Dig Dis Sci. 2004 Jan;49(1):73-7. doi: 10.1023/b:ddas.0000011605.43979.e1. PMID: 14992438.
- Kavuri V, Raghuram N, Malamud A, Selvan SR. Irritable Bowel Syndrome: Yoga as Remedial Therapy. Evid Based Complement Alternat Med. 2015;2015:398156. doi: 10.1155/2015/398156. Epub 2015 May 6. PMID: 26064164; PMCID: PMC4438173.
- Shah K, Ramos-Garcia M, Bhavsar J, Lehrer P. Mind-body treatments of irritable bowel syndrome symptoms: An updated meta-analysis. Behav Res Ther. 2020 May;128:103462. doi: 10.1016/j.brat.2019.103462. Epub 2019 Nov 12. PMID: 32229334.
- Zhou C, Zhao E, Li Y, Jia Y, Li F. Exercise therapy of patients with irritable bowel syndrome: A systematic review of randomized controlled trials. Neurogastroenterol Motil. 2019 Feb;31(2):e13461. doi: 10.1111/nmo.13461. Epub 2018 Sep 19. PMID: 30232834.
- Zhao SR, Ni XM, Zhang XA, Tian H. Effect of cognitive behavior therapy combined with exercise intervention on the cognitive bias and coping styles of diarrhea-predominant irritable bowel syndrome patients. World J Clin Cases. 2019 Nov 6;7(21):3446-3462. doi: 10.12998/wjcc.v7.i21.3446. PMID: 31750328; PMCID: PMC6854400.
- Lackner JM, Jaccard J, Keefer L, Brenner DM, Firth RS, Gudleski GD, Hamilton FA, Katz LA, Krasner SS, Ma CX, Radziwon CD, Sitrin MD. Improvement in Gastrointestinal Symptoms After Cognitive Behavior Therapy for Refractory Irritable Bowel Syndrome. Gastroenterology. 2018 Jul;155(1):47-57. doi: 10.1053/j.gastro.2018.03.063. Epub 2018 Apr 25. Erratum in: Gastroenterology. 2018 Oct;155(4):1281. PMID: 29702118; PMCID: PMC6035059.
- Peters SL, Muir JG, Gibson PR. Review article: gut-directed hypnotherapy in the management of irritable bowel syndrome and inflammatory bowel disease. Aliment Pharmacol Ther. 2015 Jun;41(11):1104-15. doi: 10.1111/apt.13202. Epub 2015 Apr 10. PMID: 25858661.
- Miller V, Carruthers HR, Morris J, Hasan SS, Archbold S, Whorwell PJ. Hypnotherapy for irritable bowel syndrome: an audit of one thousand adult patients. Aliment Pharmacol Ther. 2015 May;41(9):844-55. doi: 10.1111/apt.13145. Epub 2015 Mar 4. PMID: 25736234.
- Yuan F, Ni H, Asche CV, Kim M, Walayat S, Ren J. Efficacy of Bifidobacterium infantis 35624 in patients with irritable bowel syndrome: a meta-analysis. Curr Med Res Opin. 2017 Jul;33(7):1191-1197. doi: 10.1080/03007995.2017.1292230. Epub 2017 Mar 7. PMID: 28166427.
- Tiequn B, Guanqun C, Shuo Z. Therapeutic effects of Lactobacillus in treating irritable bowel syndrome: a meta-analysis. Intern Med. 2015;54(3):243-9. doi: 10.2169/internalmedicine.54.2710. PMID: 25748731.
- McFarland LV, Dublin S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J Gastroenterol. 2008 May 7;14(17):2650-61. doi: 10.3748/wjg.14.2650. PMID: 18461650; PMCID: PMC2709042.
- Whelan K. Probiotics and prebiotics in the management of irritable bowel syndrome: a review of recent clinical trials and systematic reviews. Curr Opin Clin Nutr Metab Care. 2011 Nov;14(6):581-7. doi: 10.1097/MCO.0b013e32834b8082. PMID: 21892075.
- Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014 Oct;109(10):1547-61; quiz 1546, 1562. doi: 10.1038/ajg.2014.202. Epub 2014 Jul 29. PMID: 25070051.
- Wilson D, Evans M, Weaver E, Shaw AL, Klein GL. Evaluation of serum-derived bovine immunoglobulin protein isolate in subjects with diarrhea-predominant irritable bowel syndrome. Clin Med Insights Gastroenterol. 2013 Dec 5;6:49-60. doi: 10.4137/CGast.S13200. PMID: 24833942; PMCID: PMC4020402.
- Hilal, R. , Mitchell, P. , Guerra Jr., E. and Burnett, B. (2014) Case Series of 10 Drug-Refractory IBS Patients Who Respond to Oral Serum-Derived Bovine Immunoglobulin/Protein Isolate (SBI). Open Journal of Gastroenterology, 4, 321-328. doi: 10.4236/ojgas.2014.410046.
- Weinstock, L. and Jasion, V. (2014) Serum-Derived Bovine Immunoglobulin/Protein Isolate Therapy for Patients with Refractory Irritable Bowel Syndrome. Open Journal of Gastroenterology, 4, 329-334. doi: 10.4236/ojgas.2014.410047.
- Good L, Rosario R, Panas R. New therapeutic option for irritable bowel syndrome: serum-derived bovine immunoglobulin. World J Gastroenterol. 2015 Mar 21;21(11):3361-6. doi: 10.3748/wjg.v21.i11.3361. PMID: 25805945; PMCID: PMC4363768.
- Crawford C, Panas R. Post-Infectious Irritable Bowel Syndrome with Functional Diarrhea Following C. difficile Infections: Case Studies of Responses Using Serum-Derived Bovine Immunoglobulin. Journal of Gastroenterology and Hepatology Research. Vol 4, No 4 (2015).
- Valentin N, Camilleri M, Carlson P, Harrington SC, Eckert D, O’Neill J, Burton D, Chen J, Shaw AL, Acosta A. Potential mechanisms of effects of serum-derived bovine immunoglobulin/protein isolate therapy in patients with diarrhea-predominant irritable bowel syndrome. Physiol Rep. 2017 Mar;5(5):e13170. doi: 10.14814/phy2.13170. PMID: 28275113; PMCID: PMC5350178.
- Shaw AL, Tomanelli A, Bradshaw TP, Petschow BW, Burnett BP. Impact of serum-derived bovine immunoglobulin/protein isolate therapy on irritable bowel syndrome and inflammatory bowel disease: a survey of patient perspective. Patient Prefer Adherence. 2017 May 31;11:1001-1007. doi: 10.2147/PPA.S134792. PMID: 28615929; PMCID: PMC5460652.
- Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015 Mar 3;313(9):949-58. doi: 10.1001/jama.2015.0954. PMID: 25734736.
- Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000Res. 2018 Jul 9;7:F1000 Faculty Rev-1029. doi: 10.12688/f1000research.14592.1. PMID: 30026921; PMCID: PMC6039952.
- Hawrelak JA, Myers SP. The causes of intestinal dysbiosis: a review. Altern Med Rev. 2004 Jun;9(2):180-97. PMID: 15253677.
- Thabane M, Marshall JK. Post-infectious irritable bowel syndrome. World J Gastroenterol. 2009 Aug 7;15(29):3591-6. doi: 10.3748/wjg.15.3591. PMID: 19653335; PMCID: PMC2721231.
- Chen B, Kim JJ, Zhang Y, Du L, Dai N. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis. J Gastroenterol. 2018 Jul;53(7):807-818. doi: 10.1007/s00535-018-1476-9. Epub 2018 May 14. PMID: 29761234.
- Camilleri M, Gorman H. Intestinal permeability and irritable bowel syndrome. Neurogastroenterol Motil. 2007 Jul;19(7):545-52. doi: 10.1111/j.1365-2982.2007.00925.x. PMID: 17593135.
- Barbara G. Mucosal barrier defects in irritable bowel syndrome. Who left the door open? Am J Gastroenterol. 2006 Jun;101(6):1295-8. doi: 10.1111/j.1572-0241.2006.00667.x. PMID: 16771952.
- Barbara G, Zecchi L, Barbaro R, Cremon C, Bellacosa L, Marcellini M, De Giorgio R, Corinaldesi R, Stanghellini V. Mucosal permeability and immune activation as potential therapeutic targets of probiotics in irritable bowel syndrome. J Clin Gastroenterol. 2012 Oct;46 Suppl:S52-5. doi: 10.1097/MCG.0b013e318264e918. PMID: 22955358.
- Catassi C, Alaedini A, Bojarski C, Bonaz B, Bouma G, Carroccio A, Castillejo G, De Magistris L, Dieterich W, Di Liberto D, Elli L, Fasano A, Hadjivassiliou M, Kurien M, Lionetti E, Mulder CJ, Rostami K, Sapone A, Scherf K, Schuppan D, Trott N, Volta U, Zevallos V, Zopf Y, Sanders DS. The Overlapping Area of Non-Celiac Gluten Sensitivity (NCGS) and Wheat-Sensitive Irritable Bowel Syndrome (IBS): An Update. Nutrients. 2017 Nov 21;9(11):1268. doi: 10.3390/nu9111268. PMID: 29160841; PMCID: PMC5707740.
- Deng Y, Misselwitz B, Dai N, Fox M. Lactose Intolerance in Adults: Biological Mechanism and Dietary Management. Nutrients. 2015 Sep 18;7(9):8020-35. doi: 10.3390/nu7095380. PMID: 26393648; PMCID: PMC4586575.
- Schnabel L, Buscail C, Sabate JM, Bouchoucha M, Kesse-Guyot E, Allès B, Touvier M, Monteiro CA, Hercberg S, Benamouzig R, Julia C. Association Between Ultra-Processed Food Consumption and Functional Gastrointestinal Disorders: Results From the French NutriNet-Santé Cohort. Am J Gastroenterol. 2018 Aug;113(8):1217-1228. doi: 10.1038/s41395-018-0137-1. Epub 2018 Jun 15. PMID: 29904158.
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2):252-8. doi: 10.1111/j.1440-1746.2009.06149.x. PMID: 20136989.
- Barbara G, Cremon C, Carini G, Bellacosa L, Zecchi L, De Giorgio R, Corinaldesi R, Stanghellini V. The immune system in irritable bowel syndrome. J Neurogastroenterol Motil. 2011 Oct;17(4):349-59. doi: 10.5056/jnm.2011.17.4.349. Epub 2011 Oct 31. PMID: 22148103; PMCID: PMC3228974.
- Jin DC, Cao HL, Xu MQ, Wang SN, Wang YM, Yan F, Wang BM. Regulation of the serotonin transporter in the pathogenesis of irritable bowel syndrome. World J Gastroenterol. 2016 Sep 28;22(36):8137-48. doi: 10.3748/wjg.v22.i36.8137. PMID: 27688655; PMCID: PMC5037082.
- Liu L, Liu BN, Chen S, Wang M, Liu Y, Zhang YL, Yao SK. Visceral and somatic hypersensitivity, autonomic cardiovascular dysfunction and low-grade inflammation in a subset of irritable bowel syndrome patients. J Zhejiang Univ Sci B. 2014 Oct;15(10):907-14. doi: 10.1631/jzus.B1400143. PMID: 25294380; PMCID: PMC4201319.
- Keszthelyi D, Troost FJ, Jonkers DM, van Eijk HM, Dekker J, Buurman WA, Masclee AA. Visceral hypersensitivity in irritable bowel syndrome: evidence for involvement of serotonin metabolism–a preliminary study. Neurogastroenterol Motil. 2015 Aug;27(8):1127-37. doi: 10.1111/nmo.12600. Epub 2015 May 31. PMID: 26031193.
- Chedid V, Dhalla S, Clarke JO, Roland BC, Dunbar KB, Koh J, Justino E, Tomakin E, Mullin GE. Herbal therapy is equivalent to rifaximin for the treatment of small intestinal bacterial overgrowth. Glob Adv Health Med. 2014 May;3(3):16-24. doi: 10.7453/gahmj.2014.019. PMID: 24891990; PMCID: PMC4030608.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!