What’s the Most Accurate SIBO Breath Test for Diagnosis?
- What Is SIBO? Best SIBO Breath Test|
- Breath Test Meta-Analysis|
- Glucose vs. Lactulose Testing|
- Lactulose Test Challenges|
- Glucose Test Advantages|
- Breath Testing Usefulness|
- Bottom Line|
- Glucose breath tests are more accurate than lactulose breath tests for the diagnosis of small intestinal bacterial overgrowth (SIBO).
- Elevations of methane or hydrogen after 90-100 minutes usually show bacteria in the large intestine, which is normal. Misreading this can lead to false positives.
There are two types of SIBO breath tests: lactulose breath tests and glucose breath tests. The lactulose test is generally more popular, but the data indicate it’s not as accurate.
What is the best test for small intestinal bacterial overgrowth (SIBO)? Let’s discuss.
What Is SIBO?
Small intestinal bacterial overgrowth (SIBO) is exactly what the name implies: an excess of normal gut bacteria in the small intestine. Symptoms of SIBO include:
- Gas or flatulence
- Bloating
- Abdominal pain
- Altered bowel function, including diarrhea, constipation, or other alterations in transit time
- Weight loss or nutritional deficiencies from malabsorption
- Food intolerances, such as lactose intolerance or fructose malabsorption

New evidence suggests there may also be a correlation with symptoms like heartburn 1.
SIBO has also been correlated with irritable bowel syndrome (IBS ) 2 3, fibromyalgia 4, rheumatoid arthritis 5, non-responsive celiac disease 6, inflammatory bowel diseases (IBD) (including Crohn’s disease 7), rosacea 8, and metabolic health issues like being overweight, high blood sugar, and high cholesterol 9 10 11. And, surprisingly, one study showed that being hypothyroid was a risk factor for SIBO as well 12.
Abdominal adhesions from injury or surgery 13, chronic constipation 14 15, use of proton pump inhibitors (PPIs) 16, and small intestinal diseases 17 18 are recognized as common causes of SIBO. So, it’s not a surprising contention that imbalances in the digestive system — in this case, SIBO — may correlate with many symptoms and conditions. This is why it can be very helpful to have a diagnostic test to tell you whether you have small intestinal bacterial overgrowth.
SIBO Breath Testing
The most practical and clinically available tests for diagnosing SIBO are two types of breath tests: glucose breath tests and lactulose breath tests.
To prepare for a methane or hydrogen breath test for SIBO, the patient either drinks a glucose solution or a lactulose solution and then collects breath samples with an at-home breath test kit. The lab measures the levels of hydrogen and methane gas in the samples, which was produced in the small intestine.
Best SIBO Breath Test? A Meta-Analysis Review
If you’re planning to run a SIBO breath test, you’ll want to use the highest quality test. Thankfully, a meta-analysis — a summary of all available high-quality data on a subject — has been published to give a definitive answer about which breath test is best for the diagnosis of SIBO. The paper is titled “Breath Test for Non-Invasive Small Intestinal Bacterial Overgrowth Diagnosis: A Systematic Review with Meta-Analysis” 19.
Glucose Breath Test vs. Lactulose SIBO Breath Testing
The authors of the meta-analysis concluded, “Overall, our results clearly showed that glucose breath tests had higher sensitivity and specificity than lactulose breath tests” 20.
- Sensitivity tells you if you were correctly diagnosed with the condition.
- Specificity tells you if you were correctly found not to have that condition.
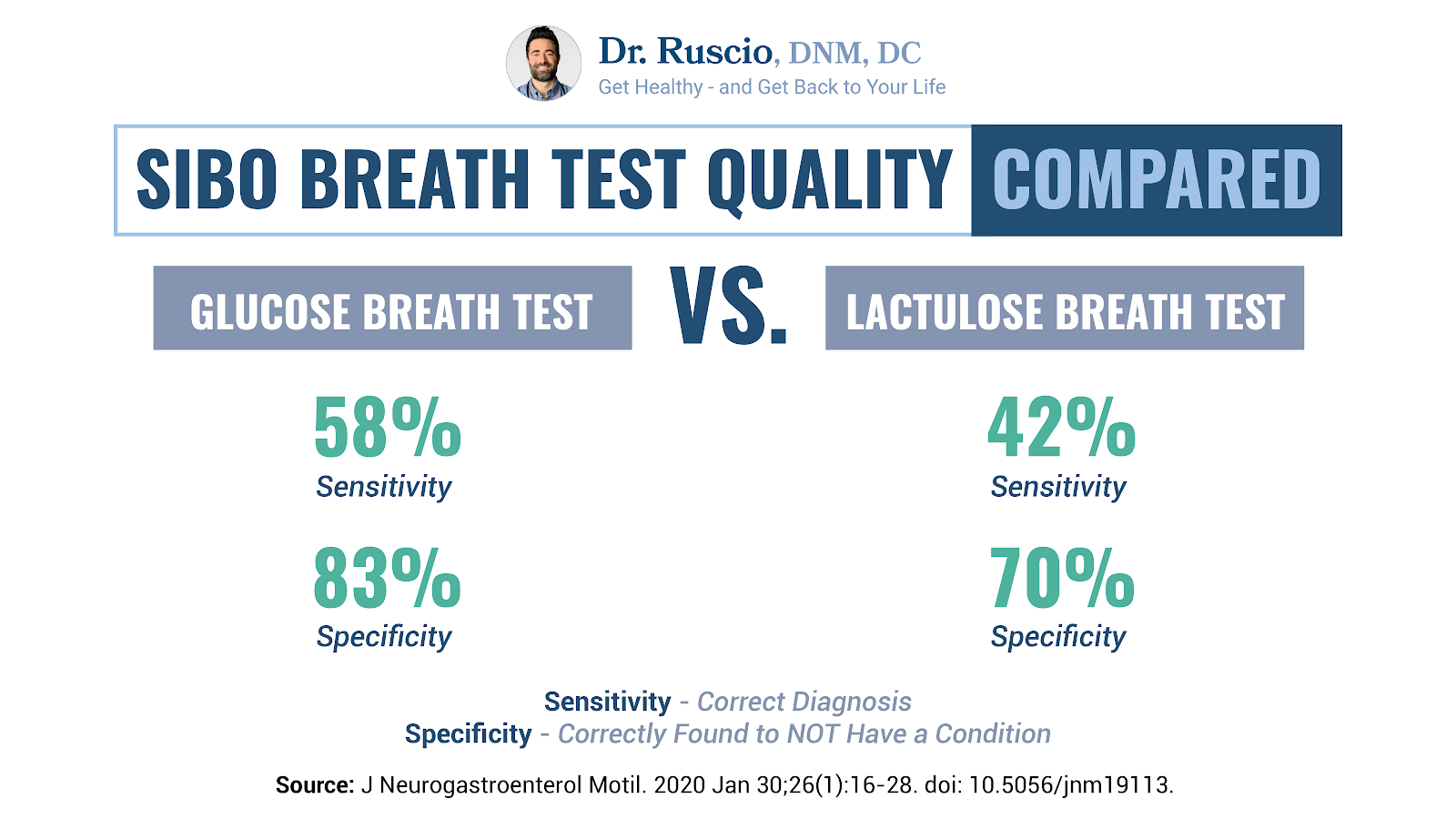
In the study, glucose breath tests showed a sensitivity of 58% and a specificity of 83%, compared to 42% sensitivity and specificity at 70% for lactulose breath tests 21.
The lower these numbers, the higher the likelihood of false negatives or false positives.
The meta-analysis data clearly show the glucose breath test has better scores for sensitivity and specificity, meaning it correctly diagnoses those who have the condition, and it correctly identifies who does not have the condition more often.
This is very relevant because patients are frequently incorrectly diagnosed with SIBO and are then subjected to unnecessary fear, dietary restrictions, and treatments.
This is likely because the lactulose breath test — while helpful in the hands of an astute clinician who uses it correctly — actually suffers from a higher number of false positives. This is the most commonly used SIBO breath test.
In this context, the glucose breath test has better sensitivity and specificity than the lactulose breath test and, therefore, should be preferred in clinical practice.
Lactulose Breath Test and False Positives
One of the challenges with the lactulose breath test is in the time interpretation of the test. This is a common error that leads to incorrect SIBO diagnosis.
Here is what a typical SIBO breath test result looks like:
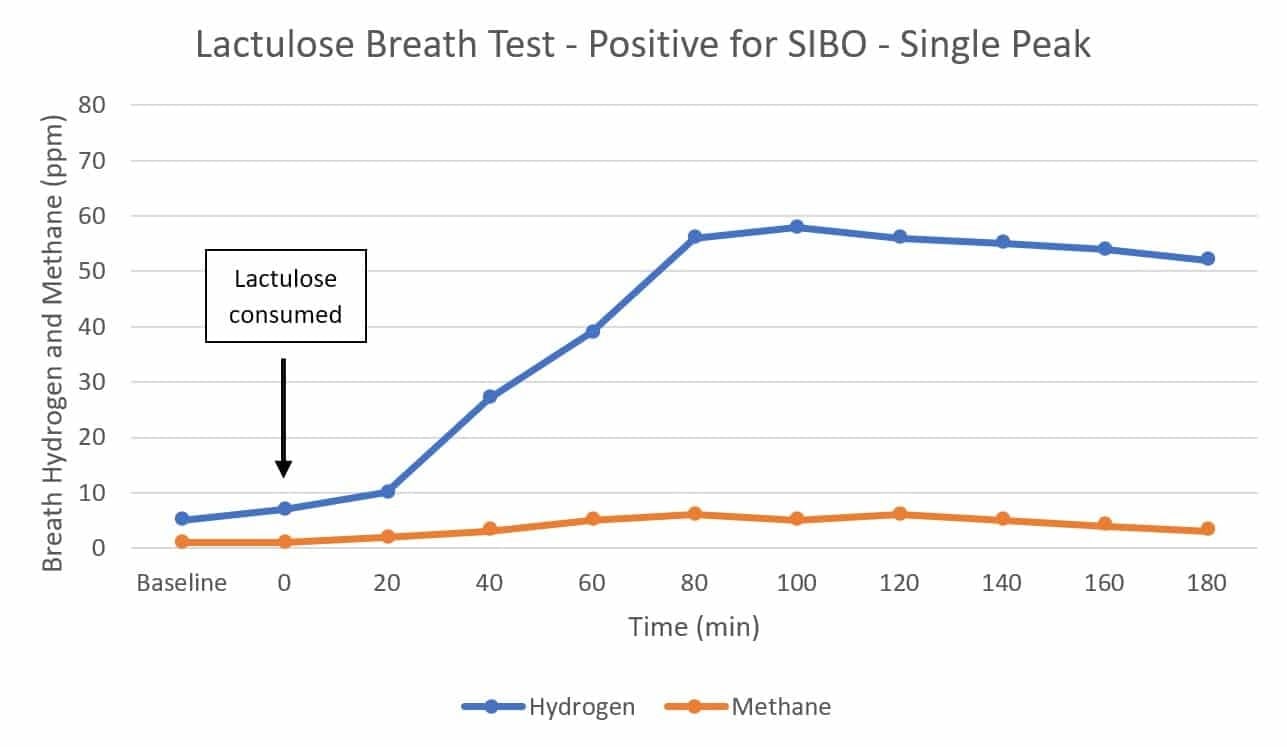
Test samples are collected at either 15- or 20-minute intervals. When looking at the lactulose breath test, it’s important to identify at what point you no longer see readings from the small intestine.
Research indicates the preferred window is 80-90 minutes 22, but you could go up to 100 minutes. The 80- or 90-minute mark generally shows the transition to the large intestine. This matters because rising gas levels in the large intestine are normal.
Unfortunately, SIBO lab analyzers haven’t really caught up with this interpretation. So, it’s important that clinicians understand the correct time interpretation.
People who have a gas elevation at 100 or 120 minutes, and sometimes even at 140 minutes, may be falsely told they have SIBO. They may then be prescribed SIBO treatment with antibiotics like Rifaximin when they really need nothing of the sort.
Clinicians need to be stringent with the time interpretation of the lactulose breath test in order to mitigate this false positive rate.
If you’re using a lactulose breath test, it’s important to not be overly liberal in diagnosing SIBO, especially if the only elevation of gases is seen towards the end of the test.
Glucose Breath Test Advantages
The glucose breath test seems to protect against that false positive.
I feel this is very important for patients to understand because this update hasn’t yet permeated the SIBO community. While most providers have the best intentions when diagnosing, it seems some patients are told they have SIBO when they don’t. This is a problem because it subjects people to unnecessary fear, worry, and taking on potentially unhealthy dietary restrictions and treatments.
How Useful Are SIBO Breath Tests?
The overall utility of SIBObreath testing is moderate. It can help to steer decisions, but it’s not the end-all-be-all.
The meta-analysis authors concluded though breath tests don’t perform as well as the gold-standard testing, they are useful because they are less expensive and invasive 23.
So essentially, though SIBO breath testing is imperfect, it’s probably the most justifiable test compared with sampling jejunal secretions by endoscopy.
We can only test for some of the imbalances we know exist in the small intestine, which means it’s not in the best interest of patients or providers to overly focus on testing.
We can use testing as part of the process to determine what may be going on, but we can also use many therapies for treating SIBO without lab results.
Probiotics are one example. They can be effective and helpful for small intestine bacterial overgrowth and other microbiome imbalances 24. One meta-analysis and several clinical trials show probiotics can be an effective treatment for SIBO 25 26 27. You don’t need a SIBO breath test to use a probiotic for IBS or SIBO symptoms.
The same likely applies for Small Intestinal Fungal Overgrowth (SIFO), since probiotics also have antifungal effects.
SIBO Breath Testing: Bottom Line
SIBO breath testing can be helpful, but it has limitations. Of the SIBO breath tests, the glucose breath test is best. However, a well-trained clinician can responsibly use a lactulose test.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- https://ddw.scientificposters.com/epsAbstractDDW.cfm?id=6
- Schmulson M, Bielsa MV, Carmona-Sánchez R, Hernández A, López-Colombo A, López Vidal Y, Peláez-Luna M, Remes-Troche JM, Tamayo JL, Valdovinos MA. Microbiota, gastrointestinal infections, low-grade inflammation, and antibiotic therapy in irritable bowel syndrome: an evidence-based review. Rev Gastroenterol Mex. 2014 Apr-Jun;79(2):96-134. English, Spanish. doi: 10.1016/j.rgmx.2014.01.004. Epub 2014 May 23. PMID: 24857420.
- Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020 Jul 10;11:664. doi: 10.3389/fpsyt.2020.00664. PMID: 32754068; PMCID: PMC7366247.
- Pimentel M, Wallace D, Hallegua D, Chow E, Kong Y, Park S, Lin HC. A link between irritable bowel syndrome and fibromyalgia may be related to findings on lactulose breath testing. Ann Rheum Dis. 2004 Apr;63(4):450-2. doi: 10.1136/ard.2003.011502. PMID: 15020342; PMCID: PMC1754959.
- Podas T, Nightingale JM, Oldham R, Roy S, Sheehan NJ, Mayberry JF. Is rheumatoid arthritis a disease that starts in the intestine? A pilot study comparing an elemental diet with oral prednisolone. Postgrad Med J. 2007 Feb;83(976):128-31. doi: 10.1136/pgmj.2006.050245. PMID: 17308218; PMCID: PMC2805936.
- Tursi A, Brandimarte G, Giorgetti G. High prevalence of small intestinal bacterial overgrowth in celiac patients with persistence of gastrointestinal symptoms after gluten withdrawal. Am J Gastroenterol. 2003 Apr;98(4):839-43. doi: 10.1111/j.1572-0241.2003.07379.x. PMID: 12738465.
- Shah A, Morrison M, Burger D, Martin N, Rich J, Jones M, Koloski N, Walker MM, Talley NJ, Holtmann GJ. Systematic review with meta-analysis: the prevalence of small intestinal bacterial overgrowth in inflammatory bowel disease. Aliment Pharmacol Ther. 2019 Mar;49(6):624-635. doi: 10.1111/apt.15133. Epub 2019 Feb 8. PMID: 30735254.
- Parodi A, Paolino S, Greco A, Drago F, Mansi C, Rebora A, Parodi A, Savarino V. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008 Jul;6(7):759-64. doi: 10.1016/j.cgh.2008.02.054. Epub 2008 May 5. PMID: 18456568.
- Mathur R, Chua KS, Mamelak M, Morales W, Barlow GM, Thomas R, Stefanovski D, Weitsman S, Marsh Z, Bergman RN, Pimentel M. Metabolic effects of eradicating breath methane using antibiotics in prediabetic subjects with obesity. Obesity (Silver Spring). 2016 Mar;24(3):576-82. doi: 10.1002/oby.21385. Epub 2016 Feb 1. PMID: 26833719; PMCID: PMC4769647.
- Basseri RJ, Basseri B, Pimentel M, Chong K, Youdim A, Low K, Hwang L, Soffer E, Chang C, Mathur R. Intestinal methane production in obese individuals is associated with a higher body mass index. Gastroenterol Hepatol (N Y). 2012 Jan;8(1):22-8. PMID: 22347829; PMCID: PMC3277195.
- Mathur R, Amichai M, Chua KS, Mirocha J, Barlow GM, Pimentel M. Methane and hydrogen positivity on breath test is associated with greater body mass index and body fat. J Clin Endocrinol Metab. 2013 Apr;98(4):E698-702. doi: 10.1210/jc.2012-3144. Epub 2013 Mar 26. PMID: 23533244; PMCID: PMC3615195.
- Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014 May;18(3):307-9. doi: 10.4103/2230-8210.131155. PMID: 24944923; PMCID: PMC4056127.
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017 Feb 7;23(5):842-852. doi: 10.3748/wjg.v23.i5.842. PMID: 28223728; PMCID: PMC5296200.
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017 Feb 7;23(5):842-852. doi: 10.3748/wjg.v23.i5.842. PMID: 28223728; PMCID: PMC5296200.
- Roland BC, Ciarleglio MM, Clarke JO, Semler JR, Tomakin E, Mullin GE, Pasricha PJ. Small Intestinal Transit Time Is Delayed in Small Intestinal Bacterial Overgrowth. J Clin Gastroenterol. 2015 Aug;49(7):571-6. doi: 10.1097/MCG.0000000000000257. PMID: 25319735.
- Su T, Lai S, Lee A, He X, Chen S. Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. J Gastroenterol. 2018 Jan;53(1):27-36. doi: 10.1007/s00535-017-1371-9. Epub 2017 Aug 2. PMID: 28770351.
- Cohen-Mekelburg S, Tafesh Z, Coburn E, Weg R, Malik N, Webb C, Hammad H, Scherl E, Bosworth BP. Testing and Treating Small Intestinal Bacterial Overgrowth Reduces Symptoms in Patients with Inflammatory Bowel Disease. Dig Dis Sci. 2018 Sep;63(9):2439-2444. doi: 10.1007/s10620-018-5109-1. Epub 2018 May 14. PMID: 29761252.
- Losurdo G, Marra A, Shahini E, Girardi B, Giorgio F, Amoruso A, Pisani A, Piscitelli D, Barone M, Principi M, Di Leo A, Ierardi E. Small intestinal bacterial overgrowth and celiac disease: A systematic review with pooled-data analysis. Neurogastroenterol Motil. 2017 Jun;29(6). doi: 10.1111/nmo.13028. Epub 2017 Feb 12. PMID: 28191721.
- Losurdo G, Leandro G, Ierardi E, Perri F, Barone M, Principi M, Leo AD. Breath Tests for the Non-invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review With Meta-analysis. J Neurogastroenterol Motil. 2020 Jan 30;26(1):16-28. doi: 10.5056/jnm19113. PMID: 31743632; PMCID: PMC6955189.
- Losurdo G, Leandro G, Ierardi E, Perri F, Barone M, Principi M, Leo AD. Breath Tests for the Non-invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review With Meta-analysis. J Neurogastroenterol Motil. 2020 Jan 30;26(1):16-28. doi: 10.5056/jnm19113. PMID: 31743632; PMCID: PMC6955189.
- Losurdo G, Leandro G, Ierardi E, Perri F, Barone M, Principi M, Leo AD. Breath Tests for the Non-invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review With Meta-analysis. J Neurogastroenterol Motil. 2020 Jan 30;26(1):16-28. doi: 10.5056/jnm19113. PMID: 31743632; PMCID: PMC6955189.
- Rezaie A, Buresi M, Lembo A, Lin H, McCallum R, Rao S, Schmulson M, Valdovinos M, Zakko S, Pimentel M. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. Am J Gastroenterol. 2017 May;112(5):775-784. doi: 10.1038/ajg.2017.46. Epub 2017 Mar 21. PMID: 28323273; PMCID: PMC5418558.
- Losurdo G, Leandro G, Ierardi E, Perri F, Barone M, Principi M, Leo AD. Breath Tests for the Non-invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review With Meta-analysis. J Neurogastroenterol Motil. 2020 Jan 30;26(1):16-28. doi: 10.5056/jnm19113. PMID: 31743632; PMCID: PMC6955189.
- Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017 Apr;51(4):300-311. doi: 10.1097/MCG.0000000000000814. PMID: 28267052.
- Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017 Apr;51(4):300-311. doi: 10.1097/MCG.0000000000000814. PMID: 28267052.
- Soifer LO, Peralta D, Dima G, Besasso H. Eficacia comparativa de un probiótico vs un antibiótico en la respuesta clínica de pacientes con sobrecrecimiento bacteriano del intestino y distensión abdominal crónica funcional: un estudio piloto [Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study]. Acta Gastroenterol Latinoam. 2010 Dec;40(4):323-7. Spanish. PMID: 21381407.
- Leventogiannis K, Gkolfakis P, Spithakis G, Tsatali A, Pistiki A, Sioulas A, Giamarellos-Bourboulis EJ, Triantafyllou K. Effect of a Preparation of Four Probiotics on Symptoms of Patients with Irritable Bowel Syndrome: Association with Intestinal Bacterial Overgrowth. Probiotics Antimicrob Proteins. 2019 Jun;11(2):627-634. doi: 10.1007/s12602-018-9401-3. Erratum in: Probiotics Antimicrob Proteins. 2018 Mar 28;: PMID: 29508268; PMCID: PMC6541575.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!