How to Answer the Question ‘Is Hypothyroidism Genetic?’
- What Is Hypothyroidism?|
- Is Hypothyroidism Genetic?|
- Thyroid and Epigenetics|
- What to Do About Hypothyroidism|
- The Bottom Line|
- Recommended Products|
Patients with a family history of hypothyroidism often ask us questions like these: Is hypothyroidism genetic? Will I become hypothyroid if my mother and sister both have thyroid disease? If hypothyroid disease runs in my family, does that mean I’ll always struggle with my thyroid health?
Research in epigenetics does suggest that your genetics influence your risk of developing hypothyroidism. However, it’s important to emphasize that your genes aren’t the whole picture.
Studies suggest that whether or not your genetic risk expresses itself is significantly affected by how you live your life. Specifically, this means your diet, stress, and environment. This means that you can affect your health outcomes by making good choices.
In this article, we’ll explain what hypothyroidism is, the connection between epigenetics and thyroid disease, and what you can do to maintain your thyroid health and improve your hypothyroidism.

What Is Hypothyroidism?
Hypothyroidism — an underactive thyroid — is when your thyroid gland doesn’t make enough thyroid hormone.
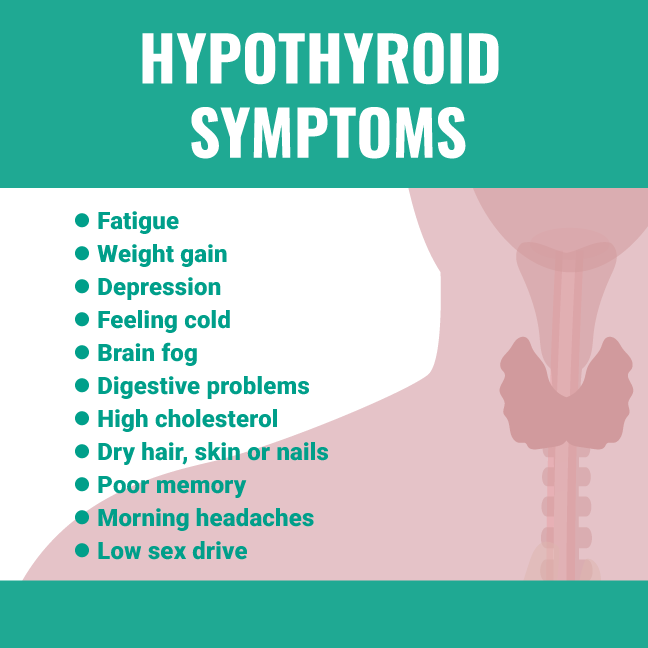
Common symptoms of hypothyroidism include:
- Fatigue
- Constipation
- Weight gain or obesity
- Dry skin
- Hair loss
- Depression
- Feeling cold
- Brain fog
- Low sex drive
According to the American Thyroid Association, the most common type of hypothyroidism (in the US) is autoimmune thyroiditis, also called Hashimoto’s thyroiditis. The estimated prevalence of Hashimoto’s disease is between 1% and 2% in the United States, and women are 10 times more likely to have it than men [1].
Autoimmune thyroiditis means that your immune system is attacking your thyroid gland, which can impair your thyroid function.
Additional thyroid symptoms associated with Hashimoto’s thyroiditis include non-painful goiter, thyroid nodules, or pain and swelling in your thyroid area.
Is Hypothyroidism Genetic?
It’s not uncommon to meet hypothyroid women whose mothers, aunts, and daughters are also hypothyroid. Is there a genetic link? In short, the answer is “yes.” Studies have found that:
- Having a first-degree family member with a thyroid disorder is an increased risk factor for developing a thyroid condition [2].
- Approximately 30%-60% of hypothyroidism is associated with a family history of hypothyroidism [3, 4].
Researchers use genetic sequencing tests to identify likely candidate genes that may increase the risk of thyroid problems, including both hypothyroidism and hyperthyroidism. Let’s explore what they’ve learned about genetics and specific thyroid conditions.

Hashimoto’s Thyroiditis and Genetics
Hashimoto’s disease (autoimmune hypothyroidism) is thought to be caused by a combination of inherited genes and environmental triggers [5, 6].
Four particular gene regions, including the thyroid-stimulating hormone receptor (TSHR), are associated with autoimmune thyroid disease and autoimmune disease in general [7, 8]. However, the specific genes or gene combinations that cause hypothyroidism remain unclear [9, 10], and researchers have been unable to pinpoint the exact genes responsible for Hashimoto’s [11].
Despite the genetic risks of developing Hashimoto’s thyroiditis, a family history of thyroid disease doesn’t sentence you to becoming hypothyroid. And if you are diagnosed with Hashimoto’s, you can still lead a healthy life. Autoimmune hypothyroidism generally responds to standard medical treatment as well as diet and lifestyle improvements.
Congenital Hypothyroidism and Genetics
A much rarer form of hypothyroidism is congenital hypothyroidism due to a physical abnormality of the thyroid gland. It can also be caused by a problem with the pituitary gland, which normally signals the thyroid to produce thyroid hormone [12].
Newborns are screened for congenital hypothyroidism soon after birth with a blood test, as a lack of treatment can cause severe developmental delays.
Research generally has suggested that less than 5% of congenital hypothyroidism cases are associated with known gene abnormalities [12]. However, genetics may play a bigger role than previously thought in congenital hypothyroidism. A research team reviewing medical histories of children diagnosed with congenital hypothyroidism found that a significant portion of them had first-degree relatives with thyroid conditions [13], and another study found similar results [14].
Thyroid Disease and Epigenetics
Why are only 30-60% of hypothyroidism cases associated with family history [3, 4]? Though our genes can’t change, the field of epigenetics suggests that the way we live our lives influences whether or not those genes express themselves [5, 15].
Environmental triggers that influence thyroid genes and health include things like your iodine status [16], toxin exposure [17], or specific foods [18].
A common environmental trigger for thyroid disease is gut imbalance. The hygiene hypothesis suggests that Western diets and lifestyles, which are often low in exposure to and diversity of beneficial bacteria, can impact gut colonization and immune system health [19].
As an example of how gut bacteria can influence your thyroid health, treatment of pathogens like H. pylori [20] and Blastocystis hominis [21] have resolved thyroid conditions. SIBO (small intestinal bacterial overgrowth) has also been closely linked to thyroid disease [22, 23].
The good news is you can positively influence your thyroid health by being mindful of your food and environmental toxin exposures and by attending to your gut health.

What to Do About Hypothyroidism
Even though your genes may be part of the reason you’re hypothyroid, don’t despair about your future just yet.
For people who are truly hypothyroid, standard thyroid replacement therapy with levothyroxine (synthetic thyroid hormone) is usually quite effective. Yet many people still don’t feel well even after their thyroid labs normalize with thyroid treatment.
If this sounds like you, there are options beyond focusing on your genes, which you can’t change. Let’s talk about what you can do to improve your hypothyroidism.
Improve Your Gut Health for Better Thyroid Function
It may not seem like your gut has anything to do with your thyroid, but thyroid-like symptoms like fatigue or depression may actually come from your gut [24, 25]. Additionally, poor gut health can make it harder to absorb your thyroid medication [26].
Irritable bowel syndrome (IBS) [24], small intestinal bacterial overgrowth (SIBO) [23, 27], low stomach acid [28, 29], H. pylori infection [20], and leaky gut [30] are all associated with thyroid symptoms or thyroid disease. Treating these related conditions often improves thyroid symptoms and, in some cases, has decreased patients’ thyroid medication dose [31, 32].
Resolving gut infections [33] and eating a gut-healthy diet [34] can help improve your thyroid symptoms and the effectiveness of your thyroid medication.
Epigenetic Eating for Hypothyroidism
What you eat and the quality of your food is important for supporting your thyroid health because epigenetic triggers, such as particular foods and iodine, are a risk for developing hypothyroidism.
For example, low-carb [35], gluten-free [36], and dairy-free diets [37] have been shown to influence thyroid lab markers and antibodies. Pesticides and herbicides are known to negatively impact the thyroid and other endocrine organs [17, 38, 39, 40]. And foods high in iodine or iodine supplements have been shown to heavily influence the development of hypothyroidism [41, 42, 43].
Eating organically grown food can help protect against the chemical toxins that affect your thyroid. But there are many possible healthy diets to support your thyroid health.
To choose a thyroid-supporting diet, follow these principles:
For more support in choosing the right diet for your thyroid health, reach out to our clinic or our health coach.
Hypothyroidism Diagnosis

Many people are misdiagnosed with hypothyroidism [44], so it’s helpful to make sure that you have been appropriately diagnosed.
Research suggests that two common blood tests are the gold standard to diagnose hypothyroidism:
- Thyroid-stimulating hormone (TSH — also called thyrotropin)
- Free T4 (thyroxine) thyroid hormone test
You are considered hypothyroid if you have the following:
- High TSH levels
- Low T4 hormone levels
- Thyroid symptoms.
Sometimes, your doctor will also run a free T3 (triiodothyronine) thyroid hormone test. Though many functional medicine providers pay a lot of attention to the T3 hormone, research suggests that low T3 is a sign of poor gut health [45, 46]. We’ve noticed in the clinic that T3 levels typically normalize once gut health improves.
Hashimoto’s thyroiditis is diagnosed with the combination of thyroid symptoms and the following [47]
- Elevated TSH levels
- Low T4 levels
- Elevated levels of TPO (thyroid peroxidase) antibodies or TG (thyroglobulin) antibodies
- Changes in your thyroid gland seen on ultrasound
If you’re unsure whether your hypothyroid diagnosis is accurate, schedule a follow-up with your doctor or healthcare provider.
The Bottom Line
Though your hypothyroidism may be linked to your genes, this doesn’t mean that you are destined to — or stuck with — poor thyroid health for life. What you eat and how you live can turn those genes on or off.
This is great news. It means that you have the power to influence your thyroid health by making good choices. Improving your gut health by eating a healthy diet and treating gut infections can help make sure your thyroid genes put their best foot forward.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Vanderpump MPJ. The epidemiology of thyroid disease. Br Med Bull [Internet]. 2011;99:39–51. Available from: http://dx.doi.org/10.1093/bmb/ldr030 PMID: 21893493
- Vaidya B, Kendall-Taylor P, Pearce SHS. The genetics of autoimmune thyroid disease. J Clin Endocrinol Metab [Internet]. 2002 Dec;87(12):5385–5397. Available from: http://dx.doi.org/10.1210/jc.2002-020492 PMID: 12466323
- Panicker V, Wilson SG, Spector TD, Brown SJ, Falchi M, Richards JB, Surdulescu GL, Lim EM, Fletcher SJ, Walsh JP. Heritability of serum TSH, free T4 and free T3 concentrations: a study of a large UK twin cohort. Clin Endocrinol [Internet]. 2008 Apr;68(4):652–659. Available from: http://dx.doi.org/10.1111/j.1365-2265.2007.03079.x PMID: 17970774
- Hansen PS, Brix TH, Sørensen TIA, Kyvik KO, Hegedüs L. Major genetic influence on the regulation of the pituitary-thyroid axis: a study of healthy Danish twins. J Clin Endocrinol Metab [Internet]. 2004 Mar;89(3):1181–1187. Available from: http://dx.doi.org/10.1210/jc.2003-031641 PMID: 15001606
- Ragusa F, Fallahi P, Elia G, Gonnella D, Paparo SR, Giusti C, Churilov LP, Ferrari SM, Antonelli A. Hashimotos’ thyroiditis: Epidemiology, pathogenesis, clinic and therapy. Best Pract Res Clin Endocrinol Metab [Internet]. 2019 Dec;33(6):101367. Available from: http://dx.doi.org/10.1016/j.beem.2019.101367 PMID: 31812326
- Antonelli A, Ferrari SM, Corrado A, Di Domenicantonio A, Fallahi P. Autoimmune thyroid disorders. Autoimmun Rev [Internet]. 2015 Feb;14(2):174–180. Available from: http://dx.doi.org/10.1016/j.autrev.2014.10.016 PMID: 25461470
- Brand OJ, Gough SCL. Genetics of thyroid autoimmunity and the role of the TSHR. Mol Cell Endocrinol [Internet]. 2010 Jun 30;322(1-2):135–143. Available from: http://dx.doi.org/10.1016/j.mce.2010.01.013 PMID: 20083159
- Tandon N, Zhang L, Weetman AP. HLA associations with Hashimoto’s thyroiditis. Clin Endocrinol [Internet]. 1991 May;34(5):383–386. Available from: http://dx.doi.org/10.1111/j.1365-2265.1991.tb00309.x PMID: 1676351
- Panicker V. Genetics of thyroid function and disease. Clin Biochem Rev [Internet]. 2011 Nov;32(4):165–175. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22147956 PMCID: PMC3219766
- Balázs C. [The role of hereditary and environmental factors in autoimmune thyroid diseases]. Orv Hetil [Internet]. 2012 Jul 1;153(26):1013–1022. Available from: http://dx.doi.org/10.1556/OH.2012.29370 PMID: 22735372
- Biondi B, Kahaly GJ, Robertson RP. Thyroid Dysfunction and Diabetes Mellitus: Two Closely Associated Disorders. Endocr Rev [Internet]. 2019 Jun 1;40(3):789–824. Available from: http://dx.doi.org/10.1210/er.2018-00163 PMCID: PMC6507635
- Peters C, van Trotsenburg ASP, Schoenmakers N. DIAGNOSIS OF ENDOCRINE DISEASE: Congenital hypothyroidism: update and perspectives. Eur J Endocrinol [Internet]. 2018 Dec 1;179(6):R297–R317. Available from: http://dx.doi.org/10.1530/EJE-18-0383 PMID: 30324792
- Castanet M, Lyonnet S, Bonaïti-Pellié C, Polak M, Czernichow P, Léger J. Familial forms of thyroid dysgenesis among infants with congenital hypothyroidism. N Engl J Med [Internet]. 2000 Aug 10;343(6):441–442. Available from: http://dx.doi.org/10.1056/NEJM200008103430614 PMID: 10939901
- Sindhuja L, Dayal D, Sodhi KS, Sachdeva N, Bhattacharya A. Thyroid dysfunction and developmental anomalies in first degree relatives of children with thyroid dysgenesis. World J Pediatr [Internet]. 2016 May;12(2):215–218. Available from: http://dx.doi.org/10.1007/s12519-015-0061-z PMID: 26684308
- Cañas CA, Cañas F, Bonilla-Abadía F, Ospina FE, Tobón GJ. Epigenetics changes associated to environmental triggers in autoimmunity. Autoimmunity [Internet]. 2016;49(1):1–11. Available from: http://dx.doi.org/10.3109/08916934.2015.1086996 PMID: 26369426
- Ban Y, Tomer Y. Genetic susceptibility in thyroid autoimmunity. Pediatr Endocrinol Rev [Internet]. 2005 Sep;3(1):20–32. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16369210 PMID: 16369210
- Patrick L. Thyroid disruption: mechanism and clinical implications in human health. Altern Med Rev [Internet]. 2009 Dec;14(4):326–346. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20030460 PMID: 20030460
- Feil R, Fraga MF. Epigenetics and the environment: emerging patterns and implications. Nat Rev Genet [Internet]. 2012 Jan 4;13(2):97–109. Available from: http://dx.doi.org/10.1038/nrg3142 PMID: 22215131
- Lambrecht BN, Hammad H. The immunology of the allergy epidemic and the hygiene hypothesis. Nat Immunol [Internet]. 2017 Sep 19;18(10):1076–1083. Available from: http://dx.doi.org/10.1038/ni.3829 PMID: 28926539
- Bertalot G, Montresor G, Tampieri M, Spasiano A, Pedroni M, Milanesi B, Favret M, Manca N, Negrini R. Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection. Clin Endocrinol [Internet]. 2004 Nov;61(5):650–652. Available from: http://dx.doi.org/10.1111/j.1365-2265.2004.02137.x PMID: 15521972
- El-Zawawy HT, Farag HF, Tolba MM, Abdalsamea HA. Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17. Ther Adv Endocrinol Metab [Internet]. 2020 Feb 21;11:2042018820907013. Available from: http://dx.doi.org/10.1177/2042018820907013 PMCID: PMC7036484
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol [Internet]. 2017 Feb 7;23(5):842–852. Available from: http://dx.doi.org/10.3748/wjg.v23.i5.842 PMCID: PMC5296200
- Konrad P, Chojnacki J, Kaczka A, Pawłowicz M, Rudnicki C, Chojnacki C. [Thyroid dysfunction in patients with small intestinal bacterial overgrowth]. Pol Merkur Lekarski [Internet]. 2018 Jan 23;44(259):15–18. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29374417 PMID: 29374417
- Han CJ, Yang GS. Fatigue in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis of Pooled Frequency and Severity of Fatigue. Asian Nurs Res [Internet]. 2016 Mar;10(1):1–10. Available from: http://dx.doi.org/10.1016/j.anr.2016.01.003 PMID: 27021828
- Frändemark Å, Jakobsson Ung E, Törnblom H, Simrén M, Jakobsson S. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil [Internet]. 2017 Jan;29(1). Available from: http://dx.doi.org/10.1111/nmo.12898 PMID: 27401139
- Virili C, Bassotti G, Santaguida MG, Iuorio R, Del Duca SC, Mercuri V, Picarelli A, Gargiulo P, Gargano L, Centanni M. Atypical celiac disease as cause of increased need for thyroxine: a systematic study. J Clin Endocrinol Metab [Internet]. 2012 Mar;97(3):E419–22. Available from: http://dx.doi.org/10.1210/jc.2011-1851 PMID: 22238404
- Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol [Internet]. 2017 Apr;51(4):300–311. Available from: http://dx.doi.org/10.1097/MCG.0000000000000814 PMID: 28267052
- Lahner E, Annibale B. Pernicious anemia: new insights from a gastroenterological point of view. World J Gastroenterol [Internet]. 2009 Nov 7;15(41):5121–5128. Available from: http://dx.doi.org/10.3748/wjg.15.5121 PMCID: PMC2773890
- Sterzl I, Hrdá P, Matucha P, Cerovská J, Zamrazil V. Anti-Helicobacter Pylori, anti-thyroid peroxidase, anti-thyroglobulin and anti-gastric parietal cells antibodies in Czech population. Physiol Res [Internet]. 2008 Feb 13;57 Suppl 1:S135–41. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18271683 PMID: 18271683
- Küçükemre Aydın B, Yıldız M, Akgün A, Topal N, Adal E, Önal H. Children with Hashimoto’s Thyroiditis Have Increased Intestinal Permeability: Results of a Pilot Study. J Clin Res Pediatr Endocrinol [Internet]. 2020 Sep 2;12(3):303–307. Available from: http://dx.doi.org/10.4274/jcrpe.galenos.2020.2019.0186 PMCID: PMC7499128
- Centanni M, Gargano L, Canettieri G, Viceconti N, Franchi A, Delle Fave G, Annibale B. Thyroxine in goiter, Helicobacter pylori infection, and chronic gastritis. N Engl J Med [Internet]. 2006 Apr 27;354(17):1787–1795. Available from: http://dx.doi.org/10.1056/NEJMoa043903 PMID: 16641395
- Talebi S, Karimifar M, Heidari Z, Mohammadi H, Askari G. The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial. Complement Ther Med [Internet]. 2020 Jan;48:102234. Available from: http://dx.doi.org/10.1016/j.ctim.2019.102234 PMID: 31987229
- Bugdaci MS, Zuhur SS, Sokmen M, Toksoy B, Bayraktar B, Altuntas Y. The role of Helicobacter pylori in patients with hypothyroidism in whom could not be achieved normal thyrotropin levels despite treatment with high doses of thyroxine. Helicobacter [Internet]. 2011 Apr;16(2):124–130. Available from: http://dx.doi.org/10.1111/j.1523-5378.2011.00830.x PMID: 21435090
- Altobelli E, Del Negro V, Angeletti PM, Latella G. Low-FODMAP Diet Improves Irritable Bowel Syndrome Symptoms: A Meta-Analysis. Nutrients [Internet]. 2017 Aug 26;9(9). Available from: http://dx.doi.org/10.3390/nu9090940 PMCID: PMC5622700
- Esposito T, Lobaccaro JM, Esposito MG, Monda V, Messina A, Paolisso G, Varriale B, Monda M, Messina G. Effects of low-carbohydrate diet therapy in overweight subjects with autoimmune thyroiditis: possible synergism with ChREBP. Drug Des Devel Ther [Internet]. 2016 Sep 14;10:2939–2946. Available from: http://dx.doi.org/10.2147/DDDT.S106440 PMCID: PMC5028075
- Krysiak R, Szkróbka W, Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes [Internet]. 2019 Jul;127(7):417–422. Available from: http://dx.doi.org/10.1055/a-0653-7108 PMID: 30060266
- Asik M, Gunes F, Binnetoglu E, Eroglu M, Bozkurt N, Sen H, Akbal E, Bakar C, Beyazit Y, Ukinc K. Decrease in TSH levels after lactose restriction in Hashimoto’s thyroiditis patients with lactose intolerance. Endocrine [Internet]. 2014 Jun;46(2):279–284. Available from: http://dx.doi.org/10.1007/s12020-013-0065-1 PMID: 24078411
- Maqbool F, Mostafalou S, Bahadar H, Abdollahi M. Review of endocrine disorders associated with environmental toxicants and possible involved mechanisms. Life Sci [Internet]. 2016 Jan 15;145:265–273. Available from: http://dx.doi.org/10.1016/j.lfs.2015.10.022 PMID: 26497928
- de Cock M, de Boer MR, Govarts E, Iszatt N, Palkovicova L, Lamoree MH, Schoeters G, Eggesbø M, Trnovec T, Legler J, van de Bor M. Thyroid-stimulating hormone levels in newborns and early life exposure to endocrine-disrupting chemicals: analysis of three European mother-child cohorts. Pediatr Res [Internet]. 2017 Sep;82(3):429–437. Available from: http://dx.doi.org/10.1038/pr.2017.50 PMID: 28288144
- Duntas LH. Chemical contamination and the thyroid. Endocrine [Internet]. 2015 Feb;48(1):53–64. Available from: http://dx.doi.org/10.1007/s12020-014-0442-4 PMID: 25294013
- Yoon S-J, Choi S-R, Kim D-M, Kim J-U, Kim K-W, Ahn C-W, Cha B-S, Lim S-K, Kim K-R, Lee H-C, Huh K-B. The effect of iodine restriction on thyroid function in patients with hypothyroidism due to Hashimoto’s thyroiditis. Yonsei Med J [Internet]. 2003 Apr 30;44(2):227–235. Available from: http://dx.doi.org/10.3349/ymj.2003.44.2.227 PMID: 12728462
- Tajiri J, Higashi K, Morita M, Umeda T, Sato T. Studies of hypothyroidism in patients with high iodine intake. J Clin Endocrinol Metab [Internet]. 1986 Aug;63(2):412–417. Available from: http://dx.doi.org/10.1210/jcem-63-2-412 PMID: 3722332
- Kasagi K, Iwata M, Misaki T, Konishi J. Effect of iodine restriction on thyroid function in patients with primary hypothyroidism. Thyroid [Internet]. 2003 Jun;13(6):561–567. Available from: http://dx.doi.org/10.1089/105072503322238827 PMID: 12930600
- Livadas S, Bothou C, Androulakis I, Boniakos A, Angelopoulos N, Duntas L. Levothyroxine Replacement Therapy and Overuse: A Timely Diagnostic Approach. Thyroid [Internet]. 2018 Nov 30; Available from: http://dx.doi.org/10.1089/thy.2018.0014 PMID: 30351232
- Ejtahed H-S, Angoorani P, Soroush A-R, Siadat S-D, Shirzad N, Hasani-Ranjbar S, Larijani B. Our Little Friends with Big Roles: Alterations of the Gut Microbiota in Thyroid Disorders. Endocr Metab Immune Disord Drug Targets [Internet]. 2020;20(3):344–350. Available from: http://dx.doi.org/10.2174/1871530319666190930110605 PMID: 31566142
- Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function? Nutrients [Internet]. 2020 Jun 12;12(6). Available from: http://dx.doi.org/10.3390/nu12061769 PMCID: PMC7353203
- Caturegli P, De Remigis A, Rose NR. Hashimoto thyroiditis: clinical and diagnostic criteria. Autoimmun Rev [Internet]. 2014 Apr;13(4-5):391–397. Available from: http://dx.doi.org/10.1016/j.autrev.2014.01.007 PMID: 24434360





Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!