Everything You Need To Know About Histamine Intolerance
Causes of Histamine Intolerance and How to Overcome It
- What Is Histamine|
- Symptoms|
- Histamine Intolerance & Your Gut|
- Testing|
- Treating Histamine Intolerance|
- Low-Histamine Diet|
- Probiotics|
- Other Supplements|
- The Bottom Line|
You probably know that histamine symptoms like hay fever, hives, and itching can be caused by seasonal or environmental allergies to things like pollen or animal dander. But you might not know that digestive and allergic symptoms can also be caused by histamine intolerance — a food intolerance triggered by histamine-rich food and drinks.
Histamine intolerance affects approximately 1% of Americans 1. Women are more likely to develop histamine intolerance than men 2 3, and a surprising 30-55% of people with digestive symptoms or conditions like IBS, IBD, and Crohn’s disease have it 4.
Let’s discuss what histamine intolerance is, what causes and triggers it, how it’s connected to gut health, and how to overcome it.

What Is Histamine, and What Does It Do?
Histamine is a naturally occurring organic chemical that is produced in your body. High amounts of histamine are also present in certain foods, such as red wine, fermented foods, and aged meats and cheeses.
When your body is exposed to an allergen, like pollen or dust, histamine is released from MAST cells, which are immune cells that travel the body looking for allergens. This release of histamine directs your body to mobilize a white blood cell immune response to neutralize the threat.
When the immune system releases histamine in your tissues, you may experience allergy symptoms, such as itchy eyes, skin rashes, inflammation, or in extreme cases, life-threatening anaphylaxis.
Histamine is also a brain neurotransmitter and it’s also part of the complex series of biochemical reactions that release stomach acid 5, so a certain amount of histamine helps your body function normally.
Histamine intolerance is primarily an issue with excess histamine in the digestive tract, which can develop from gut imbalances.
Histamine Intolerance Symptoms
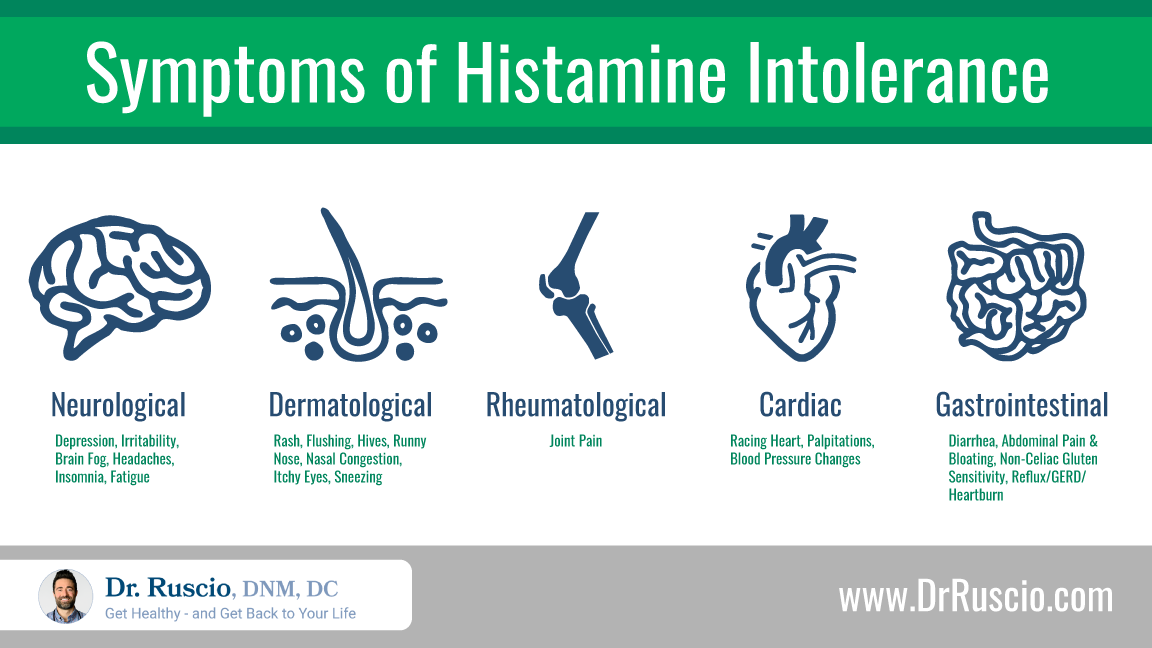
The common symptoms of histamine intolerance are broad, affecting not just the digestive tract, but also the skin, brain, joints, and heart. You might be familiar with the itchy eyes, runny nose, nasal congestion, skin flushing, hives, or sneezing that come with seasonal allergies, 6 and these symptoms can also happen with histamine intolerance. High levels of histamine can also trigger digestive symptoms like bloating 7, and diarrhea 8, heart rate changes or palpitations 9, low blood pressure 10, and headaches 11.
Histamine Intolerance and Your Gut
Histamine intolerance results from an excess of histamine in the digestive system where sensitivity to high histamine foods causes both digestive and non-digestive symptoms. This sensitivity often results from poor gut health.
Histamine in the non-digestive tissues is cleared by the enzyme HNMT, but histamine in the digestive system — from bacteria, food, drinks, or an immune response to food allergens — is broken down by the DAO (diamine oxidase) enzyme 12. If your levels of DAO enzyme are low, a build-up of histamine levels in your digestive system can cause histamine symptoms.
There are several possible underlying causes for an increase of histamine in the digestive tract or a decrease of DAO enzyme levels.
Dysbiosis & SIBO
The digestive tract is full of histamine receptors, and the expression of these histamine receptors is often altered in people with gastrointestinal diseases 13.
One study suggested that inflammation and intestinal permeability (leaky gut) caused by bacterial imbalance were likely involved in histamine intolerance 14. Another study showed that 30%-55% of people with digestive symptoms also have histamine intolerance 15. Bacteria produce histamine, so an overgrowth of bacteria contributes to histamine load.
SIBO (small intestinal bacterial overgrowth) is a specific type of dysbiosis that damages the lining of the small intestine and may trigger the loss of tolerance to dietary histamine 16. SIBO symptoms overlap significantly with histamine intolerance symptoms 17, indicating that at least some portion of histamine intolerance cases are related to SIBO.
Low Levels of DAO Enzyme
The DAO enzyme is responsible for breaking down histamine in the digestive tract. Low DAO activity can lead to excess histamine and histamine intolerance symptoms. Low DAO levels have been associated with two Inflammatory Bowel Disease conditions — Crohn’s disease and ulcerative colitis 18 19 — and histamine intolerance is associated with leaky gut 20.
Genetics also play an important role in levels of DAO enzyme. Some people have variations in the genes that affect DAO enzyme function. If those gene variants are turned on, that person may be less efficient at breaking down dietary histamine due to a shortage of DAO enzyme 21.
Hormone Fluctuations
Some women notice that their histamine intolerance symptoms are worse during certain parts of their menstrual cycle. This may be one reason why histamine intolerance is more common for women than men 22 23. Several studies suggest that estrogen fluctuations may decrease the amount of DAO enzyme available to help break down histamine 24 25 26.
Over-Consuming Histamine Foods or DAO-Blockers
If you eat lots of high-histamine foods, or foods the block DAO, such as alcohol 27, or black or green tea, your levels of histamine may exceed your ability to break down histamine. When levels of histamine build-up, either due to eating high-histamine foods or reduced DAO action in the gut, histamine symptoms occur.
In your unique situation, there is likely not one particular cause, but a perfect storm of causes and triggers that tips the balance toward histamine intolerance.
One way this can happen is when people shift to a healthier diet but include high amounts of high histamine foods, like spinach, avocados, sauerkraut, and kombucha. These are all perfectly healthy foods. But if you already have a brewing histamine problem close to the tipping point, suddenly increasing them could lead to histamine symptoms.
How To Test for Histamine Intolerance
There’s no clear-cut test for histamine intolerance. Avoid getting pulled into the thinking that you need expensive testing to sort this problem out. That said, there are several options that provide at least partial answers.
The most accurate test would be a positive response to a low-histamine diet. If your symptoms resolve on a low-histamine diet and return with the reintroduction of high-histamine foods, this highly suggests your symptoms are caused by histamine intolerance.
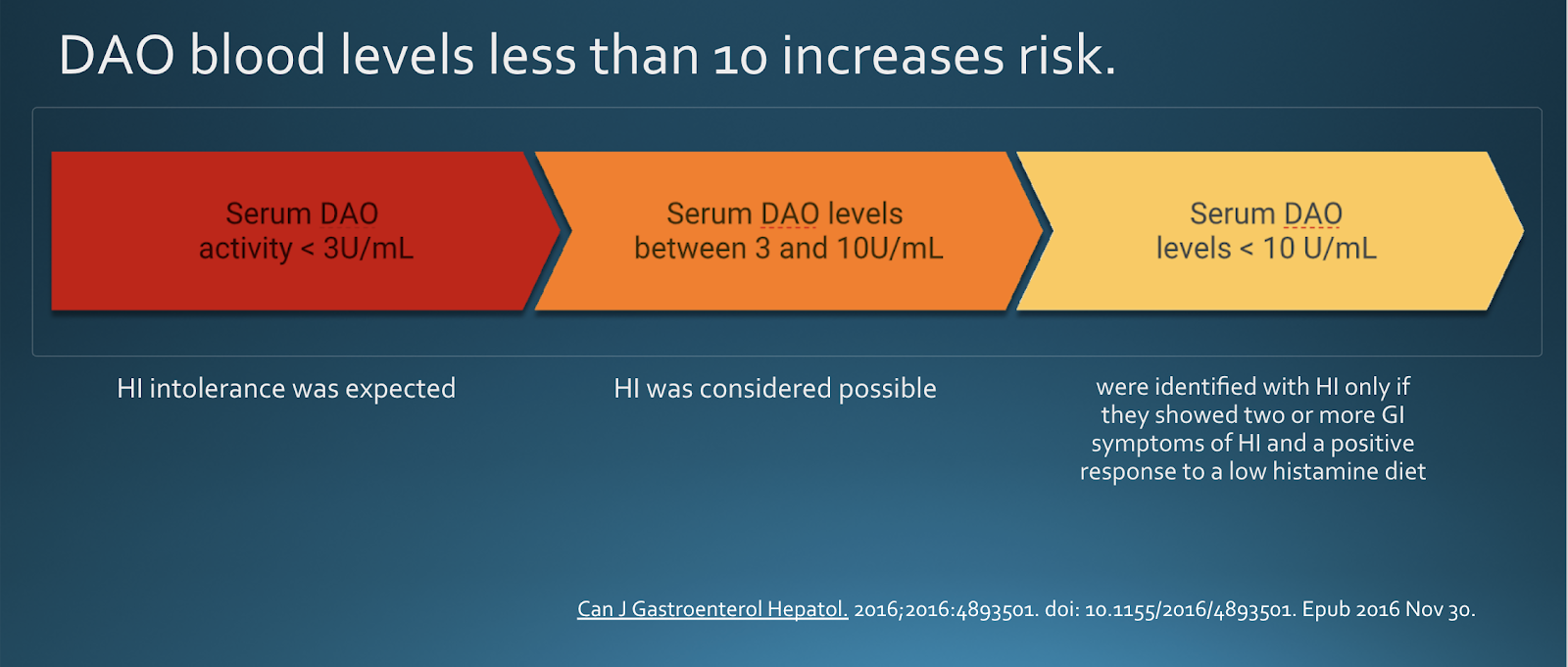
Testing serum DAO levels may also help diagnose histamine intolerance. Research suggests serum DAO levels correlate with histamine intolerance symptoms 28 29 30. In one study, DAO levels below 10 U/ml were shown to increase the risk of histamine intolerance, especially in people who also showed digestive symptoms and responded to a low histamine diet 31.
Similar to a histamine elimination diet, doing a trial with a DAO supplement may give you good information. If your symptoms subside when using DAO, that’s a sign that histamine intolerance is the cause of your symptoms.
Allergy tests, like the skin prick tests offered by allergists, check for IgE-mediated allergies to things like dust, pollen, or certain foods. Positive results on skin prick tests do not indicate intolerance to histamine foods. People with histamine symptoms but negative results on a skin prick test may still find relief from a low-histamine diet.
Treating Histamine Intolerance: Diet, Probiotics, & Supplements
A low histamine diet, coupled with a DAO enzyme and gut health support is the best option available to help you reduce your histamine burden and resolve histamine intolerance symptoms.
Eating a basic, anti-inflammatory diet to avoid common food sensitivities and additives is one of the first steps to take to repair your gut health. The paleo diet is a good, basic option.
Low-Histamine Diet
If you continue to have histamine symptoms on a basic healing diet, adapt that diet to the low-histamine diet. A low-histamine diet has been shown to reduce or eliminate histamine intolerance symptoms 32, and to increase levels of DAO enzyme 33. Eliminate high histamine foods for 2-3 weeks and assess your symptoms. If they haven’t changed, chances are histamine isn’t the cause.
If you do experience relief on the low-histamine diet, you can slowly reintroduce histamine foods to try and discover your unique tolerance threshold.
High-Histamine Foods
Histamine in food is produced by bacteria and yeast as they break the amino acid histidine down into histamine. This means that fermented foods, or foods made with yeast, like alcohol or vinegar, are higher in histamine than other foods. Histamine liberators, like citrus fruits or energy drinks, may also need to be avoided.
In addition to high-histamine foods, a key thing to avoid during a low-histamine diet is leftovers. Histamine levels in protein-rich leftovers, like meat dishes, or raw meat and fish, increase the longer they are stored in the refrigerator. Store leftovers in the freezer, and cook or freeze raw meat quickly to avoid high histamine levels.
For your reference, here is a partial list of histamine-rich foods to avoid on a low-histamine diet. For a more complete list, see our Histamine Diet mini eBook.
- Alcoholic beverages of any kind (especially red wine)
- Certain fruits and vegetables, including avocado, dried fruits, eggplant, spinach, and tomatoes, and ketchup
- Fermented meat and dairy products, including aged cheeses, salami, sausages, and pepperoni
- Fermented foods, including kombucha, water kefir, kimchi, sauerkraut, pickles, miso, natto, soy sauce, tamari, coconut aminos, liquid aminos, and vinegars
- Fish and seafood, particularly tuna or mackerel, especially if left over, smoked, salted, or canned, or not gutted and frozen immediately after harvest 34
- Tea (black, green, white, or yerba mate tea)
- Yeast products
Low-Histamine Foods
There are plenty of delicious foods to eat on a low-histamine diet. Build healthy, simple, and tasty menus centered around:
- Fresh meat and lower histamine fish
- Gluten-free grains like rice, quinoa, or millet
- Fresh vegetables like lettuce, cucumbers, zucchini, kale, onions, green beans, peppers, or sweet potatoes
- Fresh fruits like apples, blueberries, kiwis, or pears
- Healthy fats like olive oil, butter, ghee, coconut oil, or coconut milk
- Herbal teas
See How to Use a Low Histamine Diet for Histamine Intolerance for more detailed information.
Probiotics for Histamine Intolerance
The low-histamine diet, DAO enzymes, and antihistamine medications can help reduce histamine intolerance symptoms, but one study showed that once DAO supplementation was stopped, the symptoms returned 35. Probiotics are one strategy for resolving the underlying dysbiosis that may be increasing inflammation, damaging the small intestinal lining, and reducing DAO levels.
There is some controversy about whether or not probiotics improve histamine intolerance. We don’t have direct research that shows probiotics improve histamine intolerance, but we do have evidence that probiotics benefit immune- and histamine-mediated conditions.
Research suggests that probiotics actually lower histamine levels in the digestive tract 36.
Research clearly shows that probiotics reduce gut inflammation and help resolve infections that increase histamine intolerance, such as SIBO 37 38 39, as well as bacterial and parasitic infections 40 41 42 43. Probiotics have also been shown to benefit histamine-mediated conditions, such as seasonal allergies 44 45, non-allergic rhinitis 46, and eczema and asthma 47 48 49. Though the specific mechanism has not been demonstrated in studies, these data suggest that probiotics can help mediate histamine symptoms.
Some suggest the need to take special, “low-histamine” probiotics. This isn’t necessary because probiotics appear to be net-antihistamine. Including a quality probiotic from each of the three main categories — Lactobacillus and Bifidobacteria blends, Saccharomyces boulardii, and soil-based probiotics — is an effective strategy to improve histamine intolerance. For more on how to use probiotics, see our Probiotics Starter Guide.
Other Supplements To Help Histamine Intolerance
Vitamin B6 is an important cofactor for the efficient function of the DAO enzyme. Several studies demonstrated that vitamin B6 supplementation helps reduce symptoms of histamine intolerance, suggesting that B6 deficiency may reduce levels of DAO enzyme 50 51 52.
Quercetin is a plant flavonoid that has demonstrated an antihistamine and anti-inflammatory effect and may help reduce histamine intolerance symptoms 53 54 55.
Vitamin C has been shown to reduce serum histamine levels 56, and is known to have antihistamine properties 57. Supplemental vitamin C may help you manage your symptoms of histamine intolerance while you work on the underlying causes.
The Bottom Line
Digestive, allergic, and neurological symptoms may be caused by histamine intolerance, which is a loss of your body’s ability to properly break down dietary histamine. Testing your response to a low-histamine diet or a DAO supplement can help you determine if histamine intolerance is the cause of these symptoms. Probiotics can improve the gut dysbiosis and inflammation that is likely causing your histamine intolerance.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Kohn JB. Is there a diet for histamine intolerance? J Acad Nutr Diet. 2014 Nov;114(11):1860. doi: 10.1016/j.jand.2014.09.009. Epub 2014 Oct 24. PMID: 25439083.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Reinhart Jarisch. Histamine Intolerance: Histamine and Seasickness
- Enko D, Meinitzer A, Mangge H, Kriegshäuser G, Halwachs-Baumann G, Reininghaus EZ, Bengesser SA, Schnedl WJ. Concomitant Prevalence of Low Serum Diamine Oxidase Activity and Carbohydrate Malabsorption. Can J Gastroenterol Hepatol. 2016;2016:4893501. doi: 10.1155/2016/4893501. Epub 2016 Nov 30. PMID: 28042564; PMCID: PMC5155086.
- Prinz C, Zanner R, Gerhard M, Mahr S, Neumayer N, Höhne-Zell B, Gratzl M. The mechanism of histamine secretion from gastric enterochromaffin-like cells. Am J Physiol. 1999 Nov;277(5):C845-55. doi: 10.1152/ajpcell.1999.277.5.C845. PMID: 10564076.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Schnedl WJ, Lackner S, Enko D, Schenk M, Holasek SJ, Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intest Res. 2019 Jul;17(3):427-433. doi: 10.5217/ir.2018.00152. Epub 2019 Mar 7. PMID: 30836736; PMCID: PMC6667364.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Wöhrl S, Hemmer W, Focke M, Rappersberger K, Jarisch R. Histamine intolerance-like symptoms in healthy volunteers after oral provocation with liquid histamine. Allergy Asthma Proc. 2004 Sep-Oct;25(5):305-11. PMID: 15603203.
- Izquierdo-Casas J, Comas-Basté O, Latorre-Moratalla ML, Lorente-Gascón M, Duelo A, Soler-Singla L, Vidal-Carou MC. Diamine oxidase (DAO) supplement reduces headache in episodic migraine patients with DAO deficiency: A randomized double-blind trial. Clin Nutr. 2019 Feb;38(1):152-158. doi: 10.1016/j.clnu.2018.01.013. Epub 2018 Feb 15. PMID: 29475774.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Sander LE, Lorentz A, Sellge G, Coëffier M, Neipp M, Veres T, Frieling T, Meier PN, Manns MP, Bischoff SC. Selective expression of histamine receptors H1R, H2R, and H4R, but not H3R, in the human intestinal tract. Gut. 2006 Apr;55(4):498-504. doi: 10.1136/gut.2004.061762. Epub 2005 Nov 18. PMID: 16299042; PMCID: PMC1856162.
- Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol. 2018 Aug;69(4). doi: 10.26402/jpp.2018.4.09. Epub 2018 Dec 9. PMID: 30552302.
- Enko D, Meinitzer A, Mangge H, Kriegshäuser G, Halwachs-Baumann G, Reininghaus EZ, Bengesser SA, Schnedl WJ. Concomitant Prevalence of Low Serum Diamine Oxidase Activity and Carbohydrate Malabsorption. Can J Gastroenterol Hepatol. 2016;2016:4893501. doi: 10.1155/2016/4893501. Epub 2016 Nov 30. PMID: 28042564; PMCID: PMC5155086.
- Lappinga PJ, Abraham SC, Murray JA, Vetter EA, Patel R, Wu TT. Small intestinal bacterial overgrowth: histopathologic features and clinical correlates in an underrecognized entity. Arch Pathol Lab Med. 2010 Feb;134(2):264-70. doi: 10.1043/1543-2165-134.2.264. PMID: 20121616.
- Bures J, Cyrany J, Kohoutova D, Förstl M, Rejchrt S, Kvetina J, Vorisek V, Kopacova M. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010 Jun 28;16(24):2978-90. doi: 10.3748/wjg.v16.i24.2978. PMID: 20572300; PMCID: PMC2890937.
- Schmidt WU, Sattler J, Hesterberg R, Röher HD, Zoedler T, Sitter H, Lorenz W. Human intestinal diamine oxidase (DAO) activity in Crohn’s disease: a new marker for disease assessment? Agents Actions. 1990 Apr;30(1-2):267-70. doi: 10.1007/BF01969057. PMID: 2115243.
- Raithel M, Matek M, Baenkler HW, Jorde W, Hahn EG. Mucosal histamine content and histamine secretion in Crohn’s disease, ulcerative colitis and allergic enteropathy. Int Arch Allergy Immunol. 1995 Oct;108(2):127-33. doi: 10.1159/000237129. PMID: 7549499.
- Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol. 2018 Aug;69(4). doi: 10.26402/jpp.2018.4.09. Epub 2018 Dec 9. PMID: 30552302.
- Maintz L, Yu CF, Rodríguez E, Baurecht H, Bieber T, Illig T, Weidinger S, Novak N. Association of single nucleotide polymorphisms in the diamine oxidase gene with diamine oxidase serum activities. Allergy. 2011 Jul;66(7):893-902. doi: 10.1111/j.1398-9995.2011.02548.x. Epub 2011 Apr 13. PMID: 21488903.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Reinhart Jarisch. Histamine Intolerance: Histamine and Seasickness
- Bonds RS, Midoro-Horiuti T. Estrogen effects in allergy and asthma. Curr Opin Allergy Clin Immunol. 2013 Feb;13(1):92-9. doi: 10.1097/ACI.0b013e32835a6dd6. PMID: 23090385; PMCID: PMC3537328.
- Jing H, Wang Z, Chen Y. Effect of oestradiol on mast cell number and histamine level in the mammary glands of rat. Anat Histol Embryol. 2012 Jun;41(3):170-6. doi: 10.1111/j.1439-0264.2011.01120.x. Epub 2011 Nov 24. PMID: 22112012.
- Vasiadi M, Kempuraj D, Boucher W, Kalogeromitros D, Theoharides TC. Progesterone inhibits mast cell secretion. Int J Immunopathol Pharmacol. 2006 Oct-Dec;19(4):787-94. doi: 10.1177/039463200601900408. PMID: 17166400.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Mušič E, Korošec P, Šilar M, Adamič K, Košnik M, Rijavec M. Serum diamine oxidase activity as a diagnostic test for histamine intolerance. Wien Klin Wochenschr. 2013 May;125(9-10):239-43. doi: 10.1007/s00508-013-0354-y. Epub 2013 Apr 12. PMID: 23579881.
- Manzotti G, Breda D, Di Gioacchino M, Burastero SE. Serum diamine oxidase activity in patients with histamine intolerance. Int J Immunopathol Pharmacol. 2016 Mar;29(1):105-11. doi: 10.1177/0394632015617170. Epub 2015 Nov 16. PMID: 26574488; PMCID: PMC5806734.
- Enko D, Meinitzer A, Mangge H, Kriegshäuser G, Halwachs-Baumann G, Reininghaus EZ, Bengesser SA, Schnedl WJ. Concomitant Prevalence of Low Serum Diamine Oxidase Activity and Carbohydrate Malabsorption. Can J Gastroenterol Hepatol. 2016;2016:4893501. doi: 10.1155/2016/4893501. Epub 2016 Nov 30. PMID: 28042564; PMCID: PMC5155086.
- Son JH, Chung BY, Kim HO, Park CW. A Histamine-Free Diet Is Helpful for Treatment of Adult Patients with Chronic Spontaneous Urticaria. Ann Dermatol. 2018 Apr;30(2):164-172. doi: 10.5021/ad.2018.30.2.164. Epub 2018 Feb 21. PMID: 29606813; PMCID: PMC5839887.
- Lackner S, Malcher V, Enko D, Mangge H, Holasek SJ, Schnedl WJ. Histamine-reduced diet and increase of serum diamine oxidase correlating to diet compliance in histamine intolerance. Eur J Clin Nutr. 2019 Jan;73(1):102-104. doi: 10.1038/s41430-018-0260-5. Epub 2018 Jul 18. PMID: 30022117.
- Rahmani J, Miri A, Mohseni-Bandpei A, Fakhri Y, Bjørklund G, Keramati H, Moradi B, Amanidaz N, Shariatifar N, Khaneghah AM. Contamination and Prevalence of Histamine in Canned Tuna from Iran: A Systematic Review, Meta-Analysis, and Health Risk Assessment. J Food Prot. 2018 Dec;81(12):2019-2027. doi: 10.4315/0362-028X.JFP-18-301. PMID: 30476444.
- Schnedl WJ, Schenk M, Lackner S, Enko D, Mangge H, Forster F. Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food Sci Biotechnol. 2019 May 24;28(6):1779-1784. doi: 10.1007/s10068-019-00627-3. PMID: 31807350; PMCID: PMC6859183.
- Toh ZQ, Anzela A, Tang ML, Licciardi PV. Probiotic therapy as a novel approach for allergic disease. Front Pharmacol. 2012 Sep 21;3:171. doi: 10.3389/fphar.2012.00171. PMID: 23049509; PMCID: PMC3448073.
- Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017 Apr;51(4):300-311. doi: 10.1097/MCG.0000000000000814. PMID: 28267052.
- Soifer LO, Peralta D, Dima G, Besasso H. Eficacia comparativa de un probiótico vs un antibiótico en la respuesta clínica de pacientes con sobrecrecimiento bacteriano del intestino y distensión abdominal crónica funcional: un estudio piloto [Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study]. Acta Gastroenterol Latinoam. 2010 Dec;40(4):323-7. Spanish. PMID: 21381407.
- Leventogiannis K, Gkolfakis P, Spithakis G, Tsatali A, Pistiki A, Sioulas A, Giamarellos-Bourboulis EJ, Triantafyllou K. Effect of a Preparation of Four Probiotics on Symptoms of Patients with Irritable Bowel Syndrome: Association with Intestinal Bacterial Overgrowth. Probiotics Antimicrob Proteins. 2019 Jun;11(2):627-634. doi: 10.1007/s12602-018-9401-3. Erratum in: Probiotics Antimicrob Proteins. 2018 Mar 28;: PMID: 29508268; PMCID: PMC6541575.
- Eslami M, Yousefi B, Kokhaei P, Jazayeri Moghadas A, Sadighi Moghadam B, Arabkari V, Niazi Z. Are probiotics useful for therapy of Helicobacter pylori diseases? Comp Immunol Microbiol Infect Dis. 2019 Jun;64:99-108. doi: 10.1016/j.cimid.2019.02.010. Epub 2019 Mar 5. PMID: 31174707.
- Demirel G, Celik IH, Erdeve O, Saygan S, Dilmen U, Canpolat FE. Prophylactic Saccharomyces boulardii versus nystatin for the prevention of fungal colonization and invasive fungal infection in premature infants. Eur J Pediatr. 2013 Oct;172(10):1321-6. doi: 10.1007/s00431-013-2041-4. Epub 2013 May 24. PMID: 23703468.
- Dinleyici EC, Eren M, Dogan N, Reyhanioglu S, Yargic ZA, Vandenplas Y. Clinical efficacy of Saccharomyces boulardii or metronidazole in symptomatic children with Blastocystis hominis infection. Parasitol Res. 2011 Mar;108(3):541-5. doi: 10.1007/s00436-010-2095-4. Epub 2010 Oct 5. PMID: 20922415.
- Besirbellioglu BA, Ulcay A, Can M, Erdem H, Tanyuksel M, Avci IY, Araz E, Pahsa A. Saccharomyces boulardii and infection due to Giardia lamblia. Scand J Infect Dis. 2006;38(6-7):479-81. doi: 10.1080/00365540600561769. PMID: 16798698.
- Güvenç IA, Muluk NB, Mutlu FŞ, Eşki E, Altıntoprak N, Oktemer T, Cingi C. Do probiotics have a role in the treatment of allergic rhinitis? A comprehensive systematic review and meta-analysis. Am J Rhinol Allergy. 2016 Sep 1;30(5):157-175. doi: 10.2500/ajra.2016.30.4354. Epub 2016 Jul 20. PMID: 27442711.
- Dennis-Wall JC, Culpepper T, Nieves C Jr, Rowe CC, Burns AM, Rusch CT, Federico A, Ukhanova M, Waugh S, Mai V, Christman MC, Langkamp-Henken B. Probiotics (Lactobacillus gasseri KS-13, Bifidobacterium bifidum G9-1, and Bifidobacterium longum MM-2) improve rhinoconjunctivitis-specific quality of life in individuals with seasonal allergies: a double-blind, placebo-controlled, randomized trial. Am J Clin Nutr. 2017 Mar;105(3):758-767. doi: 10.3945/ajcn.116.140012. Epub 2017 Feb 22. PMID: 28228426.
- Gelardi M, De Luca C, Taliente S, Fiorella ML, Quaranta N, Russo C, Ciofalo A, Macchi A, Mancini M, Rosso P, Seccia V, Guagnini F, Ciprandi G. Adjuvant treatment with a symbiotic in patients with inflammatory non-allergic rhinitis. J Biol Regul Homeost Agents. 2017 Jan-Mar;31(1):201-206. PMID: 28337893.
- Yang G, Liu ZQ, Yang PC. Treatment of allergic rhinitis with probiotics: an alternative approach. N Am J Med Sci. 2013 Aug;5(8):465-8. doi: 10.4103/1947-2714.117299. PMID: 24083221; PMCID: PMC3784923.
- Toh ZQ, Anzela A, Tang ML, Licciardi PV. Probiotic therapy as a novel approach for allergic disease. Front Pharmacol. 2012 Sep 21;3:171. doi: 10.3389/fphar.2012.00171. PMID: 23049509; PMCID: PMC3448073.
- Gelardi M, De Luca C, Taliente S, Fiorella ML, Quaranta N, Russo C, Ciofalo A, Macchi A, Mancini M, Rosso P, Seccia V, Guagnini F, Ciprandi G. Adjuvant treatment with a symbiotic in patients with inflammatory non-allergic rhinitis. J Biol Regul Homeost Agents. 2017 Jan-Mar;31(1):201-206. PMID: 28337893.
- Martner-Hewes PM, Hunt IF, Murphy NJ, Swendseid ME, Settlage RH. Vitamin B-6 nutriture and plasma diamine oxidase activity in pregnant Hispanic teenagers. Am J Clin Nutr. 1986 Dec;44(6):907-13. doi: 10.1093/ajcn/44.6.907. PMID: 3098085.
- Hunt IF, Murphy NJ, Martner-Hewes PM, Faraji B, Swendseid ME, Reynolds RD, Sanchez A, Mejia A. Zinc, vitamin B-6, and other nutrients in pregnant women attending prenatal clinics in Mexico. Am J Clin Nutr. 1987 Oct;46(4):563-9. doi: 10.1093/ajcn/46.4.563. PMID: 3661474.
- Jarisch R, Wantke F. Wine and headache. Int Arch Allergy Immunol. 1996 May;110(1):7-12. doi: 10.1159/000237304. PMID: 8645981.
- Mlcek J, Jurikova T, Skrovankova S, Sochor J. Quercetin and Its Anti-Allergic Immune Response. Molecules. 2016 May 12;21(5):623. doi: 10.3390/molecules21050623. PMID: 27187333; PMCID: PMC6273625.
- Weng Z, Zhang B, Asadi S, Sismanopoulos N, Butcher A, Fu X, Katsarou-Katsari A, Antoniou C, Theoharides TC. Quercetin is more effective than cromolyn in blocking human mast cell cytokine release and inhibits contact dermatitis and photosensitivity in humans. PLoS One. 2012;7(3):e33805. doi: 10.1371/journal.pone.0033805. Epub 2012 Mar 28. PMID: 22470478; PMCID: PMC3314669.
- Jafarinia M, Sadat Hosseini M, Kasiri N, Fazel N, Fathi F, Ganjalikhani Hakemi M, Eskandari N. Quercetin with the potential effect on allergic diseases. Allergy Asthma Clin Immunol. 2020 May 14;16:36. doi: 10.1186/s13223-020-00434-0. PMID: 32467711; PMCID: PMC7227109.
- Hagel AF, Layritz CM, Hagel WH, Hagel HJ, Hagel E, Dauth W, Kressel J, Regnet T, Rosenberg A, Neurath MF, Molderings GJ, Raithel M. Intravenous infusion of ascorbic acid decreases serum histamine concentrations in patients with allergic and non-allergic diseases. Naunyn Schmiedebergs Arch Pharmacol. 2013 Sep;386(9):789-93. doi: 10.1007/s00210-013-0880-1. Epub 2013 May 11. PMID: 23666445.
- Johnston CS. The antihistamine action of ascorbic acid. Subcell Biochem. 1996;25:189-213. doi: 10.1007/978-1-4613-0325-1_10. PMID: 8821975.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!