Could Abdominal Adhesions Be Thwarting Your Gut Health?
All about visceral manipulation & massage with Dr. Jason Wysocki.
Sometimes, bands of scar tissue—called adhesions—can form in your body and stick to your organs or tissues, as a result of surgery, trauma, or inflammation. This may cause complications like intestinal blockage, restricted breathing, or difficulty moving muscles. In the gut, SIBO, IBS, IBD, and conditions like hiatal hernia may be influenced by this restriction. Fortunately, a technique called visceral therapy (also known as visceral manipulation and massage) can help. In this episode, a specialist in visceral therapy, Dr. Jason Wysocki, shares his insights about how it works and who is most likely to benefit.
Episode Intro
Dr. Michael Ruscio, DC: Hi everyone, welcome to Dr. Ruscio Radio. This is Dr. Ruscio. Today, I’m here with Dr. Jason Wysocki and we’re going to be talking about visceral therapy. This is a very interesting therapy that we talked about years ago with Larry and Belinda Wurn who are at clearpassage.com. They published a number of papers showing that this type of therapy provided relief to those with inflammation or adhesion or scar tissue in their pelvis which can interfere with stomach and intestinal function. Consider a a garden hose as a kind of crude analogy. If you step on a garden hose, you can occlude the ability of water to flow through the hose. Well, the heel of the shoe would be like the scar tissue that could impede the intestines from allowing material to move through. This is where, for some people, the difference between chronic symptoms and finally being able to get over those symptoms is having this kind of intensive, visceral or abdominal and pelvic massage, to break down some of these scar tissues, adhesions, and “sticky” points. I’m using a lot of general language here but we’ll get into some more specifics in our conversation. If you are struggling with this type of thing, you may need to break down some scar tissue, similar to if you had an injury in your shoulder with scar tissue that finally got worked out. The same thing can actually happen in your intestines, and Jason came highly recommended as someone who is in the clinical trenches doing this day in and day out and I’m just so happy to have him here to give a boots on the ground clinician perspective on how to use this, who to use this with, and also kind of where this fits in to the overall treatment algorithm. Jason, pumped to have you here. Thanks for being on the show.
[Continue reading below]
What is visceral therapy & massage?
- Visceral definition= Abdomen, thorax, organs and fascia intertwined
- Hiatal hernia syndrome, ileocecal valve syndrome, diaphragmatic release
- Massage vs manipulation
- Massage: for maintenance and to soothe
- Manipulation: moving things back into place or releasing the diaphragm for example
- Wurn technique is for abdominal adhesions, a more massage-like technique
- Previous episode with Larry and Belinda Wurn Abdominal Adhesions; an Overlooked Cause of SIBO, IBS, Gut Pain, Infertility and More
How to know if you could need visceral therapy? History, signs, symptoms …
- Prior abdominal or pelvic trauma
- C-section
- Endometriosis
- Appendectomy
- IBD
- Fertility or cycling issues
- Involved in an accident
- Motor vehicle
- Acute injury
- Traumatic Brain Injury
- Emotional trauma
Does it help chronic IBS and SIBO?
- Yes
- Red flag symptoms to watch out for
- Can’t move body parts the way you used to
- Don’t feel a full breath
- Can’t do normal activity
- Feels like food doesn’t move through a part of the body
Addressing the ileocecal valve
- The IC valve cannot just be flipped closed or open (despite what you may read online)
- Areas around the valve can cause problems and can be massaged out to improve function
Published data
- Very little, but this is starting to change
How to find a visceral therapist?
- Ask your practitioner about their training and their philosophy
- You may look for
- Structural integrators that have gone to more advanced training
- Visceral manipulators
- Someone trained in the Barral method
- Maybe Physical Therapists that have gone through advanced training
Where to learn more
In this episode…
Episode Intro … 00:00:40
Viscera and Visceral Manipulation … 00:03:44
The Ileocecal Valve … 00:21:05
Frank, Sliding and Other Hernias … 00:25:07
Finding a Qualified Practitioner … 00:30:32
The Treatment Algorithm … 00:38:42
Available Research … 00:35:22
Episode Wrap-up … 00:44:55
Download this Episode (right click link and ‘Save As’)
Dr. Jason Wysocki, ND: Thanks, Dr. Ruscio. Pleasure to be here and this is definitely a passion of mine that’s been brewing for years, so I love to talk about it and would love to get into it.
DrMR: Let’s tell people a little bit about your background and then we’ll get into all the nitty gritty regarding visceral therapy.
DrJW: Absolutely. I am a naturopathic physician by training. I practice out of Portland, Oregon, and I own the practice 8 Hearts Health & Wellness. Before becoming a naturopathic physician, I was trained in theology and counseling, so I was a counselor and mental health professional for 10 years before going into clinical medical work. My practice encompasses mostly gastrointestinal health, with its tie to mental health, men’s health, and physical medicine. This piece of the viscera and the fascia and movement and function really is at the core of a holistic view of mine that mind/body/spirit has to come together for true health.
What is Viscera and Visceral Manipulation
DrMR: Let’s define some of these terms. When I say visceral, I’m kind of vaguely referring to the abdomen, but for people who maybe don’t know what these terms mean, let’s give them some of the basic definitions to get them up to speed.
DrJW: Visceral manipulation, as a term, came from Dr. Barral who was an osteopath and he viewed visceral manipulation as the subtle movement of the organs in the abdomen, thorax, all of that area. Obviously, his work as an osteopath continues and his training continues, but visceral manipulation is now much wider known and a lot of different people are doing different therapies. How I term viscera is also as mainly the abdomen, thorax, and pretty much the organs and the fascia intertwining there.
There’s this piece that I’ve come to realize from my work with another work by Dr. Ida Rolf, Structural Integration. That the fascia and the viscera and organs in this connection and also with Chinese medicine, it doesn’t just end in the abdomen. An abdominal adhesion, though it can be worked through various techniques in the abdomen, actually has connections to other areas of the body. If that isn’t integrated completely, there could be other dysfunctions down the road or not as much clearing or movement as you would expect from just the visceral manipulation. There are specific visceral manipulations that I do which would be in the abdomen. When I say that, my greatest hits are pretty much the hiatal hernia syndrome, the ileocecal valve syndrome, the Diaphragmatic Release, any type of abdominal thing mainly dealing with the iliacus on both sides, which is pretty much the interior hip muscle and of the rectus femoris on both sides, which would be kind of the front of the leg.
DrMR: Definitely a number of things to kind of dig into here. One thing I’m trying to better understand is the difference between what we could term visceral massage, where you’re kind of massaging as compared to manipulation, which, at least as I understand it from a chiropractic view, would be more of a sudden, quick movement, whereas massage is more of a gradual repetitive movement. Is there any delineation there you want to draw between different applications?
DrJW: I would actually say all of the above, and it really depends on what specific adhesion, what specific place, what specific muscle or complex or fascia or organ that you’re working on. Obviously, just from a philosophical perspective, I actually believe less is more. I always tend to not go for the Grade 5 manipulations in the sense of the sudden jerky, really, really quick movements because I don’t think that that’s what the fascia appreciates just in terms of where it moves.
The difference that I would like to draw between massage and manipulation or fascial work and visceral massage would be that they both technically at some points have a place. The massage is really more of a maintenance thing to pretty much soothe. Maybe if there’s some type of lack of movement or just someone just can’t handle more deep work, this could be a way to kind of get through those first couple layers, get things moving a little bit, or maintain the work that you’ve now moved. That would be more of the massage side of things.
The manipulation side of things would be actually moving like in a hiatal hernia syndrome maneuver, moving the stomach back into place. Bringing it back through that diaphragm where it meets the esophagus, or allowing the liver/gall bladder to be in the right position because there’s been fascial adhesions around it or putting it back into place, or releasing the diaphragm, so someone that has chronically not been able to take a deep breath in, can’t get into rest and digest, stuck in sympathetic tone. You can actually help the diaphragm release so they can finally take a deep breath in. It doesn’t matter how much talk therapy or supplements or whatever else you do. If that diaphragm is stuck, sometimes it just needs to be moved.
DrMR: Are you familiar with the work of Larry and Belinda Wurn and the Clear Passage Technique?
DrJW: Absolutely. Larry and Belinda Wurn are friends. They are wonderful and their work specifically, and this is a really good delineation so we can really pick apart what we’re talking about, their work is specifically abdominal adhesion focused and mainly their work is focused on if there was abdominal surgery or an intestinal obstruction or endometriosis or any of the like, or fallopian tube dysfunction or uterine dysfunction or possibly a burst cyst from an ovary. These are things that would cause an abdominal adhesion that the Wurn Technique, which is very well studied, can actually release and improve. They’re doing 20 to 40 hours of intense abdominal adhesion work. Now, that can fall under the umbrella of what we’re talking about today, but that is very, very, very specialized and very, very focused.
DrMR: From what they have explained to me, it’s more so a massage than a manipulation, but I haven’t had it done first hand, so how does that kind of compare? Or maybe speak to their technique so that people can picture what that looks like in their heads.
DrJW: They’re PTs by training and massage therapists by training, and what they are doing is more of a massage. Very, very focused, very, very precise, and I actually had the privilege of Larry showing me his technique and kind of being at a practitioner training, he showed how he feels the adhesions and maybe what he might do just a little bit to kind of do that. Again, their technique is very patented and they’re wonderful people and they do a very specific thing. It would be, I believe, somewhere between a massage and manipulation, but definitely more on the massage side.
DrMR: I’m sure people are saying, “Okay, this sounds interesting.” How do people know if they could have an issue here? I understand that there are some kind of dead giveaways, If someone has had any type of prior abdominal or pelvic trauma and perhaps endometriosis, C-section, maybe an appendectomy, if they’ve had inflammatory bowel disease, if they’ve had any kind of issue with fertility recycling, or sometimes as an another example, we’ll see women who have, at some point in their cycle usually around ovulation, this pelvic pain, lower right or lower left quadrant kind of inside of their hip bone area. This type of pinpoint pain seems to be something that predicts women who will be a good candidate for some type of visceral therapy work.

Those are just some of the things that I’ve seen. It’s definitely not an exhaustive list, but what would you offer people, either clinician or patient as a guide? Kind of, “Here’s a list of things if you’ve had X, Y, or Z, you may want to consider finding someone who can offer you this kind of therapy”?
DrJW: I agree with your list and would add this. Any type of motor vehicle accident, any type of sports-related injury that didn’t completely heal, any place where something did not go through what we would consider “normal” healing. Even in the process of normal healing sometimes, again, the inflammatory process makes collagen lay down in a different way. That causes a different type of adhesion. Anyone with anything of that nature should probably at least bring that up and allow a clinician that is specialized to see if that may be a part of this process, and we’ll talk more about that in the algorithm later on. Anything of that nature would be looked at. TBIs, traumatic brain injuries of any sort because when I think about fascial manipulation, which is kind of the broader term through visceral manipulation, I kind of see the fascia as a whole body thing.

There could be adhesions in someone’s arm that will affect their migrating motor complex, and I know that that sounds absolutely wild, but I have been humbled and awed at things of that nature, too, because when you think of the fascia as sheets of collagen through the body connecting things, protecting things, communicating things, there’s all this communication between these parts that we don’t quite understand. I hope one day that we do, but right now we’re just trying to help people feel better. The things I would add to that as well on a more mental/emotional/spiritual level would be any type of trauma, whether it be emotional or sexual. There’s a book entitled The Body Remembers and this is something that I have seen, especially in my work because of my training and my incorporation of mental health and these things that this is actually a piece of some people’s healing even for their digestive symptoms as well as their mental health symptoms.
DrMR: A theory there would be that a prior emotional trauma may be kind of held in the tissues and they’re just kind of psychosomatic and one of the ways to heal from the emotional trauma is to address the adhesions in the stomach? Or at least, maybe the psychological issue has been addressed but there’s still these adhesions present as a byproduct and needs to be addressed. Is that kind of what this looks like?
DrJW: Absolutely, and again, very complex topic, but exactly. Something in the body is philosophically holding. This was a survival technique. This is what the body needed to do. It’s kind of the run from the bear, fight the tiger. At that moment, all this stuff happens. That’s a great response. That’s what the body is supposed to do. That’s what the fascia is designed to do, but sometimes something is so over the top that this gets stuck. It gets imprinted and you’re right. There are many ways to go about that because it’s a multifactorial process, but sometimes that needs to be at a purely physiological body level that you allow that to release, and sometimes the rest of the areas get taken care of.
DrMR: What about IBS? I know this is probably opening up a can of worms, but there have been some cases where chronic IBS and SIBO did seem to get over the chronicity when they had some type of visceral therapy. There does seem to be, in most of those cases, something that checks off the list of priors that we just went through. Do you see any kind of substantial percentage of people who check none of those boxes and have chronic IBS and chronic SIBO and this therapy is helpful for them?
DrJW: Yes, and that’s the place where I have to humbly say we don’t fully understand this complete connection of the body. We don’t fully understand the communication of the microbiome. We don’t fully understand how psychoneuroimmunology connects to the migrating motor complex and how the microbiome develops and what species there may be and how that signal gets put through someone’s mental/emotional/spiritual psychosocial place. That piece there for whatever reason, and there’s definitely good philosophy and ancient traditions that speak to this, but for those reasons that box of people sometimes are really helped by these therapies.
Again, I have to say at this point because I am a clinician and a practitioner and there is really no magic bullet, but with things like this, there sometimes comes a place where I look for things that will cause a rising sea that raises all ships. Any impact to outcomes and people’s symptoms and how they feel, if you can improve that tangibly, not esoterically or not by doing specific things to the body and follow that up and that’s maintained, which I have seen time and time again, that’s just something that you can’t discount.

DrMR: This also might be a challenging question, but are there certain ways in which this manifests symptomatically? For example, if someone has some adhesions or some scar tissue or some stuck points in their fascia. Of course, there’s kind of the obvious red flag if someone has very specific kind of pinpoint pain that comes and goes and it’s very localized and it’s always in that one spot. That in my mind is a red flag as compared to someone that just has this transient bloating on and off. It’s very nonspecific, it’s very kind of general. Are there others that you think people should really be surveying their symptoms to see if they may fit the profile?
DrJW: The main thing comes down to movement. Where I really see these things that wouldn’t be obvious, these red flag symptoms we all pick up, but the things that wouldn’t be obvious such as, “I can’t move my right leg the way that I used to anymore. For whatever reason, my hip is just stuck.” Or, “For whatever reason, my shoulder just doesn’t work the way that it used to.” Or, “When I breathe in, it just doesn’t have the same level of breath it used to, it stops right in my epigastrium”, which would be right in the middle right around the bottom of the ribs. “It doesn’t go down to the pelvis, it doesn’t inflate the right way. I can’t move my sacrum, or my tailbone, or my pelvis the way that I used to. I can’t dance anymore.” All of these things. Bringing it more into the digestive sphere, “I just feel something gets stuck somewhere”, and they can actually point to that. Or, “Something just doesn’t move through this part of my body. I eliminate fine, maybe I’m a little bloated, but this part I just feel something.” We try all of our questions. We try to rate them from one to 10. We ask for all of these things and that one place just keeps coming up. These would be areas where someone that’s trained in fascia work, someone that’s trained in removing adhesions and seeing that would be able to see if that is impacting this person’s symptoms or what’s going on.
DrMR: Certainly, I’ve seen patients who remark, “I just feel like gas gets stuck here, stool gets stuck here. Then, I kind of massage it and the gas kind of moves”. I think it’s like that for our audience. That’s a pretty good indication that you may want to track down a visceral therapist.
Sponsored Resources
Hi everyone. I’d like to thank Just Thrive who helped make this podcast possible, and to tell you about their prebiotic, Precision PREbiotic. This contains a blend of three different prebiotics; galacto-oligosaccharides, fructo-oligosaccharides, and xylo-oligosaccharides. These three prebiotics work together to feed your intestinal bacteria.
Now, patients with impaired digestive health should be cautious with prebiotics, but this does not mean that prebiotics should be avoided. Prebiotics have shown the ability to improve digestive symptoms, encourage the growth of healthy bacteria, decrease inflammation, and blood sugar.
So a trial of prebiotics should be included in your gut health plan. This is why I include prebiotics in the Healthy Gut, Healthy You program. If you visit thriveprobiotic.com, you can use the code RUSCIO15, for a 15% off discount, which can be applied to all Just Thrive products. They are also available on Amazon. Check them out.
Ileocecal Valve
DrMR: You mentioned two other things, the IC valve and the hiatal hernia. I’ve struggled with some of the IC valve adjustment techniques. It never really made sense to me that you could adjust, open, or close an IC valve. That to me just seems silly. How you could have this squishy ball of… picture the intestines in the stomach and how much they move around. To think that you could impact a valve in one very specific area with all these things moving. As soon as you go to put some pressure in there, things are going to squirt around like handling a bag of squid. I could see there being adhesions in that region and mobilization, manipulation, any type of massage therapy could help restore movement in the area, movement in the fascia, break down scar tissue. My thinking is some of the docs who purport to be opening or closing the IC valve are just helping to mobilize, and so what they’re describing it as is incorrect, but the therapy ends up being helpful. I am not doing this technique, so despite my reservations I could be overlooking something. What’s your narrative here on the IC valve?
DrJW: I actually agree with you, Dr. Ruscio, in the sense of it would seem that if you’re just pushing on this valve that we’re just trying to figure out why it’s stuck open or why it’s stuck closed, it’s just going to squish around. In terms of what I mean when I address ileocecal valve syndrome, and this is why I call it that, is it’s a multifactorial complex of things, to determine why that area might be having dysfunction. Again, the ileocecal valve is, in most people very, very close to the appendix and you want to definitely think about an appendectomy that went wrong or even a chronic appendicitis that is not going away. Those would just be two things I’d rattle off real quickly. When I think about the ileocecal valve, how I test it, it’s actually at the right iliacus. The right iliacus muscle is really the part that if someone has ileocecal valve dysfunction, I’m going to really be working on that muscle in coordination with the iliopsoas and psoas muscle specifically on the right but balanced on the left, and then the rectus femoris on the right connecting to those different areas to make sure that that whole area of complex is working. Then, I will never forget the diaphragm right above it. You’re exactly correct and you’re very in tune to say that if you just push on this one area, unless there’s an adhesion there and you release it, won’t accomplish much. Remember that sheet of fascia and I’ll just reference really quickly Anatomy Trains and the work of Thomas Myers, just showing that there are lines in the fascia when you dissect the body. Not that that’s the Holy Grail or something that we should wrap everything around, but just understanding that it’s almost like a sheet of Saran Wrap and if there is one area that’s wrinkled, it’s very hard to get anything unraveled until that one area is moved.
I see ileocecal valve as a complex of these areas. If anything is, as you said, squishing on this bag of squid and it shouldn’t be squishing on this bag of squid, putting those things back into proper alignment, function, integration helps possibly rectify ileocecal valve which is stuck closed or open.
DrMR: That makes a lot more sense, kind of taking this more regional approach of the tissues and area and how it might be impacting the ileocecal valve, not too much thinking that you can kind of flip it open or close with just one acute manipulation.
DrJW: No, and I wouldn’t want to do that.
Frank, Sliding and Other Hernias
DrMR: Now, hiatal hernias are also something that’s been kind of a conundrum to me and one of the things that I haven’t had a chance to really dig into the literature regarding is how high the correlation between imaging studies and those that show a positivity for hiatal hernia and any kind of dysfunction. It does seem that at least when I’ve been able to piece together, sometimes that’s thrown out there as an image finding and some of those patients seem to have dysfunction, others don’t.
I do know from my radiology training that at least in certain spine and joint radiology there is not a high correlation between what you see on the imaging findings and someone’s level of pain or dysfunction. I wonder if the same thing is true with a hiatal hernia.
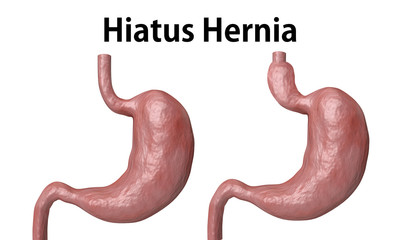
DrJW: What you said is exactly correct in the sense of symptoms and this constellation of symptoms which I’ll go through in a little bit. Do not necessarily correlate with finding on a radiographic study of a frank hiatal hernia. There also aren’t that many frank hiatal hernias, meaning there is an anatomical hiatus where the hiatal hernia comes through…
DrMR: Let’s define that for people in case they haven’t heard that term before.
DrJW: Absolutely. The epigastrium is located in the center of the body, right below the xiphoid process in the center of the thorax. This is where the stomach meets the esophagus. It’s where the lower esophageal sphincter and the diaphragm reside. The stomach is supposed to be below the diaphragm and the esophagus is above it. With a hiatal hernia, a frank one that you would see on an imaging study or an endoscopy, which is the gold standard, you will see the top of the stomach, the fundus of the stomach come through the diaphragm. That can be measured and that is measured as a hiatal hernia.

Now, there are different types of hiatal hernias. There’s the frank one, where it’s there and it’s always there and you can see that on endoscopy. You can see that on imaging. There’s a sliding one that can go up during times of extreme stress or times of extreme bloating or any type of pressure, and that’s why this is correlated with not being able to take a deep breath in, acid reflux at times, and these different constellations of symptoms. The sliding one can go back and forth, so on the imaging you may see it or you may not depending on the time, depending on the position. Then, there’s this other sphere of things which is called hiatal hernia syndrome. Someone has this constellation of symptoms, which can include brain fog, can include all these things, that they don’t have a frank hiatal hernia, but the adjustment helps these symptoms.
What I think is going on there is you’re releasing this whole area, which is the diaphragm, which is the viscera, and it really is putting things back into alignment and structure which allows the body to heal itself and try and move through these things. There’s a bunch of things there and the way that we do a hiatal hernia syndrome maneuver, which is what we call it, is very different from the chiropractic method. It’s similar. Ours is from the lineage of Dr. Ralph Failor. He was a DC/ND that was practicing in this area in the ’50s. It’s very gentle. It’s almost like the homeopathic hiatal hernia syndrome maneuver.
It’s very, very gentle. Very simple tractioning. There’s no real gripping things down and pulling and people screaming. It’s not like that. Most people just maybe feel a slight pressure or a sensation in their throat that things are moving down. What we’re looking for from that is just that someone can have a little bit more room in that area and might be able to take a deeper breath. The truth is that may need to be repeated several times or looked at again, or the actual cause needs to be addressed, which could be SIBO or bloating with the pressure pushing that back up or any type of dysfunction.

DrMR: This begs a good question. It sounds to me like there could be a decent number of people who are doing visceral manipulation or visceral therapy who… I’m trying to choose my words carefully here, who may be using a model that I wouldn’t agree with and may lack some clarity, some refinement. How do you advise people on finding a therapist who, using the hiatal hernia as an example, would potentially use a more gentle maneuver and/or if they’re concerned about their ileocecal valve, and again, for the audience, that’s the valve is the connecting point between the small intestine and the large intestine, so it’s kind of arguably an important anatomical point in the GI. They want to try to find someone who wasn’t going to think about some sort of manipulation to open or close the valve, but rather think about that in a more regional perspective like you did. Where do people go? Is there a certain type of training they should look for? How do they get started?
Finding a Qualified Practitioner
DrJW: That’s probably the most difficult question to answer. I don’t mean to be prideful, but the simple answer is anyone that’s been trained in the way that I have or Dr. Sandberg-Lewis or anyone in kind of the Portland GI area that has been trained in the same way will have that level of training. However, that doesn’t answer your question, so moving beyond that, I really think this asks the bigger question of what practitioners do you trust? Who do you want to partner with for whatever part of the healing journey you’re on? It really begins with a discussion. I really encourage patients to really ask, “What’s your philosophy? What’s your training?” If a practitioner doesn’t want to answer that, that may be an answer in itself.
What’s their philosophy? What’s their training? How they’re going to go about this. Do they even believe in it? That’s actually a huge piece of things, too, because I think this is a partnership. I think this is a partnership between practitioner and patient and especially when you’re going to be doing hands-on therapies, that can be quite intimate, and as we described before, this can be releasing more than just the diaphragm. This could be releasing a previous trauma or something else that’s happened. You want someone that is going to hold that space for you, that you feel you can trust and that can help move those things through for you and that you feel is safe and knowledgeable.
That starts with a discussion and I think most practitioners would be honest and say, “That’s not my level of training”, and possibly move on until you find someone. Definitely, the people that would be more trained in how I’m speaking would be probably structural integrators, at least the ones that have gone to a little bit more advanced training, visceral manipulators possibly in the Barral Method or PTs that have taken that advanced trained. That is just a broad spectrum look, but I have to be honest, it’s a very difficult question. One of my purposes is to really put together a network of people that can help people across the country because I see people by distance and I have patients all over the place. I want people that I can send to and trust, so this is something I think we all need to work on and bring the discussion to a higher place.
DrMR: Regarding published data, have we gotten to the point yet where some of these techniques have been studied a little more rigorously?
DrJW: Unfortunately, no. To some degree, The Fascial Institute and The Rolf Institute are really starting to move forward at least on fascial work. This is the place where, one, we just don’t want to throw things at people or do things quickly. This is based on a lot of ancient techniques. A lot of time has been put into this and Dr. Rolf has developed a system of fascial work that is whole body that she developed in the ’50s and ’60s and she was a PhD biochemist and studied with osteopaths. The osteopathic tradition, the structural integration tradition, the visceral manipulation tradition is really where we’re pulling these from.
Classically, I have to be honest with you, Dr. Ruscio, the studies are actually not bearing out what we want to see and I think that the studies are not showing what we want them to see is because they’re just not focused on the things they need to be focused on for the outcomes that we’re looking for. Normally, they’re going after things and markers like low back pain, not increasing migrating motor complex or the marker of constipation or too quick of a migrating motor complex and diarrhea or bloating. They’re not really looking at those things, unfortunately.
The other piece of that is I think fascial work is in its infancy. It’s really interesting embryologically so that the way that the fascia develops is the connection between the mesoderm and ectoderm, which is the middle growth of things, kind of where the organs and all that stuff grows, and then the nerves. Anyone that does functional digestion is fascinated by the connection between neurology and kind of the organs and how these things move and connect and how it connects to the immune system and the mind-gut connection and the microbiome. I actually think that this piece of things is probably… we’re a little before our time in the sense of working through that and I hope in my lifetime we understand more.
Available Research

DrMR: Well, I do, too. I think it’s so much easier for a given technique to permeate more broadly into the health and medical community when there is that research, but I also know it’s not always as easily said as done. I’m glad to hear that some steps are being taken there and hopefully we’ll have more in the future. Actually, it’s kind of a tangential supporting point. The Wurn Technique, they have published quite a bit that really substantiates, “Hey, this stuff can have a measurable impact on digestion, on recurrence of SIBO, on fertility.” At least there’s some evidence for those who are skeptical, showing that doing something that you may on the surface say, “Well, you have someone rub your belly for a while. How is that going to help X, Y, or Z?” Well, if it’s done in a very particular way and you’re worked up appropriately, we have some evidence being published that shows it can be successful. Hopefully that body of research will really start to bloom here over the next several years or so.
DrJW: Just to give a personal kind of pull to that, I think expanding that research to not just focus on fascia in one area or a particular adhesion, but look more globally in the sense of how this works in the whole body may help expand the research and may help give some more insight into how this communication system works because, again, philosophically, and not to get this too much off topic, Chinese medicine looks at what I believe this fascia system to be as a three heater, or Sanjiao. This is the place where every other organ is monitored by this piece to say whether the temperature is correct, whether the environment is correct, and it checks into that in Chinese medicine. In working this in the right way, whether it be in the abdomen, whether it be in the arm, whether it be in the feet, whether it be in the head, whether it be in the mouth, addressing this helps a rising sea that raises all ships. Admittedly, I am speaking more just clinically rather than research based and that’s not normally where I sit. As a trained naturopathic physician, I kind of read articles for fun, I wish there was more.

It’s kind of one of those things that this was birthed in me from my mentors and teachers, but also from my clinical practice and really coming to a place where patients were following the best I know of science, the most clinically-informed evidence-based research. Doing it all and not getting the results that they wanted. Not living the life that they wanted, so I went back and got this training as a doctor, and again, I was trained in a lot of body work before that but specifically fascia work and now have incorporated more and more in my practice for this specific reason.
The Treatment Algorithm
DrMR: For the person who has been doing let’s say more evidence-based treatments for IBS and/or for SIBO but not getting the traction and the results that they would want to, where do you see this kind of fitting into the larger treatment algorithm? I’ll just quickly give my perspectives here. This wouldn’t be one of the first things that I would try unless someone had some of the clear indicators that we described earlier and/or the warning signs or flags. If those are present, I would still start with frontline therapies, diet, stress, lifestyle, probiotics, maybe antimicrobials, and see if that, as an example, that pinpoint pain that you’re always getting when you’re ovulating, goes away. If it doesn’t and things improve and then regress and improve and regress, or just never really improve too much and you’ve gone through some of the preliminary therapies and you’re floundering, that’s when I see this really having some utility, especially if you have some of those flag signs.
Now, for someone who doesn’t have any of those warning signs or flags, I would still consider this, although I’d want to exhaust more of the available treatments first just because we don’t have the flag that justifies a referral for this earlier in the process. That’s by no means definitive. That’s just kind of the way I’m doing it. I’m curious how you’re positioning this.
DrJW: I have to say that I’m in development on this and I’m just going to be honest with that. I don’t disagree with how your particular view of it is in the sense of looking at this as a piece of the puzzle that I believe should be considered and incorporated, but where? Actually, the true answer that I’m coming to right now in my practice is that I think depends. Like you were saying, if there is one of these signs or someone has been very body oriented or injury oriented or if these red flags are really, really transparent or someone has had like three C-sections, obviously, let’s not put them through three years of antimicrobial treatments and pharmaceutical treatments and elemental diets of all forms or the combination of all of them before we at least consider this.
The other piece of this is where I really wanted and why I went back to do this was specifically to increase the efficacy of prokinetics. This was my onus to get back to do this and I believe that that’s probably classically where it should be in the algorithm is somewhere in the end of the treatment phase and moving into the prevention phase. For those that don’t know what that is, the treatment phase would be addressing either a SIBO, a high methane, or high hydrogen or hydrogen sulfide or one of these things for addressing the constellation of IBS symptoms with many of the evidence-informed approaches and then following that up with prokinetic therapy or prevention therapy, whatever that might be.

Somewhere in there, looking at trying to increase the efficacy of that, trying to extend the time between a possible relapse. That’s where I classically use this, and seeing it coming up in my practice for people that need that extra level of support. That’s when we really jump into the sessions, which I would recommend as like the structural integration 0 approach, which is a whole-body approach. Of course, it addresses the abdomen, but it addresses fascia in the whole body and I could go through that if you’d like me to, but in addition to that, I think add this body of people that have already gone through all these treatments, had multiple relapses and all of these things and they didn’t necessarily have those red flags. Those would be people I would consider. It’s really a three-pronged approach of people that are showing signs, people that are kind of in this middle area that may need some extra support, or those that have really failed most of the other things. Or, not only failed, that’s a harsh word, but they didn’t get the results they wanted.
DrMR: Well, it sounds like we’re generally in agreement there with really trying to kind of individualize when we make the recommendation.
View Dr. Ruscio’s Additional Resources
This has been just a fantastic conversation and I do think this is something that people need to have more on their radar screen. We have published at least one case study in our clinician’s newsletter where we had a huge, almost life-changing level of improvement from referring the patient for visceral therapy. These cases are definitely out there and one of the things that I now incorporate into my paperwork are some questions about prior trauma just to make sure that I am capturing this information in an easy fashion as patients are completing their paperwork. I find that works better and I get more honest answers than me asking in the room and putting them on the spot.
Episode Wrap-Up

I like giving people some time to go through the paperwork and to think through their past and reflect and try to check off, “Yes, there’s been a prior history of abdominal trauma”, either in a C-section, gallbladder removal, appendectomy, uterine fibroids, whatever. We can provide a list for people. Clinicians, that’s one thing you can incorporate in your paperwork to already give yourself that item of visceral therapy in your differential diagnosis and your problems list as something to consider. Having that and then keeping that in mind as you monitor someone through treatment and look at how they progress can make it much easier for that to stick out to you in terms of, “Okay, I’ve got this flag and we’re now three months in”, and they’re really not getting the traction that you would like. Maybe it’s a good time to consider this referral.
Just a note there for clinicians in terms of how I’m integrating this into my flow and the one case study that’s in our newsletter. Jason, is there anything that you want to kind of leave people with in terms of closing thoughts? Also, please repeat your website, your clinic name, anywhere else you want to point people online.
DrJW: Well, absolutely. Thanks again, Dr. Ruscio, for having me on and this has been a great discussion and I hope it’s one of many for different topics and the different applications that we can talk about here. I just want to reiterate that this was born, at least for me, out of trying to find something to help SIBO outcomes, to help functional digestive outcomes, to help irritable bowel disease outcomes, for people that weren’t necessarily responding to conventional therapies. I honestly have been amazed by the responses. Again, there is no golden bullet and I’m a terrible salesman, that’s why I’m not that anymore in my life, so I kind of partner with people, explain these things, and say, “Hey, this is what’s happened.”

I don’t have just one case study, I don’t have just 10, I have dozens of people that I’ve worked on in various ways because sometimes we do the greatest hits, sometimes we do all the sessions, and sometimes we just do some visceral manipulation or different techniques. There’s just a slew of results from that. Quite honestly, I’ve never had anyone say to me that it did not make things slightly better. Did it address the complete symptom? I have many that said yes, and plenty of people that are SIBO free now because they did this. Other people at least have some improvement from this therapy, and of course, that’s why you want someone that has done this for a while, that understands what they’re doing, is safe in their approach, and they’re not just going to bust things apart because that can actually cause more harm than good.
DrMR: That doesn’t sound nice.
DrJW: No, not at all, and again, I’m not sure you can bust fascia apart to be honest. I think it’s more an integration. I think it’s more of a change in the psychoneuroimmunology. I think it’s a multi-faceted approach to do that. Of course, to your point, add diet, lifestyle, the best supplements we know, the best evidence-based approach, it’s kind of a both-and, it’s not an either-or.
DrMR: Sure. No, I think that’s well said. And your website?
DrJW: 8 Hearts Health & Wellness is the clinic I own. I practice in Portland, Oregon. People can find me and my bio and our other wonderful practitioners on 8hearts.org, and just check us out. I have a bunch of podcasts on this exact topic with SIBO and structural integration and visceral work. That could be where someone could get more information, at least to start there, and then of course feel free to reach out to our clinic. We have a wonderful staff that can help and direct and we have just amazing practitioners, so please check us out there.
DrMR: Awesome. Well, Jason, thank you again and to our audience, if any of this resonated, I would definitely look into either working with Dr. Jason or someone at his clinic if they’re able to accommodate you via distance. We’ll try to find some resources regarding the training that he mentioned earlier, someone near you with that type of training and have a conversation and see if they strike you as a reasonable person because this can be a missing part of the puzzle for some cases. Jason, again, thanks a lot. It was a great conversation and I really appreciate what you’re doing.
DrJW: Thanks, Dr. Ruscio, and may I just point out, we actually do have some patients that travel to see us. We do accommodate people that travel to get a really, really close place to have this work done and we try and get that done with their schedule and travel and we try and make that work with the resources and time that they have. That is also an option for some people that that might be something they want to look into. Just to kind of throw that out there that I’m not just leaving it out that they’re going to have to find someone in their area. That is something that we do quite often, actually.
DrMR: It’s great that you have that resource for people because that is such a huge milestone just being able to find a competent provider that you trust and you feel confident in. There you have it, everyone. A great resource to get your adhesions and fascia moving properly so you can get your gut in better shape.
DrJW: Great. Thanks, Dr. Ruscio. I appreciate it.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.What do you think? I would like to hear your thoughts or experience with this.
- Get help using this information to become healthier.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.



Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!