Identifying ‘Silent Reflux’ or LPR Symptoms and Causes
Telltale Signs that You May Have Laryngopharyngeal Reflux (LPR)
- What is LPR|
- LPR Symptoms|
- LPR Causes|
- LPR and GERD|
- LPR, IBS, and the Gut|
- LPR Complications|
- Treating LPR|
- Bottom Line|
- Recommended Products|
Reflux is typically associated with symptoms like heartburn and indigestion, but hoarseness, sore throat, and coughing can also be symptoms of a reflux disorder called laryngopharyngeal reflux (LPR).
Because LPR doesn’t always cause classic symptoms like heartburn, it may go undiagnosed and is commonly referred to as “silent reflux.”
A range of different conditions, including gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), and sleep apnea, have been found to overlap with LPR and may cause or contribute to the disorder.
In this article, we’ll explore the common and sometimes surprising LPR symptoms and what may be causing them.
We’ll also explore LPR’s relationship with gastroesophageal reflux disease (GERD) and IBS, and suggest a few potential treatments and dietary approaches that may help.

What is LPR?
LPR occurs when the contents of the stomach reflux (backflow) into your voice box (your larynx) and your throat (your pharynx).
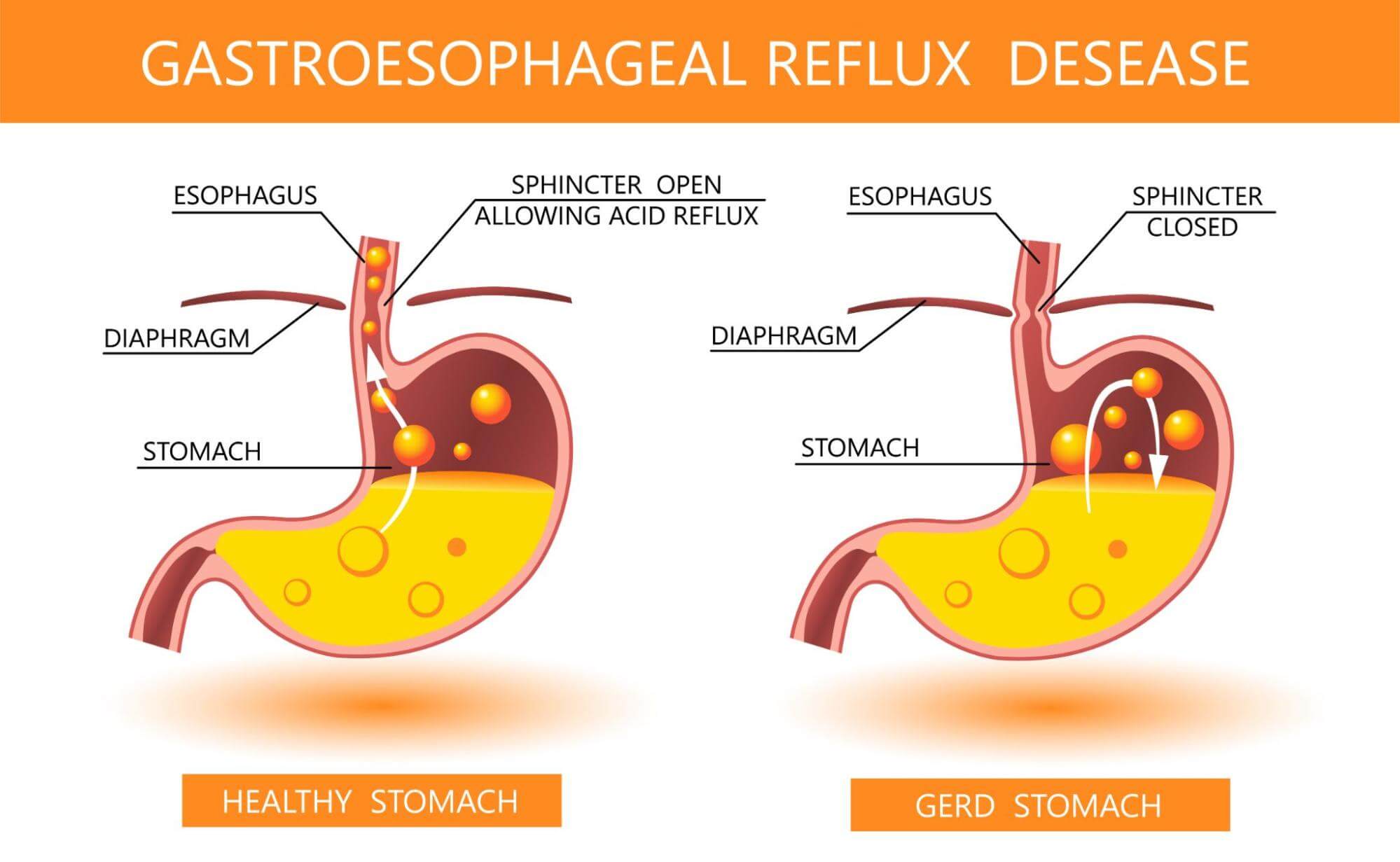
LPR differs from gastroesophageal reflux disease (GERD), in which contents of the stomach come back up into the esophagus but do not necessarily reach the throat.
There are four barriers that should keep reflux from encroaching on your throat and voice box [1]:
| Barrier | What it is and what it does |
| Upper esophageal sphincter | The group of muscles at the top of your esophagus where it joins the pharynx; should only open when swallowing. |
| Lower esophageal sphincter | The group of muscles connecting the esophagus to the stomach, which should prevent stomach acid from entering the esophagus. |
| Esophageal peristalsis | Coordinated contractions that push food and saliva down the esophagus and into the stomach. |
| Epithelial resistance factors | The mucus lining and aqueous layer that line the esophagus, acting as a barrier to large molecules and an acid-neutralizing buffer, respectively. |
Of these four barriers, your upper esophageal sphincter is the final gatekeeper. This sphincter should only open when you’re swallowing, so that food, liquids, and saliva may pass down to your esophagus.
If the esophageal sphincter is dysfunctional, it may remain open, allowing stomach contents to pass up to the larynx and pharynx.
LPR Symptoms

There are a number of different symptoms associated with LPR, most of which are related to the throat. Classic reflux symptoms like heartburn may or may not occur.
LPR symptoms may include:
- Sore throat
- Hoarseness
- Chronic throat clearing
- Chronic cough
- Heartburn
- Regurgitation
- Dysphagia (difficulty swallowing)
- Globus (feeling of a lump in your throat)
Heartburn and Regurgitation
Like most symptoms of LPR, heartburn can be a symptom of many conditions, including GERD, which shares many of LPR’s characteristics. Heartburn is a burning sensation in your chest area that can last for a few minutes or several hours. Heartburn may leave a bitter or sour taste in the back of your throat. Indigestion, a sensation of stomach discomfort, is also common.
Heartburn is a common symptom in North America, with 19.8% of the population reporting heartburn and regurgitation at least weekly [2].
Hoarseness
Hoarseness is one of the most common symptoms of LPR. With hoarseness, your vocal quality may become breathy, harsh, rough, or low-pitched. While hoarseness may be more annoying than painful, it’s an important sign to pay attention to, as it may point to dysfunction within the upper digestive tract.
Chronic Throat Clearing
When your stomach’s contents are refluxing back into your throat, your body’s natural response is to try to clear them out. In your body’s effort to remove that irritation, chronic throat clearing can make matters worse by causing wear and tear on your vocal cords.
The irritation brought on by chronic clearing can also lead to swelling in your throat. This can lead to a build-up of saliva on your throat, resulting in the need for more throat clearing, which can turn into a vicious cycle.
Dysphagia (Difficulty Swallowing)
Dysphagia, or difficulty swallowing, is a common symptom of LPR that may in part be brought on by chronic throat clearing.
In severe cases, dysphagia can lead to malnutrition, weight loss, dehydration, aspiration pneumonia, or choking [3, 4, 5].
Chronic Cough
Laryngopharyngeal reflux may help to explain a mysterious, chronic cough. One small study looked at 28 patients who complained of chronic cough and hadn’t previously been diagnosed with or treated for reflux. The study found that all 28 patients had findings consistent with LPR. After lifestyle changes and reflux medication, 60.7% of them said their symptoms improved [6].
Globus (Lump in Throat)
Globus is a term used to describe the feeling of having a lump in the back of the throat. Globus occurs when swallowing saliva, not when eating or drinking. LPR has been shown to be the most common cause of this symptom, which often occurs alongside chronic throat clearing and/or coughing [7].
What Causes LPR?

From GERD to sleep apnea, research points to many potential causes of LPR. Here are a few of the possible culprits:
Reflux Theory and Reflex Theory
“Reflux theory” and “reflex theory” suggest two different mechanisms by which LPR may occur:
- Reflux theory suggests that your stomach contents are regurgitated all the way back into your throat, directly injuring it [8].
- Reflex theory suggests that acidification occurs in your lower esophagus. Then, it causes LPR-related symptoms in your throat by way of your vagus nerve. The vagus nerve regulates numerous reflex actions, including coughing and swallowing [9, 10].
Sleep Apnea
A systematic review and meta-analysis of 10 studies points to a relationship between people who have obstructive sleep apnea (OSA) and LPR. Of the 870 patients with obstructive sleep apnea observed, 394 (45.2%) also had LPR.
The frequency of sleep apnea occurrences, however, didn’t differ between patients with LPR and those without it [11].
Pepsin
Pepsin is a digestive enzyme that may be involved in the development of LPR. One observational study found that 82% of LPR patients had pepsin in their saliva. However, their pepsin levels weren’t associated with LPR symptoms [12].
An additional review of 18 studies further explains that pepsin in reflux can exacerbate LPR symptoms [13].
Other potential causes of LPR may include:
- Impaired esophageal motility (contractions that should push food and saliva down the esophagus are weaker than normal) [14]
- Hiatal hernia (part of the stomach pushes up into the chest) [15]
- H. pylori infections [16, 17]
Does GERD Cause LPR?
LPR and GERD have a close, but not entirely understood, relationship.
A comprehensive literature review of 18 studies showed that LPR and GERD have several symptoms in common, and that at least 50% of LPR patients have GERD.
While it remains unclear whether or not GERD causes LPR, research has shown that patients with GERD can eventually develop LPR if left untreated [18].
Here’s how LPR and GERD symptoms are alike and how they differ:
| Symptom or Cause | LPR | GERD |
| Hoarseness | Common symptom | Less common symptom |
| Chronic Throat Clearing | Common symptom | Not a common symptom |
| Chronic Cough | Common symptom | Common symptom |
| Heartburn | Less common symptom | Common symptom |
| Regurgitation | Common symptom | Common symptom |
| Difficulty Swallowing | Common symptom | Common symptom |
| Lump in Throat Sensation | Common symptom | Common symptom |
Understanding LPR, IBS, and the Gut

LPR and gut health also share a close relationship, and reflux is a common symptom of irritable bowel syndrome (IBS).
One study involving 6,476 patients found that functional issues in the GI tract were frequent in patients with both GERD and IBS [19]. Another large sample study points to a connection between LPR, GERD, IBS, and depression. These studies suggest that there may be a common underlying cause related to the gut [20].
If IBS and LPR share an underlying gastrointestinal cause, then identifying and resolving the common issue may help to resolve symptoms of both.
Diets that have been shown to help treat IBS, like the low FODMAP diet, may also help with LPR symptoms, especially if they share an underlying cause.
While research hasn’t yet looked at the low FODMAP diet for LPR, some studies have found it to be helpful for reflux symptoms associated with GERD [21, 22].
LPR Complications
LPR can cause long-term irritation and damage if left untreated. Stomach acid that pools in your throat and larynx can lead to chronic vocal injury or scarring of the vocal cords. LPR may also irritate conditions like bronchitis, emphysema, and asthma. Here are a few of the possible complications:
- Chronic Respiratory Conditions: An analysis of 113 patients found LPR “appears to be a major cause of chronic respiratory symptoms” [23].
- Airway reflux and chronic obstructive pulmonary disease (COPD): Two patient studies suggest there may be a connection between LPR and airway reflux and COPD [24, 25].
- Subglottic stenosis: LPR may in rare cases lead to subglottic stenosis, the narrowing of the airway just below the vocal cords. Common symptoms of subglottic stenosis include difficulty breathing or noisy breathing [26].
- Cancer of the larynx: Multiple studies also point to a connection between LPR and cancer of the larynx. However, several factors make this relationship unclear, including the roles of alcohol and tobacco, as well as how frequently reflux is misdiagnosed [27, 28, 29].
Treating LPR

Since the causes and symptoms vary, there currently isn’t a standard LPR treatment. However, there are multiple treatment options available, including some helpful dietary and lifestyle changes.
Dietary Changes for LPR
Multiple studies have been conducted to help identify the correlations between food and beverages and LPR. While there are some foods that may be more likely than others to trigger LPR symptoms, the ideal diet for LPR depends on a number of personal factors. An elimination and reintroduction diet can help you to determine which foods are problematic for you.
An elimination diet may be based on the Paleo diet, which has been shown to reduce inflammation and help with a number of different conditions.
Another strategy is to eliminate the foods and beverages that commonly cause LPR symptoms, including:
Healing Your Gut to Treat LPR
If modifying your diet doesn’t lead to sufficient improvement, the next step is to take a closer look into your gut health.
Small intestinal bacterial overgrowth (SIBO) is one potential culprit. SIBO is often confused with reflux disorders, as it produces gas that can lead to symptoms of reflux. Bacterial overgrowth can also lead to increased stomach acid.
Probiotics may be able to help with LPR. Probiotic therapy has been shown to improve GERD symptoms in multiple studies [32].
Standard Treatments
Standard treatments for LPR may include:
- Proton pump inhibitors (PPIs)
- H2 blockers (antihistamines)
- Antacids
In some cases, a surgical procedure called fundoplication is recommended. This procedure involves wrapping part of the stomach around part of the esophagus in order to keep contents of the stomach from flowing back up.
The Bottom Line
If you have symptoms like a chronic cough, a sore throat that won’t let up, or difficulty swallowing, they may be related to LPR. The key to resolving your symptoms lies in determining their root cause and finding the right treatment plan and diet for you.
For more personalized support with your symptoms, request a consultation at my functional medicine center.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Brown J, Shermetaro C. Laryngopharyngeal Reflux. 2021 Jan 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 30137832.
- Gelardi M, Ciprandi G. Focus on gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR): new pragmatic insights in clinical practice. J Biol Regul Homeost Agents. 2018 Jan-Feb,;32(1 Suppl. 2):41-47. PMID: 29436209.
- Namasivayam AM, Steele CM. Malnutrition and Dysphagia in long-term care: a systematic review. J Nutr Gerontol Geriatr. 2015;34(1):1-21. doi: 10.1080/21551197.2014.1002656. PMID: 25803601.
- Sue Eisenstadt E. Dysphagia and aspiration pneumonia in older adults. J Am Acad Nurse Pract. 2010 Jan;22(1):17-22. doi: 10.1111/j.1745-7599.2009.00470.x. PMID: 20074192.
- Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003 Jul;124(1):328-36. doi: 10.1378/chest.124.1.328. PMID: 12853541.
- Yeakel H, Balouch B, Vontela S, Alnouri G, Sataloff RT. The Relationship Between Chronic Cough and Laryngopharyngeal Reflux. J Voice. 2020 Nov 28:S0892-1997(20)30425-2. doi: 10.1016/j.jvoice.2020.11.011. Epub ahead of print. PMID: 33262000.
- Hamilton NJI, Wilcock J, Hannan SA. A lump in the throat: laryngopharyngeal reflux. BMJ. 2020 Nov 2;371:m4091. doi: 10.1136/bmj.m4091. PMID: 33139245.
-
Determinants of reflux-induced chronic cough
- Barrett C, Patel D, Vaezi M. Laryngopharyngeal Reflux and Atypical Gastroesophageal Reflux Disease. Gastrointestinal Endoscopy Clinics of North America. 2020. Volume 30, Issue 2, Pages 361-376. ISSN 1052-5157, ISBN 9780323754644. https://doi.org/10.1016/j.giec.2019.12.004.
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018 Mar 13;9:44. doi: 10.3389/fpsyt.2018.00044. PMID: 29593576; PMCID: PMC5859128.
- G Magliulo, G Iannella, A Polimeni, M De Vincentiis, G Meccariello, G Gulotta, B Pasquariello, F Montevecchi, A De Vito, G D’Agostino, R Gobbi, G Cammaroto, C Vicini. Laryngopharyngeal reflux in obstructive sleep apnoea patients: Literature review and meta-analysis. American Journal of Otolaryngology. 2018. Volume 39, Issue 6, Pages 776-780. ISSN 0196-0709. https://doi.org/10.1016/j.amjoto.2018.09.006.
- Ah Ra Jung, Oh Eun Kwon, Jung Min Park, Sung Hwa Dong, Su Young Jung, Young Chan Lee, Young-Gyu Eun. Association Between Pepsin in the Saliva and the Subjective Symptoms in Patients With Laryngopharyngeal Reflux. Journal of Voice, PlumX Metrics. 2017. Volume 33, Issue 2, Pages 150-154. DOI: https://doi.org/10.1016/j.jvoice.2017.10.015
- Lechien JR, Akst LM, Hamdan AL, et al. Evaluation and Management of Laryngopharyngeal Reflux Disease: State of the Art Review. Otolaryngology–Head and Neck Surgery. 2019;160(5):762-782. doi:10.1177/0194599819827488
- Passaretti S, Mazzoleni G, Vailati C, Testoni PA. Oropharyngeal acid reflux and motility abnormalities of the proximal esophagus. World J Gastroenterol 2016; 22(40): 8991-8998<br/ ><br/ >Passaretti S, Mazzoleni G, Vailati C, Testoni PA. Oropharyngeal acid reflux and motility abnormalities of the proximal esophagus. World J Gastroenterol 2016; 22(40): 8991-8998 [PMID: 27833390 DOI: 10.3748/wjg.v22.i40.8991]
- Saruç, M., Aksoy, E.A., Vardereli, E. et al. Risk factors for laryngopharyngeal reflux. Eur Arch Otorhinolaryngol 269, 1189–1194 (2012). https://doi.org/10.1007/s00405-011-1905-3
- Campbell R, Kilty SJ, Hutton B, Bonaparte JP. The Role of Helicobacter pylori in Laryngopharyngeal Reflux: A Systematic Review and Meta-analysis. Otolaryngology–Head and Neck Surgery. 2017;156(2):255-262. doi:10.1177/0194599816676052
- Lin, D. and Koskella, B. (2015), Friend and foe: factors influencing the movement of the bacterium Helicobacter pylori along the parasitism–mutualism continuum. Evol Appl, 8: 9-22. https://doi.org/10.1111/eva.12231
- Advances in the diagnosis and management of gastroesophageal reflux disease doi:10.1136/bmj.m3786
- Yarandi SS, Nasseri-Moghaddam S, Mostajabi P, Malekzadeh R. Overlapping gastroesophageal reflux disease and irritable bowel syndrome: Increased dysfunctional symptoms. World J Gastroenterol 2010; 16(10): 1232-1238<br/ ><br/ >Yarandi SS, Nasseri-Moghaddam S, Mostajabi P, Malekzadeh R. Overlapping gastroesophageal reflux disease and irritable bowel syndrome: Increased dysfunctional symptoms. World J Gastroenterol 2010; 16(10): 1232-1238 [PMID: 20222167 DOI: 10.3748/wjg.v16.i9.1232]
- Kamani, T., Penney, S., Mitra, I. et al. The prevalence of laryngopharyngeal reflux in the English population. Eur Arch Otorhinolaryngol 269, 2219–2225 (2012). https://doi.org/10.1007/s00405-012-2028-1
- Austin GL, Thiny MT, Westman EC, Yancy WS Jr, Shaheen NJ. A very low-carbohydrate diet improves gastroesophageal reflux and its symptoms. Dig Dis Sci. 2006 Aug;51(8):1307-12. doi: 10.1007/s10620-005-9027-7. Epub 2006 Jul 27. PMID: 16871438.
- Yancy WS Jr, Provenzale D, Westman EC. Improvement of gastroesophageal reflux disease after initiation of a low-carbohydrate diet: five brief case reports. Altern Ther Health Med. 2001 Nov-Dec;7(6):120, 116-9. PMID: 11712463.
- K.M. Nowak. Laryngopharyngeal Reflux as a Major Cause of Chronic Respiratory Symptoms and Asthma Mimic among Community Health Center Patients. The Journal of Allergy and Clinical Immunology. 2009. Volume 123, Issue 2, S85. DOI:https://doi.org/10.1016/j.jaci.2008.12.298
- Molyneux ID, Morice AH. Airway reflux, cough and respiratory disease. Ther Adv Chronic Dis. 2011 Jul;2(4):237-48. doi: 10.1177/2040622311406464. PMID: 23251752; PMCID: PMC3513884.
- Jung YH, Lee DY, Kim DW, Park SS, Heo EY, Chung HS, Kim DK. Clinical significance of laryngopharyngeal reflux in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015 Jul 15;10:1343-51. doi: 10.2147/COPD.S84337. PMID: 26203240; PMCID: PMC4507795.
- https://www.hopkinsmedicine.org/otolaryngology/specialty_areas/complex_airway/conditions/subglottic_stenosis.html
- Coca-Pelaz A, Rodrigo JP, Takes RP, Silver CE, Paccagnella D, Rinaldo A, Hinni ML, Ferlito A. Relationship between reflux and laryngeal cancer. Head Neck. 2013 Dec;35(12):1814-8. doi: 10.1002/hed.23208. Epub 2013 Jun 22. PMID: 23794281.
- McCormick CA, Samuels TL, Battle MA, Frolkis T, Blumin JH, Bock JM, Wells C, Yan K, Altman KW, Johnston N. H+/K+ATPase Expression in the Larynx of Laryngopharyngeal Reflux and Laryngeal Cancer Patients. Laryngoscope. 2021 Jan;131(1):130-135. doi: 10.1002/lary.28643. Epub 2020 Apr 6. PMID: 32250454.
- Wang JS, Wu MK, Li JR. [Observational study on patients with laryngeal cancer and/or vocal leukoplakia concurrent with laryngopharyngeal reflux]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2018 Aug 7;53(8):587-591. Chinese. doi: 10.3760/cma.j.issn.1673-0860.2018.08.006. PMID: 30121996.
- Lechien JR, Bobin F, Mouawad F, Zelenik K, Calvo-Henriquez C, Chiesa-Estomba CM, Enver N, Nacci A, Barillari MR, Schindler A, Crevier-Buchman L, Hans S, Simeone V, Wlodarczyk E, Harmegnies B, Remacle M, Rodriguez A, Dequanter D, Eisendrath P, Dapri G, Finck C, Karkos P, Pendleton H, Ayad T, Muls V, Saussez S. Development of scores assessing the refluxogenic potential of diet of patients with laryngopharyngeal reflux. Eur Arch Otorhinolaryngol. 2019 Dec;276(12):3389-3404. doi: 10.1007/s00405-019-05631-1. Epub 2019 Sep 12. PMID: 31515662.
- Min C, Park B, Sim S, Choi HG. Dietary modification for laryngopharyngeal reflux: systematic review. J Laryngol Otol. 2019 Feb;133(2):80-86. doi: 10.1017/S0022215118002256. Epub 2019 Jan 16. PMID: 30646967.
- Cheng J, Ouwehand AC. Gastroesophageal Reflux Disease and Probiotics: A Systematic Review. Nutrients. 2020 Jan 2;12(1):132. doi: 10.3390/nu12010132. PMID: 31906573; PMCID: PMC7019778.


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!