Choosing the Right Thyroid Medication – An Evidenced-Based Algorithm and a SIBO Study
What is the best thyroid medication? You may have heard that you require a special medication that combines T4 and T3, but this isn’t true for most. The majority of people appear to respond best to T4 alone, although some may need a higher dose to feel optimal. For those who do not respond fully to this, there are other considerations including T4 plus T3 medications or even liquid T3. This is important because if you jump to a T4 plus T3 medication too quickly you could risk side effects, including cardiovascular symptoms. Let’s discuss this and a SIBO case study illustrating why less treatment is often more effective.
Episode Intro
Dr. Michael Ruscio, DC: Hey, everyone. Welcome to Dr. Ruscio Radio. This is Dr. Ruscio. Today, let’s talk about an evidence-based—or I should say, it’s my using an evidence-based model to create an algorithm for utilization of thyroid hormone prescription—so T4, T4 plus T3, maybe T3 alone, a liquid gel tab of T4. And there are some surprises here. So we’ll come to that more fully in a moment.
[Continue reading below]
Dr. R’s Fast Facts Summary
Evidence based and clinically sound algorithm for thyroid hormone utilization
Several studies looking at T4 versus T4 + T3 versus liquid T4 have been shared in recent newsletter editions. Here are a few points (paraphrased) that might surprise you.
- Some cases of subclinical hypothyroid might actually be true hypothyroid when utilizing more sensitive lab methodologies like dialysis with liquid chromatography with mass spectrometry.
- Starting with T4 plus T3 may carry a fairly high incidence of adverse events (please don’t rush to defend the need for T3 after hearing this, simply realize that a case should be built for T3 and it should not be used indiscriminately).
- Utilizing a higher dose of T4 might achieve the desired clinical improvement without increased risk of adverse events incurred with the addition of T3.
- The T4 dose increase did not cause adverse events. Dr. R’s note: contrast this with the study we reviewed in June 2018 finding the addition of T3 was prone to causing side effects.
- Interestingly, despite the increase in the dose of LT4, no patients experienced symptoms of overdose
- Don’t some patients do better on T4 plus T3? Yes, however this might represent the minority rather than the majority.1 out of the 33 patients appeared to be a candidate for T4 plus T3 .
- 2 other papers have found that up to 50% may prefer T4+T3 BUT this is not what the totality of the data supports
- The T4 dose increase did not cause adverse events. Dr. R’s note: contrast this with the study we reviewed in June 2018 finding the addition of T3 was prone to causing side effects.
- For those with impaired absorption a liquid T4 may be the best option
- https://www.ncbi.nlm.nih.gov/pubmed/27943146
- How often do normal hypothyroid patients need or prefer liquid thyroid hormone?
- 49% will have better TSH and 62% will have better symptomatic control
- For those not optimally responding to an increased dose of T4 the addition of T3 is a consideration and benefit has been documented.
*These points have been codified into a suggested decision-making algorithm to guide thyroid hormone use. This is listed in the August 2018 issue of the Future of Functional Medicine Review Clinical Newsletter.
- Labs presented with borderline positive SIBO and commensal dysbiosis however, the patient did not need to be treated with antimicrobial therapy and a prokinetic.
- Not all lab findings require treatment – Sometimes less is more
- All symptoms improved with the program prescribed
- Modified 2-4 day fast – body aches and digestive symptoms gone
- Probiotics, female hormone support, iodine, adrenal support – improved energy
- Stop Ox bile – caused diarrhea
- Continue vitamin B -12 until improved
- Reading someone’s symptoms and their response is paramount
- Get help with choosing the right thyroid medication.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Download Episode (Right click on link and ‘Save As’)
DrMR: And also, I’d like to go over a case study of a patient who had a chronic case. She came back with a mild, mild case of SIBO. She also had the positive autoimmunity markers for motility impairment that can underlying chronic SIBO. Yet the solution to her case was not using prokinetics, was not treating SIBO. It was actually getting her off a supplement that she was reacting to.
And again, I don’t mean to continue to perhaps highlight cases that are contrary to what some of, I guess you could call it, the SIBO community orthodoxy would be. But these things are important.
And sometimes, when someone needs or doesn’t need “a specialist,” it’s sometimes to determine these simple things, and not necessarily someone who has knowledge of a bacteria no one knows about or a treatment no one knows about.
Really, many—I would say the majority of the cases, at least what I see, and I’m open to the fact that there may be others who see a specialized subset of patients who are more chronic (but I do have some suspicion about that being not always fully accurate and maybe a little bit of a scapegoat) who do need those treatments. There are many cases where the actual missing link is not something that’s highly elusive but rather requires the mastering of the fundamentals.
And it’s been incredibly helpful. And what’s really nice now is seeing doctors new into practice who are actually reading the newsletter and then treating people with what they’ve learned in the newsletter and seeing this great outcome with minimal testing, with minimal treatment. Yet, the patient responses have been fantastic.
And hopefully, we’ll have one of those discussions with two—I believe they’re both medical residents right now who are using some of this in application.
If you want to check out your first month of access to the Future of Functional Medicine Review clinical newsletter for $1, go to DrRuscio.com/Review.
Thyroid T4 with T3
So let’s start into the bits on thyroid. So I linked to the August 2018 edition (subscription required) where I put together this evidence-based and clinically sound algorithm for thyroid hormones. And I’m not going to go through this ad nauseum. But I do want to hit some of the high points. And one of the things that I think may be surprising to people is the evidence, not that I get too deep into thyroid.
I do get deep into thyroid. But what I should say is, I usually start people off with optimizing their digestive health before tinkering too deeply into thyroid. And it’s amazing to me how oftentimes no further tinkering into the thyroid is needed once you optimize one’s gut health, although there are definitely times.
But what’s interesting here is to see that the majority of the data—not to say there are no data that contest this—but the majority of the data show that we should not be bullish with starting everyone off on T4 plus T3. And admittedly, this was a little bit surprising to me, not for any other reason than the standard opinion of many people in integrative, functional, and natural medicine is that you must be given T3 along with the T4.
And when you actually look at the data, the majority of the data actually show that you have a higher predilection toward negative reactions when starting everyone in a T4 plus T3 treatment protocol.
And so let me read a few bullet points here. And then we can fill in some of the justification. Firstly, a little bit tangential. We’ve already covered this in the past. But some cases of subclinical hypothyroidism might actually be true hypothyroid. And you may identify this when utilizing a more sensitive lab methodology. Specifically, this is the dialysis with liquid chromatography with mass spectrometry. It’s always a mouthful for me, that one.
So probably nothing incredibly new there. But we do go through some of the evidence that substantiates that. And we link to how you can order these through LabCorp and Quest. Or if you’re doing a cash pay lab, you would likely need the LabCorp or Quest code to go through your cash pay conglomerate.
Now, here’s the two other points that are a bit more contentious. And I’ll just read a quote out of the newsletter. This is me essentially quoting myself. But,
“Starting with T4 plus T3 may carry fairly high incidences of adverse events. And utilizing higher doses of T4 might achieve the desired clinical improvement without increased risk of adverse events incurred with the addition of T3.”
And I further continue that,
“The T4 dose increase [in this study here],” and I’ll link to it in a moment, “did not cause adverse events.”
And I contrast this with a study we reviewed in the June 2018 issue, finding that the addition of T3 was prone to causing side effects. And I’ll quote the paper here.
“Interestingly, despite the increase in the dose of T4, no patients experienced symptoms of overdose.”
So this is important to understand this. And I’ve seen patients. And it was surprising to me at first. And I thought this was just an outlier. But I’ve seen—I don’t want to say a lot of patients. I’ve seen enough patients now where I know it’s not just an isolated incidence, who have started on T4 plus T3 and not felt well on that combination dosing.
“But don’t some patients do better on T4 plus T3? Yes, however, as we’ve discussed prior,” and this is in prior issues of the newsletter because I’ve been chronicling this, “this might represent the minority rather than the majority. Today’s paper reinforced that one out of 33 patients appeared to be a candidate for T4 plus T3.”
“Now, note. Two other papers have found that up to 50% of patients may prefer T4 with T3. But this is not what the totality of the data supports.”
And that’s the key distinction. Yes, there are people who will do better on T4 plus T3. But it’s not everyone.
And so what does this mean? I can already hear the people who are very pro-combination T4 plus T3 wanting to argue with me on this. It’s not to say that you’re wrong and that you should never do that. But what we should do is we should work this into the construction of our algorithm where we should start people with T4 and see how they do. Then potentially, one of the next things we consider is the addition of T4 plus T3.
So I should continue here that the authors of this same paper that I’m referencing point out that there are several studies showing no additional benefit of T4 plus T3 therapy, leading three meta-analyses to conclude the same.
“A host of follow-up reports of studies that failed to confirm their observations with all studies indicating no benefit of combined T4 plus T3 therapy.”
And they cite 15 through 26, so the references would be 15, 16, 17, 18, 19…so you have essentially 11 studies there with only one exception. And they link to that study.
“These reports were subsequently summarized in three meta-analyses that came to the same conclusion, conclusion being that there was no benefit when using T4 plus T3.”
Again, what does this mean? Don’t go to the conclusion that I’m saying we should never use T3. There is documentation that the addition of T3 to T4 or using something like Armour or Nature Throid or WP Thyroid can be helpful. But that may be anywhere from 50% to 1 in 33. So perhaps a third. And I believe there’s data in one of our newsletters that supports that it might be about a third of patients that really fall into that camp.
Now, why is this important? Well, one of the reasons why this is important is because of negative cardiovascular side effects which are, I believe, the—or if not the, one of the most commonly reported adverse events when we give people T4 plus T3 who don’t really appear to need it.
So again, does this mean that I’m saying that we should never use combination formulas? No, for some people, they’re clearly helpful. But we should not take this and inflate it to say that everyone now needs T4 plus T3; and if your endocrinologist doesn’t start you on T4 plus T3, they are being malicious in some way or withholding a therapy that could be helpful for you.
We can start someone on the T4, see how they do. The next best thing, at least according to the evidence, would then be to increase their T4, potentially to get them down into the lowest half of the TSH reference range. So below 2.5 for the TSH is the typical goal. And we may even want to get someone closer to 0.5. And in this study that I’m referencing here, they found that that actually led to the desired symptomatic improvement sans (without) the negative, mainly but not limited to, cardiovascular adverse events that seem to be reported in the studies that go with a T4 plus T3 combination.
Sponsored Resources
Hey, guys. We’ve discussed at length the benefits of probiotics. But it can be hard to know which specific probiotic products to use. One probiotic that I endorse is Just Thrive Probiotic. Just Thrive is one of the few category 3 (AKA, soil-based) probiotics I recommend. In fact, one exciting study has found that the strains in Just Thrive probiotic can begin healing leaky gut.

And good news! If you’d like to try Just Thrive, they’re offering 25% off your first purchase when you use the code RUSCIO at checkout (R-U-S-C-I-O). They’re available at ThriveProbiotic.com or on Amazon. Check them out.
So essentially, we see in the hierarchy starting to emerge here that we would want to start someone with a T4 formula. And I would argue—and I believe the first time I pointed this out was in an interview with Dr. Kara Fitzgerald on her podcast, New Frontiers in Functional Medicine—that what I typically do is start someone or recommend someone start with a T4 and then take steps to optimize their gut health.
So what happens typically is someone is already on a hormone (let’s say levothyroxine) from their endocrinologist. They come in. And they think that they should be on a combination. And I say, “Well, hold on a minute. Let’s take some steps to improve your gut health, which will, A) improve absorption, and, B) improve conversion, and then reevaluate.”
And for many of these patients, they need to do nothing further. In fact, we’ve documented and released unofficial on our website case studies showing that people were actually able to take less thyroid hormone and feel better.
Liquid T4 – A Better Option for Some
So you start there. Then you consider a higher dose of the T4. Then you would consider T4 plus T3 or potentially a liquid form of T4, especially in those who have chronic digestive impairment. And for some people, the best you can get them to is a position where they still have some active, ongoing digestive symptoms. And so they may be malabsorbing. And so they may do better on just a liquid T4.
So this builds the case for absorption. It also builds the case that a higher dose of tablet T4 may be equivalent to giving someone a switch from a tablet form of T4 to a liquid form of T4 because you could look at this in one of two ways. We want to get more T4 into the system. So we can give someone a liquid gel tab that’s easier to absorb and bypasses the fact that their [absorption] may not be optimal. Or we can give them a higher dose of the tablet T4. And we’re overcompensating for the malabsorption now.
So that’s the hierarchy. So what this looks like—and I list this all out in the write up in the clinical newsletter with the supporting references. But essentially, what you’re looking at is something a little bit different than what some of the field recommends. But it’s not to say that the recommendations of the much of the field of functional, integrative, and alternative medicine is wrong. It’s just, okay. Perhaps we were a little bit too bullish with T3. And now we need to codify that into a little bit more of a reasonable hierarchy.
And this is not very different from what I recommend with SIBO and IBS, which is we don’t always have to start with the strongest therapies that are helpful for a somewhat nonresponsive minority, like going right into herbal antimicrobials or antibiotics along with prokinetics.
We can oftentimes start with some basic dietary changes, getting the right diet into the right person combined with probiotics sometimes. And that is enough to get us where we want to be.
So I’m very excited about that hierarchy because, again, I’ve seen patients who have had these negative side effects from T3. It’s not the majority, at least in my observation, although patients may not be reporting a lot of this to me. So I may be missing some of it.
And I’ve also seen patients who become more fatigued. And I think that’s also something important to mention. If you have too much thyroid hormone in the system—too much—that can actually exacerbate fatigue in some people.
So yes, while some people who are fatigued will do better when they get their levels to where they should be—yes, of course—there is this mistaken thinking that if we push, push, push, push, push the thyroid hormone always to the highest end of the range that it’s always going to be better for people. And for some people, they actually regress.
And what I think happens there is their thyroid is now generally where it should be. And we don’t need to nitpick the numbers to a highly granular degree but rather have a look at a lateral system of the body. The two most common things that I see causing non-responsive, what-are-thought-to-be “hypothyroid symptoms” (as I do air quotes here) is 1) the gut—no surprise there—and then 2) female hormones.
So hopefully, some things there that will help providers and patients navigate the available thyroid hormone prescription landscape a little bit more efficiently.
So again, that decision algorithm is codified into a simple list of bullets in the August issue of the Future of Functional Medicine Review. And then in subsequent issues, we had been picking apart these studies one by one that helped to build us to this case.
Case Study
So then in the March 2018 edition (subscription required) of the Future of Functional Medicine Review, there was a case study that I entitled, “Digestive Enzymes Causing What Looked Like SIBO and then Led to a Complete Resolution after Avoiding Enzymes, Using Iodine and Female Hormone Support.”
Now, admittedly, I was a little bit strapped for time today in my prep. So I didn’t really have a chance to read through this case study to refresh my memory on a lot of the details. So I figured I can either not do it or try to do it perhaps not as smoothly as you may be accustomed to. So I’m going to try doing it the non-smooth method here. And hopefully, this will not be too kludgey. But bear with me if it is.
So Katherine came in as a 35-year-old female previously diagnosed with SIBO, low T3, and low ferritin. She was on Nature Throid. She was on LDN. She was on B12 injections. And she was on bioidentical progesterone. Her chief complaints were diarrhea, gas and bloating, hair loss, fatigue, brain fog, and joint pain.
And I also list these in the newsletter. You’ll see them with the severity out of a 1 to 10 scale and the frequency. And that’s important because sometimes, the way people will list their complaints is inverse of logic. So they will list bloating as their top complaint. Yet the severity is a 2, and it is occasional. And then they will list fatigue as their last complaint. But it is an 8/10, and it is intermittent.
So this is why I now always ask patients to report the severity and the frequency because you need to know what the most problematic symptoms of the symptoms listed are. And sometimes, the way patients report them is a little bit counterintuitive.
So in any case, my initial impression,
“Katherine presents as a generally healthy 35-year-old female with a good diet, lifestyle. But exercise is limited by her health. And she has a good outlook on her health. She has been diagnosed with SIBO, previously treated with rifaximin, followed by herbal antimicrobials and responded well but then later relapsed. A low FODMAP/AIP diet has also been helpful, as have been enzymes. I suspect she merely needs more follow up and follow through in her care. And she will do quite well. And that her GI is the main underlying driver of the sequelae.
There are some other diagnoses or differential diagnoses to mind. Adhesions could be one. Hormonal imbalances could be another.”
And I list my full differential diagnosis list. And this is the problems list that I always keep in the back of my head when working with a patient. And essentially, all you do here is you start with the top of the list, which is usually the most common and most likely factors, and you keep working your way down the list. And I list her prognosis as good to excellent.
So just a quick recap on her previous diets. Low FODMAP helps her gut. Autoimmune paleo helps brain fog, joint pain. Fasting, she does not do well with.
Previous treatments. Nature Throid was slightly helpful. Rifaximin followed with herbal antimicrobials improved her greatly. Then she relapsed like we mentioned a moment ago. Progesterone helps moods and cycles. B12 she thinks helped. Low-dose naltrexone was tolerated, but she didn’t really notice anything. HCl, she didn’t really notice anything. And enzymes with bile she feels helps her GI.
And the rationale there,
“Given her digestive symptoms, ordering a full GI workup for dysbiosis is warranted. Testing for the vinculin and CDTB antibodies can rule out IBD as a cause of her diarrhea.”
And that’s, in my mind, the most appropriate way to use that at this point. 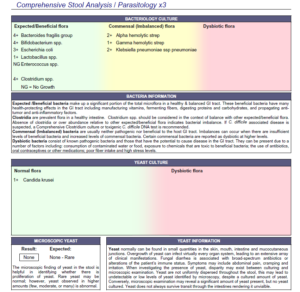
It’s not to be a naysayer. But there are so many things that are speculation that if you wallow in the speculation, and especially when you do this at the expense of mastering the fundamentals, that will definitely decrease the efficacy of one’s practice.
And I have become progressively more confident in that. And I think you’ll see part of why I say that here in a moment. And then,
“The wellness panel will screen for anemias and for hypothyroid, amongst other things.”
And again, we already have talked about the history there. So the recommendations.
“Please perform a modified two- to four-day fast. Then continue with your previous AIP and low FODMAP-like diet.”
And she had gone AIP, gone low FODMAP. And then she had reintroduced to her tolerable boundaries. So that’s a pretty good place to start. I’m not going to really modify much from there.
And we put her on iodine, a multivitamin, and an omega-3/6/9 blend in addition to an herbal adrenal support formula and an herbal progesterone formula. And in addition to that, we also put her on two probiotics—a Lactobacillus bifidobacterium category probiotic, an S. boulardii probiotic—and continued her on an enzyme with HCl. And the rationale here.
“Fasting will evaluate if she might do well with an intermittent fasting approach incorporated into the more longer term.” And also with foods—“Certain foods are still driving her symptoms. Iodine and female hormone herbs may balance hormones causing fibrocystic-like breast symptoms.”
I should shoot back up to her symptoms. I didn’t mention this. I should mention this now. In addition to her chief complaints, I also track other symptoms that people don’t list in their chief complaints. And she had some female hormone symptoms like thinning hair, painful periods. And her GI felt worse during aspects of her cycle. And she also had heavy menstrual flow. She had anxiety, mood swings, and also fibrocystic breast-like symptoms (tenderness, pain). And then,
“Probiotics and enzymes may improve her GI symptoms.”
View Dr. Ruscio’s Additional Resources
Case Study Continued
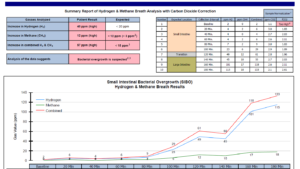
So her third visit about 30 days later, her labs show that she has a peak value of hydrogen of 23. And her methane is 6. So I don’t really consider that a problem with the methane. And the 23 I also don’t really consider to be a problem. That is so close to the borderline that I do not consider that to be problematic. Technically, that is positive for SIBO. But I do not consider that to be a problem.
Her Doctor’s Data profile showed a bit of overgrowth of her commensal (normal) bacteria and a bit of overgrowth of Candida krusei. And she also showed red blood cells one time on her ova and parasite. She had parietal cell autoimmunity via LabCorp. And she also has positivity for the CDTB antibodies through IBS Check through Quest.
So essentially, we see very mild, not even what I really consider clinically positive SIBO. We see the autoimmunity that may underlie the SIBO. And we see some potential bacterial and yeast dysbiosis but nothing that I would really shake a stick at. So the summary here. Essentially,
“We found borderline positive SIBO and commensal dysbiosis. The overgrowth of commensal via stool testing is something I interpret with caution as the meaning of this is unclear. We found antibodies against her parietal cells in the stomach and the autoimmunity that underlies SIBO, the CDTB antibodies.”
With the labs and the write up for you also. So let’s now talk about her subjective assessment, her symptoms, because this helps contextualize how we should be interpreting these lab results.
So the modified fast. She felt very weak and hungry. But her body aches and digestive symptoms were gone. The initial program which involved, remember, probiotics and female hormone support, some iodine, some adrenal support, and some enzymes improved energy.
The ox bile caused diarrhea. So this was contained in the enzyme formula. Or I should say more accurately, the enzyme caused diarrhea. But knowing that bile is probably the most likely culprit in an enzyme formula to cause diarrhea, I listed in my notes, “Bile likely caused diarrhea.”
“Overall, today is better. Improved. She gained some weight.” She was underweight previously. And that really wasn’t much of a complaint. But that became more apparent when she gained some weight.
Her fatigue was better. Her diarrhea was better. Her gas and bloating was better. Her joint pain was better but still slightly present.
Nonresponsive symptoms (symptoms that were the same). Brain fog, hair loss, and some of her female symptoms like the fibrocystic-like breast symptoms. 
“Katherine has been diagnosed with SIBO previously, treated with rifaximin followed by herbal antimicrobials and responded but then relapsed. A low FODMAP diet has also been helpful, as have been enzymes historically. And she may, again, simply require more follow through with her GI plan.
Today’s positive IBS detects may indicate potential post-antimicrobial prokinetic therapies could be important. Labs today also show very mild SIBO, bacterial and fungal dysbiosis and anti-parietal cell antibodies. Her digestion and joint pain responded well to a modified fast, but she was weak and tired.
The initial program might be helping. And today, we will maintain the current plan and continue with the B12 and LDN from her local doctor. Follow up in one to three months. And essentially consider treating the dysbiosis more directly if she is not improving.”
And I list here a key point. How did she notice ox bile caused diarrhea? So she had been taking supplemental bilateral historically. But I ask patients to come off all previous supplements when starting care. This is for a few reasons. One is because sometimes people are taking things that they are reacting to but are unaware that this is the case. And this supplement holiday can be a key aspect of pinpointing the root cause of, in this case, her diarrhea.
So apologize for the kludginess here. But she was taking an enzyme that I had recommended with HCl pancreatic enzymes and bile. And she was also taking ox bile that she had self prescribed. But she went off those things before going back on them as part of my go off everything, start with some dietary changes, and then add your supplements in later. And she noticed right when she added in the supplements that she had a flare of her diarrhea.
So this is why one of the aspects I lay out in the case studies is layering the initiation of starting therapies because now it’s much easier to discern the fact that the bile is likely causing the diarrhea. So my recommendations.
“Continue with your current plan. Start on the vitamin B12 weekly until the stomach antibodies are normal.”
And I asked her just to follow up with the doctor who was administering the B12 injections to keep an eye on that.
“And then once you’ve seen the anti-parietal cell antibodies return to normal, then revert to once monthly dosing. And we asked her to discontinue the bile and the enzymes and follow up in a few months.”
So essentially, when she followed up, she had corroborated that the enzymes and the bile, she was highly intolerant to those. And those were the main culprit for her diarrhea. She felt like continued time on the iodine was really helping her fibrocystic breast. And the progesterone herbs were also helping.
And overall, she had gained weight. She was up to 114 pounds, which she was thrilled about. Her fatigue was better. Her diarrhea was better. Her gas and bloating was better. Her joint pain was better. And her fibrocystic-like breast symptoms were gone, or at least much improved. And her brain fog was gone. The only thing that had not improved was there was still a degree of hair loss.
So essentially, I think closed my impression. But she had done great. And really, the big thing that needed to be addressed there was, I think, 1) some probiotic and 2) some female hormone support and then 3) having her just figure out how to stop the use of a natural treatment (in this case, bile) that was flaring her symptoms.
Now, what about the fact that she had that mild SIBO and the CDTB antibodies? Well, this is why I say we should not look at lab results literally.
And if that is a conversation that is needed to be had, then fine. But before we jump to those very heavy and daunting prognoses, we should be sure that that’s actually the case. And that has not been borne out yet. The utility of the anti-motility antibodies has not really been borne out yet other than being an early screening tool to distinguish between IBS and IBD. And that does seem to have some definite clinical utility.
But does this mean that anyone who has these positive antibodies is going to be a chronic, relapsing case? No! We’ve covered two case studies already who had these antibodies positive and had had a “SIBO relapse” in the past. And with just the right approach, their symptoms were gone. And they maintained in remission.
So this is another case of that where the 23 of her hydrogen peaking which is really not even positive enough to be considered clinically significant, by some could be called SIBO. Technically, you can call it SIBO. But does that mean that the SIBO was causing the diarrhea? No, it was the fact that she was using bile. And she didn’t need to.
So I hope it’s becoming clear why I am not a huge advocate of looking at labs literally, but always cross referencing lab results to the patient context and also realizing that lab results only give you part of the data needed to get someone healthy.
And so if you look at all these case studies, if we had been treating the labs literally, she would have been treated for SIBO again, and she would have been put on a prokinetic, neither one of which she needed.
And if that had been done in the absence of the observation that bile was causing her diarrhea, guess what would have happened? She would not have improved. So she would have gone on another SIBO treatment, maybe even the elemental diet and then maybe even a stronger prokinetic. And she gets sucked into the merry-go-round of treatment that never ends because more treatment was not the solution to the problem.
And I don’t mean to be preaching here. But it’s very disheartening seeing and knowing that this happens. And again, I don’t think it’s any clinician trying not to help a patient. I think every clinician, every practitioner, every provider, every doctor is honestly—the vast majority; there may be a few charlatans out there—trying to help people.
But I think the unfortunate thing is that we need to be doing better with our education and with how we look at these things because if you just jump to the most impactful treatments and the most pessimistic prognosis based upon lab findings or the most pessimistic interpretation of lab findings, then that oftentimes lands you in a position where you’re doing a great disservice to the patient.
Episode Wrap-Up
So I hope that that all makes sense. I close with three bullet points. Not all lab findings require treatment. Sometimes, less is more. And reading someone’s symptoms and their response is paramount. So that’s just another case study, hopefully showcasing that we don’t have to do more to get better patient results.
And again, this case study, along with everything else from today’s podcast is just me summarizing the wealth of information contained in the Future of Functional Medicine Review clinical newsletter. If you haven’t checked it out yet and you feel inclined to do so, I would really encourage you to do that. For just $1, you can obtain your first month of access. And that gives you access, again, to almost two years of back issues, including case studies and research studies and also practice tips and questions of the month.
So hopefully, this is all making sense. If I’m being too critical, I do apologize. And I’m sorry if some of the passion slips out here. But it’s disheartening seeing some people suffering, knowing how much it sucks to suffer when you’re not feeling well, knowing how terrible that is. That anyone has to suffer for one moment more than they need to.
And if that is happening because of a non-fully sharpened clinical approach in functional medicine, I want to do everything I can to help rectify that.
But these things are in no way a criticism of the people in the system. It’s just a passionate outcry on my part to sharpen our skills so that we can get people to well more quickly and not have them flounder through the debilitating and demotivating experience of not feeling well.
So let me know what you think, guys. And hopefully, you learned some valuable information today. And I will talk to you next time. Alright. Thanks!
Thank you for listening to Dr. Ruscio Radio today. Check us out on iTunes and leave a review. Visit DrRuscio.com to ask a question for an upcoming podcast, post comments for today’s show, and sign up to receive weekly updates. That’s D-R-R-U-S-C-I-O.com.
- August 2018 edition of the Future of Function Medicine Review (subscription required)
- June 2018 edition of the Future of Function Medicine Review (subscription required)
- Combination L-T3 and L-T4 therapy for hypothyroidism.
- Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: meta-analysis of randomized controlled trials.
- Thyroxine alone or thyroxine plus triiodothyronine replacement therapy for hypothyroidism.
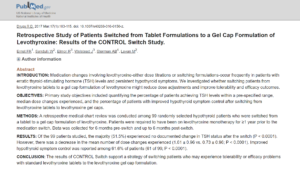
- Retrospective Study of Patients Switched from Tablet Formulations to a Gel Cap Formulation of Levothyroxine: Results of the CONTROL Switch Study.
- Digestive Enzymes Causing What Looked Like SIBO and then Led to a Complete Resolution after Avoiding Enzymes, Using Iodine and Female Hormone Support. (subscription required)
- Just Thrive Probiotic
- Future of Functional Medical Review Clinical Newsletter
- Dr. Ruscio’s Additional Resources
What do you think? I would like to hear your thoughts or experience with this.
- Get help with choosing the right thyroid medication.
- Get your personalized plan for optimizing your gut health with my new book.
- Healthcare providers looking to sharpen their clinical skills, check out the Future of Functional Medicine Review Clinical Newsletter.
Dr. Ruscio is your leading functional and integrative doctor specializing in gut related disorders such as SIBO, leaky gut, Celiac, IBS and in thyroid disorders such as hypothyroid and hyperthyroid. For more information on how to become a patient, please contact our office. Serving the San Francisco bay area and distance patients via phone and Skype.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!