How Does Blastocystis Hominis Affect Your Digestive Health?
Does B. Hominis Cause IBS, Or Is It Just Another Organism?
- Understanding Blastocystis|
- Symptoms of Infections|
- Testing|
- What to Do About Lab Findings|
- Using a Holistic Treatment Approach|
What exactly is Blastocystis hominis, and can it disrupt your digestive health or contribute to IBS? Blastocystis hominis (also known as B. hominis, Blastocystis spp, or Blastocystis sp) , is a single-cell protozoan parasite that can live in the human gastrointestinal tract.
While it may sound alarming to have a parasitic infection, keep in mind this is not necessarily something to worry about. Whether or not this parasite is pathogenic (harmful) in general is still not clear.

Ultimately, the best way to deal with B. hominis is to focus on improving your overall gut health from top to bottom rather than trying to determine whether or not this one organism is responsible for your symptoms or focusing exclusively on its eradication.
In this article, we’ll break down what Blastocystis hominis is, how it relates to digestive conditions, including IBS, how to treat an infection using probiotics and other gut supports, and what it means (and doesn’t mean) if you see this parasite pop up on your stool test.
Understanding Blastocystis Hominis
Blastocystis hominis is a type of protozoan parasite (a microorganism that has adapted to live in human cells or tissues). Other types of protozoan parasites include dientamoeba fragilis, entamoeba histolytica, and giardia.
For a long time, Blastocystis was thought to be simply a harmless yeast. Then, in the 1970’s, it was discovered to be a protist, or beneficial organism living in some people’s intestines. But recently, in the last decade, some studies suggested that it might in fact be linked to some gastrointestinal problems, skin symptoms, and other issues. It’s now in question whether this should be considered a neutral (commensal) organism or a pathogen [1].
The prevalence of blastocystis is higher than you might think. It is a common organism that infects between 50% and 100% of people in developing nations, as well as 5% to 15% of individuals in developed countries where public health is a top priority [1].
As with many infectious diseases, B. Hominis‘ main mode of transmission seems to be from some contact with fecal matter, which is then orally transmitted to the digestive tract. However, the exact etiology may not be as certain. This may mean that the B. Hominis is transmitted through drinking contaminated water or eating tainted food, particularly in developing countries where water standards may be different.
Even in a developed country, you may still come in contact with B. Hominis in any number of locales — perhaps at a restaurant where there has been a slip in hygiene standards, or while taking public transportation where someone else may have touched something and you inadvertently come in contact with it [1].
Symptoms of Blastocystis Hominis Infections
There are a variety of possible signs that you may have a Blastocystis hominis infection (blastocystosis). Some people with Blastocystis in their guts may experience symptoms such as:
- Diarrhea
- Nausea or vomiting
- Cramping or abdominal pain
- Gas
- Constipation
- Fatigue
- Lack of appetite
- Weight loss
- Bloating
- Chronic IBS
Meanwhile, others feel completely fine and have no symptoms from such intestinal parasites [1, 2].
Of course, these symptoms can also point to any number of conditions or imbalances. So, how do you know if B. hominis is the culprit? While a test might tell you that you have blastocystis hominis in your gut, it can’t tell you how that parasite relates to your symptoms.
That’s why the best solution is to address your symptoms and your overall gut health using a balanced, stepwise approach. You are likely to remove potentially harmful organisms like blastocystis hominis in the process as you support an overall healthy digestive system. Let’s explore both testing and treatment in more detail.
Testing for Blastocystis Hominis

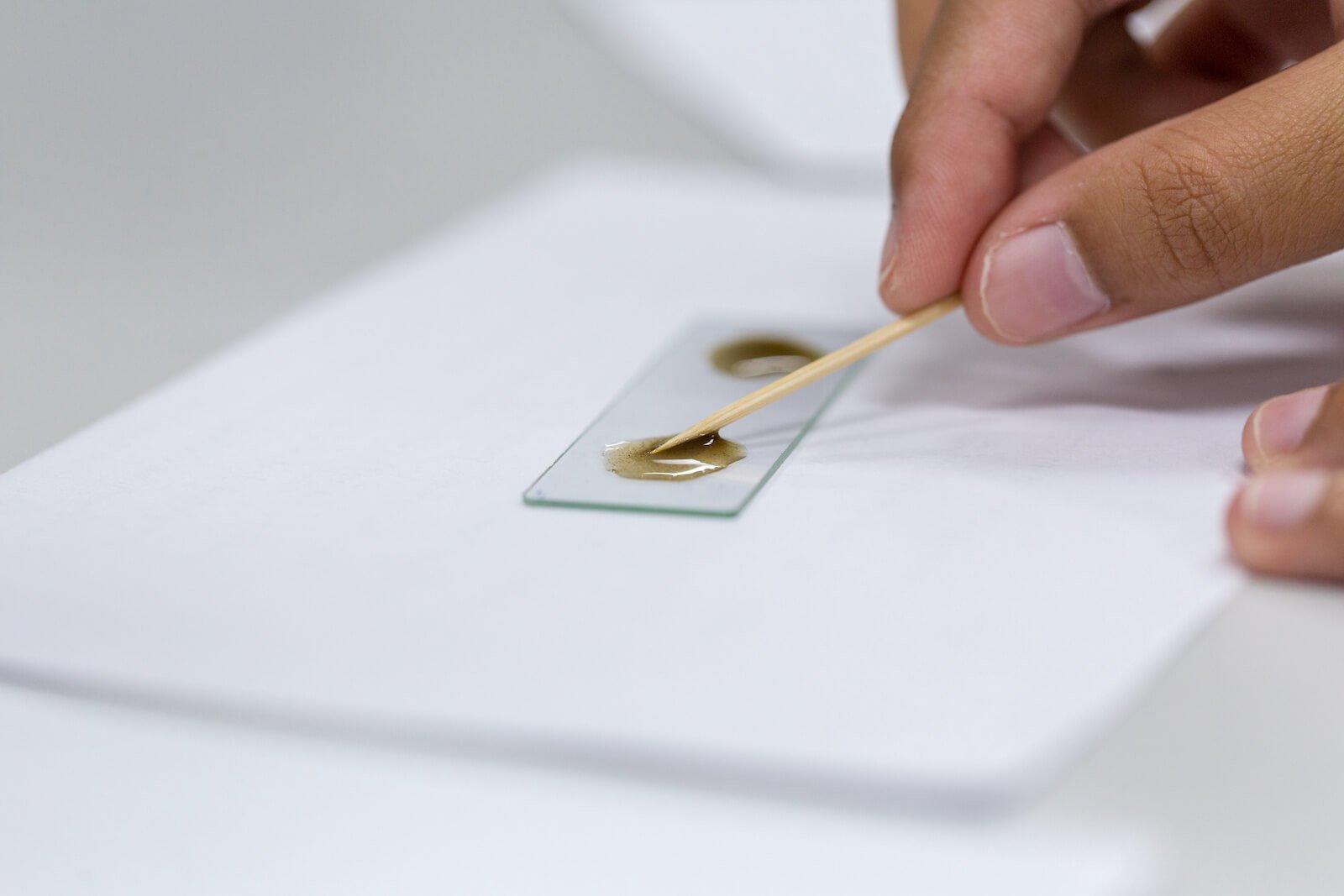
If Blastocystis is on your radar, you have likely undergone some testing for possible parasitic diseases in the gastrointestinal tract. Keep in mind that some tests are more able to detect specific organisms than others. Some tests may also be able to identify even more specific Blastocystis subtypes or genotypes.
Possible ways to find out about the microbiology of the gut in a lab include:
- DNA PCR (Polymerase Chain Reaction) testing which is the gold standard for detecting organisms such as B. hominis in stool samples. This technique amplifies even tiny amounts of DNA from organisms such from the Blastocystis species that’s extracted from the stool. This needs a DNA polymerase enzyme to make new DNA strands and increase the amount that can be studied. It is considered the most accurate testing method due to higher specificity and sensitivity.
- Microscopy in which stool samples are examined under a microscope
- In vitro culture in which fecal matter is placed in special cultures that allow organisms to grow over time.
Functional medicine stool tests like the GI-Map (Microbial Assay Plus) or the GI360 use PCR or a variation on PCR technology. These can detect DNA from both bacterial and parasitic pathogens in stool samples and can offer a comprehensive overview of what’s going on in the gut [3].
What Does It Mean If B. Hominis Shows up on Your Stool Test?
If Blastocystis shows up on your stool test, this means it’s been found in your gut. And that might be all it means.
While it can be helpful to have a more thorough understanding of what is going on in your gut, the pathogenicity of Blastocystis is still unclear. In other words, the research is mixed on whether or not Blastocystis hominis contributes to symptoms or causes harm. And by narrowing in on this one finding, it’s possible to miss the true underlying causes of your symptoms, or the bigger picture of your gut health.
Remember, B. Hominis doesn’t always cause symptoms. And for some, it’s not problematic at all. Several studies and many more case reports show healthy, asymptomatic individuals having B. hominis in their guts [4].
In some cases, parasites like blastocystis hominis are actually considered to be helpful for our systems. For example, Blastocystis spp has been found to be beneficial in some cases by stimulating mucus production in the gut, which can relieve symptoms of colitis and improve gut health [1].
On the other hand, other research suggests that Blastocystis often causes symptoms that need treatment. For example, a 2018 observational study of children with B. Hominis and functional abdominal pain indicates that treating Blastocystis is associated with an improvement in symptoms compared to placebo. The study found that 69% of the children who were treated for this parasite improved, while this was true for only 35% of those who didn’t get Blastocystis treatment [5].
B. Hominis and Your Gut Microbiome
One factor that may make the difference in whether Blastocystis has pathogenic results may be the other bacteria in your gut microbiota. Blastocystis is often detected in those with a large amount of bacterial diversity in their guts [1].
What remains unclear, however, is whether changes in the gut microbiome are caused by Blastocystis. Or, are the changes found in your gut the reason that there is more colonization of Blastocystis [1]?
Instead of thinking of this as an infection that needs eradication with the aid of medication, it may be best to think of Blastocystis in the gut as a lab finding associated with general gut imbalances.
Does Blastocystis Hominis Contribute to IBS?

There is a modest connection between irritable bowel syndrome (IBS) and B. hominis. Here’s a closer look at what the research says:
IBS and Blastocystis Hominis Research
| Evidence for Yes | Evidence for No | Bottom Line | |
| Is B. Hominis connected to IBS? | A systematic-review and meta-analysis showed that there was a significant chance of having both Blastocystis and IBS [6]. | One study showed that B. Hominis was actually more common among healthy people (27%) than among those with IBS (18%) [7]. | Maybe. B. hominis is common among those with IBS. But, it’s also common among those who are healthy. The overall health of your gut may affect whether or not B. hominis is problematic. |
| Does B. Hominis Treatment Improve Digestive Symptoms? | Several studies have shown that treating B. hominis, including with antibiotics such as metronidazole (Flagyl) and the probiotic Saccharomyces boulardii, leads to modest improvements in symptoms such as diarrhea and abdominal pain [5, 8, 9]. | A randomized clinical trial involving children with abdominal pain found that antibiotic treatment for B. hominis did not improve symptoms more than a placebo [10]. | Yes, often. Most studies have found that B. hominis treatment leads to improvements in digestive symptoms. However, these improvements are generally modest. |
| Does B. Hominis need to be eradicated for symptom improvement? | One study showed that in patients who only had Blastocystis as a potential cause of diarrhea, there was an association between symptom improvement and the eradication of the B. Hominis [11]. | Some studies have shown symptomatic improvements with B. hominis treatment, even if the parasite was not actually eradicated. For example, one study involving children with digestive issues found that symptoms improved in 40% of cases, while B. hominis was only eradicated in 27% of the group [12]. | No. Actual eradication of the B. Hominis does not usually appear to be necessary to reap the benefits. Improving the balance within your gut microbiome, rather than specifically getting rid of Blastocystis hominis, appears to work best for most people. |
What to Do About B. Hominis Lab Findings
So, if you’ve been told that you have B. Hominis in your system, perhaps detected by PCR testing, it’s important not to worry. The best thing to do is to use a holistic treatment approach in order to address your overall gut health (which should address the parasite, but not in isolation).
Keep in mind that we are all far more than the sum of our lab results, and the role of Blastocystis in causing ailments in the gut remains unclear. The fact is that testing can offer just a sliver of information when it comes to your individual health. While a tool such as the GI-MAP is extremely sensitive and can offer us some data on whether B. Hominis is present, it cannot tell us if this is the cause of your symptoms.
The last thing you want to do is to focus on these findings alone and blindly work to eradicate B. Hominis. With this approach, not only could you end up chasing your own tail, but also you may find that you miss your real gut or health problems.
Also, if we jump too quickly to eradicate one specific lab finding like B. Hominis, we may overuse some antibiotics and antimicrobials, which may become less effective in treating some infections.
Remember, your symptoms need to be assessed together with other aspects of your personal history. Information from a test such as the GI-MAP is just one piece of the puzzle. And if you don’t have any symptoms or your symptoms have improved, that’s even less of a reason to worry about a stray finding of B. Hominis.
Probiotics Alone Can Treat B. Hominis
Research has shown that the probiotic S. boulardii alone can be an effective treatment against Blastocystis in children.
In one study, 48 children with B. Hominis were randomly selected to receive treatment within one of three groups – treatment with the probiotic S. boulardii, treatment with Flagyl (metronidazole) or no treatment at first.
Investigators found that after 10 days of treatment, symptoms had resolved in 77% of those in the S. boulardii probiotics group, 67% of those in the Flagyl group, and 40% of those who received no treatment at first.
| Treatment Group | No treatment | Antibiotic (Flagyl) | Probiotic (S. boulardii) |
| B. Hominis Symptom Resolution Rate [12] | 40% (least effective) | 67% | 77% (MOST effective) |
The S. boulardii probiotic was actually somewhat more effective than the Flagyl. However, the difference was not clinically significant [12].
Also, when probiotics are given together with antibiotics, this can possibly increase the success. Research done in combating SIBO (small intestinal bacterial overgrowth) shows that when metronidazole treatment was given with S. boulardii, it boosted the gastrointestinal outcomes.
The treatment succeeded here in 55% of cases when the antibiotic was given with the probiotic. However, when the probiotic was used alone, this only worked in 33% of cases. Meanwhile, the medicine only worked for 25% of patients in this study [13].
Using a Holistic Treatment Approach

When dealing with gut-related issues that may be linked to less virulent parasites such as B. Hominis, a holistic, stepwise approach is best. Antiparasitic and other antimicrobial treatments, if used at the wrong time, often come with the risk of side effects.
Using a holistic approach may be less harmful and ultimately support the microbiota so it can effectively do its job and combat this parasitic infection.
Here’s the approach I use with my patients:
- First, we lay a solid foundation. This involves maximizing the functioning of your gut and immune system with the aid of a personalized anti-inflammatory diet to meet your needs, an exercise plan individualized for you, and taking steps to ensure you are getting proper rest.
- If needed, add probiotics to your regimen. These alone may be enough. In particular, adding probiotics such as Saccharomyces boulardii (S. boulardii) to your regimen can often effectively eradicate B. hominis, as well as other protozoa.
- If symptoms persist, then add conventional medication or herbal antimicrobials. This is the time to try conventional antimicrobials or antibiotics. Conventional treatments include medications such as metronidazole, trimethoprim/sulfamethoxazole, nitazoxanide, iodoquinol, paromomycin, ketoconazole and tinidazole. When paired with probiotics, these can be even more effective [2].
I have found this approach to be effective almost all of the time.
If you don’t lay the appropriate foundation with diet, lifestyle, and foundational gut supports like probiotics, the result is generally that antimicrobials, including antibiotics, will be less effective.
Keeping Blastocystis Findings in Perspective
So, if you find yourself diagnosed as having B. Hominis in your gastrointestinal tract or you have irritable bowel syndrome, don’t worry just because it falls under the umbrella of parasites. We are gaining new insights about this Protozoan parasitic infection all the time.
What we understand about this is that many will ultimately do just fine even without treatment. If you do develop gastrointestinal symptoms, as long as you prime your system to succeed and work with your doctor your health should not be impacted in the long run.
You can use this approach on your own, or if you prefer we can help you to navigate through these steps. You can reach out for a consultation here.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Lepczyńska M, Białkowska J, Dzika E, Piskorz-Ogórek K, Korycińska J. Blastocystis: how do specific diets and human gut microbiota affect its development and pathogenicity? Eur J Clin Microbiol Infect Dis. 2017 Sep;36(9):1531–40. DOI: 10.1007/s10096-017-2965-0. PMID: 28326446. PMCID: PMC5554277.
- Sekar U, Shanthi M. Blastocystis: Consensus of treatment and controversies. Trop Parasitol. 2013 Jan;3(1):35–9. DOI: 10.4103/2229-5070.113901. PMID: 23961439. PMCID: PMC3745668.
- Gingras BA, Maggiore JA. Performance of a new molecular assay for the detection of gastrointestinal pathogens. Access Microbiol. 2020 Aug 19;2(10):acmi000160. DOI: 10.1099/acmi.0.000160. PMID: 33195974. PMCID: PMC7660239.
- Leder K, Hellard ME, Sinclair MI, Fairley CK, Wolfe R. No correlation between clinical symptoms and Blastocystis hominis in immunocompetent individuals. J Gastroenterol Hepatol. 2005 Sep;20(9):1390–4. DOI: 10.1111/j.1440-1746.2005.03868.x. PMID: 16105126.
- Toro Monjaraz EM, Vichido Luna MA, Montijo Barrios E, Cervantes Bustamante R, Zárate Mondragón F, Huante Anaya A, et al. Blastocystis Hominis and Chronic Abdominal Pain in Children: Is there an Association between Them? J Trop Pediatr. 2018 Aug 1;64(4):279–83. DOI: 10.1093/tropej/fmx060. PMID: 28985427.
- Rostami A, Riahi SM, Haghighi A, Saber V, Armon B, Seyyedtabaei SJ. The role of Blastocystis sp. and Dientamoeba fragilis in irritable bowel syndrome: a systematic review and meta-analysis. Parasitol Res. 2017 Sep;116(9):2361–71. DOI: 10.1007/s00436-017-5535-6. PMID: 28668983.
- Krogsgaard LR, Andersen LO ’Brien, Johannesen TB, Engsbro AL, Stensvold CR, Nielsen HV, et al. Characteristics of the bacterial microbiome in association with common intestinal parasites in irritable bowel syndrome. Clin Transl Gastroenterol. 2018 Jun 19;9(6):161. DOI: 10.1038/s41424-018-0027-2. PMID: 29915224. PMCID: PMC6006308.
- Rossignol J-F, Kabil SM, Said M, Samir H, Younis AM. Effect of nitazoxanide in persistent diarrhea and enteritis associated with Blastocystis hominis. Clin Gastroenterol Hepatol. 2005 Oct;3(10):987–91. DOI: 10.1016/s1542-3565(05)00427-1. PMID: 16234044.
- Batista L, Pérez Jove J, Rosinach M, Gonzalo V, Sainz E, Loras C, et al. Low efficacy of metronidazole in the eradication of Blastocystis hominis in symptomatic patients: Case series and systematic literature review. Gastroenterología y Hepatología (English Edition). 2017 Jun;40(6):381–7. DOI: 10.1016/j.gastre.2016.11.012. PMID: 28279442.
- Heyland K, Friedt M, Buehr P, Braegger CP. No advantage for antibiotic treatment over placebo in Blastocystis hominis-positive children with recurrent abdominal pain. J Pediatr Gastroenterol Nutr. 2012 May;54(5):677–9. DOI: 10.1097/MPG.0b013e31823a29a7. PMID: 22002479.
- Nigro L, Larocca L, Massarelli L, Patamia I, Minniti S, Palermo F, et al. A placebo-controlled treatment trial of Blastocystis hominis infection with metronidazole. J Travel Med. 2003 Apr;10(2):128–30. DOI: 10.2310/7060.2003.31714. PMID: 12650658.
- Dinleyici EC, Eren M, Dogan N, Reyhanioglu S, Yargic ZA, Vandenplas Y. Clinical efficacy of Saccharomyces boulardii or metronidazole in symptomatic children with Blastocystis hominis infection. Parasitol Res. 2011 Mar;108(3):541–5. DOI: 10.1007/s00436-010-2095-4. PMID: 20922415.
- García-Collinot G, Madrigal-Santillán EO, Martínez-Bencomo MA, Carranza-Muleiro RA, Jara LJ, Vera-Lastra O, et al. Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020 Apr;65(4):1134–43. DOI: 10.1007/s10620-019-05830-0. PMID: 31549334.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!