Home Remedies for Gastritis Attacks: A Step-By-Step Guide
Natural Therapies To Heal Your Digestive Symptoms
- Home Remedy for Gastritis Attack|
- Diet & Lifestyle|
- Probiotics|
- Nutritional Supplements|
- Elemental Diet|
- Herbal Remedies|
- What is Gastritis?|
- Trying a Paleo, low FODMAP, or autoimmune Paleo diet, adjusting meal time behaviors, and taking probiotics can help prevent and heal gastritis attacks.
- By following an elimination diet and reintroduction process, you can determine the ideal diet to manage gastritis.
- In some cases, elemental and semi-elemental diets may relieve inflammation and reduce the symptoms associated with gastritis attacks.
- Nutritional supplements like vitamin B12, iron, and vitamin D may be important for those with gastritis-related malabsorption.
- Several traditional Chinese medicine preparations have been found to improve gastritis symptoms.
If gastritis (chronic inflammation of the stomach lining) is causing your stomach pain, bloating, and fatigue, home remedies that include an anti-inflammatory diet, probiotics, and changing your meal time behaviors can help improve your symptoms.
Spicy foods, coarse cereals (like oats, buckwheat, and millet), milk, and legumes may worsen and/or trigger gastritis symptoms [1, 2, 3]. However, that doesn’t mean you need to avoid these foods indefinitely, as a healthy gut can tolerate a wide variety of foods without triggering symptoms.
Following a step-by-step food elimination and reintroduction process with a Paleo, low FODMAP, or autoimmune Paleo diet, can lower inflammation and give your digestive system the chance to heal. If, after adjusting your diet, you need more support, a gut reset with an elemental diet is effective for calming the digestive tract.
In addition to finding your ideal diet, taking probiotics and adjusting your dietary habits like slowing down at meal time and eating smaller meals at routine times may also be helpful. If you’re hoping to prevent or treat chronic gastritis complications like anemia, nutritional supplements like iron and vitamin B12 can be important.
In this article, we’ll provide the home remedy for gastritis attacks, discuss how to heal the underlying causes of gastritis, and share how improving digestive health can prevent further gastritis complications.
Home Remedy for Gastritis Attack
While treatment needs to be personalized, a home remedy for gastritis attack protocol often includes:
- An anti-inflammatory diet (Paleo, low FODMAP, or autoimmune Paleo)
- Eating smaller meals and eating more slowly
- Avoiding alcohol
- Probiotics
Additional tools may include elemental dieting, nutritional supplements, and traditional Chinese herbal medicines.
We’ve created the below step-by-step home remedy for gastritis attack guide to get you on the road to healing. Work through each step and take note of your symptoms, you’ll likely start to feel better quickly as you move through the process.
Step One: Anti-Inflammatory Diet and Lifestyle Measures
While there’s no one specific diet for gastritis, following a step-by-step elimination diet process can help you pinpoint food sensitivities that could be causing inflammation and making it difficult for your gut to heal. This elimination process allows you to ultimately determine which dietary plan works best for you.
I typically recommend starting with the Paleo diet, which removes common food allergens and inflammatory foods like:
- Grains
- Beans
- Legumes
- Lentils
- Processed foods
- Dairy products
- Artificial sweeteners
- Alcohol
By minimizing your exposure to foods that could provoke an immune response, you quiet inflammation, balance your gut bacteria and improve your gut microbiome, which further reduces inflammation [4, 5, 6, 7, 8, 9].
On the Paleo diet, you’ll eat the following foods for two to three weeks:
- Fresh vegetables
- Fresh fruits (in moderation)
- Grass-fed, lean meats
- Fresh fish and eggs
- Healthy fats, like olive oil, coconut oil, avocado oil and avocados
- Nuts and seeds
If you feel great after a few weeks on the Paleo diet, then you can use this diet as a framework to start to reintroduce the healthy foods that you’ve eliminated. You’ll want to reintroduce one food at a time for a few days and monitor for any negative effects. If you tolerate an eliminated food, then you can add it back to your maintenance meal plan. If your gastritis symptoms recur, then keep that food out of your diet for a little longer.
Keep in mind that some foods, like spicy foods, sugar, and alcohol, are potent gastritis triggers, and may need to be left out of your diet for a few months while your gut continues to heal.
Alternatively, if you’ve been on the Paleo diet for a few weeks with very little improvement, you may want to consider the low FODMAP diet.
A low FODMAP diet is more restrictive and targets possible underlying imbalances that could be causing inflammation. This type of diet starves overgrown or pathogenic bacteria and has been shown to improve a variety of gastrointestinal symptoms like abdominal pain, bloating, gas, and leaky gut [10, 11, 12, 13, 14, 15]. Here’s the low FODMAP diet at a glance:

If you’re feeling better after a few weeks on the low FODMAP diet, you can begin to reintroduce foods the same way as with the Paleo diet. You’ll monitor for a re-emergence of your symptoms and avoid any foods that cause discomfort.
If you’ve gone through the Paleo and low FODMAP plans but feel there’s room for improvement, you may want to check out the autoimmune Paleo diet, which is the most restrictive diet option of the three.
If your gastritis is caused by autoimmunity, also known as autoimmune gastritis (AIG) this diet may be worth a try if the others have failed. The autoimmune Paleo diet further eliminates foods that may cause inflammation in some people like eggs and nightshade vegetables. It can be helpful for people with certain autoimmune and/or inflammatory conditions [16, 17, 18].
Here’s a chart of foods to include and foods to avoid on this type of diet:
| Foods to Include | Foods to Avoid |
| Grass-fed or wild-caught animal lean proteins (meat, fish, poultry, organ meats, bone broth) | All grains, eggs, and legumes such as green beans, black beans, white beans, kidney beans, and garbanzo beans |
| Healthy fats and oils (coconut oil and coconut milk, olive oil, avocados and avocado oil) | All nuts and seeds, such as almonds, walnuts, and chia seeds, including their derivatives like seed and vegetable oils and flours (like almond flour) |
| Wide variety of fresh fruits and vegetables (sweet potatoes, greens, lettuce, cucumbers, zucchini, berries, apples, and melon) | Nightshade vegetables (tomatoes, potatoes, peppers, eggplant, tomatillos) and spices derived from nightshades (paprika and cayenne pepper) |
| Non-dairy fermented foods (sauerkraut, kombucha, kimchi) | All dairy products, including ghee, kefir, milk, cheese, and cream |
| Herbs and spices not derived from seeds (cinnamon, turmeric, thyme, oregano, basil, rosemary) | Spices derived from seeds, including fennel, cumin, dill, anise, mustard, coriander, and nutmeg |
| Stevia and maple syrup | Most added or artificial sweeteners and food additives, plus coffee and alcohol |
The autoimmune Paleo diet is very restrictive and is why we don’t recommend it as a first option for gastritis attacks.
In addition to diet therapy, you can also try changing up your eating habits to calm gastritis. In one 2020 observational study of patients with chronic gastritis, those who ate too fast, had irregular meal times, and ate leftovers tended to have more stomach aches and bloating [1]. Implementing the following strategies may be helpful:
- Eat smaller meals
- Eat more slowly
- Eat at routine times
- Chew your food thoroughly
- Avoid leftovers
- Limit alcohol consumption
If after implementing the elimination diet and reintroduction process you still don’t feel like you’re 100%, then move to step two and consider adding probiotics.
Step Two: Probiotics for Gastritis
While the research on using probiotics to treat gastritis is sparse, probiotics are an effective treatment for Helicobacter pylori (H. pylori) infection which is a common cause of chronic atrophic gastritis [19]. In some cases, probiotics may completely eradicate H. pylori bacteria by preventing it from attaching to the stomach lining [20].
Several systematic reviews and meta-analyses have found probiotics (multi-strain seem to be the most effective), in conjunction with traditional antibiotic treatment, led to higher H. pylori eradication rates and lower incidence of treatment side effects [21, 22, 23]. However, one review found probiotics in addition to standard therapy didn’t improve eradication rates above placebo [24]. While the research on using probiotics to eliminate an H. pylori infection is mixed, the majority of the evidence points toward them being helpful, especially when used alongside the standard therapy.
It’s important to also note that long-term use of probiotics has additional health benefits and can reduce the risk of developing disorders associated with the gastric inflammation caused by H. pylori infection like peptic ulcers, gastritis, and gastric (stomach) cancer [25].
Probiotics have been well-studied, are overwhelmingly safe, and are well-tolerated by most people, so they’re worth a try to see if they can improve your gastritis symptoms. Our triple therapy probiotic sticks are a multi-species probiotic option in a therapeutic dose to help support gut and immune health.
Step Three: Nutritional Supplements
If you’ve been diagnosed with gastritis and you’re working through the step-by-step natural remedy guide, you may need to consider adding some nutritional supplements.
Chronic inflammation of the stomach lining destroys the parietal cells, which secrete hydrochloric acid. This means your stomach can’t release the stomach acid needed to break down the food you eat [26]. When acid production is altered, the end result is continued inflammation and malabsorption, which can lead to [27, 28, 29]:
- Iron deficiency
- Folate deficiency
- Calcium and magnesium deficiency
- Stomach cancer
- Vitamin B12 deficiency
- Pernicious anemia (an autoimmune condition that destroys intrinsic factors in the stomach and decreases vitamin B12 absorption in the intestines).
Depending on your micronutrient levels, which can be determined by a blood test, you may benefit from iron, vitamin B12, and/or vitamin D supplements. Interestingly, probiotics have been shown in clinical trials to improve the absorption of all of these nutrients [30, 31, 32, 33].
This is one of the reasons we often recommend initiating probiotic therapy before other nutritional supplements. It prepares the gut for maximum absorption, as does an anti-inflammatory diet. Remember, it’s important to speak with your provider before adding any nutritional supplements.
Vitamin B12 and Iron
Supplementation with vitamin B12 and iron may prevent or reverse many symptoms including anemia, fatigue, hair loss, and neurological issues [29]. Be sure to ask your doctor to check your levels if you have chronic gastritis.
Oral iron supplements and intravenous (IV) iron are similarly effective for raising iron levels [29]. However, unless you have severe iron deficiency anemia, it’s best to start with the oral form, as it has a lower risk of side effects than IV iron. It’s important to note that oral iron can be hard on the gut even if you aren’t in an active gastritis flare, so try starting with a form that’s easier on the stomach (ferrous gluconate and ferrous bisglycinate). If you experience GI upset and/or your iron levels aren’t increasing then you may need to consider IV iron.
Vitamin B12 injections are best for a recently diagnosed B12 deficiency, especially when neurological symptoms are present but can be replaced with oral B12 for long-term maintenance [29]. In addition, two studies found that vitamin B12 injections can reduce stomach autoimmunity/ pernicious anemia [34, 35].
Research shows that oral vitamin B12 is effective at maintaining healthy levels and treating pernicious anemia in those with gastritis when taken at a high dose of 500-1,000 mcg per day [36].
Vitamin D
Vitamin D is an important modulator of the immune system and vitamin D deficiency can further contribute to autoimmune gastritis and its complications [37]. It’s important to have your vitamin D level checked and to speak with your healthcare provider about appropriate supplementation and/or sun exposure.
As I discuss in Healthy Gut, Healthy You, sun exposure has been shown to protect against digestive tract disease and inflammation. There are simple tracking apps that allow you to track and estimate your vitamin D dosing from the sun, like D Minder.
Elemental Heal for Gastritis


A short gut reset with an elemental diet may be helpful as a home remedy for gastritis attacks that are the result of immune dysfunction and/or food intolerances or reactivity. You’ll likely notice a benefit within two days of starting this meal-replacement diet.
However, if your gastritis is related to an H. pylori infection, an elemental diet alone may not cut it and you should seek out a healthcare provider for assistance.
The elemental diet is a liquid meal replacement that’s very easily absorbed in the digestive tract and supplies all macronutrients and essential vitamins. The formula (hypoallergenic, anti-bacterial, and anti-inflammatory) is sold as a powder that you simply mix, blend, or shake up with water and sip on throughout the day.
Semi-elemental diets differ in that instead of the proteins being fully broken down into amino acids, they’re partly broken down. Semi-elemental diets seem to work just as well as full elemental versions and may have a better taste profile than standard elemental diets. However, we created a great-tasting elemental diet formula that is available for purchase through our online store.
Elemental and semi-elemental diets can be beneficial for autoimmune disorders like inflammatory bowel disease and rheumatoid arthritis and are likely a great option for autoimmune gastritis [38, 39]. They’re also helpful for healing a variety of other digestive complaints.
The elemental diet shouldn’t be considered an initial therapy, but if you haven’t responded to diet, lifestyle changes, and probiotic therapy, it may provide more gut-healing benefits and symptom relief.
Herbal Remedies for Gastritis
Several traditional Chinese medicine formulations have been found to improve gastritis symptoms. The following chart outlines the research:
| Chinese Herbal Medicine | Gastritis Benefit |
| Banxia Ziexin decoction [40] | • More effective and safer at treating atrophic gastritis than a mix of Chinese and western medicine • Improved abdominal pain and belching • Better at inhibiting H. pylori, reducing inflammation related to H. pylori, reducing glandular atrophy, intestinal metaplasia, and gastric precancer |
| Xiangsha Yangwei [41] | Combined with western medicine was better and safer than western medicine alone at alleviating clinical symptoms of chronic gastritis |
| Jianpi Yiqi therapy [42] | Alone or in combination with western medicine was better and safer at treating stomach ache, distention, belching, and fatigue in patients with chronic atrophic gastritis |
| Chinese herbal decoction (unspecified) [43] | Alone or in combination with western medicine was better than western medicine alone at improving clinical outcomes and tissue damage in those with chronic atrophic gastritis |
| Chihu-Shugan-San [44] | More effective than chemotherapy for treating chronic gastritis with no serious side effects |
Chinese herbal medicine seems to be an effective option with minimal side effects. However, it shouldn’t be considered a first-line therapy for gastritis. You probably won’t get the most benefit out of your supplements when your gut is inflamed and unable to fully absorb nutrients.
It’s important to heal your gut with diet, meal time strategies, and probiotics first. These are low-cost and effective tools that calm inflammation and allow for better nutrient absorption. If you work through the step-by-step guide and still need some additional support, herbal therapies may then be an additional possibility.
We’ve provided a home remedy for gastritis attacks, now let’s focus on what gastritis is and why it’s important to identify and treat it early.
What is Gastritis?
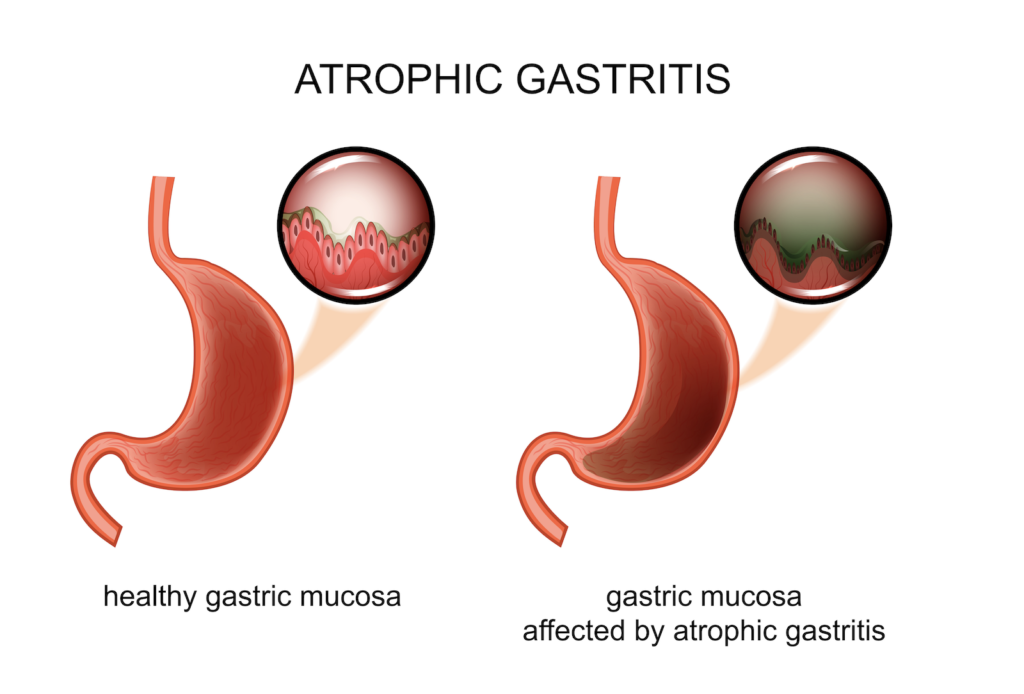
Gastritis refers to a group of conditions that cause inflammation of the stomach lining. Acute gastritis comes on suddenly and can be caused by certain medications like non-steroidal anti-inflammatory drugs (NSAIDs).
If this irritation lasts for a long time, chronic atrophic gastritis develops, which is severe irritation and an eventual breakdown of the stomach lining. Atrophic gastritis is thought to affect 23.9 to 31.6% of the population and those aged 35 to 44 seem to be at the highest risk [45].
Here’s a quick overview of gastritis symptoms, causes, and treatments:
| Common Symptoms [28, 29, 46] | Causes [19, 27, 29] | Treatments [19, 21, 22, 25, 27, 41, 42, 43, 44, 47] |
| • Upper abdominal pain • Feeling full quickly when eating • Fatigue • Pale complexion • Nausea • Vomiting • Marked fullness after eating • Indigestion • Anemia • Brain fog | • Helicobacter pylori infection • Autoimmunity • Inflammation from a variety of factors like food sensitivities, medications, other environmental factors | • Identify and remove food sensitivities • Eradicate H. pylori • Reduce inflammation (anti-inflammatory diet and probiotics) • Supplement to replete micronutrients • Herbal medicine |
Gastritis can be diagnosed by [27, 29, 45]:
- Endoscopy with a stomach biopsy (tissue sample)
- Antibody testing (anti-parietal cell, anti-intrinsic factor, and anti-H. Pylori antibodies)
- Pepsinogen I:pepsinogen II ratio (pepsinogen is a substance secreted by the stomach wall)
- Lab tests for hemoglobin, mean cell volume, and gastrin-17

What Causes Gastritis?
Atrophic gastritis is commonly caused by H. pylori bacterial infection and/or an autoimmune process (called autoimmune gastritis), both of which cause chronic inflammation [19].
If you have slight irritation, you may not have any symptoms at all but as the inflammation worsens you may begin to notice gastritis symptoms like [19, 29]:
- Upper abdominal pain
- Nausea
- Vomiting
- Feeling too full
- Indigestion
- Fatigue
- Heartburn/ acid reflux
- Loss of appetite
- Weight loss
It’s important to identify and treat gastritis quickly to prevent long-term complications. If you have the symptoms of gastritis and/or any of the following conditions, which are associated with gastritis, you may want to speak with your healthcare provider [45, 48]:
- Unexplained iron deficiency anemia
- Macrocytosis or macrocytic anemia (red blood cells that are larger than normal)
- Persistent indigestion
- Autoimmune thyroid disease
- Type 1 diabetes
- Family history of gastric cancer or precancer
- Continuous use of acid blockers/proton pump inhibitors (PPI)
- Hashimoto’s thyroiditis
- Celiac disease
- Rheumatoid arthritis
- Grave’s disease
- Connective tissue disease
- Psoriasis
Whether you’ve just been diagnosed or you’ve been trying to manage gastritis symptoms for a long time, there are several effective natural treatments. Healing your gut with our step-by-step guide can help give you long-term relief.
Natural Remedies Are Effective for Gastritis
It’s important to treat the inflammation that underlies gastritis in order to fully resolve your symptoms. Our natural remedy guide will likely improve your symptoms despite the cause, and help prevent gastritis complications.
If you’re struggling with gastritis symptoms, start by implementing an anti-inflammatory diet and diet-related strategies like smaller, more routine meals. If you need some additional support, add in probiotics and reevaluate your symptoms. Depending on your level of micronutrient insufficiency, you may benefit from vitamin B12, iron, and/or vitamin D supplementation.
If you’ve worked through the step-by-step guide but still feel unwell, you may need more specialized support. Contact us at the Ruscio Institute for Functional Medicine for a personalized healing plan.
The Ruscio Institute has developed a range of high-quality formulations to help our patients and audience. If you’re interested in learning more about these products, please click here. Note that there are many other options available, and we encourage you to research which products may be right for you.
Dr. Michael Ruscio is a DC, natural health provider, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!