The Truth About the Symptoms of Hashimoto’s Flare-Ups
How to Live Well with Hashimoto’s
- Thyroid Antibodies|
- Symptoms of Hashimoto's Flare-Up|
- Immune System|
- Low Thyroid Function|
- Thyroid Medication|
- Thyroid-Gut Connection|
- Preventing Flare-Ups|
If you suspect you’re experiencing symptoms of Hashimoto’s flare ups, there are two very different possible causes:
- Immune system activation and inflammation (often linked to a gut health or female hormone imbalance)
- Low thyroid function (hypothyroid)
Standard healthcare for Hashimoto’s disease tends to focus on treating hypothyroidism. But this is only part of the equation, and it leaves many patients struggling with unresolved symptoms. In fact, contrary to what many believe, the majority of Hashimoto’s patients don’t actually develop hypothyroidism at all [1].
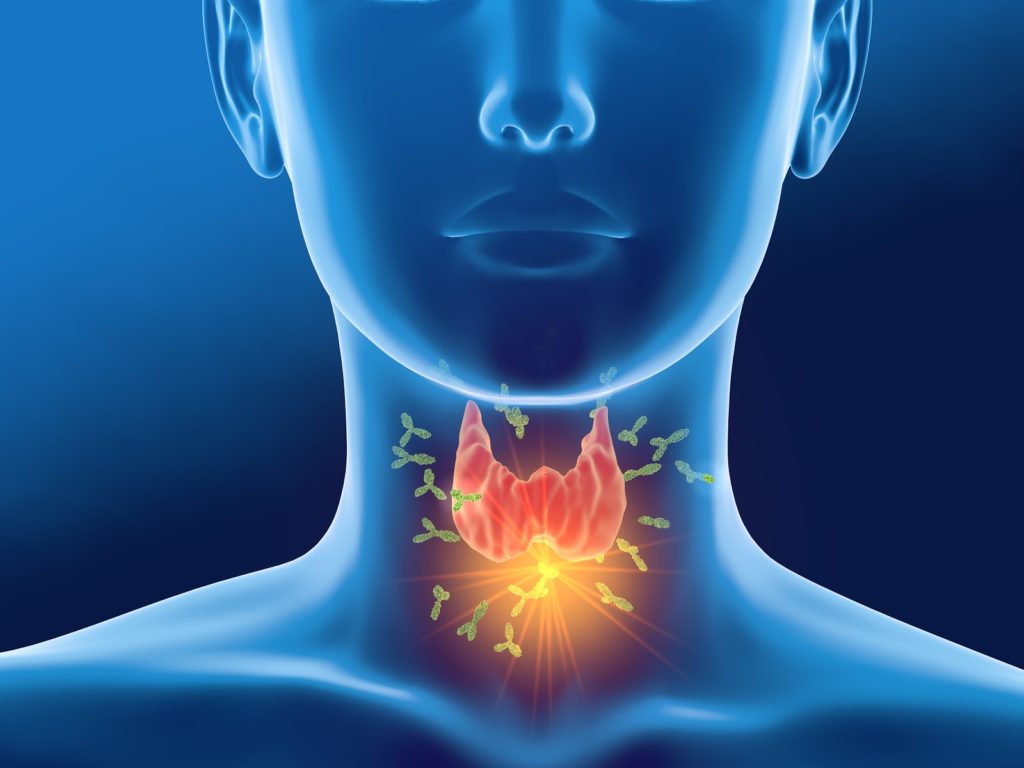
Hashimoto’s disease itself is an autoimmune disease in which the immune system attacks the thyroid gland, and it’s marked by elevated thyroid antibodies. But these changes occur gradually, meaning that it’s unlikely for a flare of symptoms to be caused by a surge in antibodies associated with Hashimoto’s. There’s likely something else at play– often a gut or female hormone imbalance, which we’ll cover in more detail below. In this article, we’ll explore how you can calm your immune system, lower inflammation, and feel better. But first, let’s take a closer look at the two distinct reasons for Hashimoto’s symptoms.
Symptoms of Hashimoto’s Flare Ups May Not Be What You Think
If you’ve been diagnosed with Hashimoto’s and you’re experiencing a sudden burst of symptoms, it’s natural to assume that it’s the Hashimoto’s itself that’s flaring up and causing the problem. But in fact, it’s unlikely for a Hashimoto’s “flare up” to be the cause of your symptoms. That’s because Hashimoto’s generally causes slow, subtle changes to the thyroid gland over the course of many years, which suggests that the TPO antibodies that characterize Hashimoto’s are not likely to be causing symptoms.
Studies of correlations between TPO antibodies and symptoms have suggested that high TPO antibodies are not associated with reduced quality of life or disease severity in general [2, 3]. Instead, symptoms that occur for those with Hashimoto’s are more likely to be caused by underlying gut imbalances or female hormone imbalances, rather than by Hashimoto’s or the elevated antibodies it’s associated with.
Immune System Activation
Hashimoto’s disease is an autoimmune disorder that affects thyroid function. As with all autoimmune diseases, the body’s immune system attacks its own tissues in a case of mistaken identity. With Hashimoto’s, this overzealous immune response causes thyroid inflammation or thyroiditis.
When you experience symptoms of Hashimoto’s flare-up, you’re likely having an autoimmune flare. This means that your immune system has gone into overdrive and is generating inflammation.
For many thyroid patients, the root cause of an inflammatory flare is linked to poor gut health in what’s known as the gut-thyroid connection [4]. Improving your gut health can calm inflammation, reduce symptoms of a Hashimoto’s flare up, and decrease thyroid autoimmunity [5, 6, 7, 8, 9, 10, 11, 12]. It may also be related to an imbalance of the female hormone estrogen (which can often be rooted in gut issues too).
Low Thyroid Function
Over time, the inflammatory process can damage the thyroid gland and impair thyroid function, eventually leading to thyroid issues like hypothyroidism.
It’s important to note that although Hashimoto’s is the most common cause of hypothyroidism, not everyone who has Hashimoto’s has hypothyroidism. In fact, in the majority of cases, Hashimoto’s does not lead to hypothyroidism– only 9-19% of individuals with the autoimmune condition develop hypothyroidism [1].
The idea that Hashimoto’s automatically means hypothyroidism is a common misconception that can lead to overtreatment of thyroid issues when thyroid hormone levels are actually not a problem.
If you do have hypothyroidism, your thyroid gland does not produce enough T4 thyroid hormone (thyroxine). Your bloodwork may also show high TSH (thyroid stimulating hormone), which is produced by the pituitary gland and used to make T4. When you have impaired thyroid function, TSH is underutilized, so the number gets higher. The disruption of low T4 causes your metabolism to slow down. Symptoms of hypothyroidism (underactive thyroid), include:
- Fatigue
- Dry skin
- Hair loss
- Weight gain
- Brain fog
- Poor mood
- Decreased heart rate
- Inconsistent menstrual cycle

Thyroid Medication
Hypothyroidism is easily treated with thyroid replacement hormone. Levothyroxine (Synthroid) is the most commonly prescribed thyroid medication.
If you are taking thyroid medication and your lab results are normal, you shouldn’t experience symptoms of hypothyroidism. However, many patients do continue to struggle with tiredness, brain fog, poor mood, and other symptoms, despite taking medication.
In this case, your symptoms are likely caused by inflammation and dysfunction in the gut-thyroid connection, not a lack of thyroid hormone.
The Gut-Thyroid Connection
Fatigue, brain fog, and mood issues aren’t just associated with autoimmune thyroid disease. They are also common symptoms of gut disorders. And while Hashimoto’s and hypothyroidism affect 1-2% and 0.6% of the population respectively, functional gastrointestinal disorders affect an estimated 40% [13, 14].
Here are a few examples:
- More than 50% of IBS (irritable bowel syndrome) patients have symptoms of fatigue, according to a meta-analysis of 17 studies [15].
- Sixty-eight percent of patients with suspected non-celiac gluten sensitivity reported a lack of well-being [16]. These patients also reported tiredness (64%), headache (54%), anxiety (39%), brain fog (38%), and other non-digestive symptoms.
- In a systematic review, IBS patients were three times as likely as healthy subjects to have either anxiety or depression [17].
- Depression is prevalent in both IBS and IBD (inflammatory bowel disease) patients [18].
Other studies associate gut conditions with sleep disorders [19], headaches [16, 20], dermatitis [21], rosacea [22], and joint pain [23].
Gut health and thyroid health go hand-in-hand, as do gut health and many other systems in your body. While there may be a genetic component to predispose a person to thyroid issues or other autoimmunity, there’s a good chance that poor gut health can turn those genes on. Likewise, improving gut health can help quell, lessen, or even eliminate the problem.
Female Sex Hormones and Thyroid
When your endocrine system (the system in your body that regulates all sorts of hormones, including thyroid hormone, stress hormones, and sex hormones) goes haywire, you can experience a lot of the same symptoms as when you have poor gut health. This includes mood swings, irritability, headache, fatigue, constipation, abdominal cramping, anxiety, insomnia, and more [24].
Hormones are powerful chemicals. Understanding the feedback loop between gut health and hormonal health — especially how stress plays a role in disrupting balance — in addition to the interplay within the greater endocrine system (sex hormones, thyroid hormones, and others that may be affected) might help you get to the root cause of your flare ups a lot more successfully.
Stress is a major factor across the spectrum of challenges I’ve just enumerated. When you experience stress, your body puts energy toward creating stress hormones like cortisol rather than creating sex hormones like estrogen and testosterone. It also puts more energy into fight or flight, sending blood to your muscles rather than putting energy toward digesting your food.
High levels of stress also increases gut permeability (leaky gut) and negatively impacts your gut microbiome [25, 26]. Interestingly, female hormonal fluctuation can also affect your digestion (you may experience digestive upset as a PMS symptom, for example) [27].
What Happens to Thyroid Health When Gut Conditions Are Treated?

Treating the gut has been shown to have a direct, positive impact on thyroid health. For example:
- One small study found a remarkable drop in TPO antibodies (a marker of autoimmune thyroiditis) when patients were treated for H. pylori gut infections [5]. Other studies show that treating H. pylori can improve TSH levels [6, 7, 11].
- Treating Blastocystis hominis (a parasitic gut infection) has been shown to reduce inflammatory markers, thyroid antibodies, and TSH levels [8].
- Gut treatments have also been shown to improve thyroid-like symptoms, including fatigue [28, 29, 30], mild to moderate depression [31], and anxiety [32].
- Eliminating common trigger foods can also be helpful for some thyroid patients. In one study, lactose restriction led to a significant decrease in TSH levels for thyroid patients with lactose intolerance [9]. Another study found that a gluten-free diet reduced the need for thyroid medication in patients with atypical celiac disease [10].
Improving your gut health is an important part of an overall plan for better thyroid health.
How to Prevent Symptoms of Hashimoto’s Flare-Ups

If you have Hashimoto’s disease and struggle with symptoms of “Hashimoto’s flare-ups”, there’s a lot you can do to feel better and regain your energy.
Take a step-by-step approach to address the most fundamental health and wellness foundations first. For some patients, symptoms will start to resolve after taking a few steps. Other patients will need to complete more steps.
1. Get Your Thyroid Hormone Levels in Range
An important first step is to resolve true hypothyroid symptoms with medication. Keep in mind that while thyroid hormone medication is important for those with true hypothyroidism, it has been found not to be helpful for those with subclinical hypothyroidism (in spite of it commonly and erroneously being prescribed for the latter) [33, 34]. If you’re unsure, you can use the guide here to help you and your practitioner interpret your thyroid test results.
Standard blood tests for thyroid hormone levels are simple, straightforward, and very accurate:
- High TSH and low free T4 indicate hypothyroidism
- Low TSH and high free T4 indicate hyperthyroidism (overactive thyroid, Grave’s disease)
If you are hypothyroid, a thyroid medication like Synthroid (levothyroxine) can help get your TSH and T4 levels in range.
Once your TSH and T4 levels are normal, don’t try to optimize your medication for better results. Focus your next steps on calming the immune system and reducing inflammation.
2. Make Lifestyle Improvements
An unhealthy lifestyle can contribute to your autoimmune condition. Along with poor diet, here are the most common lifestyle issues I see in my Hashimoto’s patients:
- Lack of sleep
- Too much or too little exercise
- Too much stress (cortisol)
- Poorly controlled blood sugar
If you identify any of these issues as problem areas for you, take steps to improve your lifestyle and work on practicing better self-care.
3. Eat an Anti-Inflammatory Diet
Eating a simple, real food diet is the foundation of gut and thyroid health. A healthy diet can reduce the burden of inflammation in your body, improve your gut health, and reduce symptoms [35, 36, 37, 38, 39].
There’s no one-size-fits-all thyroid diet. However, these dietary approaches are often helpful:
- Don’t eat processed foods. Eat foods free of additives and chemical preservatives.
- You can try a lower-carb diet. It was shown in one study to reduce thyroid antibodies by 44% in people with Hashimoto’s thyroiditis (but not celiac disease) [40].
- Identify and remove foods that trigger your symptoms. A gluten-free diet(or gluten-reduced) may help reduce antibodies [41].
- A low-iodine diet or avoiding supplemental iodine sources may be helpful for thyroid patients [42].
If you want to follow a specific diet template or meal plan, the paleo diet is anti-inflammatory, lower in carbs and trigger foods, and suitable as a long-term diet.
If a paleo-type diet doesn’t resolve all of your symptoms, the AIP diet (autoimmune paleo or autoimmune protocol) is a good next step. The AIP diet is an elimination diet intended to help you identify food triggers that cause inflammatory symptoms. In extreme or severe cases, you might consider a gut reset with the elemental diet. It’s been shown to help with gas, bloating, and other digestive issues. However, seek medical advice regarding this diet.
4. Take Probiotics
Probiotics are effective because they work to balance the community of microorganisms that live in your gut [43], fight harmful microorganisms [44, 45, 46], promote a healthy immune response [47, 48, 49], and reduce inflammation [43].
A study of hypothyroid patients found that probiotic supplements reduced the need for thyroid medication and reduced fatigue [12].
5. Take Supplements
Vitamin D may improve your thyroid health and lower thyroid antibodies [50, 51, 52]. Safe sun exposure is free and the most bioavailable way to get adequate vitamin D. Supplemental vitamin D is recommended during winter months in higher latitudes.
Selenium supplements can reduce TPO antibodies in thyroid patients [53, 54]. However, long-term supplementation is less beneficial [55, 56]. Consider 3-6 months of supplementation to boost your selenium levels.
Supplementing with HCI (betaine hydrochloride) can increase stomach acid levels, and may help with the absorption of iron, vitamin B12, and thyroid medication. Up to 40% of hypothyroid patients may have low stomach acid [57, 58].
Some thyroid patients may benefit from iron supplementation. If your blood tests show serum ferritin (the storage form of iron) levels significantly below 100 mg/l with iron, supplementing with iron may help to improve fatigue [59].
6. Treat Gut Infections
If lifestyle improvements, diet, and probiotics haven’t fully resolved your symptoms, the next step is to look for hidden gut infections.
Research shows a correlation between thyroid problems and gut infections, including SIBO (small intestinal bacterial overgrowth) [60, 61], H. pylori infection [62, 63], and B. hominis infection [8].
Testing for and treating gut infections is best done with the help of an experienced health practitioner.
7. Adjust Thyroid Medications
As your gut health improves, you may absorb your thyroid medication better. Lab tests and consultation with your doctor can help to determine if you need to fine tune your thyroid medication. This is important, as you don’t want to go too far in the wrong direction and send yourself into hyperthyroid, which has a whole other list of symptoms (including heart palpitations).
Some patients may need alternative thyroid medication, such as T4/T3 combination therapy, but this is not the majority.
Should You Be Concerned About Thyroid Antibodies?
Thyroid tests for TPO antibodies measure the degree of autoimmune activity in Hashimoto’s disease [64]. TPO levels over 35 IU/mL are generally considered positive for autoimmunity.
Many patients are able to significantly reduce TPO levels through diet and lifestyle changes or by treating a gut infection. However, you don’t need to lower your TPO levels to zero. In fact, striving to do so can create stress and be counterproductive.
Research shows that patients with TPO levels below 300 are unlikely to become hypothyroid [1] and patients with TPO levels below 500 have minimal risk of becoming hypothyroid [65]. Essentially, there is not enough autoimmune activity to significantly damage the thyroid gland at these levels.
If your TPO levels are high, a sensible goal is to get your TPO level below 500.
You Don’t Need to Be Tired and Frustrated with Hashimoto’s
If you struggle with ongoing symptoms, keep in mind that more thyroid medication may not be the answer. Even if your symptoms are not necessarily symptoms of Hashimoto’s flare ups, they can usually be improved by addressing underlying imbalances that are contributing to inflammation.
Poor gut health is a very common cause of symptoms like fatigue, brain fog, poor mood, weight gain, and more. This may be a bigger contributor to your symptoms than your thyroid hormone levels or thyroid antibody levels.
Luckily, focusing on your gut health and attending to your daily habits like sleep or stress management can help you manage and resolve symptoms. For more individualized guidance, reach out to our functional health center.
The Ruscio Institute has developed a range of high quality formulations to help our patients and audience. If you’re interested in learning more about these products, please click here. Note that there are many other options available, and we encourage you to research which products may be right for you.
Dr. Michael Ruscio is a DC, Naturopathic Practitioner, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.➕ References
- Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The Prevalence, Incidence and Natural Course of Positive Antithyroperoxidase Antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS ONE. 2017 Jan 4;12(1):e0169283. DOI: 10.1371/journal.pone.0169283. PMID: 28052092. PMCID: PMC5215694.
- Patti M, Christian R, Palokas M. Association between anti-thyroid antibodies and quality of life in patients with Hashimoto thyroiditis: a systematic review and meta-analysis. JBI Evid Synth. 2021 Mar 17;19(9):2307–38. DOI: 10.11124/JBIES-20-00043. PMID: 33741837.
- Mincer DL, Jialal I. Hashimoto Thyroiditis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. PMID: 29083758.
- Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function? Nutrients. 2020 Jun 12;12(6). DOI: 10.3390/nu12061769. PMID: 32545596. PMCID: PMC7353203.
- Bertalot G, Montresor G, Tampieri M, Spasiano A, Pedroni M, Milanesi B, et al. Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection. Clin Endocrinol (Oxf). 2004 Nov;61(5):650–2. DOI: 10.1111/j.1365-2265.2004.02137.x. PMID: 15521972.
- Ribichini D, Fiorini G, Repaci A, Castelli V, Gatta L, Vaira D, et al. Tablet and oral liquid L-thyroxine formulation in the treatment of naïve hypothyroid patients with Helicobacter pylori infection. Endocrine. 2017 Sep;57(3):394–401. DOI: 10.1007/s12020-016-1167-3. PMID: 27848196.
- Centanni M, Gargano L, Canettieri G, Viceconti N, Franchi A, Delle Fave G, et al. Thyroxine in goiter, Helicobacter pylori infection, and chronic gastritis. N Engl J Med. 2006 Apr 27;354(17):1787–95. DOI: 10.1056/NEJMoa043903. PMID: 16641395.
- El-Zawawy HT, Farag HF, Tolba MM, Abdalsamea HA. Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17. Ther Adv Endocrinol Metab. 2020 Feb 21;11:2042018820907013. DOI: 10.1177/2042018820907013. PMID: 32128107. PMCID: PMC7036484.
- Asik M, Gunes F, Binnetoglu E, Eroglu M, Bozkurt N, Sen H, et al. Decrease in TSH levels after lactose restriction in Hashimoto’s thyroiditis patients with lactose intolerance. Endocrine. 2014 Jun;46(2):279–84. DOI: 10.1007/s12020-013-0065-1. PMID: 24078411.
- Virili C, Bassotti G, Santaguida MG, Iuorio R, Del Duca SC, Mercuri V, et al. Atypical celiac disease as cause of increased need for thyroxine: a systematic study. J Clin Endocrinol Metab. 2012 Mar;97(3):E419-22. DOI: 10.1210/jc.2011-1851. PMID: 22238404.
- Bugdaci MS, Zuhur SS, Sokmen M, Toksoy B, Bayraktar B, Altuntas Y. The role of Helicobacter pylori in patients with hypothyroidism in whom could not be achieved normal thyrotropin levels despite treatment with high doses of thyroxine. Helicobacter. 2011 Apr;16(2):124–30. DOI: 10.1111/j.1523-5378.2011.00830.x. PMID: 21435090.
- Talebi S, Karimifar M, Heidari Z, Mohammadi H, Askari G. The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial. Complement Ther Med. 2020 Jan;48:102234. DOI: 10.1016/j.ctim.2019.102234. PMID: 31987229.
- Carlé A, Pedersen IB, Knudsen N, Perrild H, Ovesen L, Laurberg P. Hypothyroid symptoms and the likelihood of overt thyroid failure: a population-based case-control study. Eur J Endocrinol. 2014 Nov;171(5):593–602. DOI: 10.1530/EJE-14-0481. PMID: 25305308.
- Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of rome foundation global study. Gastroenterology. 2021 Jan;160(1):99-114.e3. DOI: 10.1053/j.gastro.2020.04.014. PMID: 32294476.
- Han CJ, Yang GS. Fatigue in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis of Pooled Frequency and Severity of Fatigue. Asian Nurs Res (Korean Soc Nurs Sci). 2016 Mar;10(1):1–10. DOI: 10.1016/j.anr.2016.01.003. PMID: 27021828.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR, Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12(1):85. DOI: 10.1186/1741-7015-12-85. PMID: 24885375. PMCID: PMC4053283.
- Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2019 Jul;50(2):132–43. DOI: 10.1111/apt.15325. PMID: 31157418.
- Geng Q, Zhang Q-E, Wang F, Zheng W, Ng CH, Ungvari GS, et al. Comparison of comorbid depression between irritable bowel syndrome and inflammatory bowel disease: A meta-analysis of comparative studies. J Affect Disord. 2018 Sep;237:37–46. DOI: 10.1016/j.jad.2018.04.111. PMID: 29758449.
- Wang B, Duan R, Duan L. Prevalence of sleep disorder in irritable bowel syndrome: A systematic review with meta-analysis. Saudi J Gastroenterol. 2018 Jun;24(3):141–50. DOI: 10.4103/sjg.SJG_603_17. PMID: 29652034. PMCID: PMC5985632.
- Li C, Yu S, Li H, Zhou J, Liu J, Tang W, et al. Clinical features and risk factors for irritable bowel syndrome in Migraine patients. Pak J Med Sci Q. 2017 Jun;33(3):720–5. DOI: 10.12669/pjms.333.12379. PMID: 28811802. PMCID: PMC5510134.
- Ianiro G, Rizzatti G, Napoli M, Matteo MV, Rinninella E, Mora V, et al. A Durum Wheat Variety-Based Product Is Effective in Reducing Symptoms in Patients with Non-Celiac Gluten Sensitivity: A Double-Blind Randomized Cross-Over Trial. Nutrients. 2019 Mar 27;11(4). DOI: 10.3390/nu11040712. PMID: 30934747. PMCID: PMC6521061.
- Parodi A, Paolino S, Greco A, Drago F, Mansi C, Rebora A, et al. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008 Jul;6(7):759–64. DOI: 10.1016/j.cgh.2008.02.054. PMID: 18456568.
- Podas T, Nightingale JMD, Oldham R, Roy S, Sheehan NJ, Mayberry JF. Is rheumatoid arthritis a disease that starts in the intestine? A pilot study comparing an elemental diet with oral prednisolone. Postgrad Med J. 2007 Feb;83(976):128–31. DOI: 10.1136/pgmj.2006.050245. PMID: 17308218. PMCID: PMC2805936.
- Gudipally PR, Sharma GK. Premenstrual Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. PMID: 32809533.
- Vanuytsel T, van Wanrooy S, Vanheel H, Vanormelingen C, Verschueren S, Houben E, et al. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut. 2014 Aug;63(8):1293–9. DOI: 10.1136/gutjnl-2013-305690. PMID: 24153250.
- Karl JP, Margolis LM, Madslien EH, Murphy NE, Castellani JW, Gundersen Y, et al. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am J Physiol Gastrointest Liver Physiol. 2017 Jun 1;312(6):G559–71. DOI: 10.1152/ajpgi.00066.2017. PMID: 28336545.
- Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. 2014 Jun 14;20(22):6725–43. DOI: 10.3748/wjg.v20.i22.6725. PMID: 24944465. PMCID: PMC4051914.
- Maes M, Leunis J-C. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Neuro Endocrinol Lett. 2008 Dec;29(6):902–10. PMID: 19112401.
- Altobelli E, Del Negro V, Angeletti PM, Latella G. Low-FODMAP Diet Improves Irritable Bowel Syndrome Symptoms: A Meta-Analysis. Nutrients. 2017 Aug 26;9(9). DOI: 10.3390/nu9090940. PMID: 28846594. PMCID: PMC5622700.
- Marum AP, Moreira C, Saraiva F, Tomas-Carus P, Sousa-Guerreiro C. A low fermentable oligo-di-mono saccharides and polyols (FODMAP) diet reduced pain and improved daily life in fibromyalgia patients. Scand J Pain. 2016 Aug 22;13:166–72. DOI: 10.1016/j.sjpain.2016.07.004. PMID: 28850525.
- Ng QX, Peters C, Ho CYX, Lim DY, Yeo W-S. A meta-analysis of the use of probiotics to alleviate depressive symptoms. J Affect Disord. 2018 Mar 1;228:13–9. DOI: 10.1016/j.jad.2017.11.063. PMID: 29197739.
- Yang B, Wei J, Ju P, Chen J. Effects of regulating intestinal microbiota on anxiety symptoms: A systematic review. Gen Psych. 2019 May 17;32(2):e100056. DOI: 10.1136/gpsych-2019-100056. PMID: 31179435. PMCID: PMC6551444.
- Burgos N, Toloza FJK, Singh Ospina NM, Brito JP, Salloum RG, Hassett LC, et al. Clinical Outcomes After Discontinuation of Thyroid Hormone Replacement: A Systematic Review and Meta-Analysis. Thyroid. 2021 May;31(5):740–51. DOI: 10.1089/thy.2020.0679. PMID: 33161885. PMCID: PMC8110016.
- Livadas S, Bothou C, Androulakis I, Boniakos A, Angelopoulos N, Duntas L. Levothyroxine replacement therapy and overuse: A timely diagnostic approach. Thyroid. 2018 Nov 30; DOI: 10.1089/thy.2018.0014. PMID: 30351232.
- Torpy DJ, Tsigos C, Lotsikas AJ, Defensor R, Chrousos GP, Papanicolaou DA. Acute and delayed effects of a single-dose injection of interleukin-6 on thyroid function in healthy humans. Metab Clin Exp. 1998 Oct;47(10):1289–93. DOI: 10.1016/s0026-0495(98)90338-9. PMID: 9781636.
- van der Poll T, Romijn JA, Wiersinga WM, Sauerwein HP. Tumor necrosis factor: a putative mediator of the sick euthyroid syndrome in man. J Clin Endocrinol Metab. 1990 Dec;71(6):1567–72. DOI: 10.1210/jcem-71-6-1567. PMID: 2229314.
- Boelen A, Platvoet-Ter Schiphorst MC, Wiersinga WM. Association between serum interleukin-6 and serum 3,5,3’-triiodothyronine in nonthyroidal illness. J Clin Endocrinol Metab. 1993 Dec;77(6):1695–9. DOI: 10.1210/jcem.77.6.8263160. PMID: 8263160.
- Bartalena L, Brogioni S, Grasso L, Velluzzi F, Martino E. Relationship of the increased serum interleukin-6 concentration to changes of thyroid function in nonthyroidal illness. J Endocrinol Invest. 1994 Apr;17(4):269–74. DOI: 10.1007/BF03348974. PMID: 7930379.
- Bartalena L, Bogazzi F, Brogioni S, Grasso L, Martino E. Role of cytokines in the pathogenesis of the euthyroid sick syndrome. Eur J Endocrinol. 1998 Jun;138(6):603–14. DOI: 10.1530/eje.0.1380603. PMID: 9678522.
- Esposito T, Lobaccaro JM, Esposito MG, Monda V, Messina A, Paolisso G, et al. Effects of low-carbohydrate diet therapy in overweight subjects with autoimmune thyroiditis: possible synergism with ChREBP. Drug Des Devel Ther. 2016 Sep 14;10:2939–46. DOI: 10.2147/DDDT.S106440. PMID: 27695291. PMCID: PMC5028075.
- Krysiak R, Szkróbka W, Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes. 2019 Jul;127(7):417–22. DOI: 10.1055/a-0653-7108. PMID: 30060266.
- Katagiri R, Yuan X, Kobayashi S, Sasaki S. Effect of excess iodine intake on thyroid diseases in different populations: A systematic review and meta-analyses including observational studies. PLoS ONE. 2017 Mar 10;12(3):e0173722. DOI: 10.1371/journal.pone.0173722. PMID: 28282437. PMCID: PMC5345857.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106–13. DOI: 10.2174/1389200219666180813144834. PMID: 30101706. PMCID: PMC6340155.
- Wang F, Feng J, Chen P, Liu X, Ma M, Zhou R, et al. Probiotics in Helicobacter pylori eradication therapy: Systematic review and network meta-analysis. Clin Res Hepatol Gastroenterol. 2017 Sep;41(4):466–75. DOI: 10.1016/j.clinre.2017.04.004. PMID: 28552432.
- García-Collinot G, Madrigal-Santillán EO, Martínez-Bencomo MA, Carranza-Muleiro RA, Jara LJ, Vera-Lastra O, et al. Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020 Apr;65(4):1134–43. DOI: 10.1007/s10620-019-05830-0. PMID: 31549334.
- Greco A, Caviglia GP, Brignolo P, Ribaldone DG, Reggiani S, Sguazzini C, et al. Glucose breath test and Crohn’s disease: Diagnosis of small intestinal bacterial overgrowth and evaluation of therapeutic response. Scand J Gastroenterol. 2015 May 19;50(11):1376–81. DOI: 10.3109/00365521.2015.1050691. PMID: 25990116.
- Toribio-Mateas M. Harnessing the power of microbiome assessment tools as part of neuroprotective nutrition and lifestyle medicine interventions. Microorganisms. 2018 Apr 25;6(2). DOI: 10.3390/microorganisms6020035. PMID: 29693607. PMCID: PMC6027349.
- Stenman LK, Lehtinen MJ, Meland N, Christensen JE, Yeung N, Saarinen MT, et al. Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults-Randomized Controlled Trial. EBioMedicine. 2016 Nov;13:190–200. DOI: 10.1016/j.ebiom.2016.10.036. PMID: 27810310. PMCID: PMC5264483.
- Frei R, Akdis M, O’Mahony L. Prebiotics, probiotics, synbiotics, and the immune system: experimental data and clinical evidence. Curr Opin Gastroenterol. 2015 Mar;31(2):153–8. DOI: 10.1097/MOG.0000000000000151. PMID: 25594887.
- Mackawy AMH, Al-Ayed BM, Al-Rashidi BM. Vitamin d deficiency and its association with thyroid disease. Int J Health Sci (Qassim). 2013 Nov;7(3):267–75. PMID: 24533019. PMCID: PMC3921055.
- Bozkurt NC, Karbek B, Ucan B, Sahin M, Cakal E, Ozbek M, et al. The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis. Endocr Pract. 2013 Jun;19(3):479–84. DOI: 10.4158/EP12376.OR. PMID: 23337162.
- Wang S, Wu Y, Zuo Z, Zhao Y, Wang K. The effect of vitamin D supplementation on thyroid autoantibody levels in the treatment of autoimmune thyroiditis: a systematic review and a meta-analysis. Endocrine. 2018 Mar;59(3):499–505. DOI: 10.1007/s12020-018-1532-5. PMID: 29388046.
- Wichman J, Winther KH, Bonnema SJ, Hegedüs L. Selenium Supplementation Significantly Reduces Thyroid Autoantibody Levels in Patients with Chronic Autoimmune Thyroiditis: A Systematic Review and Meta-Analysis. Thyroid. 2016 Dec;26(12):1681–92. DOI: 10.1089/thy.2016.0256. PMID: 27702392.
- Gärtner R, Gasnier BCH. Selenium in the treatment of autoimmune thyroiditis. Biofactors. 2003;19(3–4):165–70. DOI: 10.1002/biof.5520190309. PMID: 14757967.
- Winther KH, Wichman JEM, Bonnema SJ, Hegedüs L. Insufficient documentation for clinical efficacy of selenium supplementation in chronic autoimmune thyroiditis, based on a systematic review and meta-analysis. Endocrine. 2017 Feb;55(2):376–85. DOI: 10.1007/s12020-016-1098-z. PMID: 27683225. PMCID: PMC5272877.
- Zheng H, Wei J, Wang L, Wang Q, Zhao J, Chen S, et al. Effects of Selenium Supplementation on Graves’ Disease: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2018 Sep 26;2018:3763565. DOI: 10.1155/2018/3763565. PMID: 30356415. PMCID: PMC6178160.
- Lahner E, Annibale B. Pernicious anemia: new insights from a gastroenterological point of view. World J Gastroenterol. 2009 Nov 7;15(41):5121–8. DOI: 10.3748/wjg.15.5121. PMID: 19891010. PMCID: PMC2773890.
- Sterzl I, Hrdá P, Matucha P, Čeřovská J, Zamrazil V. Anti-Helicobacter Pylori, anti-thyroid peroxidase, anti-thyroglobulin and anti-gastric parietal cells antibodies in Czech population. Physiol Res. 2008 Feb 13;57 Suppl 1:S135–41. DOI: 10.33549/physiolres.931498. PMID: 18271683.
- Rayman MP. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc Nutr Soc. 2019 Feb;78(1):34–44. DOI: 10.1017/S0029665118001192. PMID: 30208979.
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017 Feb 7;23(5):842–52. DOI: 10.3748/wjg.v23.i5.842. PMID: 28223728. PMCID: PMC5296200.
- Konrad P, Chojnacki J, Kaczka A, Pawłowicz M, Rudnicki C, Chojnacki C. [Thyroid dysfunction in patients with small intestinal bacterial overgrowth]. Pol Merkur Lekarski. 2018 Jan 23;44(259):15–8. PMID: 29374417.
- Shi W-J, Liu W, Zhou X-Y, Ye F, Zhang G-X. Associations of Helicobacter pylori infection and cytotoxin-associated gene A status with autoimmune thyroid diseases: a meta-analysis. Thyroid. 2013 Oct;23(10):1294–300. DOI: 10.1089/thy.2012.0630. PMID: 23544831.
- Choi YM, Kim TY, Kim EY, Jang EK, Jeon MJ, Kim WG, et al. Association between thyroid autoimmunity and Helicobacter pylori infection. Korean J Intern Med. 2017 Mar;32(2):309–13. DOI: 10.3904/kjim.2014.369. PMID: 28092700. PMCID: PMC5339455.
- Fröhlich E, Wahl R. Thyroid Autoimmunity: Role of Anti-thyroid Antibodies in Thyroid and Extra-Thyroidal Diseases. Front Immunol. 2017 May 9;8:521. DOI: 10.3389/fimmu.2017.00521. PMID: 28536577. PMCID: PMC5422478.
- Ehlers M, Jordan AL, Feldkamp J, Fritzen R, Quadbeck B, Haase M, et al. Anti-Thyroperoxidase Antibody Levels >500 IU/ml Indicate a Moderately Increased Risk for Developing Hypothyroidism in Autoimmune Thyroiditis. Horm Metab Res. 2016 Sep 8;48(10):623–9. DOI: 10.1055/s-0042-112815. PMID: 27607246.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!