- Overview Context:
- Estelle is a 59 yo menopausal female seeking improvement in overall health. Her major symptoms are joint pain, stomach discomfort, acne, rosacea, and migraines.
Symptoms and Concerns
- Initial Symptoms:
- Abdominal pain
- Acid reflux
- Joint pain
- Acne
- Rosacea
- Migraines
- Onset, Timeline, and History:
- Acne and rosacea began around age 32, concurrent with onset of migraines
- Joint pain began at age 40 and has progressively gotten worse
Past Medical History
Prior diagnosis
- Rheumatoid arthritis
- Medications:
- Celecoxib (NSAID)
- Meloxicam (NSAID)
- Sulfasalazine
- Dexilant
- Spironolactone
- Premarin (oral estrogen)
Prior Testing and Treatment History
- Previous Diets:
- Whole 30 (Paleo Diet)
- 10% improvement in joint pain
- Intermittent fasting
- Improved bloating, lost 12 pounds
- Stopped due to becoming lightheaded
- Previous Treatments:
- Antibiotics
- Improved acne and rosacea
- Antibiotics
- Clinical Commentary:
- Inflammatory joint pain and rosacea are two symptoms that are frequently associated with dysbiosis, and they often improve when the gut is treated. A few aspects of her history indicate she’ll do well working through our treatment approach:
- Joint pain improved (even slightly) with an anti-inflammatory diet
- Acne and rosacea improved with antibiotics (predicts dysbiosis)
- Inflammatory joint pain and rosacea are two symptoms that are frequently associated with dysbiosis, and they often improve when the gut is treated. A few aspects of her history indicate she’ll do well working through our treatment approach:
- Diet:
- “Relaxed” Paleo diet
- Aim for 50% improvement over current diet quality by mostly eliminating processed foods and significantly limiting dairy and gluten intake
- Begin intermittent fasting for 12-16 hours daily
- Health coaching appointment to support dietary change
- Lifestyle:
- Continue to walk 10 minutes twice daily
- Treatment:
- Elemental diet exclusively for 2-4 days
- Lactobacillus & bifidobacterium, saccharomyces boulardii, and soil-based probiotics
- GI support nutrients
- Followup: 5 weeks
- Clinician Comments
- I frequently have patients start with elemental dieting as a trial. This is often a game changer when a patient has reported they feel better with fasting.
- Our goal was to start with modest improvements to Estelle’s lifestyle, beginning to walk a little and improving the quality of her diet by 50%. My hope was these changes in combination with basic supplementation would significantly shift her symptoms.
- Subjective Assessment
- Current Symptoms:
- Improved:
- Energy
- Stomach pain (gone)
- Reflux
- Same:
- Insomnia
- Worse:
- Acne
- Improved:
- Current Symptoms:
- Treatment Response:
- Intermittent fasting: Intermittent fasting daily and well tolerated
- Relaxed Paleo Diet: Reports significant improvement in energy and reduced stomach discomfort on relaxed Paleo diet
- Elemental Diet Reset: Unable to complete elemental diet for more than 1 day due to increased hunger
- Notes:
- 90% adherence to Paleo diet and daily IF
- Discontinued Dexilant (PPI medication) for reflux, but this led to rebound heartburn
- Discontinued spironolactone for acne
- Intermittent fasting: Intermittent fasting daily and well tolerated
- Updated Treatment Recommendations
- New Treatment:
- Increase dose of probiotics
- Begin herbal antimicrobials (HABx)
- Restart Dexilant and take every other day
- Followup: 4 weeks
- New Treatment:
- Clinician Comments
- Estelle was very eager to stop the PPI, and unfortunately experienced some rebound heartburn. In her case I recommended that she bring the PPI back on every other day. After we have further progress we will work to wean off this completely.
- Subjective Assessment
- Current Symptoms:
- Improved:
- Reflux/stomach issues gone
- Mild improvements in acne and joint pain
- Same:
- Poor sleep
- Worse:
- Energy (from poor sleep)
- Improved:
- Treatment Response:
- Herbal Antimicrobials: Mild improvement in joint pain and acne
- Current Symptoms:
- Impression:
- Estelle is making steady progress from a GI perspective. She had a positive but partial response to the Habx, suggesting we have a bit more work to do.
- Acne and joint pain are beginning to shift in a positive direction.
- She is still struggling with her sleep, so we decided to pivot towards using adaptogens, improve her sleep hygiene, have her try HeartMath, and discuss hormone replacement therapy (HRT) with her PCP.
- Updated Treatment Recommendations
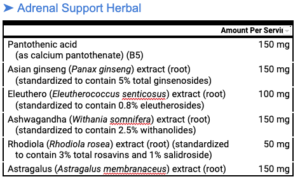
- New Treatment:
- Continue herbal antimicrobials
- Sleep:
- Reduce blue light exposure
- Add in passionflower extract
- Stress:
- Adrenal adaptogenic blend
- HeartMath biofeedback device for ten minutes twice daily
- Adrenal adaptogenic blend
- Referral:
- Follow up with PCP about HRT
- New Treatment:
- Subjective Assessment: 95% better overall
- Current Symptoms:
- Improved:
- Sleep
- Reflux
- Same:
- Joint pain
- Acne
- Worse:
- None
- Improved:
- Treatment Response:
- HABx: Reflux decreased
- HeartMath: Did not start
- Paleo diet: Difficulty maintaining this diet
- Estrogen patch (HRT): Sleeping better, more energy
- Sleep hygiene/passionflower: Sleeping better, more energy
- Current Symptoms:
- Impression:
- Estelle is sleeping better from better sleep hygiene and a prescription for an estrogen patch, which replaced her oral estrogen.
- Her heartburn is much improved, but Estelle is frustrated she hasn’t been able to come off her PPI yet.
- Estelle has been using NSAIDs (meloxicam and celecoxib) chronically to manage her joint pain. Ongoing use of these medications frequently slows GI healing.
- This seems to be the case for Estelle as she has progressed more slowly than would be expected.
- NSAIDs can also cause a number of rashes.
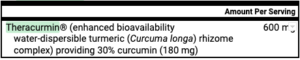
- The main symptom remaining is joint pain. We will try curcumin, which is frequently helpful for inflammatory joint pain in order to reduce NSAID use.
Updated Treatment Recommendations
- New Treatment:
- Start curcumin
- Talk to PCP about a suitable replacement for celecoxib
- “I’m worried that using celecoxib daily is slowing your progress, and is contributing to acne by hurting your GI health. I would prefer to reduce joint pain in other ways as we discussed. Please talk to your prescribing doctor about a replacement prescription.”
- Stop the herbal antimicrobials as the reflux is completely gone
- Slowly wean off Dexilant
- Followup: 5 weeks
- Start curcumin
- Subjective Assessment
- Current Symptoms:
- Improved:
- Sleeping much improved
- Joint pain
- Acne
- Same:
- None
- Worse:
- None
- Improved:
- Treatment Response:
- Curcumin: “The curcumin is helping me a lot! I hardly ever take the meloxicam for arthritis pain and when I do, just half the dose is usually enough.”
- Discontinuing Meloxicam: ”Heartburn disappeared when I stopped the meloxicam.”
- Current Symptoms:
- Impression:
- Curcumin significantly helped her joint pain, which gave Estelle the confidence to lower her NSAID dose, which in turn helped her further improve her gut health and eliminate her heartburn.
- Updated Treatment Recommendations
- New Treatment:
- Please continue your current program for 2-3 months, but try adding in some fasting
- After 2-3 months, we will work together to wean the GI support to the minimum needed to maintain improvement
- New Treatment:
Concluding thoughts
Estelle was a patient who I initially expected to be a simple case, but eventually required some problem solving and follow through to get her optimally well. It’s a good reminder not to give up, and to keep searching for drivers of illness, especially when patients don’t respond how you expect them to.
Her case is a good reminder that:
- Joint pain and rosacea frequently predict dysbiosis and therefore a positive response to diet, probiotics and herbal antimicrobials.
- NSAIDS may be the reason that your patient’s GI symptoms are not improving.
- Curcumin can be a very helpful tool to reduce joint pain.
- Give the body what it needs, remove any obstacles to cure, and allow the body time to heal.
Clinical Take Home Points
Review Background
- Thiamine, vitamin B1, has been suggested as beneficial in the setting of chronic fatigue given that it is a cofactor for enzymes necessary for glucose metabolism and ATP production. After learning that thiamine (and its derivative TTFD) was potentially helpful in the setting of chronic fatigue, we performed a review of the evidence. This led to us offering thiamine to our patients that were still experiencing fatigue despite having begun other therapies.
Inflammatory Bowel Disease
- Randomised clinical trial: high-dose oral thiamine versus placebo for chronic fatigue in patients with quiescent inflammatory bowel disease
- PMID: 33210299
- Pilot study investigating high dose thiamine (600-1800 mg /day) given for 4 weeks to patients with IBD and fatigue
- Compared to placebo, thiamine led to greater reductions in fatigue (-4.5 vs +0.75 points)
- The authors conclude: “We showed a significant beneficial effect of high-dose oral thiamine on chronic fatigue in IBD. The treatment was well tolerated.”
- Long-term maintenance treatment with 300 mg thiamine for fatigue in patients with inflammatory bowel disease: results from an open-label extension of the TARIF study
- PMID: 34592862
- This was a follow up to the above study from the same group
- Patients with IBD and fatigue were treated with either 300 mg thiamine daily or no treatment for 12 weeks
- “Regardless of allocation … fatigue severity increased in the study period… No significant effect of 300 mg oral thiamine was found.”
- “We found no beneficial effect on fatigue from thiamine taken in doses of 300 mg per day for 12 weeks following high-dose treatment.”
- Summary
- Higher-dose thiamine (600-1800 mg/day) led to greater improvements in fatigue compared to lower dose thiamine (300 mg/day)
- It is unclear if the increase in fatigue in the follow up study was related to an insufficient dose of thiamine or the longer treatment period of 12 weeks
Hashimoto’s thyroiditis
- Thiamine and Hashimoto’s thyroiditis: a report of three cases
- PMID: 24351023
- Three patients on thyroid hormone replacement for Hashimoto’s thyroiditis, still experiencing fatigue, were treated with either 600 mg oral or IV thiamine for 4 days.
- “Treatment with thiamine led to partial or complete regression of the fatigue within a few hours or days”
- Note: This was a small study with no placebo group.
Exercise-Induced Fatigue
- The effects of endurance training and thiamine supplementation on anti-fatigue during exercise
- PMID: 25566430
- 27 participants were randomized to one of the following for 1 month:
- Aerobic training alone
- Aerobic training + placebo
- Aerobic training + thiamine (10 mg/kg/day)
- Thiamine led to the greatest improvements in:
- rate of perceived exertion (RPE) (how hard one feels their body is working during exercise)
- Serum lactate (elevated in those with post-exertional malaise)
- Commentary: Thiamine led to a reduction in the RPE, which will likely allow an individual to exercise for longer, thus gaining more benefit from exercise.
- Effects of thiamine supplementation on exercise-induced fatigue
- PMID: 8815395
- 16 volunteers
- All were treated with the following for 3 days prior to a bout of exercise:
- Placebo
- Oral thiamine (TTFD) (100 mg/day)
- “Thiamine supplementation significantly suppressed the increase in blood glucose in the normal thiamine group and significantly decreased the number of complaints shortly after exercise in the subjective fatigue assessment of 30 items.”
How This Changes Clinical Practice
Clinical Takeaways
- Although there aren’t any large clinical trials, the current literature shows a pattern of effectiveness. This is a great example of being evidence-based, but not evidence limited
- We believe this therapy is worth considering as it is safe and low cost.
- We have found thiamine to be helpful for many (but not all) of our patients dealing with chronic fatigue. As of this writing, it seems to work best for reducing post-exertional malaise, which is common in many patients with ME/CFS, as well as improving brain fog, cognition, and overall energy.
- Consider using this therapy early on for patients who are struggling to muster the energy to make the changes that will help them heal, such as increased physical activity.
- TTFD, the thiamine derivative, is absorbed more effectively compared to thiamine salts, so we are pivoting to using TTFD with our patients.
- Given the above trials that showed initial benefit for 4 weeks, but worsening fatigue with longer term use, we recommend an initial trial of thiamine, after which we have them stop the supplement and observe how they feel. If their symptoms return, we ask them to continue it for another 12 weeks.
Background
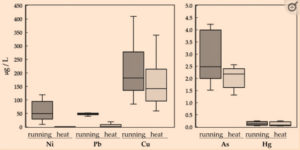
- In the December 2021 issue, we reviewed a paper showing that many toxic elements were preferentially excreted through sweat (especially Cd, Pb, Al, Ni).
Study purpose
- Does sweating induced by exercise or sauna lead to better detoxification of heavy metals?
Intervention:
- In this study, 12 healthy volunteers had sweat samples collected during both:
- Exercise (running) x 20 minutes
- Sauna therapy x 20 minutes
Main Results:
- “The results demonstrated that the sweating method affected the excretion of heavy metals in sweat, with the concentrations of Ni, Pb, Cu, and As being significantly higher during dynamic exercise than during sitting in the sauna.”
Clinician Commentary:
- While this study only included a small number of healthy volunteers, it showed the importance of exercise as a tool for detoxification.
- Note that only 20 minutes of exercise was necessary to increase the excretion of multiple heavy metals.
- Given the numerous benefits of sauna therapy, including reduced risk of cardiac death, all-cause mortality, Alzheimer’s Disease and improved depression and cardiorespiratory fitness, we encourage the combined use of regular exercise and sauna therapy to improve health.
Background
- Air pollution is well known to trigger asthmatic airway responsiveness and increased airway resistance.
Study purpose
- Does N-acetylcysteine reduce airway reactivity to air pollution in asthmatic patients?
Intervention:
- Healthy and asthmatic participants were randomized to the following for 6 days prior to exposure to clean or polluted air:
- Placebo
- NAC 600 mg 3x/day
Main Results:
- NAC supplementation led to:
- 20% reduction in baseline airway reactivity (prior to air pollution exposure)
- NO increase in airway reactivity when exposed to air pollution
- This study found the antioxidant supplement NAC had a protective effect against air pollution on lung function.
Clinician Commentary
- While asthmatic patients don’t make up a large part of the patient population at the clinic, we are increasingly aware of the consequences of air pollution, such as increased risk of all-cause mortality, cardiovascular disease, and certain types of cancer.
- NAC is safe and may be a helpful option for reducing the effects of air pollution.
When a patient has struggled with their health for a long time, it is understandable that they want to feel better right away. In order to help patients get better, we often have a bias that more treatment is better, however, this is not necessarily true.
Early in my career, after a patient began to see improvement in their symptoms, I regularly gave into the temptation of offering more treatment. “Okay, that worked, now let’s try this!” I now jokingly refer to this as “getting greedy for more improvement.”
Unfortunately, adding in more therapies too soon can cause us to either lose sight of what is working or neglect to build off the treatments that are helping. In the worst case scenario, we can actually make a patient feel worse by giving them something their bodies are not ready for.
These days, if a patient who has been experiencing symptoms for years tells me that they feel 10% better with an intervention, I’ll celebrate with them and coach them to double down and “ride the wave!” The idea is to see how far they can go because if you push them too hard, they might fall right off their surfboard!
It can be challenging to tell a patient that the best thing that they can do is to continue their program for 8 weeks and then check back in, but there are many times where it is simply the right approach to take. I’ve found that sometimes it’s wisest to get out of the way as soon as your patient begins to progress, because healing often requires time and consistency.