TREATING CLINICIAN: JOE MATHER, M.D.
Patient Summary: James
- James is a 73-year old man with a life-long history of constipation and atopic skin disease. His primary concern is dry, itchy skin that becomes unbearable 4-5x per week. This began around 2 years ago, but the last 6 months have been miserable.
- He reports asthma, allergies, severe sinus, and raw skin on hands his entire life. “As a child of the 50’s, I lived in farming country with constant crop spraying.” Asthma & eczema improved when he moved away.
- Patient has had multiple ICU visits due to allergic reaction to asthma medications/shots.
- Chief Complaints:
- Full-body itchy skin. Usually either above hips or legs & feet. Scalding showers required to stop itching.
- He also complains of constant dry, itching, and cracked skin on fingers and palms.
- James mentions that after almost every meal, he will fall asleep after eating within 5-10 minutes. When he wakes up, he reports the itching will have worsened.
- He reports “full body muscle tension that keeps him awake.” This is usually accompanied by shivers and anxiety.
- He also reports fatigue, asthma, episodes of constipation, mood swings/irritability, and depression.
- While James is an outwardly happy and optimistic person, he admits that his depression and anxiety have been severe.
- Full-body itchy skin. Usually either above hips or legs & feet. Scalding showers required to stop itching.
- Prior Diagnosis:
- Asthma and allergies
- Shingles – Jan 2019 through October 2020
- Depression and Anxiety from 30’s-60’s
- Alcoholic from early 40’s until rehab at age of 61
- Medications:
- Flovent Diskus 250 mcg before bed (not consistent in taking this)
- Proair AFA Albuterol Sulfate Inhaler – taken as needed
- Treatment History Summary:
- He has pursued multiple alternative medical treatments (energy medicine, homeopathy, meditation, breathwork) and conventional therapies. He has tried many different types of supplements.
- He has tried various restrictive diets: “I eat a low sulfur diet. I’ve been grain-free, nut-free, red meat-free, nightshade-free for 2 years, and milk-free for my entire life. I don’t eat chard, kale, cabbage, pineapple, bananas.”
- Onset:
- Moved into his current home 3 years ago and began to worsen with increasing rash, body pain, and fatigue. He notes black mold in the home. Two years ago, he experienced a full-body breakout that looked and felt like shingles.
- Clinical Comments:
A few items stood out after meeting James:
- James looks to be experiencing extreme mast cell reactivity based on repetitive experience of falling asleep directly after meals with worsening itching. High carb meals in a patient with insulin resistance can cause fatigue, but rarely this degree of severity. In my experience, mold is the primary reason that a patient would experience this degree of immune reactivity and sensitivity to food.
- He worsened after moving to his current home. This is a big red flag for environmental exposure, especially mold. Other environmental exposures to consider are radon exposure and carbon monoxide poisoning.
- Other signs pointing to mold are
- Asthma in an adult
- Chronic, recurrent sinus infections
- After our first visit, James began to address his home.
- “Remediation company coming tomorrow.” He found another place to stay and is planning to move out of his current home immediately.
- Differential Dx
- Highly suspect mold exposure, MCAS
- Secondary issues
- Likely multitype dysbiosis (bacterial, mold, yeast)
- Nutrient, protein, and calorie insufficiency
- Rule out heavy metal toxicity in the initial work up.
- Clinical Decision Making
- The first priority in treating mold is to get out of the problematic environment. James is already convinced of the need to do this so we are able to move on to confirm the diagnosis of mold with a mycotoxin test, rule out heavy metals, and start shoring up his gut health.
- As he was being made symptomatic with his current restrictive diet, clearly this was not a helpful strategy. I loosened his diet to a general paleo diet while avoiding any foods that made him feel worse.
- Probiotics will start to help repair the gut, combat dysbiosis, and act as binders. Also helpful for anxiety and depression.
- 2-4 day trial of Elemental Diet Reset. This is frequently helpful in severe MCAS. Ongoing Elemental Diet will help support nutrition as we help James heal.
- Recommended Testing
- CBC, CMP, B12, TSH, FT3, FT4, ferritin, iron panel, vitamin D, ANA, heavy metal panel
- RealTime Laboratories Mycotoxin testing
- Doctors Data Random Heavy Metal Urinary Testing
- Initial Treatment Recommendations
- Diet and Lifestyle
- Paleo Diet
- 2-4 day trial of an Elemental Diet then use as needed for nutritional support
- Supplements
- Lacto-Bifido Probiotic Blend, ¼ tsp, 1-2x per day
- Saccharomyces boulardii, 2 pills, 1-2x per day
- Soil-Based Probiotic, 1-2 pills, 1-2x per day
- Lacto-Bifido Probiotic Blend, ¼ tsp, 1-2x per day
- Follow-up Plan
- 4-6 weeks
- Diet and Lifestyle
- Patient Self-Assessment
- Rates health 50/100, reports overall 50% improvement since our first visit.
- Improved
- Itchy and painful skin
- No asthma
- Same
- Sleeping after meals
- Worse
- Hands and forearm skin swelling, cracking, and itching. (Got better when he stopped taking a mineral supplement.)
- Has moved out of his moldy house: “The best thing we’ve done to help this! Once I slept away from that house I slept the entire night long for the first time in 2 years.”
- James did not start probiotics.
- At the end of the visit, James mentioned that he was extremely depressed and “at the edge of commiting suicide.”
- Unfortunately, psychiatric symptoms are very common with mold toxicity, and can be the most distressing symptom present. In this case, happily, James did not have a plan, had not resumed drinking, and was happy to schedule with a counselor and psychiatrist to see alongside our work. He ended the visit encouraged at the prospect of getting better.
- Other updates:
- Itchy painful skin initially helped with 5-day Prednisone, but 10 days later was worse than ever.
- Restarted Dulera.
- Began 1 tab of Cetirizine HCL at night for sinus problems – very little trouble since then.
- Lab Results
- April 2021 Blood Chemistry:
- CBC, no anemia
- CMP – ASL, ALT within normal limits
- D=28
- Iron 128, F=60, B12=637
- April 2021 RealTime Labs Mycotoxin Mold Test:
- Ochratoxin 1.64, Aflatoxin 5.72, Trichothecene 0.09, Gliotoxin 0.02, Zearalenone 1.34
- April 2021 Blood Chemistry:
- Lab Interpretation and Diagnosis
- Normal blood work. He did not complete the heavy metal blood panel or urine test.
- RealTime Laboratory Mycotoxin test confirms mold toxicity.
- Clinical Decision Making
- James’ response to a new environment is an excellent sign, and perhaps will be the key factor in his recovery. His improvement increased his trust in me so that he felt comfortable sharing the depth of his depression, which should mean that he gets the mental health care he needs. I hope that this story helps give you the confidence to make the very hard recommendation of asking a patient to move. It might save their life.
- His positive response to Cetirizine fits with a diagnosis of MCAS, and makes additional therapy here more likely to help.
- I asked James to first restart probiotics and then add in additional MCAS support.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue Paleo Diet with the Elemental Diet as needed
- Supplements
- Start probiotics
- MCAS support
- Continue Cetirizine
- Start an H2 blocker (pepcid, tagamet, or zantac)
- Resveratrol : 1-2 caps 30 min prior to eating
- AllQlear: 1-3 tablets 30 min prior to eating
- (optional) Vitamin D with K: 2 drops, 1-2x per day
- Follow-up Plan
- 4-6 weeks, earlier if needed
- Diet and Lifestyle
- Patient Self-Assessment
- Rates health 60/100, reports overall 80% improvement since our first visit
- James is living out of a brand new RV, on an extended cross country tour with his wife. “This will tell you how much better I’m feeling, I’m following my wife on my motorcycle!”
- No GI symptoms at present.
- “I’m much better mentally. Depression doesn’t stay with me like it used to.”
- However, “My hands still have cracking in them.” Itching continues, preventing sleep.
- Improved
- Bleeding, itchy skin with sharp pains from the bones – completely gone.
- Overactive sinuses – still happens, but not as often.
- Same
- Sleeping after meals
- Sleepless nights
- Depression in mornings (usually after a sleepless night)
- General depression (feels that magnesium citrate powder does help)
- Worse
- Itchy skin
- Dry, cracking skin on hands
- Response to Treatment
- James did not start AllQlear due to worry that he would react to it. Did not try resveratrol or quercetin.
- He did not tolerate either the soil based or lactobacillus blend, so we will simply have him continue on saccharomyces boulardii. He should have no problem adding the former classes of probiotics at a later date when his system is less reactive.
- Visit Recommendations
- I suspect that you have hand eczema. Please make an appointment with a dermatologist to ask if a steroid cream and moisturizer combination can help reduce the cracking in your hands.
- For the itching:
- Please switch to a low histamine diet for 1-2 weeks
- Then add the additional antihistamine supplements listed below
- Follow up 4-5 weeks
- Our next step will be to add binders to lower the amount of mold toxins in your system.
- Clinical Comments
- When you don’t hear from a very ill patient in 6 months, you’ve usually done a good job!
- In James’ case, despite minimal therapies and not yet starting binders or antifungal agents, he is back to enjoying a vibrant life. His depression is not gone, but is more manageable and he is not suicidal. Following the move out of his home, we are in a position to help him heal in a way that was not previously possible.
- James should get some improvement through the addition of conventional therapies for hand eczema, which is a very difficult and stubborn form of eczema.
- Given his ongoing reactivity, we’ll trial a low histamine diet and additional mast cell/histamine support prior to starting binders. If the diet is helpful, he will continue this for a time – if not, then he will simply move back to a paleo diet.
- When you don’t hear from a very ill patient in 6 months, you’ve usually done a good job!
- Updated Treatment Recommendations
- Diet and Lifestyle
- Low histamine diet
- GI
- Magnesium Citrate Powder
- Saccharomyces boulardii
- Magnesium Citrate Powder
- New Supplements
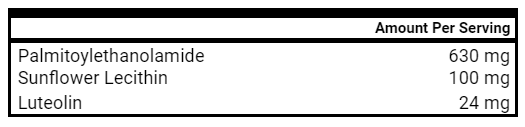
- PEA
- Perilla Seed Extract
- PEA
- Medication
- H2 Blocker – Pepcid or Tagamet
- Cetirizine – 1 tablet twice daily
- Follow-up Plan
- Follow up in 4-5 weeks, to add binders
- Diet and Lifestyle
Clinical Rule and Final Clinician Comments
Clinician’s Comments:
It is very difficult to ask a patient to move. I wanted to highlight another case study in which a patient dramatically improved upon leaving a problematic environment to help you understand the importance of this initial step in treating mold toxicity, and to give you the confidence to make this recommendation.
Patients who do not change their environment are typically stuck “treading water” on a rotating mix of binders, herbal treatments, strict diets, and MCAS support with little improvement to show for their massive effort. We want to help our patients skip mold purgatory and skip right to feeling better. Patients that move see improvements in their symptoms quickly, typically within a few days.
The cure for poisoning is to stop being poisoned. A reduction in ongoing toxin exposure (mycotoxins, VOCs, mold, and associated bacteria) is often sufficient for the body to begin healing and feeling better without massive effort or expense.
Ask your mold toxic patient to spend 1-2 weeks in a new environment. This cost of simply renting an Airbnb or staying in a clean hotel for a week is comparable to many professional inspections, and unfortunately, many inspections often end with more questions than answers. If there is a problem in their environment, then they will feel better after a short time away, and will worsen as soon as they return to their home.
Clinical Rule: In mold toxicity, prioritize getting your patient out of mold.
Research Question
- What has the best evidence in reducing postmenopausal symptoms: Chaste Tree, Dong Quai, or Black Cohosh?
- It is important to note that the placebo effect is large in menopausal symptoms, and many symptoms will reduce over time. As one review makes clear:
- “It has been shown repeatedly that placebo relieves up to 50% of hot flashes within 3 months compared with approximately 80–90% relief achieved with oral estrogen. Furthermore, in 20–40% of patients, hot flashes frequency may decrease in 3 months without any treatment.”
- It is important to note that the placebo effect is large in menopausal symptoms, and many symptoms will reduce over time. As one review makes clear:
Chaste Tree/Vitex:
- Chaste Tree has the largest amount of evidence supporting its use: two reviews [1, 2], one randomized placebo controlled double blinded study, and two placebo controlled clinical trials [3, 4] of blends that primarily featured vitex.
- From the narrative review:
- “The result of the present study showed that this valuable plant is helpful in alleviation of pain resulting from postmenstrual disease [2].
- However, in one randomized trial, Vitex combined with St. John’s wort was not found to be superior to placebo for the treatment of menopausal symptoms.
Main Results:
- In the clinical trial, 52 menopausal women were randomized to Vitex or placebo, and after 8 weeks, the Vitex groups had reduced total menopausal score, vasomotor symptoms, and anxiety. There were no differences in depression or sexual dysfunction.
Dong Quai:
- Dong Quai performed the weakest of the three herbs. There is no compelling evidence supporting the use of Dong Quai, especially as a monotherapy.
Main Results:
- There lacks sufficient evidence to use black cohosh and dong quai as monotherapy.
Evidence:
- Two clinical trials have demonstrated no effect.
- In the first, 100 menopausal women were randomized to a Dong Quai blend or placebo. After 6 months, there were no differences in vasomotor symptoms.
- In the second, 71 postmenopausal women were randomized to Dong Quai or placebo for 6 months.
- “Used alone, dong quai does not produce estrogen-like responses in endometrial thickness or in vaginal maturation and was no more helpful than placebo in relieving menopausal symptoms.”
Black Cohosh:
- Black Cohosh has perhaps been the widest studied, with compelling evidence for and against its use.
Refuting Evidence
- A Cochrane review of 16 RCTs was completed reviewing 2,027 peri- and post- menopausal women where black cohosh used as monotherapy at 40 mg for an average 23 weeks. In this review there was no significant difference between black cohosh and placebo in the frequency of hot flashes or in menopausal symptoms score [5].
- Similarly, a study of 89 post-menopausal women showed that the women randomized to black cohosh had less reduction in vasomotor symptoms compared to placebo [6].
Supporting Evidence
- In a review of alternate therapies used in menopause the authors have this to say of black cohosh
- “A meta-analysis of several short-term and relatively small RCTs comparing black cohosh use with placebo ‘revealed a trend towards reducing vasomotor symptoms’, but only in cases of mild to moderate symptoms. This was particularly notable when hot flushes were associated with sleep and mood disturbances.” [7]
- In one of these studies, 122 menopausal women were randomized to black cohosh or placebo and after 12 weeks, a greater reduction in menopausal symptoms was found in women with a high initial symptoms [8]. In a similar study, 304 women were randomized to black cohosh or placebo. The treatment group showed reduced vasomotor symptoms with a moderate effect size [9].
- In one notable study, breast cancer survivors on tamoxifen who suffered from hot flashes were put on Black Cohosh or placebo for 12 months [10].
- “Almost half of the patients of the intervention group were free of hot flushes, while severe hot flushes were reported by 24.4% of patients of the intervention group and 73.9% of the usual-care group (P<0.01).”
Combination Therapy
One study was performed to evaluate the role of combining herbal treatments [11].
- 50 healthy pre and postmenopausal women were randomized to placebo or combo treatment (black cohosh, dong quai, milk thistle, red clover, American ginseng, chaste-tree berry) for 3 months.
- After 3 months, 73% decrease in hot flushes, 69% reduction of night sweats, and improvement in sleep quality.
- Hot flushes ceased completely in 47% of women in the intervention group compared with only 19% in the placebo group.
Main Results:
- Vitex has the most evidence supporting its use.
- There is no support for the use of Dong Quai as monotherapy.
- Black Cohosh compelling evidence for and against its use.
- In all of the studies reviewed the herbs were shown to be safe.
- Combination therapy using multiple herbal ingredients in a blend may be most effective. This matches with our clinical experience at the RIFM.
Distribution and relevance of Dientamoeba fragilis and Blastocystis species in gastroenteritis: results from a case-control study
Study Purpose
- The actual role of Dientamoeba fragilis and Blastocystis in patients with gastrointestinal symptoms is still under debate.
Intervention:
- A multicenter case-control study was performed in the Netherlands to elucidate the clinical relevance of molecular diagnostics results in gastroenteritis (GE). In the present study, a real-time PCR for Blastocystis was performed on 1374 case samples and 1026 control samples.
Main Results:
- A negative relation between D. fragilis-positive cases and diarrhea was found in this study population, as the prevalence of both D. fragilis and Blastocystis were lower in cases with GE symptoms than in controls.
- A significantly lower overall detection of D. fragilis and Blastocystis was found in cases of GE (both 25.8%) as compared to controls (37.6% and 40.0%, respectively).
- The difference for D. fragilis was statistically significant for subjects above 20 years of age. For Blastocystis, the difference was statistically significant in all age groups, except in children less than 5 years of age.
- More GE symptoms were reported in cases without D. fragilis or Blastocystis. No association could be established between any of the individual symptoms and the presence of D. fragilis or Blastocystis.
Author’s Conclusion:
- This study suggests that the presence of these protozoans may be considered characteristic of a healthy intestinal microbiome.
Study Purpose
- To clarify the evaluation of Iron Deficiency Anemia (IDA), given significant practice variation.
Methodology:
- Recommendations were from a panel primarily composed of gastroenterologists (which could have biased the interventions towards use of procedures).
Main Recommendation:
- Increase the ferritin cut off for the diagnosis of IDA from 15 to 45.
- In the Sept 2019 FFMR we suggested a cut off of 30.
- Based on a review of over 220 systematic reviews and meta-analyses, this change increases the sensitivity of a diagnosis of IDA from 0.6 to 0.85, while only decreasing the sensitivity from 0.99 to 0.92.
Secondary Recommendations:
- The panel highly recommends that a diagnosis of IDA in men and postmenopausal women should initiate an upper endoscopy and colonoscopy given the relatively high incidence of cancer in these groups.
- 16 studies of men and postmenopausal women with IDA found that the overall lower GI tract malignancy rate was 8.9% and the upper GI malignancy rate was 2%.
- The panel suggests that a diagnosis of IDA in premenopausal women should lead to upper endoscopy and colonoscopy compared to iron replacement only.
- Premenopausal women were more likely to have IDA attributed to menorrhagia rather than cancer.
- In premenopausal women, 9 studies found that the incidence of lower GI malignancy was 0.9%, and the upper GI malignancy rate 0.1%.
- A diagnosis of IDA should also prompt consideration of Celiac Disease as well as testing for H. pylori.
- The panel advised against routine endoscopy biopsies for the diagnosis of autoimmune gastritis due to a lack of literature supporting this practice.
Benefits of Increased Screening:
- In men and postmenopausal women, the number of missed colon cancers would decrease from 128 to 47 per 1 million patients. The number of gastroesophageal cancers in this cohort would drop from 32 to 12 per 1 million patients.
- In premenopausal women, the number of missed colon cancers would decrease from 298 to 109 per 1 million patients. The number of gastroesophageal cancers in this cohort would drop from 66 to 24 per 1 million patients.
Harms of Increased Screening:
- With increased bidirectional endoscopies, the false positive rate of cancer would increase from 82 to 655 per 1 million in men and postmenopausal women, and increase the number of perforations from 0.08 to 0.62 per 1 million.
- For premenopausal women, the false positive rate of cancer would increase from 329 to 2632 per 1 million, and the number of perforations from 0.31 to 2.48 per 1 million.
Author’s Conclusion:
- The main benefit of increased screening is the increased detection of malignancies, balanced against the risk of unnecessary procedures, perforations, and false positive diagnoses.
Clinician Takeaways
- Diagnose IDA with a ferritin less than 45, and recommend endoscopy and colonoscopy in men and postmenopausal women with IDA.
Proton Pump Inhibitors Do Not Reduce the Risk of Esophageal Adenocarcinoma in Patients with Barrett’s Esophagus: A Systematic Review and Meta-Analysis
- PPIs are widely used for the treatment of Barrett’s esophagus, but it is not known how effective this strategy is at reducing the progression of Barrett’s to adenocarcinoma. Nine observational studies, comprising five cohort and four case-control studies (including a total of 5712 patients with BE), were identified.
- “No dysplasia- or cancer-protective effects of PPIs usage in patients with BE were identified by our analysis.”
- Comment: The risk of progression of Barrett’s to cancer is very low – about 0.1% each year, so the usual recommendation to add PPI therapy would result in very few cases of cancer prevention unless the magnitude of effect was extremely strong. This review shows this not to be the case.
Highly bioavailable curcumin derivative ameliorates Crohn’s disease symptoms: A randomized, double-blind, multicenter study
- This randomized, double-blinded study was performed at 5 independent medical centers in Japan. Theracurmin (360 mg/day, n=20) or placebo (n=10) was administered to patients with active mild-to-moderate Crohn’s disease for 12 weeks. Efficacy was assessed by evaluating clinical and endoscopic remission, healing of anal lesions, and blood levels of inflammatory markers.
- In the Theracurmin group, a significant reduction in clinical disease activity was observed in week 12 relative to that in week 0 (P=0.005).
- On intention-to-treat analysis, clinical remission rates were 35%, 40%, and 40% at weeks 4, 8, and 12, respectively, which were significantly higher than those in the placebo group (all 0%; P=0.033, P=0.020, and P=0.020, respectively).
- Reduction in endoscopic Crohn’s disease severity (P=0.032) was observed at week 12 in the Theracurmin group.
- The endoscopic remission rates were 15% and 0% in the Theracurmin® and placebo groups, respectively.
- Significant healing of anal lesions (P=0.017) was observed at week 8 in the Theracurmin group.
Clinical efficacy of Saccharomyces boulardii or metronidazole in symptomatic children with Blastocystis hominis infection
- This randomized single-blinded clinical trial included children presenting with gastrointestinal symptoms (abdominal pain, diarrhea, nausea-vomiting, flatulence) more than 2 weeks and confirmed B. hominis by stool examination (B. hominis cysts in the stool with microscopic examination of the fresh stool).
- Randomization was performed by alternating inclusion:
- Group A: S. boulardii (250 mg twice a day) for 10 days
- Group B: metronidazole (30 mg/kg twice daily) for 10 days
- Group C: no treatment
- At the end of the first month after inclusion:
- Clinical cure rate was 94.4% in group A and 73.3% in group B (p = 0.11).
- Parasitological cure rate for B. hominis was very comparable between both groups, 94.4% in group A vs. 93.3% in group B. ( p = 0.43).
Association between sauna bathing and fatal cardiovascular and all-cause mortality events
- Prospective cohort study of 2315 middle-aged (42-60 years) men from Eastern Finland. Study participants were followed who reported having a sauna bathing session 1 time per week, 2 to 3 times per week, and 4 to 7 times per week, respectively.
- After adjustment for risk factors, men with 2-3 sauna bathing sessions per week had a hazard ratio of sudden cardiac death (SCD) was 0.78 compared to men who only bathed once a week. The hazard ratio of men with 4-7 sauna bathing sessions per week was 0.37 (p for trend = .005).
- Increased frequency of sauna bathing is associated with a reduced risk of SCD, CHD, CVD, and all-cause mortality (p for trend ≤.005).
- The degree or risk reduction is the greatest when:
- Bathing 4-7 times a week
- For sessions greater than > 19 minutes, compared to <11 minutes
- “The recommended temperature for a sauna is usually 80°C to 100°C at the level of the (bather’s face)”
How to guide patients who are NOT following up on recommendations?
Listener asks:
How to guide patients who are NOT following up on recommendations?
Gently, but firmly address the issue directly. If you ask compassionately, and if you have earned some trust in your initial interactions with the patient, most people will simply tell you directly what the issue is.
It is my experience that this mostly happens when I haven’t done a good job making sure I understand a patient’s expectations and goals for working with me.
Recently, I was frustrated that a patient hadn’t followed through on my initial recommendations to start a Paleo low FODMAP diet, Triple Probiotics, and complete a breath test. The disconnect was that I was trying very hard to resolve her symptoms for good using what I felt was the best treatment, but she had scheduled an appointment with me in order to pursue further treatment with an Elemental Diet, but hadn’t mentioned that in our first two visits. Once we were aligned, I was able to tweak my suggestions to fit in a course of Elemental Diet with the other recommendations.
Schedule time to reflect on every case
As clinicians, our most valuable asset is giving the very best recommendations possible for each individual seeking our care. One of the best ways to make sure you are doing this is to build 5-10 minutes into your schedule following each case for reflection and review, as the period of time when the facts of a case are fresh in your mind is especially valuable.
At the RIFM, we use this time to update our differential diagnosis, the hierarchy or the order of operations that we plan to offer our patient, and individualizing their treatment plan. Since I’ve begun this practice, I frequently find insights come to mind that alter their treatment for the better that would not have otherwise been present if I were simply rushing through their charting.