Patient Summary:
- Overview Context:
- Whitney is a 34 yo female who is seeking guidance with ongoing fatigue, weight gain, and rosacea. She has a history of Graves’ disease and chronic iron deficiency treated with both blood transfusion and IV iron infusions.
- She reports “I have lots of autoimmune symptoms going on and I’d like to calm it down. I would also eventually like to get off the doxycycline that I’ve been prescribed for rosacea.”
Symptoms and Concerns
- Chief Complaints:
- Fatigue
- Weight Gain
- Rosacea
- Occasional headaches
- Thinning hair
- Stomach discomfort (she thinks this is due to doxycycline)
- Onset, Timeline and History:
- 2013 – Diagnosed with Graves’ after the birth of her first child.
- 2016 – 2nd child born, Graves’ flares and iron levels drop. Weight gain begins.
- 2018 – Diagnosed with Hashimoto’s as TPO antibodies become positive.
- 2019 – Begins noticing rash on face.
- August 2020 – Diagnosed with rosacea.
- December 2020 – COVID-19 diagnosis; worsening of symptoms for several months afterwards.
- September 2021 – Symptoms (fatigue, headache, hair loss) alleviated with blood transfusion.
- Sept 2021 – SIBO breath test reveals mild H2 positive SIBO.
- Past 6 months: Despite exercising and a healthy diet, she continues to gain weight.
Past Medical History
- Prior Diagnosis:
- Graves’ disease (2013)
- Hashimoto’s (2018)
- Rosacea (2020)
- Medications:
- Compounded T4/T3 thyroid hormone
- Doxycycline
Prior Testing and Treatment History
- Prior Testing Summary:
- Thyroid blood work (from PCP):
- TSH <0.01 ((0.5-5 mIU/L)
- FT3 4.3 (1.7-3.7 pg/mL)
- FT4 1.04 (0.9-2.3 ng/dL)
- TPO >1000 (<35 IU/mL)
- TRAB 5.2 (<1.75 IU/L)
- TSI 7.91 (<0.1)
- Thyroid blood work (from PCP):
- Previous Diets:
- Gluten free
- Dairy free
- Paleo
Initial Impression
- Clinical Commentary:
- Her labs previously done with her PCP show a suppressed TSH and uncontrolled thyroid autoimmunity.
- Previous TRAB and TSI indicative of Graves’; new positive TPO shows expanding autoimmunity to include Hashimoto’s.
- Recommended Testing
- Complete blood count
- B12
- Anti-parietal cell antibodies (APCA)
- Intrinsic factor antibodies
- Initial Treatment Recommendations
- Diet:
- Maintain current whole foods diet
- Lifestyle:
- Continue walking daily
- Decrease HIIT and replace with resistance training
- Treatment:
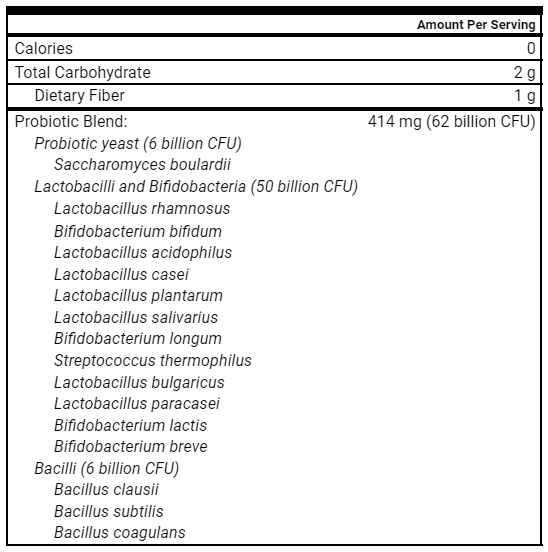
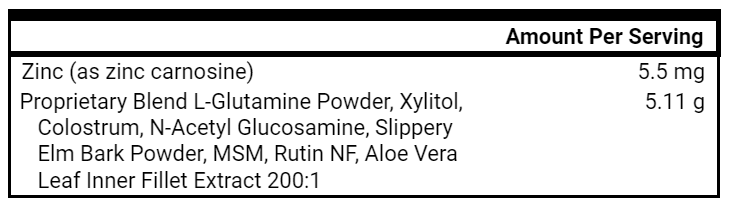
- Lacto-Bifidus, S. Boulardii, Soil-Based Probiotics
- GI Support Nutrients
- Collagen
- B-Complex
- Iron Supplement
- Lacto-Bifidus, S. Boulardii, Soil-Based Probiotics
- Follow-up: 5 weeks
- Diet:
- Clinician Summary
- Given that many cases of rosacea and Hashimoto’s start with GI dysfunction, we are starting with GI-focused therapies.
- Anti-parietal cell antibodies (APCA) were ordered given Whitney’s background of anemia and Hashimoto’s. Both conditions make the presence of autoimmunity against the stomach more likely, as 20% of thyroid autoimmunity patients are positive for APCA.
- If APCA is positive, I will trial HCl earlier in treatment and refer them to a gastroenterologist to discuss endoscopy as a means to screen for atrophic gastritis.
- Intrinsic Factor ordered to rule out pernicious anemia given chronic iron deficiency requiring transfusions, as this was not previously done.
- Subjective Assessment
- Current Symptoms:
- Improved:
- Rosacea
- Completely gone.
- Fatigue
- “Mostly the same… mild”
- Rosacea
- Same:
- Weight gain
- Improved:
- Treatment Response:
- Triple probiotics and GI Supportive Nutrients
- Very helpful, rosacea resolved
- Triple probiotics and GI Supportive Nutrients
- Current Symptoms:
- Lab Results
- Intrinsic factor Abs – 1.0 (range 0 – 1.1)
- APCA – 1.3 (range 0 – 20)
- CBC – normal, negative for anemia
- B12 – 616 (200-1,100 pg/mL)
- Updated Treatment Recommendations
- Note to patient: “I’m so happy that your rosacea is gone. This tells us that we have improved the health of your microbiome and immune system through your program so far. Keep it up!”
- New Treatment Recommendations:
- Start:
- Vitamin D – 2,000 IU QD
- Herbal antimicrobials
- Continue:
- Lacto-Bifidus, S. Boulardii, Soil-Based Probiotics
- GI Support Nutrients
- Collagen
- B-Complex
- Iron supplement
- Stop:
- Doxycycline
- If you flare, then start the herbal antimicrobials recommended.
- Doxycycline
- Labs
- Thyroid Panel: TSH, fT4, fT3, TPO
- Start:
- Follow-up: 5 weeks
- Subjective Assessment
- 95/100, 20% better from last.
- “Stopped doxycycline!!!!!!!!! Lost 10lbs!!!!!!”
- Weaned doxycycline and did not need herbal antimicrobials
- Current Symptoms:
- Improved:
- Weight
- Lost 10 pounds
- Fatigue
- Resolved (had additional iron infusion)
- Rosacea
- Still gone
- Weight
- Same:
- NA
- Worse:
- Reports mucus in stools 4x/week since January 2022
- Improved:
- Current Symptoms:
- Labs:
- TSH 0.84 (0.5-5 mIU/L)
- FT3 2.8 (1.7-3.7 pg/mL)
- FT4 0.9 (0.9-2.3 ng/dL)
- TRAB 2.2 (<1.75 IU/L)
- TPO >1000 (<35 IU/mL)
- TSI 3.96 (<0.1)
- CBC 13.3/38.0
- Ferritin 28 (12-150 ng/mL)
- Iron 27 (30-170 µg/dL)
- B12 925 (130-700 ng/L)
- Interpretation of labs:
- TSH is no longer suppressed. TRAB and TSI antibodies trending down from February, indicating improved autoimmunity. No change in TPO antibodies. Ferritin is increasing for the first time without infusions. I suspect less blood loss. B12 levels have also increased.
- Impression:
- Despite many symptoms improved or resolved, worsening mucus in the stool suggests 1) we have missed a gastrointestinal pathogen or 2) she has subclinical IBD that has contributed to her symptoms.
- Updated Treatment Recommendations
- New Treatment Recommendations:
- Start:
- Curcumin BID
- Double Lacto-Bifidus, S. Boulardii, Soil-Based Probiotics
- Double GI Support Nutrients
- Continue:
- Vitamin D – 2,000 IU QD
- Collagen
- B-Complex
- Iron Supplement
- Labs
- GI 360 Stool Test
- Start:
- Followup: 3-4 weeks
- New Treatment Recommendations:
- Treatment Rationale:
-
- We are increasing her dose of probiotics and GI Support Nutrients, and adding in curcumin in order to heal her gut lining and reduce inflammation. Curcumin has been found to significantly improve IBD and lead to increased rates of clinical and endoscopic remission compared to placebo. We are recommending the GI 360 stool test to assess for pathogens and elevated calprotectin.
- We are increasing her dose of probiotics and GI Support Nutrients, and adding in curcumin in order to heal her gut lining and reduce inflammation. Curcumin has been found to significantly improve IBD and lead to increased rates of clinical and endoscopic remission compared to placebo. We are recommending the GI 360 stool test to assess for pathogens and elevated calprotectin.
-
- Subjective Assessment
- 90/100
- No mucus since last visit
- Current Symptoms:
- Improved:
- Mucus in stool
- Gone
- Weight
- Stable
- Fatigue
- Stable
- Rosacea
- Still gone
- Mucus in stool
- Same:
- NA
- Worse:
- NA
- Improved:
- Lab Results
- GI 360 Stool Test
- Dysbiosis Index 3 (1-5, 5 most dysbiosis)
- Yeast Moderate
- H pylori – Negative
- Blood – Present
- Calprotectin 18 (≤80 ug/g)
- GI 360 Stool Test
- Lab Interpretation and Diagnosis
- Bacterial and yeast dysbiosis present
- No pathogens present
- Calprotectin levels normal
- Blood in the stool
- Impression:
- Whitney is making progress and has responded well to higher dose GI Supportive Nutrients and curcumin. Her stool test confirms bacterial and yeast dysbiosis.
- Updated Treatment Recommendations
-
- New Treatment Recommendations:
- Start:
- Immunoglobulins
- If you find improvement in stools, continue for 3 months.
- If you do not notice a change in stools after 1 month, discontinue.
- Immunoglobulins
- Continue:
- Curcumin BID
- Double Lacto-Bifidus, S. Boulardii, Soil-Based Probiotics
- Double GI Support Nutrients
- Vitamin D – 2,000 IU QD
- Collagen
- B-Complex
- Iron Supplement
- Labs
- None
- Start:
- Followup: 5 weeks
- New Treatment Recommendations:
-
Final thoughts
- Highlighted Clinical Rules
- Consider pushing further into therapies that have a clear positive signal as compared to adding new therapies (e.g. doubling dose of probiotics before adding antimicrobials).
- We had a very clear signal of benefit from probiotics and GI Repair Nutrients in improving her rosacea and autoimmune markers. Knowing these worked well, we doubled the dose and got the clinical result needed, and Whitney did not need herbal antimicrobials.
- Further dietary restriction may not be necessary in someone with an already restricted diet and/or fear around food. Correcting gut imbalances can often improve food sensitivities.
- Whitney was already on a healthy diet, and we did not need to further restrict her diet in order to improve her symptoms.
- Consider pushing further into therapies that have a clear positive signal as compared to adding new therapies (e.g. doubling dose of probiotics before adding antimicrobials).
- Clinical Commentary
- Whitney’s case is a beautiful example of healing a skin condition, like rosacea, with gut-targeted therapies. I believe she had subclinical IBD accounting for chronic blood loss, and that GI-focused treatment helped put this in remission, accounting for the normal calprotectin on her stool test. Her case is a helpful reminder to follow symptoms and be diligent in always asking for updates. If I had not asked about her stool quality at a follow up visit, she may not have volunteered the information on mucousy stools.
- Whitney’s case is a beautiful example of healing a skin condition, like rosacea, with gut-targeted therapies. I believe she had subclinical IBD accounting for chronic blood loss, and that GI-focused treatment helped put this in remission, accounting for the normal calprotectin on her stool test. Her case is a helpful reminder to follow symptoms and be diligent in always asking for updates. If I had not asked about her stool quality at a follow up visit, she may not have volunteered the information on mucousy stools.
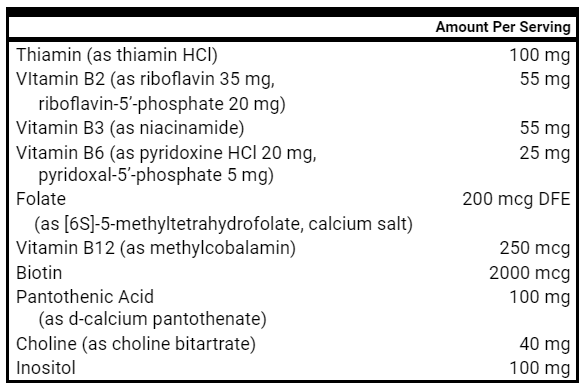
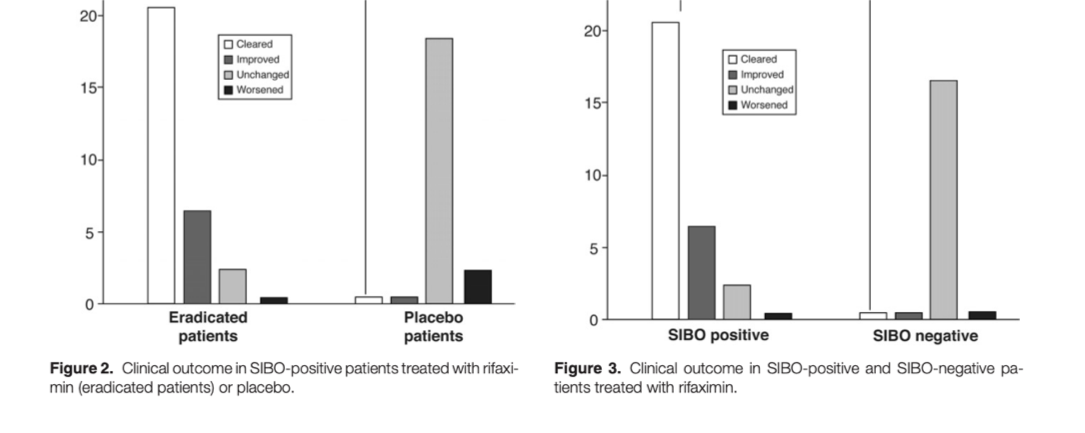
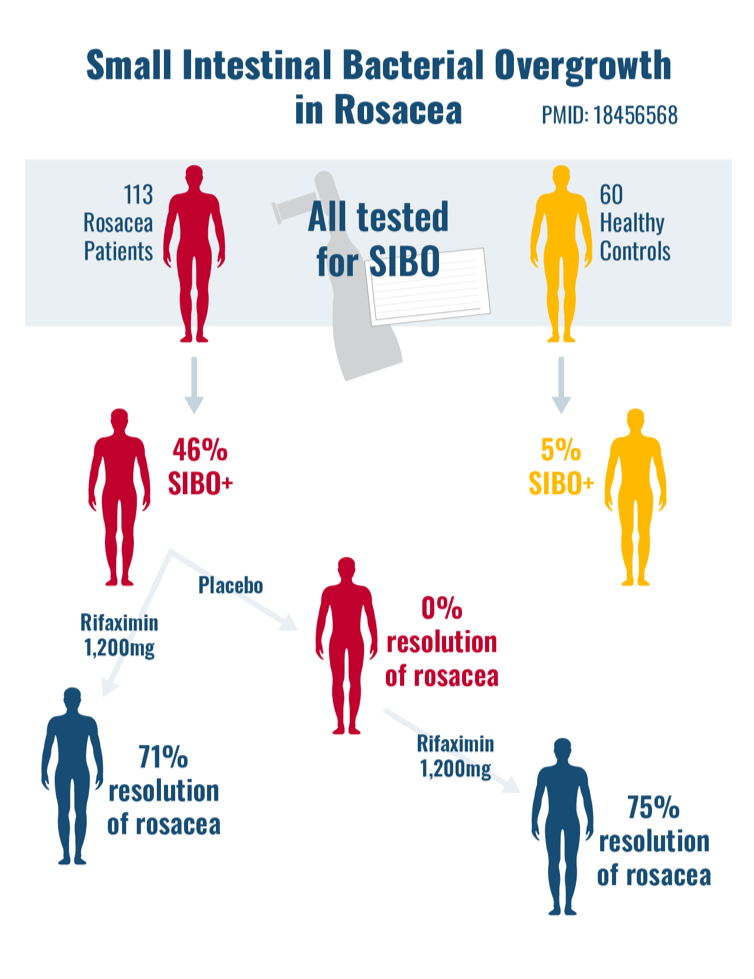
Study Purpose
- To study the prevalence of SIBO in patients with rosacea
Intervention
- 113 rosacea patients and 60 healthy controls all underwent lactulose and glucose SIBO breath testing.
- Rosacea patients who were SIBO positive and SIBO negative were randomized to either:
- Placebo, or
- Rifaximin (1,200 mg/day) x 10 days
Results
- Compared to healthy controls, SIBO was more prevalent in rosacea patients (46% vs 5%).
- Treatment with rifaximin led to an 86.5% eradication rate of SIBO.
- In rosacea patients with a positive SIBO breath test, rifaximin led to resolution of rosacea in 71% vs 0% in the placebo group.
- Patients in the placebo group were then treated with rifaximin, which led to a resolution of rosacea in 75%.
- In rosacea patients with a negative SIBO breath test, rifaximin led to NO resolution of rosacea.
- After 9 months of follow up, only 2 patients had a relapse of rosacea. They retested positive for SIBO, and upon eradication with rifaximin, rosacea cleared up again.
Author’s Conclusion
- “This study demonstrates that rosacea patients have a significantly higher SIBO prevalence than controls, and, more importantly, that the eradication of SIBO induces an almost complete regression of the cutaneous lesions in rosacea patients and maintains this excellent result for at least 9 months.”
Clinical Takeaway
- This study really ties in nicely with this month’s case study, as it highlights the important connection between gut health and rosacea.
- While this study used rifaximin for its intervention, at the RIFM, we observe similar results with herbal antimicrobials, or probiotics as seen above.
High-dose oral thiamine versus placebo for chronic fatigue in
patients with quiescent inflammatory bowel disease
Study Purpose
- To investigate the effect and safety of high-dose oral thiamine (600-1800 mg/d) on chronic fatigue in patients with quiescent IBD
Methods
- 40 IBD patients were randomized to:
- Group 1: High dose thiamine x 4 weeks, washout x 4 weeks, placebo x 4 weeks
- Group 2: Placebo x 4 weeks, washout x 4 weeks, high dose thiamine x 4 weeks
Results
- Compared to placebo, thiamine led to:
- Improvement in fatigue scores(- 4.5 points thiamine vs + 0.75 points placebo)
- Greater number of participants with improved fatigue (65% vs 30%)
- Mild side effects were detected with thiamine treatment, including:
- Headache (n = 2)
- Nausea (n = 1)
- Heartburn (n = 1)
- Oral blisters (n = 1)
- Sleeplessness (n = 1)
Author’s Conclusion
- High-dose oral thiamine led to significant improvements in fatigue in IBD patients.
Clinical Takeaway
- At the RIFM, we have been using high-dose oral thiamine for patients with post-exertional malaise with good success.
Dose–response relationship between protein intake and muscle mass increase: a systematic review and meta-analysis of randomized controlled trials
Study Questions:
- 1) Is there a dose-dependent response to increased protein intake and lean body mass?
- 2) Does increasing protein intake without resistance training lead to increased lean body mass?
Conversion of kg to lb:
- 0.5g / kg = 0.2 g/lb
- 1.3 g / kg = 0.6 g / lb
- 2.2 g / kg = 1 g/ lb
- 3.5 g / kg = 1.6 g / lb
Methods
- In 105 studies, 5,402 participants were given supplemental protein for at least 2 weeks and assessed for changes in lean body mass (LBM)
- “The hypothesis in this study was that increased protein intake would result in an increase in muscle mass in a dose-dependent manner and that ingestion of small amounts of protein, especially among a resistance-trained population, would be effective in increasing muscle mass”
Results
- Protein supplementation was effective for increasing LBM with or without resistance training.
- “Dose–response analyses indicated that total protein intake over a wide range of doses (from 0.5 to 3.5 g/kg/d) was positively correlated with an increase in LBM”.
- LBM increased by 0.39 kg for every 0.1 g/kg/d increase in total protein intake, until 1.3 g/kg/d was achieved
- For every 0.1 g/kg/d increase of total protein intake above 1.3 g/kg/d, LBM increased by only 0.12 kg
- “The rate of increase in the effect of protein supplementation rapidly diminished after 1.3 g/kg/d was exceeded, and resistance training markedly suppressed this decline.”
- In other words, consuming protein up to 1.3 g/kg/d, or 0.6 g/lb/d, was able to increase lean body mass even without resistance training.
- However, once an individual exceeds 0.6 g/lb/d, increase in LBM slows down, unless they add in resistance training.
Authors’ Conclusions
- “These findings suggest that slightly increasing current protein intake for several months by 0.1 g/kg/d in a dose-dependent manner over a range of doses from 0.5 to 3.5 g/kg/d may increase or maintain lean body mass. The effect of protein intake on LBM diminishes after the intake of 1.3 g/kg BW/d is exceeded, and resistance training markedly suppresses this decline.”
- “Therefore, both increasing protein intake and performing resistance training is recommended to optimally improve LBM.”
Clinical Takeaway
- At the RIFM we have been observing improvements in fatigue, energy, skin health and resolution of chronic GI symptoms by asking some patients to achieve a high protein intake of 1g / lb of ideal body weight. This review suggests that there are diminishing returns in LBM at increased protein above 0.6 g/lb/d, and that resistance training should be implemented in concert with doses above 0.6 g / lb to optimize LBM.
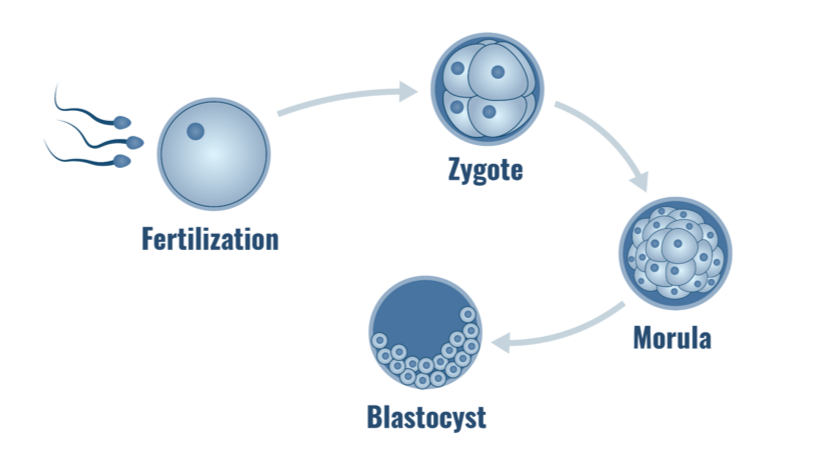
Does changing a patient’s dietary consumption of proteins and carbohydrates impact blastocyst development and clinical pregnancy rates from one cycle to the next?
https://doi.org/10.1016/j.fertnstert.2012.07.167
Introduction
- Occasionally, healthy young women undergoing infertility treatment with in-vitro fertilization (IVF) don’t have successful pregnancies because of poor blastocyst development. The objective of this study was to see if a change in patient dietary habits will impact blastocyst development and implantation, and thus, pregnancy outcomes.
Methods
- 12 women, < 35 years of age with poor blastocyst formation and a failed first IVF cycle.
- Patients were counseled on how to increase their protein intake and reduce their carbohydrate intake for 2 months prior to their next IVF cycle.
- The number of oocytes retrieved and fertilized, and blastocyst development, were compared between IVF cycles.
Results
- The average increase in protein in their diets was 16.4%, and the average carbohydrate decrease was 22.3%.
- Blastocyst formation increased significantly from 18.9% to 45.3%.
- The clinical pregnancy rate increased from 16.6% (2/12 women) to 83% (10/12 women)
Author’s Conclusion
- Young healthy women with failed IVF and poor embryo development can possibly improve pregnancy rates by increasing protein and lowering carbohydrates for 2 months prior to their IVF cycle.
Clinical Takeaway
- This study highlights the importance of optimizing one’s diet by increasing protein intake and lowering carbohydrates to improve pregnancy rates. It’s possible that by increasing protein and lowering carbohydrates, they also improved dietary quality, as high carb foods are typically processed and many high protein foods are typically healthier. Either way, just like many health conditions, this study demonstrates that focusing on nutrition is foundational to improving one’s health.
What should one do when probiotics seem to make things worse in an IBS patient?
Listener asks:
What should one do when probiotics seem to make things worse in an IBS patient? Namely, a low dose seems to do nothing, when trying to reach the dose suggested by the manufacturer, abdominal symptoms worsen and new ones appear (loud intestinal noises, runny stools). Does it mean probiotics won’t work at all? Should you go on taking them anyway?
Probiotics have been shown in numerous studies to improve GI symptoms and quality of life in patients with IBS. In this case, I would begin by problem solving with this patient because the chances are high that probiotics will be beneficial. Here are a few scenarios which may apply to this case:
- Your patient needs a slow titration on probiotics due to a large amount of dysbiosis.
- Your patient is experiencing symptoms that are not related to the probiotic. For example, this type of response to probiotics can be seen when a patient is following an inappropriate diet or using alcohol excessively.
- Your patient is using a low quality probiotic and may feel better on a different formula.
- Your patient will do fine on the probiotics following a dietary shift (e.g. basic elimination diet, or low FODMAP) or a short course of Elemental Heal.
- Your patient has limbic dysfunction, which tends to increase reactivity to many supplements.
However, just because probiotics work in the vast majority of patients with IBS, it doesn’t mean they are a good fit for everyone. If probiotics consistently make your patient worse, then I would recommend moving on to a different treatment.