Patient Info:
- Amy, 43y/o, Female
- Previous Dx:
- Hypothyroid (functional medicine doc)
- 1985 — Hives
- 2000 — Idiopathic thrombocytopenic purpura
- 2015 — Hashimoto’s, hyperthyroidism, “adrenal fatigue”, “leaky gut”
- Rx:
- NP Thyroid (Hashimoto’s/Hypothyroidism)
- Low dose Naltrexone (Hashimoto’s/Hypothyroidism)
- Chief complaints:
- Fatigue, 5-CO
- Insomnia w/ warmth, 4-CO
- Can’t lose extra weight, 4-CO
- Brain fog, 4-IN
- Bloating, 4-OC
- Anxiety, 4-OC
- Other symptoms:
- Pulsing feeling in abdomen (abdominal aortic aneurysm)
Initial Impression
- Amy is a 43 y/o female, on a paleo-like diet, with good demeanor, outlook and lifestyle.
- Dx/Rx:
- Dx: Hypothyroid, hives, idiopathic thrombocytopenic purpura, Hashimoto’s, hyperthyroidism, “adrenal fatigue”, “leaky gut”
- Rx: NP Thyroid (Hashimoto’s/Hypothyroidism), Low Dose Naltrexone (Hashimoto’s/Hypothyroidism)
- Previous Testing:
- CMP, CBC w/ diff – normal
- TPO – 250, low TSH
- Ferritin – 34
- Onset:
- Gradual onset, no known cause
- Family History:
- High blood pressure (parents + sister)
- Type I diabetes (sister)
- AFib (father)
- Prior Treatments:
- Helpful: Paleo and Paleo low FODMAP diets
- Slightly helpful: Herbal antimicrobials, Rifaxamin
- Not helpful: Any thyroid medications, probiotics
- Notes:
- Likely has GI dysbiosis paired with histamine intolerance. Also might be reacting to presumably unneeded thyroid medications.
- Prognosis:
- Good to excellent.
Previous Diets
- Fasting – not helpful
- Autoimmune Paleo Diet – not helpful
- Paleo – helpful
- Paleo low FODMAP – helpful
Dr. R’s Note:
- Are you seeing how this all fits together to support an incorrect hypothyroid diagnosis? Functional med doc made diagnosis (suspicion raised). No family history of hypothyroid (suspicion furthered). No improvement from thyroid Rx but did respond to GI therapies (suspicion extremely high).
Testing
- Tests ordered:
- Will carry over previous bloodwork
- Please send the labs that diagnosed you as hypothyroid
- Optional:
- Aerodiagnostics Lactulose SIBO breath test
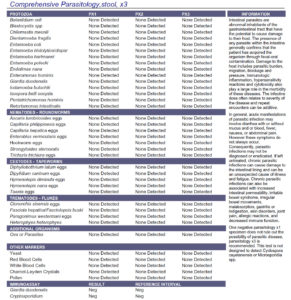
- Doctors Data Para 3 w/ pylori stool test
- Rationale
- Let’s double-check her hypothyroid diagnosis
- And examine her digestive health
Recommendations
- Diet:
- Start on the Paleo low FODMAP Diet.
- After 1 week, perform a 1-week trial also following the Low Histamine diet. Continue to restrict dietary histamine if this helps.
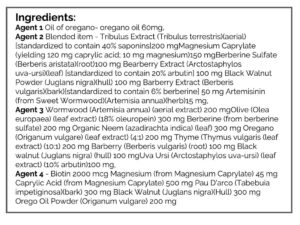
- NRT: Ferrochel, D/K, Multi, EPA/DHA
- GI: Herbal antimicrobial base protocol
- Note: Be on the diet for 2 weeks before adding in the supplements, but continue diet until our follow up. Then, be on the supplements for 3 weeks before following up. Make a note of changes noticed from diet vs. supplements
- Sequence: testing, diet, supplement program, follow up.
- Follow Up: 7 weeks
- Rationale:
- Basic starting point for GI reparative diet, plus trial on low histamine.
- Since probiotics did not yield improvement prior, we will go right to antimicrobial therapy.
Subjective Assessment:
- Stopping thyroid meds (self-selected) – is doing fine
- Paleo low FODMAP diet – is helping GI
- Low histamine – not helpful
- Antimicrobials – might help
- Improved:
- Fatigue, insomnia, brain fog, anxiety, bloating, menstrual pain, weight gain
- Same:
- n/a
- Worse:
- Constipation
Lab Interpretation:
- Stool test: Commensal – 3x overgrown. Otherwise Unremarked
- SIBO breath test: not performed
- Labs originally used to Dx hypothyroid: TSH – 3.5, Free T4 – 1.0 (normal)
- Previous bloodwork:
Impression:
- Paleo low FODMAP and herbal antimicrobials have led to all chief complaints improving today. Not responsive to a low histamine diet. Prior labs show she was not hypothyroid, and currently has mild bacterial dysbiosis. Today will continue with the current plan + add magnesium for a bit of constipation.
- Dr. R’s Note: this is madness
Recommendations
New:
- Can reintroduce a limited amount of desired FODMAP foods
- GI: Magnesium Citrate
- Continue intermittent fasting (she had done a self-elected trial here recently)
Follow up: 3-4 weeks after ending antimicrobials
Subjective Assessment:
- Second month of herbal antimicrobials – helpful, maintained improvement after stopping
- FODMAP reintroduction – went ok, but too much can aggravate symptoms
- Magnesium Citrate – slightly helpful
- Motility Support – very helpful
- Improved:
- Fatigue, insomnia, brain fog, anxiety, bloating, menstrual pain, weight gain, constipation.
- Same:
- n/a
- Worse:
- n/a
Impression:
- Overall Amy is happy with where she is. All chief complaints improved. Motility Support is better than Magnesium Citrate, FODMAP reintroduction went OK. Will maintain the plan, retest thyroid (post-medication withdrawal) and ferritin, then follow up.
- Dr. R’s Note: Yet another case where the thyroid was treated incorrectly.
Tests Ordered:
- Labcorp:
- Ferritin
- TSH, TPO, Free T4
Recommendations:
- New:
- Switch to the Motility Support and discontinue magnesium.
- Retest ferritin and thyroid in Nov, then follow up 2 weeks later.
- Experiment with a minimal dose of probiotics, aim to have one formula in each category as modeled by our Lacto-Bifido Blend, boulardii, and our Soil-based. For extra credit consider a prebiotic.
- Work to expand diet and reintroduce more foods.
- Follow Up: 2 weeks after collecting re-testing.
Subjective Assessment:
- Still feeling well, as per last visit.
- Improved:
- Fatigue, insomnia, brain fog, anxiety, bloating, menstrual pain, weight gain, constipation.
- Same:
- n/a
- Worse:
- n/a
Lab Interpretation:
Impression:
- Still feeling great. Stopped her thyroid hormone in April or May, retested about 6 months later. Thyroid labs show mild subclinical hypothyroid TSH 5.2, T4/3 wnl. Today will continue with dietary expansion and start supplement curtail.
- Dr. R’s Note: Did you know the research shows no benefit in treating subclinical hypothyroid patients with thyroid hormone? And that roughly half of these cases spontaneously correct?
Recommendations:
- New:
- Retest iron in June 2020. If over 100 on ferritin, stop iron supplement.
- Stop multivitamin when the bottle is empty.
- Experiment with Motility Support on/off for minimal effective dose.
- Follow Up: As needed or once yearly.
Dr. Ruscio’s Comments
As I have said numerous times, there are LOTS of cases who are told they are hypothyroid incorrectly while the underlying cause (gut) is overlooked. We can do better! If thyroid symptoms don’t resolve right away from medications, be sure to explore the possibility of gut involvement.
What about her TSH of 5? We already discussed the research here. Also, keep in mind that after 6 months off medication it is unlikely her TSH is still rising post-thyroid medication withdrawal.
American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation.
Am J Gastroenterol. 2014 Aug;109 Suppl 1:S2-26; quiz S27. doi: 10.1038/ajg.2014.187.
Study Purpose:
- Review the evidence on available IBS and constipation treatments.
Intervention:
- Review with practice guidelines.
Main Results:
- This study provides the most up-to-date comparison table for various IBS treatments, including rifaximin versus probiotics.
- Probiotics are more efficacious than rifaximin (caveat, evidence quality for rifaximin is better; moderate versus low).
- NNT: probiotics = 7, rifaximin = 9
- NNT = number needed to treat (how many patients are required to treat for 1 to improve)
- Probiotic adverse events are low 3% (16% on probios minus 13% on placebo = 3%).
- Total adverse events were reported by 24 RCTs containing 2,407 patients. Overall, 201 (16.5 % ) of 1,215 patients allocated to probiotics experienced any adverse event compared with 164 (13.8 % ) of 1,192 assigned to placebo with the NNH of 35 (95 % CI 16 – 362).
- Rifaximin adverse events were not statistically different between antibiotics and placebo.
- Not enough evidence to recommend prebiotics.
Additional Results:
- Fiber outperforms prescription constipation treatments (Resalor aka prucalopride, Linzess aka linaclotide).
Interesting Notes:
- Here is why it’s important to understand levels of evidence: Treatment conclusions based upon low level evidence are likely wrong (and will change).
Clinical Takeaways:
- Probiotics are effective for IBS
- Probiotics may be more effective than rifaximin for IBS
- Adverse events are low for both but might be lower for antibiotics (the difference is not statistically significant)
- Fiber is helpful for constipation
- What to tell your patients:
- Despite what many doctors and blogs report, probiotics are well-studied and helpful for IBS. Probiotics might be more effective than rifaximin.
Dr. Ruscio Comments
Both antibiotics and probiotics have a time and place in the treatment of IBS (and SIBO). However, it is disappointing to see how both natural doctors and conventional doctors are not utilizing probiotics routinely. They each have different reasons and in my opinion, the rationales by both camps are due to bias and are not what the evidence supports.
Gen Psychiatr. 2019 May 17;32(2):e100056. doi: 10.1136/gpsych-2019-100056. eCollection 2019.
Study Purpose
- Review the evidence for treatment of anxiety through modulation of intestinal microbiota
Intervention:
- Systematic review
- A total of 3334 articles were retrieved and 21 studies were included which contained 1503 subjects.
- In the 21 studies, 14 chose probiotics as interventions to regulate intestinal microbiota and six chose non-probiotic ways such as adjusting daily diets
Main Results:
- A variety of different probiotics were used
- Evidenced-limited interpretation
- We can’t recommend probiotics because we don’t know what the best strains to use are. Studies have been inconsistent.
- Evidence-based but NOT evidence-limited interpretation
- Various types of probiotics have all shown benefit for anxiety thus a variety of probiotics can achieve the benefit. There is no one best probiotic here.
- A) single probiotic interventions (four studies), and most of the probiotics were Lactobacillus, (B) two studies used two probiotic mixtures: the Swiss Lactobacillus and the long Bifidobacterium mixture, (C) five studies used at least three probiotic mixtures: Lactobacillus, Streptococcus, Bifidobacterium.
- Evidenced-limited interpretation
- 80% of studies that conducted the non-probiotic interventions were effective
- 45% of studies that used probiotic supplementations were effective
- Microbiota therapies had an efficacy of 86% for anxiety
- six of seven studies showed that regulation of intestinal microbiota could treat anxiety symptoms, the rate of efficacy was 86%.
- In summary, the overall quality of the 21 articles included in this study was high.
- Helpful, but not a cure-all
Additional Results:
- Inflammation may negatively influence the brain.
- The trillions of microorganisms located in the gut are called gut microbiota, and they perform important functions in the immune system and metabolism by providing essential inflammatory mediators, nutrients and vitamins (4). …The long-term existence of this immune activation can make brain functions change which finally lead to the kinds of mental disorders like anxiety disorder (5, 6, 7).
- The gut-brain connection is being validated by clinical research.
- a growing number of basic and clinical studies have shown that intestinal flora can modulate communication between the gut and the brain (9) via the gut-brain axis, which (10) mainly includes the nervous system, immune system and endocrine system. When intestinal flora is affected, a series of changes in physical and/or mental symptoms can occur (11).
- The patient studied were MORE than just IBS patients, thus support the gut-brain connection in a variety of conditions; chronic fatigue, RA, fibromyalgia, obesity, and diabetes.
- A total of 1503 subjects were included in the 21 studies, including patients with IBS (10 studies), healthy controls (six studies) and other patients with chronic diseases such as chronic fatigue syndrome (CFS), rheumatoid arthritis (RA), obesity, fibromyalgia and type 2 diabetes mellitus.
Limitations:
- Data here are considered preliminary. Larger studies are required to reinforce these findings.
Authors Conclusion:
- “We find that more than half of the studies included showed it was positive to treat anxiety symptoms by regulation of intestinal microbiota. There are two kinds of interventions (probiotic and non-probiotic interventions) to regulate intestinal microbiota, and it should be highlighted that the non-probiotic interventions were more effective than the probiotic interventions. More studies are needed to clarify this conclusion since we still cannot run meta-analysis so far.”
Interesting Notes:
- But can’t probiotics cause brain fog, anxiety and depression? Isn’t the low FODMAP diet harmful…. Probably not….
- In short, no matter which intervention was taken, the probability of serious adverse reactions was extremely low, and it is safe to improve the anxiety symptoms by regulating the intestinal flora.
Clinical Takeaways:
- The gut-brain connection can be modulated to improve anxiety via probiotics and dietary changes.
- What to tell your patients:
- The gut-brain connection can be modulated to improve anxiety via probiotics and dietary changes.
Dr. Ruscio Comments
More data pouring in shows how important GI health is…
Clin Transl Gastroenterol. 2018 Jun 19;9(6):162. doi: 10.1038/s41424-018-0030-7.
Study Purpose
- Assess the relationship between SIBO, brain fog, and probiotics.
Intervention:
- “Patients with gas, bloating, BF, intact gut, and negative endoscopic and radiological tests, and those without BF were evaluated.
- SIBO was assessed with glucose breath test (GBT) and duodenal aspiration/culture.
- Metabolic assessments included urinary D-lactic acid and blood L-lactic acid, and ammonia levels.
- Bowel symptoms and gastrointestinal transit were assessed.”
Main Results:
- Dr. R’s Note:
- In accordance with my suspicious, this study has been discredited, see my comments at the end of this summary. This published repudiation of Rao’s hypothesis was very reassuring as I struggled to make sure I was not letting my biased in favor of probiotics taint how I read Rao’s study. It did not seem Rao’s hypothesis was accurate or factually supported (as I’ll share below) but I always remain open to the fact that I could have a bias. Therefore it was very vindicating to see others levying the same criticism.
- Bloating, pain and distention were the most severe symptoms in both the brain fog and non-brain fog groups.
- But all brain fog subjects consumed probiotics.
- Thirty patients with BF and 8 without BF were evaluated. Abdominal bloating, pain, distension and gas were the most severe symptoms and their prevalence was similar between groups. In BF group, all consumed probiotics.
- SIBO was more common in the brain fog group, as was D-lactic acidosis
- SIBO was more prevalent in BF than non-BF group (68 vs. 28%, p = 0.05). D-lactic acidosis was more prevalent in BF compared to non-BF group (77 vs. 25%, p = 0.006).
- Transit was similar between brain fog and non-brain fog groups
- Gastrointestinal transit was slow in 10/30 (33%) patients with BF and 2/8 (25%) without.
- After stopping probiotics and taking antibiotics brain fog and GI symptoms resolved in 77% of cases.
Additional Results:
Limitations:
- There are several here, listed below in my commentary.
Authors Conclusion:
- We describe a syndrome of BF, gas and bloating, possibly related to probiotic use, SIBO, and D-lactic acidosis in a cohort without short bowel. Patients with BF exhibited a higher prevalence of SIBO and D-lactic acidosis. Symptoms improved with antibiotics and stopping probiotics. Clinicians should recognize and treat this condition.
- BF was defined as the presence of two or more of the following symptoms for more than 3 months during their initial clinic visit: mental confusion, cloudiness, impaired judgment, poor short-term memory, and difficulty with concentration.
- The glucose breath test was used
- GBT was considered positive for SIBO if there was ≥20 p.p.m. increase above baseline for H2 or for combined H2 and CH4
Interesting Notes:
- “Brain Fogginess (BF) describes a constellation of symptoms comprised of mental confusion, impaired judgment, poor short-term memory, and difficulty with concentration, which is often transient and disabling. Previously, similar symptoms, along with slurred speech and gait disturbances have been described in patients with short bowel syndrome (2, 3).
- Lactic acidosis assessment
- L-Lactic acid levels ≥2.2 mmol/L were considered positive and indicative of acidosis. Urine samples for D-lactic acid were collected at baseline, 1 h, and 3 h during and after the GBT and analyzed in a specialist lab (Mayo Clinic Laboratories, Rochester, MN).
- 30% of brain fog patients had SIBO (see diagram above) but almost roughly 90% of them had digestive symptoms… What does this tell the astute clinician? Target their symptoms!
- The most common symptoms in the BF group were abdominal pain (96.7%), bloating (93.3%), distention (90%), fullness (90%), gas (90%), cramping (80%), diarrhea (76.7%), and belching (90).
- Here where I feel Rao goes hunting for his own hypothesis, trying to tie the fact that those with chronic digestive symptoms were taking probiotics and therefore the probiotics could be causing the brain fog. Remember only 1/3 of them had SIBO breath test positive (although culture positive was 47%) and far less had the lactic acidosis…
- All patients in the BF group were taking probiotics (range 3 months to 3 years), some were taking 2–3 different varieties containing Lactobacillus species, and/or Bifidobacterium species or Streptococcus thermophilus and others. Additionally, 11 (36.7%) were using cultured yogurt daily, and 2 (6.7%) large amounts (20 oz.) of homemade cultured yogurt daily.
- We have data showing probiotics can treat D-lactic acidosis (1, 2, 3). I feel Rao’s hypothesis reflects an incomplete understanding of the anti-bacterial action of probiotics. Sadly, it seems many conventional gastros (including one’s I respect as Rao) have a bias against probiotics.
Clinical Takeaways:
- Don’t be mislead to catchy media claims, it is unlikely that probiotics were the driver of brain fog here.
- What to tell your patients:
- The claim that probiotics can cause brain fog is speculative and not what the majority of the data support.
Dr. Ruscio Comments
It is incorrect to suggest the probiotics caused the brain fog here. It’s also possible that the probiotic did contribute but say that this study does not support this claim BUT was all over the media suggesting ‘probiotics can cause brain fog’.
Thankfully Rao does mention this HUGE point
Although a meta-analysis of 57 studies indicated that probiotics are safe 22
But does leave out the important mentions that
- Probiotics can treat SIBO (meta-analysis)
- Have been shown to combat D-lactic acidosis
- Preliminary data show probiotics can improve cognition (in healthy and in certain disease states)
The elephant in the room here that the patients who responded were given a personalized antibiotic cocktail for their SIBO.
I appreciate Rao’s investigation of this issue and look forward to further research that better answers this question. Currently, I feel it be a mistake to withhold probiotic treatment in those with brain fog and this is what the totality of the evidence seems to suggest.
A published rebuttal can be found here, with a few quotes below
‘Brain Fogginess’ and D-lactic Acidosis: Probiotics are Not the Cause
In their recent study, Rao and colleagues1 incriminated probiotics in the induction of D-lactic acidosis, thereby causing such symptoms as ‘brain fogginess’, abdominal pain, and bloating. This report has been picked up by dozens of media outlets—from Newsweek to Psychology Today—and has the potential to portray probiotics, products that are safely consumed by millions around the world, in a negative light. Many benefit from probiotics2 and could be frightened—on the basis of this report—into stopping them, with potentially negative impacts on their health. For these reasons, the study deserves careful scrutiny.
The problems with this paper are first signaled by the very title of the piece where the authors conflate two separate entities, probiotics and small intestinal bacterial overgrowth (SIBO), and, in so doing, give the impression that they are equally culpable in the pathogenesis of their patients’ symptoms. No evidence is provided to support this.
The administration of probiotics and synbiotics in immune-compromised adults: Is it safe?
Benef Microbes. 2015 Mar;6(1):3-17. doi: 10.3920/BM2014.0079.
- Summary: no adverse events in immunocompromised individuals taking probiotics, in fact, they had FEWER health complications.
- Analysis of 57 clinical studies indicates that probiotic and/or synbiotic administration in immune-compromised adults is safe with regard to the current evaluated probiotic strains, dosages, and duration.
- Individuals were considered immune-compromised if HIV-infected, critically ill, underwent surgery or had an organ- or an autoimmune disease.
- There were no major safety concerns in the study, as none of the serious adverse events (AE)s were related, or suspected to be related, to the probiotic or synbiotic product and the study products were well tolerated.
- Overall, AEs occurred less frequently in immune-compromised subjects receiving probiotics and/or synbiotics compared to the control group.
- How good are the data showing probiotics are safe? Well, an analysis of 57 clinical trials is a great start. However, there have been criticisms that the quality of these trials could be better so this should be kept in mind.
Effect of probiotics on depressive symptoms: A meta-analysis of human studies.
Psychiatry Res. 2019 Sep 17:112568. doi: 10.1016/j.psychres.2019.112568. [Epub ahead of print]
- In total, 19 double-blind, randomized, placebo-controlled trials with a total of 1901 participants were included in the qualitative synthesis.
- Participants treated with probiotics showed significantly greater improvement in depressive symptoms than those receiving placebo.
- The clinical population was stratified by clinical diagnosis into those with major depressive disorder (MDD) and those with other clinical conditions. The beneficial effect of probiotics on depressive symptoms was significant in patients with MDD, but not in those with other clinical conditions and in the general population.
- In addition, multiple strains of probiotics were more effective in reducing depressive symptoms.
- In conclusion, altering the gut-brain axis with probiotics may be an approach to improve depression severity. It is essential to verify the efficacy of specific combinations or strains of probiotics for depressive symptoms by conducting studies with a larger sample size in the future.