Practitioner Case Study – August 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders
- Neurological Dysfunction in Coeliac Disease and Non-Coeliac Gluten Sensitivity.
- Rapid-fire Research – ultra concise summaries of noteworthy studies
- Urinary Iodine Concentration Is Inversely Associated With Thyroglobulin Antibodies.
- Selenium Supplementation In Patients With Subclinical Hypothyroidism Affected By Autoimmune Thyroiditis: Results Of The SETI Study.
- Epithelial Response To Butyrate Diminished In Active IBD
Practice Tip
![]()
Case Study
Patient Info:
- Abby, 45y/o, female
- Previous Dx
- Subclinical hyperthyroid, then subclinical hypothyroid
- Sarcoidosis
- Rx
- Valtrex EBV
- Chief complaints
- Bloating, 7-CO
- Constipation, 6-CO
- Lower Back/Neck Stiffness & Pain, 6-CO
- Hair Loss/Breakage, 6-CO
- Other symptoms
- Weight Gain, 4-IN
- Fatigue, 4-IN
- Granulomas, due to sarcoidosis
- Tongue scalloping
- Allostatic Load – mild
Visit 1 (day 1) – History and Exam:
Initial impression
- Abby presents as a somewhat healthy 45yo female, with a good diet, lifestyle, and demeanor.
- Dx/Rx:
- Dx: Subclinical hyperthyroid, then subclinical hypothyroid (was told she had “hyper” then “hypo”). Potential EBV.
- Rx: Valtrex EBV
- Previous testing:
- NORMAL: CMP, TSH 1x (2.5), TPO+TG, CBC w/ diff, SIBO Breath Test
- ABNORMAL: L Ferritin (18), ANA, TSH 5.9 then 6.4 (w/ normal fT4), ferritin later normalized (98).
- Onset:
- Gradual onset, potentially caused by hypothyroid, EBV or sarcoidosis. The stress of divorce seems to initiate also. Feels keto caused hyperthyroid, but was on iodine at the same time. Then stopped keto, iodine, and Armour – TSH then normalized up to 6.
- Family history
- ALS
- Prior Treatments:
- Iodine very helpful, as was Valtrex.
- VSL#3 and Armour – NR.
- Keto most helpful but might have caused subclinical hyperthyroid. Paleo also helped.
- Notes/DDX
- Likely need to start with GI therapies while stopping iodine and thyroid supports, then see where thyroid levels out.
- Mega-dose iodine may have confounded the previous trial of Keto. Female hormone support may also be needed. Graves’ antibodies should also be assessed.
- Prognosis
- Good to excellent. Is in fairly good shape now, just needs guidance on finishing touches.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Tests ordered
- LabCorp
- CBC w/ diff, lipid panel, iron panel, Hemoglobin A1c, Vitamin D
- Graves’ antibodies
- Free T4 by Dialysis
- Full GI Panel (including expanded IBD profile)
- Anti-Parietal Cell Antibodies
- Optional:
- Aerodiagnostics SIBO breath test
- GI-Map stool test with zonulin
- Rationale
- We want to obtain an up to date snapshot regarding autoimmune thyroid and what her current thyroid levels. Given the history of hyperthyroid, I added Graves’ antibodies.
- Since she has had high TSH historically, with normal free T4, we can use the dialysis-LC/MS methodology to identify if she might be pre-hypothyroid.
- We can use insurance here so I’m opting to assess GI through insurance labs, LabCorp.
- Additional data of SIBO and a GI-Map could be helpful but is not required, so I have listed as optional.
- LabCorp
Recommendations
- Diet:
- Continue on your previous diet. Stay somewhat close to the rules laid out by the Whole30 Paleo diet. Do your best to be compliant, but you do not need to be perfect.
- Experiment with less/stopping coffee
- NRT: Vit D/K, Omega-3 supplement
- GI: Fiber, prebiotic
- Note: Be on the supplements for at least 3 weeks before following up. Please make a note of the change you noticed from diet versus supplements
- Follow Up: 4 weeks
- Rationale
- What should stand out here is the recommendation of fiber and prebiotics. Depending on how severe someone’s symptoms are, they might be a good candidate for the use of fiber and prebiotics. This is not an absolute rule, but it is worth a trial when considering preliminary data has found benefit in IBS patients using either. For some, this is the only nudge to the microbiota that will be needed.
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Fiber – worsened constipation & GI, could only do a lower dose.
- Prebiotic – NR.
- Improved:
- N/A
- Same:
- Constipation, bloating, fatigue, weight, hair
- Worse:
- Lower back/neck stiffness/pain, mood, Granulomas
Lab interpretation:
- Outside Breath and stool testing:
- H. pylori breath test – negative
- SIBO breath test – negative
- GI-Map stool test with Zonulin:
- Helicobacter pylori, Candida spp.
- Fxn: Calprotectin: 344-H
- LabCorp:
- Candida Antibodies, IgA, IgG, IgM, ELISA
- IgM: 15-H
- Inflammatory Bowel Disease (IBD) Expanded Profile; ACCA, ALCA, AMCA, gASCA, pANCA.
- gASCA: 69-H
- Vitamin D: 50.4 WNL
- Ferritin: 91 WNL
- RBC 3.62-L, Creatinine 0.55-L, BUN/Creatinine Ratio 33-H
- UA-Ph 8-H
- LDL 116-H, HbA1C 4.7-L
- Candida Antibodies, IgA, IgG, IgM, ELISA
- Outside (Quest):
- H: EBV: EA (61), VCA, NA
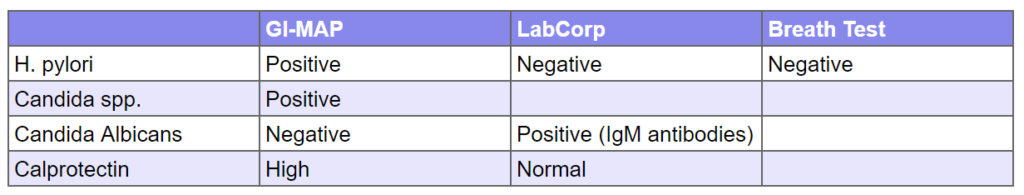
Major disparities in lab testing:
As you can see below, labs often do not match. This is why clinicians must think critically. In this case, we see where GI-Map’s DNA-based testing suffers from false positives, (presumably, we can’t say for certain).
- H. pylori was positive via GI-Map, but negative upon a breath test, LabCorp’s stool and blood test. The majority of the suggests HP was a false positive
- Candida was partially agreed upon via both tests, although not strongly via LabCorp (IgM abs alone are weak, and LabCorp’s yeast culture was negative).
- Calprotectin was positive via GI-Map but not via LabCorp. I see this often, be on the lookout. GI-Map suffers from a HIGH degree of what appears to be false positive. In a recent discussion with Dr. Ilana Gurevich, she suggested this is because GI-Map kits do not provide refrigeration needed to ensure sample quality.
Impression:
- Today has regressed. The fiber flared, prebios were neutral. Other doc found EBV reactivation, and since she had responded very well to EBV Tx in the past she will start again today. Today will also start probios, for candida, and stop fiber/prebio.
- Commentary: as you can see the fiber and prebiotic trials can go either way, this is why I advise caution.
Recommendations
- New:
- GI: Lacto-Biff, S. Boulardii, Soil-based
- Start the probiotics one at a time, every few days. Stop any that causes a negative reaction that lasts for more than a few days.
- Stop the fiber and the prebiotic
- Start the antiviral treatment with your other doctor
- GI: Lacto-Biff, S. Boulardii, Soil-based
- Follow up: 6 weeks
Visit 4
Subjective Assessment:
- Completed antiviral protocol (Vit A, D, monolaurin) – body did not respond well, rxns; rashes.
- Probios (Lacto-Biff, S. Boulardii, Soil-based) – NR.
- Improved:
- n/a
- Same:
- Constipation, bloating, fatigue, weight, hair, lower back/neck stiffness/pain.
- Worse:
- Granulomas, brain fog, mood. Got period 2x while on monolaurin (in 1 month).
Impression:
Today is the same or worse as the last visit. Antiviral protocol + travel seem to have regressed. Probios – NR. Today will start on Low Histamine + gut support nutrients, then to Habx. Abby was feeling discouraged.
Recommendations:
- New:
- Perform a 1 week trial on a Low Histamine Diet,
- The rest of my recommendations are listed here. Before you read, what would you do next?
- GI: Habx base protocol + gut support nutrients
- Cycling: Estro+Progest Harmony
- Start with gut nutrients and LH diet. Then on to Estro+Progest Harmony, then the herbal antimicrobials. Give each 3-5 days.
- Follow Up: 5-7 weeks
Dr. Ruscio’s Comments
I wanted to share this case mainly to point out an important problem with GI-MAP’s (I suspect the same problem with Doctor’s Data) calprotectin stool testing. It comes back as a false positive, a lot. Don’t let this sway you away from what is clinically indicated.
Allowing this patient to pursue a previously helpful treatment, the anti-virals, will also increase compliance as she will be less likely to have a grass-is-greener longing to see her other provider for antiviral therapies. This is where listening to the patient and entertaining therapies you might not find fruitful (antiviral treatment) can be a win from a compliance perspective. It also helps you determine what the best intervention might be via a process of elimination.
We are still not out of the woods with this case. What would you do next?
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!