Practitioner Case Study – December 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Mechanism, Clinical Studies and Distinctive Nutritional Requirement of Oral Immunoglobulins in IBS-D and SIBO
- The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study
- Fluctuation of zonulin levels in blood vs stability of antibodies
- Rapid-Fire Research – Ultra-concise summaries of noteworthy studies
- A low FODMAP gluten-fee diet improves functional gastrointestinal disorders and Overall Mental Health of Celiac Disease Patients: A Randomized Controlled Trial
- Evaluation of serum-derived bovine immunoglobulin protein isolate in subjects with diarrhea-predominant irritable bowel syndrome
- Association of thyroid hormone therapy with quality of life and thyroid-related symptoms in patients with subclinical hypothyroidism: A systematic review and meta-analysis
- Thyroxine and triiodothyronine content in commercially available thyroid health supplements
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- John, 28yo male
- Previous Dx
- Ulcerative proctitis
- Rx
- Canasa (Mesalamine suppository)
- Chief Complaints
- Loose stools, 5-CO
- Blood in stool, 3-CO
- Stomach bloat/gnawing, 2-OC
- Bloating, 2-OC
Visit 1 (Day 1) – History and Exam:
Initial Impression
- John presents as a generally healthy 28yo male with a good diet, lifestyle, and outlook on health.
- He has been dx with UC/UP recently and is on Mesalamine suppository (Canasa).
- He didn’t respond to oral 5’ASAs. He would like to find a non-suppository and natural treatment.
- We will work through treatments for UC and also investigate any other factors like SIBO/dysbiosis.
- Prognosis fair to good, due to distal nature of UP.
- Previous testing:
- Colonoscopy to diagnose UP
Previous Diets
- Low FODMAP – NR. Low CHO, DF/GF – helpful. (NR=non-responsive)
Previous Treatments
- VSL#3 – MR. Canasa – helps loose/bloody stools. Lialda (oral) – NR
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- Diagnostic Solutions GI-Map stool test
- Rationale:
- The SIBO breath test is a bit of a reach, but we do know that IBS and IBD can occur together. The challenge here is ulcerative proctitis is so distal, there may be minimal involvement of SI.
- However, it is possible, at least in theory, that the overzealous immune tone in the rectum could be driven by immune activation in the SI.
- The GI-Map shares the same rationale, but this test also contains inflammatory markers known to correlate with IBD, and UP is a subset of IBD.
- His other symptoms (bloating, loose stools, stomach gnawing) might all be caused by dysbiosis which these tests can find.
Recommendations
- Diet
- Please perform the Modified Fast for 2-4 days (see website for PDF), then
- Return to your previous low/moderate carb paleo diet that is gluten and dairy free. You can eat more carb dense carbs (ones you tolerate) to gain weight. Consider a trial of the Paleo low FODMAP Diet
- Please be on the diet for 2 weeks before starting the supplements, but continue diet until our follow up. Then be on the supplements for 3 weeks before following up. Please make note of changes you noticed from each one of these steps.
- Lifestyle
- na
- Supplemental
- NRT: Vitamin D/K, Omega 3-6-9 blend, Curcumin
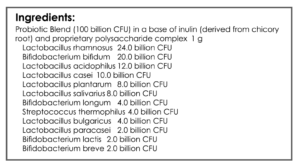
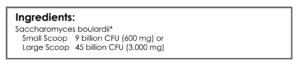
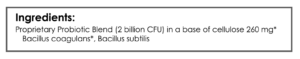
- GI: Lacto-Biff probiotic, S. boulardii, soil-based probiotic, gut repair cocktail
- Rationale
- Evidence has shown vitamin D, omega, curcumin, probiotics, and gut repair nutrient cocktails to improve IBD
- His other symptoms (bloating, loose stools, stomach gnawing) might all improve from the above treatments
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- MF (broth) – helped a lot
- Paleo LF diet – moderate help
- Supplement program – very helpful, no blood and normalized stools
- Improved:
- no CCs for about 3 weeks
- Same:
- na
- Worse:
- na
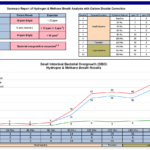
Lab Interpretation:
- Aerodiagnostics Lactulose SIBO breath test
- H2: rise 34, peak 36. CH4: 6
- DiagnosticSolutions GI-Map stool test
- H. pylori, Calprotectin (**1590**), Occult blood
- Dx
- mild H2 SIBO, H. pylori, extremely high inflammation (calprotectin)
Impression:
- 12/13/17 – John’s labs show mild H2 SIBO, H. pylori and extremely elevated Calprotectin. He has improved markedly today, all CCs improved and no further improvement needed. The Calpro is likely much improved today and methodology might be prone to false+s. Today we will maintain current plan. Then fu in 2-3 months and then first work to wean of Canasa (with GIs help) and then later to reintro diet, then finally wean off the program.
- Note: Yet another example of how we often do not need to treat lab findings if we get the initial therapies right, in this case, diet, anti-inflammatory support, and probiotics. I hope you are seeing why I am parsimonious with my use of lab testing.
Recommendations:
- Continue previous:
- Diet
- Return to your previous low/moderate carb paleo diet that is gluten and dairy free. You can eat more carb dense carbs (ones you tolerate) to gain weight. Consider a trial of the Paleo Low FODMAP Diet
- Lifestyle
- na
- Supplemental
- NRT: Vitamin D/K, Omega 3-6-9 blend, Curcumin
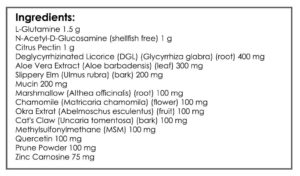
- GI: Lacto-Biff probiotic, S. boulardii, soil-based probiotic, gut repair cocktail
- Diet
- Starting
- You can use the Modified Fast periodically for a day to help calm things down, as needed.
- continue current plan
- keep up the good work!
- fu: 2-3 months
Visit 4
Subjective Assessment:
- Continuing to improve
- Improved:
- all CCs
Impression:
- 4/25/18 – Continues to improve from the program. Today decided to maintain current course for a few months, allowing him a chance to assess how he does when he occasionally missed a Canasa dose. Then we will fu and work plan of dietary reintro, followed by program curtail and +/- Canasa. Will fu when he is ready to take the next step.
Recommendations:
- Continue the previous program
- Starting
- reduce dose to probiotics to once per day
- fu: 2-6 months
Dr. Ruscio’s Comments
It’s been 7 months and I haven’t seen John, so I am assuming he has done great and was able to gradually wean off Canasa and maintain his improvements. Perhaps he occasionally needs a dose or two, but again I am assuming no news is good news since the last time we saw him he was doing great.
This is another case where we did not need to treat the lab findings. In fact, I would guess that if he aggressively treated SIBO with antimicrobials and high doses of additional anti-inflammatory cocktails, it may have flared him. Yes, labs can help, but don’t use them as a crutch instead of relying on good clinical common sense and logically applying the available treatments.
I am also suspicious that the calprotectin on some functional labs is overly sensitive. There have been a number of cases where the functional lab’s calprotectin did not match the clinical picture nor the LabCorp or Quest calprotectin I have ordered in tandem in some cases. This is just something to be aware of so as to prevent potential overreacting.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!