Patient Summary:
- Overview Context:
- Patient is a 66 year old female whose “world was turned upside down” due to GI symptoms worsened by treatment for suspected SIBO. Since being put on antibiotics, elemental dieting, and a restrictive diet for “SIBO” treatment, she has experienced fear of food, weight loss, and worse symptoms.
Symptoms and Concerns
- Chief Complaints:
- GI Symptoms:
- Stomach pain
- Nausea
- Gas
- Reflux
- Systemic Symptoms:
- Brain fog
- Fatigue
- Mood swings
- Weight loss
- GI Symptoms:
- Onset/Timeline
- 20s – Candida and antifungal treatment
- 30s – Chronic bronchitis; antibiotic use every 6 months
- 50s – GI symptoms began
- 60s – IBS diagnosis
- July 2022 – “SIBO diagnosis” (presumed by previous physician via stool test). Prescribed a low sulfur diet, antibiotic, and elemental diet.
Past Medical History
- Prior Diagnosis:
- Osteoporosis
- GERD
- Hypothyroidism
- IBS – 2019
- Medications:
- Compounded T3/T4
- Bio-identical testosterone
- Bio-identical progesterone
- Supplements:
- Similase enzymes
- Betaine HCI
- Krebs magnesium/potassium complex
- Albion magnesium lysinate glycinate
- Quercetin
- Zinc carnosine
- Vitamin D
- Fish oil
- Strontium
- Prior Surgical History
- N/A
Prior Testing and Treatment History
- Prior Testing Summary:
- Stool test
- Dysbiosis present, otherwise unremarkable
- Stool test
- Previous Diets:
- Helpful:
- Low histamine
- Low sulfur
- Fasting
- Paleo
- Intermittent fasting
- Helpful:
- Previous Treatments:
- Helpful:
- PRObiotics (lacto/bifido)
- Digestive enzymes
- Hydrochloric acid (betaine HCl)
- No change:
- Probiotics (soil-based)
- Worse:
- Synbiotics
- Antibiotics
- For presumed SIBO, worsened gas, bloating, and fatigue
- Elemental Diet
- For presumed SIBO, worsened gas, bloating, and fatigue
- Helpful:
Initial Impression
- Clinical Commentary:
- This patient came to see us with an unproven SIBO diagnosis based on stool testing, given to her by her previous functional medicine doctor. This diagnosis led the patient to undergo a restrictive low sulfur diet as well as a round of antibiotics and elemental dieting, which led to a fear of food, weight loss, and worse GI symptoms.
- Do we need to confirm or rule out a SIBO diagnosis?
- Will a SIBO diagnosis change our treatment plan, or can we treat her empirically for dysbiosis?
- Initial Testing Recommendations
- Tests:
- No tests were performed at the initial appointment.
- Rationale:
- Our main differential at this time is dysbiosis. While it’s possible she has SIBO, we don’t feel testing is necessary at this time because it won’t change our treatment plan. Our treatments for SIBO and dysbiosis are essentially the same. We willI use her symptoms and response to treatment to guide our plan.
- Tests:
- Initial Treatment Recommendations
- Diet:
- Stop the low sulfur diet
- Start the low FODMAP diet – 80% compliance only
- Lifestyle:
- Begin meditation or breathwork
- Continue current activity level and increase resistance training when able
- Spend time in nature twice weekly
- Supplements:
- Lactobacillus & bifidobacterium probiotic blend, soil-based probiotics, and saccharomyces boulardii probiotics
- Continue (on your own)
- Vitamin D
- Fish oil
- Strontium
- Discontinue:
- Similase enzymes
- Betaine HCI
- Krebs magnesium/potassium complex
- Albion magnesium lysinate glycinate
- Quercetin
- Zinc carnosine
- Followup:
- 5 weeks
- Rationale:
- Given her weight loss and fear of food, we want to expand her diet from low sulfur to a low FODMAP diet.
- Many patients are on excessive supplementation. The potential problem with this is they don’t know either what is helping or what could be worsening their symptoms. Recommending a supplement holiday can be a very powerful tool.
- Listening to how patients speak about their symptoms can be insightful. Patients who speak about food or symptoms with a fear-based narrative (e.g. “my world was turned completely upside down”) often significantly benefit from stress-reduction practices, whether that’s meditation, time in nature, or limbic retraining.
- The main components of our plan will include probiotics, a supplement holiday, dietary expansion, and stress reduction.
- Diet:
- Subjective Assessment
- 70% better.
- Current Symptoms:
- Improved:
- GI Symptoms
- Nausea
- Gas
- Stomach pain
- Reflux
- GI Symptoms
- Systemic Symptoms
- Energy
- Brain fog
- Mood swings
- Same:
- Weight
- Worse:
- NA
- Improved:
- Response to Treatment
- Diet:
- Paleo low FODMAP: Improved GI symptoms.
- Lifestyle:
- Time in nature: Improved overall sense of wellbeing
- Supplements:
- Probiotics: Improved GI symptoms
- Diet:
- Impression:
- Expanding her diet, reducing unnecessary supplementation and starting her on probiotics led to significant improvement in not only GI symptoms, but also mood, energy, and mental clarity. Her positive response to our initial plan suggests we are on the right path.
- She had tried multiple individual probiotics in the past, however in this case, the combination made the biggest difference.
- Treating the person, rather than treating a lab, led to a greater symptomatic improvement.
- Updated Treatment Recommendations
- New Treatment:
- Begin expanding the low FODMAP diet
- Double all probiotics (lacto/bifido, soil-based, and s. boulardii)
- Start herbal antimicrobial protocol (if symptom improvement plateaus)
- Health coaching for weight gain support
- Followup: 5 weeks
- New Treatment:
- Rationale
- When a treatment is working well, we like to double down. In this case we are increasing her probiotic dose as it appeared to be effective for improving GI symptoms.
- We are giving her the option to add in herbal antimicrobials if her GI symptoms aren’t continually improving. She may see continued improvements with more time on the probiotics and other recommendations, but we also like to empower the patient by including them in the decision making process.
- We are further relaxing her diet by moving from a Paleo low FODMAP diet to a standard low FODMAP diet. This allows her to include a greater variety of foods, like grains, and thus help her gain weight.
Clinician’s Comments
- As clinicians, we need to be careful with the labels we put on patients. This patient was diagnosed with SIBO despite no proper testing. This can lead to worse patient outcomes for a few reasons. First, it can lead to psychological distress, especially in someone prone to anxiety, because now they have a “condition” to worry about. Second, if a practitioner is treating based on lab findings, they may use treatments that aren’t necessary, such as antibiotics or a restrictive diet.
- Rather than treating labs, we treated her as a person. This led to a significant improvement in almost all of her symptoms after just one visit.
- When it comes to dietary restrictions, it’s important to be mindful of the law of diminishing returns. We find so often that continually restricting a patient’s diet doesn’t lead to more improvement. In fact, we find that too much restriction can worsen symptoms and mental wellbeing.
Study Purpose
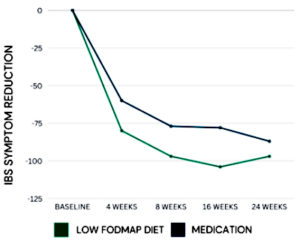
- A low FODMAP diet is commonly used for patients with IBS. This study aimed to compare the effectiveness of a low FODMAP diet versus a medication for IBS.
Intervention:
- 459 participants with IBS (IBS-C, IBS-D and IBS-M), all randomized to one of the following for 6 months:
- Low FODMAP diet (delivered via phone application)
- Spasmolytic medication (Otilonium Bromide, aka Spasmomen)
Main Results:
- After 2 months, more IBS patients responded favorably to the low FODMAP diet compared to medication (71% diet vs 61% medication).
- After 4 months, the low FODMAP diet reduced symptom scores more than medication (-105 points vs -79 points).
- In general, the low FODMAP diet led to the greatest improvements in:
- Abdominal distension
- Abdominal pain
- More severe IBS symptoms
- However, the diet and medication were equally effective in improving:
- Quality of life
- Anxiety
- Depression
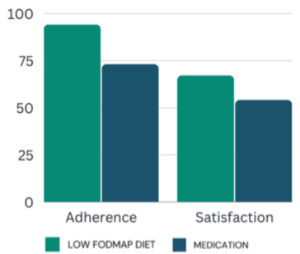
- Adherence (94% vs 73%) and satisfaction (67% vs 54%) were greater in the low FODMAP group compared to the medication group.
Authors Conclusion:
- “In conclusion, in this large primary care IBS cohort, an 8-week usage of a diet application was superior to standard medical therapy…lifestyle adjustments may be more attractive than long-term medication intake for a majority of patients in primary care. A FODMAP-lowering diet should be considered the first-line treatment for IBS in primary care.”
Clinician’s Comments
- Recommending the low FODMAP diet as a first-line intervention for those with IBS is backed by a recent 2022 expert review by the American Gastroenterological Association. They concluded “the low-FODMAP diet is currently the most evidence-based diet intervention for IBS.”
- While this diet has the most evidence for improving IBS, in the clinic we see patients improve their IBS symptoms with less restrictive diets. This observation is backed by a recent 2022 randomized controlled trial that compared the effectiveness of 3 different diets for IBS. This study found no statistically significant difference in IBS improvement when comparing a low FODMAP diet, a gluten-free diet, and a general healthy eating diet. This supports our approach of starting with the least restrictive diet before moving on to more restrictive diets.
Clinical Takeaways
- The low FODMAP diet is effective for improving IBS.
- However, we typically start with less restrictive diets, such as the Paleo diet.
- We decide which diet to start with based on their previous diet history.
- If they are on a standard american diet, then we’ll likely start with the Paleo diet.
- If they are already on a Paleo diet, then we’ll likely move right to the low FODMAP diet.
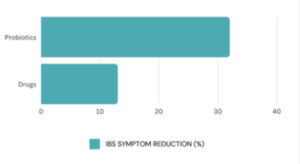
Study Purpose
- Probiotics are another commonly used treatment for IBS. This 2022 systematic review and meta-analysis aimed to compare the effectiveness of probiotics and medications for IBS.
Intervention:
- 32 randomized controlled trials on patients with IBS, randomized to either:
- Placebo vs medications
- Placebo vs probiotics
- Which medications were studied?
- Mesalazine (anti-inflammatory)
- Rifaximin (antibiotic)
- Linaclotide + Plecanatide (for constipation)
- Note: This is not an exhaustive list
- Which probiotics were studied?
- Lacto/bifido blend (10 studies)
- Soil-based (2 studies)
- S. cerevisiae (1 study)
- E. coli Nissle 1917 (1 study)
- Caveat: None of the studies included in this paper were head to head comparisons, meaning they didn’t directly compare probiotics vs medications.
Main Results:
- Both probiotics and medications were more effective than placebo for improving:
- Global IBS symptoms (32% probiotics vs 13% medications)
- Abdominal pain
- Only medications led to improvement in bloating; not probiotics.
- Adverse Events
- While there was a trend of more side effects from medications compared to probiotics, a direct comparison could not be made due to poor reporting of safety in the probiotic studies.
Authors Conclusion:
- “The meta-analyses we performed indicated that both probiotic and drug interventions might be able to improve the persistence of IBS symptoms and abdominal pain scores.”
Clinician’s Comments
- This study found similar efficacy between probiotics and medications for IBS, with some pros and cons to each intervention.
- While medications led to greater improvements in bloating, probiotics may be more effective for improving global IBS symptoms.
- Medications may lead to more side effects than probiotics.
- The data in this study could be stronger if they performed direct comparisons between probiotics versus medications for IBS. However, it still provides us with valuable data to support the use of both probiotics and medications for IBS.
- This study assessed multiple categories of probiotics, including lacto/bifido blends, soil-based, and healthy fungus (S. cerevisiae). This suggests there may not be a single best probiotic for those with IBS.
Clinical Takeaways
- Instead of thinking patients need to do either medications or probiotics, they can start with diet and probiotics. If there is no significant improvement after 4-8 weeks, they can trial IBS medication.
- Patients can either experiment with various categories of probiotics or simply take the 3 categories (lacto/bifido, soil-based, and s. boulardii) at the same time.
Listener asks:
How do you know if someone needs limbic retraining?
What is the limbic system?
The brain wants to keep us safe and alive. When our brain feels under attack (i.e. running from the lion), it initiates the appropriate defense responses necessary to help us survive. Once the threat is over, our brain can then relax and “turn off” the defenses. However, in some people, this defensive response can become over-protective. Following a trigger (e.g. physical trauma, emotional trauma, chemical exposure, mold, etc), their brain can become “stuck” in fight or flight, which can contribute to symptoms such as cognitive difficulty, mood imbalances, low energy, or increased reactivity.
Limbic retraining rewires the brain to calm down the hyper-vigilant limbic system, letting it know that you are safe. We at the clinic have found limbic retraining to be a game-changer for a certain cohort of our patients. There are a few key distinguishing features about their presentation and history that indicate they will benefit from limbic retraining, which include:
- Highly Reactive/MCAS
- Mold
- Fear-based
- Trauma/PTSD
Highly Reactive/MCAS
We see patients who are very reactive to their environment, including perfumes, fragrances, off-gassing from furniture, gasoline, and more. They may be on a very restrictive diet due to increased food reactivity, as well as have a hard time taking supplements because they experience negative reactions frequently. Many of our highly reactive patients have also been diagnosed with MCAS. We have seen limbic retraining specifically benefit these patients, and our understanding is that limbic imbalance can prime the mast cell for over activation as part of the defensive mechanism.
Mold
Patients who have a history of mold exposure, alongside mold-related symptoms, can benefit from limbic retraining. A proportion of patients with mold may have a difficult time taking therapeutic doses of binders or probiotics due to increased reactivity. We find limbic retraining helps reduce their reactivity to supplements and their environment, so they can begin feeling better.
Fear-Based
Paying attention to the way patients speak or write can be very insightful. Patients who benefit from limbic retraining are often self-identified with their condition. They may say things like “My SIBO,” or “My leaky gut” in an anxious or worried way. They could also be hyper-vigilant about their symptoms, constantly checking in with their body to see how they feel. These patients may get overly preoccupied with every small detail in their labs, or keep detailed food and supplement diaries to look for trends in their symptoms. The more often a patient is thinking about their symptoms in a fearful or worried way, the higher the probability they will benefit from limbic retraining.
Trauma/PTSD
Many patients who have been sick for a long time can often have a history of trauma as a triggering event for the onset of their symptoms. This can include physical or emotional abuse, physical trauma like an accident, an infection, or extreme stress. History of trauma followed by the onset of symptoms can be a sign that a patient may benefit from limbic retraining.
Consider using this clinically useful therapy for your patients who seem to fit these criteria. It is one of the most impactful therapies we recommend. The top programs we recommend to our patients include Gupta or DNRS.