Patient Summary:
- Overview Context:
- Elena came in as a 48 year old female with significant symptoms of anxiety, fatigue, and brain fog. She had been treated inappropriately and unsuccessfully with many interventions, such as high doses of thyroid hormone, testosterone therapy, excessive nutritional supplements, and peptide therapy. She was very fearful and felt “like a guinea pig” with all the treatment recommendations and NO improvement.
- Subjective Assessment
- Overall health rated as 50/100
- Symptoms:
- Anxiety
- Agitation
- Fatigue
- Brain fog
- Headaches
- Body tingle
- Restless leg syndrome
- Muscle twitches
- Sense of internal vibration
- Onset/Timeline
- 2016 – Hysterectomy
- 2021 – Many of her symptoms began during this time. Blood work discovered high calcium. Parathyroid adenoma found. Parathyroid glands removed.
- This successfully lowered Ca levels, but symptoms persisted
- Dec 2022 – Began to work with our clinic
- Medications:
- None
Prior Testing and Treatment History
- Prior Testing
- GI-MAP
- Dysbiosis found
- No pathogens
- GI-MAP
- Previous Treatments
- Nutrient replacement therapy
- Zinc, fish oil, cod oil, vitamin D, NAC, multivitamins, vitamin C, curcumin/turmeric, coQ10, magnesium
- Thyroid hormone replacement
- Multiple thyroid hormone formulations
- Caused insomnia and worsened anxiety
- Multiple thyroid hormone formulations
- Peptides & testosterone
- Made her feel worse
- Made her feel worse
- Dietary restrictions
- Dietary trials left her hyper-focused on eating clean
- Developed fear of food
- Dietary trials left her hyper-focused on eating clean
- Nutrient replacement therapy
Initial Impression
- Elena felt worse on every thyroid formula, predicting that she was being treated inappropriately.
- She presents as overly focused on treatments and fearful – predicting benefit from limbic retraining.
- Like many, she didn’t improve after extensive nutrient supplementation.
- Initial Treatment Recommendations
- Diet:
- Maintain higher protein, lower carbohydrate diet
- Lifestyle:
- Begin a limbic retraining program
- Gradually increase your exercise
- Begin Epsom salt baths
- Supplements:
- Patient instructed to stop all supplements
- No supplements were given
- Other
- Discuss discontinuing thyroid hormone with your prescribing physician
- Followup:
- 5 weeks
- Diet:
- Clinical Commentary:
- Elena had been made worse from overtreatment by her previous practitioners, so our first step together was to get her to a new baseline by simplifying her program and refocusing on fundamentals.
- The fundamentals we chose were the Gupta Program, a gradual increase in physical activity, and Epsom salt baths which Elena had previously found helpful.
- Subjective Assessment
- 60/100, 0% better/worse.
- Current Symptoms:
- Improved:
- Sleep
- Same:
- Muscle twitches/internal vibration
- Dizziness
- “Jitters”
- Fatigue
- Headaches
- Worse:
- Dizziness in the morning
- Improved:
- Response to Treatment
- Lifestyle:
- Limbic retraining program: Hasn’t started
- Exercise: She “felt exhausted after weights” – started rowing and biking instead
- Epsom salt baths: Helpful for muscles and GI regularity, but made her heart race and made her feel weird & jittery
- Stopping thyroid medication: Improved sleep
- Lifestyle:
- Updated Treatment Recommendations
- New Treatment:
- Lower bathwater temperature and have Epsom salt baths 1-3 times a week, maintain exercise, and aim not to overdo it.
- Begin limbic retraining
- Begin lactobacillus/bifidobacterium, soil-based, and saccharomyces boulardii probiotics.
- Begin thiamine supplementation
- Testing:
- Urinary mycotoxins
- Heavy metals
- Urine
- Blood
- Followup: 5 weeks
- New Treatment:
- Clinical Commentary:
- Elena began sleeping better after she stopped thyroid, but her main symptoms have not stabilized, suggesting another factor is at play.
- Many patients with chronic fatigue, mold, or heavy metal toxicity feel particularly fatigued by lifting weights, and do better by starting with low intensity cardio and progressing from there.
- Feeling worse after Epsom salt baths suggests a toxic etiology, as Epsom salt baths can mobilize toxins. The cluster of muscle twitches / internal vibration, headaches, and anxiety also support a toxic etiology.
- Subjective Assessment
- 75/100, 50% better.
- Current Symptoms:
- Improved:
- Jitteriness
- Dizziness
- Sleep
- Fatigue
- Same:
- Body tingles
- Worse:
- None
- Improved:
- Response to Treatment
- Lifestyle:
- Gupta: Just started program
- Epsom salt baths: She decided to discontinue completely
- Supplements:
- Probiotics: Tolerating probiotics without issues
- Thiamine: Has helped energy
- Lifestyle:
Labs:
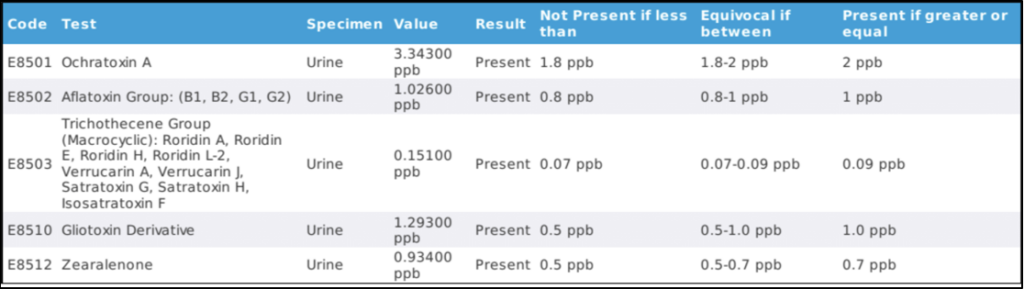
Mold Testing
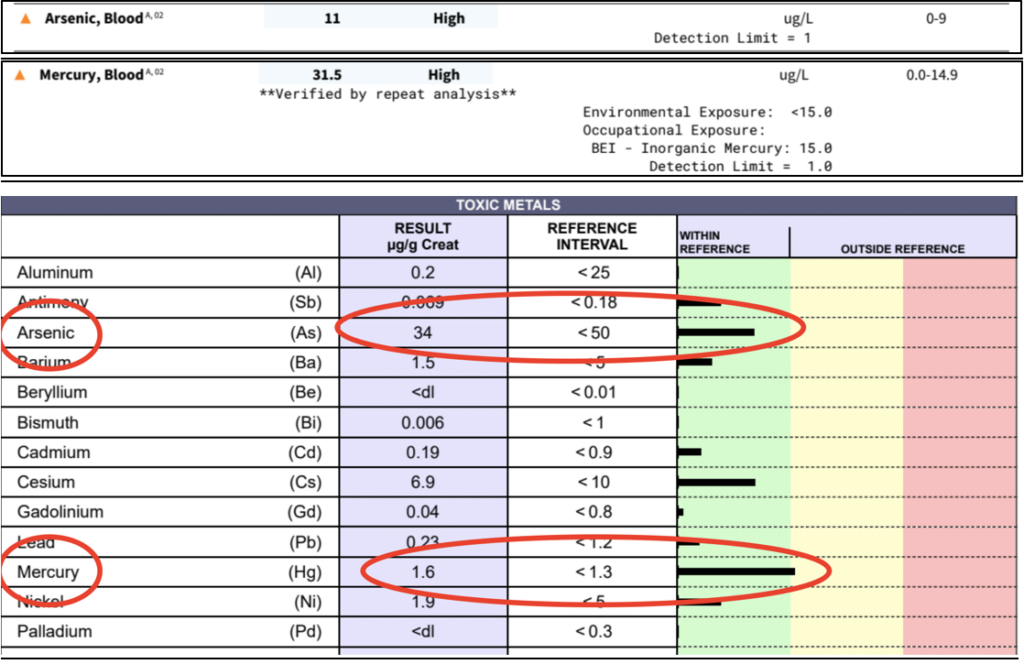
Heavy Metals (Blood)
- Lab Interpretation:
- Elena has the highest blood mercury that I’ve seen in clinical practice. Elena explained that she was eating high amounts of sushi, fish & oysters for years, believing these protein sources to be the healthiest. Furthermore, she grew up in Russia near chemical plants, and remembers playing with a broken mercury thermometer as a child.
- Her urinary mycotoxin test is positive, but not nearly as elevated and concerning as the elevated mercury levels.
- While Elena described feeling 50% better, I suspect that this figure wasn’t completely accurate, and may be artificially inflated by her experience of finally seeing treatments beginning to help her to feel better rather than make her feel worse.
- Updated Treatment Recommendations
- New Treatment:
- Increase probiotics to twice daily
- Eliminate all seafood. Review other sources of mercury.
- Slowly begin Heavy Metal Detox Program
- Followup: 4 weeks
- New Treatment:
- Heavy Metal Detox Protocol
- First, please:
- Continue all of my previous recommendations
- Drink plenty of water (1/2 your body weight in ounces)
- Sweat regularly (sauna or aerobic exercise 20-30 mins 2-3x weekly)
- Move your bowels regularly
- Second, add the below supplements one at a time, spaced apart by 3 days. After 90 days we will hold all supplements and retest your heavy metals to see if additional detoxification is needed.
- Modified Citrus Pectin: Starting with 1/2 scoop in water 1x daily, increase as tolerated to 1 scoop three times daily.
- Note: Each scoop contains 5 grams of MCP.
- Activated Charcoal: 1-2 capsules on empty stomach daily taken with chlorella
- Chlorella: 1-2 capsules on capsule on empty stomach with daily taken with charcoal
- (optional) Multi-Vitamin: 1 tablet, 1x per day, with food
- Modified Citrus Pectin: Starting with 1/2 scoop in water 1x daily, increase as tolerated to 1 scoop three times daily.
Closing Thoughts
- The cause of Elena’s symptoms may have seemed unclear at first, but it became relatively straightforward once we identified mercury toxicity. Reflecting back on her history, she had a few key signs that an environmental toxin was at the root of her symptoms, including:
- History of excess fish consumption
- Feeling worse from Epsom salt baths
- Post-exertional fatigue
- Past exposure to mercury
- While it will take some time to clear this high mercury load, she should improve steadily now that the issue has been identified.
Clinical Review Purpose
- Many women are looking to optimize their fertility. The role of thyroid dysfunction and treatment in fertility is debated. What can we learn from a review of the latest studies?
Do patients with subclinical hypothyroidism (SCH) have higher rates of miscarriage compared to euthyroid patients?
- Yes
- A meta analysis of 9 studies showed that women with SCH had a nearly 2x increased risk of having a miscarriage. Further, treatment with thyroid hormone lowered the risk so that it was equal to women without SCH.
- Women with SCH and thyroid antibodies had a 2.5x increased risk of miscarriage.
- No
- A 2016 study taking place across 4 medical centers in the US tracked 1,193 women of childbearing age who had a history of 1-2 pregnancy losses. In this study, there was no association between elevated TSH or thyroid antibodies with pregnancy loss.
- Another study done across 49 hospitals in the UK followed over 19,000 women with a history of miscarriage or infertility. They found that the prevalence of SCH in this population was low (2.4%), suggesting that thyroid is not a major contributor to miscarriage.
Do patients with SCH have a higher rate of premature birth?
- Yes
- A study of 47,000 women in the US showed that there was a 1.4% higher rate of preterm birth among women with SCH compared to women without. The higher the TSH, the higher the likelihood of preterm birth.
- There was a 1.6% increased chance of preterm birth for women with elevated TPO antibodies
- “Among pregnant women without overt thyroid disease, subclinical hypothyroidism, isolated hypothyroxinemia, and TPO antibody positivity were significantly associated with higher risk of preterm birth.”
Does Hashimoto’s thyroiditis lower the success rate of in-vitro fertilization (IVF)?
- Yes
- A 2023 meta-analysis of 7 studies and 8,431 euthyroid women evaluated if thyroid autoimmunity increased the risk for worse IVF outcomes. This study found if TPO was less than 100 IU/mL, there was NO increased risk for worse IVF outcomes. However, when TPO antibodies were >100 IU/ml, there was a 2x increased risk for miscarriage and a 34% reduced chance of delivery.
- “This meta-analysis suggests that, for euthyroid patients, high levels of TPO-Ab (>100 IU/mL) could adversely influence the pregnancy outcome of assisted reproductive technology.”
- A 2023 meta-analysis of 7 studies and 8,431 euthyroid women evaluated if thyroid autoimmunity increased the risk for worse IVF outcomes. This study found if TPO was less than 100 IU/mL, there was NO increased risk for worse IVF outcomes. However, when TPO antibodies were >100 IU/ml, there was a 2x increased risk for miscarriage and a 34% reduced chance of delivery.
- No
- A systematic review and meta-analysis compared IVF success rates for women with positive anti-thyroid antibodies (TPO and or TG). There was no difference in pregnancy or miscarriage rates, the number of embryos transferred, or the number of oocytes retrieved.
- “The findings of the present study suggest that thyroid autoimmunity has no effect on pregnancy outcomes in euthyroid women alone, or in euthyroid women and women with subclinical hypothyroidism.”
- A systematic review and meta-analysis compared IVF success rates for women with positive anti-thyroid antibodies (TPO and or TG). There was no difference in pregnancy or miscarriage rates, the number of embryos transferred, or the number of oocytes retrieved.
Can treatment with levothyroxine lower the rate of miscarriages and preterm birth in women with SCH and/or thyroid autoimmunity?
- Yes
- The best study on this topic is a 2019 meta-analysis of nearly 8,000 women. This study strongly suggests levothyroxine treatment is beneficial to women with SCH or thyroid autoimmunity. In women with SCH, levothyroxine significantly decreased the risk of pregnancy loss, as well as improved outcomes in assisted reproduction (i.e IVF). In women with thyroid autoimmunity, levothyroxine decreased the risk of pregnancy loss and preterm birth rates.
- In a 2022 randomized controlled trial, 1,736 pregnant women with a history of miscarriages were randomized to either placebo or levothyroxine. In women with SCH, treatment with levothyroxine led to a significant reduction in miscarriage rate (21% levothyroxine vs 40% placebo). Levothyroxine also led to reduced miscarriages in women with TPO antibodies (7% levothyroxine vs 27% placebo). The authors conclude:
- “Levothyroxine therapy is recommended for SCH and TPOAb + women in pregnant women with recurrent pregnancy loss.”
How This Changes Clinical Practice
Summary of the Evidence
- The best evidence suggests subclinical hypothyroidism leads to higher rates of miscarriage and preterm birth.
- The presence of TPO antibodies >100 IU/mL increases the risk for miscarriage in women undergoing IVF. When TPO antibodies are <100 IU/mL, this does not lead to worse pregnancy outcomes.
- In women with subclinical hypothyroidism and/or elevated TPO antibodies, levothyroxine appears to lead to better pregnancy outcomes.
Clinical Takeaways
- This review confirms that thyroid health should absolutely be considered if a patient is struggling with fertility.
- At the RIFM, we see many patients who are inappropriately being given thyroid hormone and are hurt by overtreatment. While the majority of published trials have not shown benefit in treating subclinical hypothyroidism, the evidence above suggests that fertility is the exception to the rule.
During this year’s Forum for Integrative Medicine, I was asked if probiotics worsen SIBO. I wanted to answer it here as we get asked this question often by both patients and other providers.
Simply put, we have excellent clinical trial data supporting the use of probiotics for SIBO.
- From a 2019 study, we learn that probiotics are more effective when a patient has both IBS and SIBO (71% symptom reduction) compared to those that only had IBS (11% symptom reduction).
- We also have a recent 2023 clinical trial of 48 patients with SIBO and IBS-D. The probiotic saccharomyces boulardii led to greater improvements in diarrhea and IBS symptoms, and reduced bacterial overgrowth based on breath testing.
- Finally, we know that probiotics are similarly effective as Rifaximin in SIBO. Based on this 2017 meta-analysis of 7 studies, probiotics eradicate SIBO 53% of the time, while Rifaximin had a 59% eradication rate. What is even more noteworthy, the 2017 meta-analysis found when probiotics were used alongside antibiotics, there was an 85.8% eradication rate! This is an excellent data point showing that probiotics don’t worsen SIBO outcomes, but rather enhance the efficacy of antimicrobial therapy for eradicating SIBO.
We want to be careful of mechanistic or theoretical explanations. Theories are designed to be tested. If this theory was true, we would expect to see worse outcomes when giving probiotics to SIBO patients. However, both clinical experience and the medical literature support the utility of probiotics to resolve SIBO and reduce symptoms.
An important side note: This doesn’t mean a patient with SIBO won’t have a negative reaction to probiotics. Patients can react to probiotics (although it’s rare), However, we need to be careful we don’t assume they’re reacting because it’s “feeding SIBO”. There are a few common reasons we see patients react to probiotics. To review the top 5 most common reasons someone is reacting to probiotics, please check out the 2022 October FFHR edition practitioner question.