Patient Summary:
- Overview Context:
- Maddison is a 40-year-old female primarily coming to the clinic to seek answers for her severe histamine response to many foods. She is very physically active, great sleep hygiene, and has a stressful career.
Symptoms and Concerns
- Chief Complaints:
- Brain fog
- “Histamine Reaction” after eating – severe
- Vomiting
- Dizziness
- Throat itching and swelling
- Systemic rash (throat, chest, face, arms, torso)
- Bloating, Gas, Heartburn – Frequent, not severe
- Constipation – 3 BM/week
- Fatigue – frequent, not severe
- Onset, Timeline, and History:
- 2008 – Traumatic miscarriage
- A few weeks after her miscarriage, she became intolerant towards many different unknown foods, leading to what she called “histamine reactions”. These were happening on a weekly or biweekly basis.
- She reports even when all precautions were taken, she would still have a histamine reaction, but did not know why or from where.
- 2012 – Living on her own
- Because of her food reactions, she felt she needed to live on her own without roommates to avoid exposure to any possible triggers.
- 2016 – Severe reaction to gluten developed
- Gluten exposure, whether that was physical contact with it, accidentally consuming it or even if it was in the air, would lead to anaphylaxis, requiring the use of an epi-pen and Benadryl.
- 2008 – Traumatic miscarriage
Past Medical History
- Prior Diagnosis:
- Hypothyroidism (questionable diagnosis, never able to get records from previous doctor)
- Celiac Disease – 2006 (doesn’t have records to support diagnosis)
- Medications:
- Armour Thyroid 48.75 mg QD
- Cetirizine (Zyrtec) 10 mg QD
- Supplements (self-prescribed):
- Magnesium Citrate and Magnesium Glycinate
- Amino Acids
- HCL w/ Pepsin
- Probiotics
- Melatonin
- Theanine Serene
- Pancreatic Enzymes
- Topical Progesterone
- Gliadin-X
- Vitamin D3
- DIM
- Butyrate
- Iron
Prior Testing and Treatment History
- Previous Diets:
- Helpful:
- Low histamine/low FODMAP/low carb combination – Helpful for brain fog, gas, heartburn and bloating
- Reactive:
- Fermented foods, grains, gluten, onions, garlic, broccoli, cauliflower, raw kale, spinach
- Helpful:
- Previous Treatments:
- Helpful:
- Cetirizine – for histamine reactions
- Gliadin-X -if exposed to gluten
- Antibiotics – improved bloating, gas and brain fog
- Non-responsive:
- She is on many supplements that she is unclear whether they are helping or not
- Helpful:
Initial Impression
- Clinical Commentary:
- Does her positive response to low FODMAP + antibiotics indicate dysbiosis?
- Are her histamine-type symptoms a result of underlying GI imbalance/dysbiosis?
- Should we implement further dietary guidance/restrictions at this point or are we at the point of diminishing returns?
- She has already restricted many foods, is eating a very limited diet and actually appears to be undereating with not enough calories or carbohydrates, which is likely contributing to fatigue. I believe her reactivity to foods is a result of dysbiosis and limbic system imbalance secondary to trauma from miscarriage. By focusing on gut-centric care and addressing the limbic system, she should be able to expand her diet, reduce her symptoms, and be much less reactive.
- Recommended Testing
- GI-MAP Stool Test
- Blood Work: Lipids, CBC, CMP, ESR, CRP, anti-TPO, TSH, fT3, fT4, Homocysteine, Ferritin, B12, Folate, Vitamin D, HbA1c.
- Initial Treatment Recommendations
- Diet:
- Maintain your current low histamine/low FODMAP diet for now until we can reduce GI reactivity. Work on increasing carbohydrates, particularly on workout days.
- Lifestyle:
- Daily meditation
- Treatment:
- Triple therapy probiotics (Lacto/bifido, soil-based, s. boulardii)
- Start one probiotic at a time, slowly, given her history of hyper-reactivity.
- Start one probiotic at a time, slowly, given her history of hyper-reactivity.
- GI support nutrients
- Electrolytes (due to low carb diet)
- Triple therapy probiotics (Lacto/bifido, soil-based, s. boulardii)
- Followup: 4 weeks
- Diet:
- Clinician Summary
- My reason for performing the stool test was given the severity of her histamine-like reactions, I wanted to ensure there was no significant GI pathogen present, as well as assessing inflammatory markers like Calprotectin.
- I am not going to further restrict her diet because she is already too low carb/calorie, and further restrictions may do more harm than good. I am implementing triple therapy probiotics and gut healing support because of the high suspicion of dysbiosis and increased intestinal permeability. These therapies will be supportive whether or not there is a pathogen present. The combination of probiotics and gut gut healing nutrients can restore the lining of the gut and thus help with histamine degradation and restoring immune tolerance to food.
- Subjective Assessment
- Current Symptoms:
- Improved:
- Slight improvements in bloating, gas and heartburn
- Same:
- Brain fog
- Histamine reaction
- Fatigue
- Constipation
- Worse: none
- Improved:
- Treatment Response:
- Triple probiotics and GI support nutrients: Tolerated treatments well, but most symptoms remain unchanged besides gas, bloating and heartburn.
- Current Symptoms:
- Lab Results
- GI-MAP
- Shiga-like Toxin E. Coli stx2 7.50e2 (<1.00e3)
- No Parasites
- No H. Pylori
- Moderate deficiency dysbiosis
- Elastase 740
- Calprotectin 187 (High)
- Blood Chemistry
- Ferritin 38 ng/mL
- TSH 0.59 mIU/L
- fT3 3.4 pg/mL
- fT4 1.1 ng/dL
- Anti-TPO 1 IU/mL
- Vitamin D 24 ng/mL
- GI-MAP
- Lab Interpretation and Diagnosis
- Stool test revealed moderate dysbiosis and GI inflammation present. Pathogenic E. Coli toxin present but not flagged high.
- Blood work found vitamin D deficiency, low-normal ferritin, and euthyroidism without antibodies.
- Impression:
- My intention at this point in treatment is to support her gut with probiotics, while also working towards eliminating the dysbiotic bacteria. I intentionally chose single-herb antimicrobials instead of multi-herb because I wanted to minimize the risk of causing a histamine reaction (due to many different herbs in various antimicrobial products). I also wanted her to stop many of her supplements as they seemed unnecessary, which the patient agreed with. Given her symptom of fatigue + low-normal ferritin, I felt it was indicated to continue taking iron.
- Updated Treatment Recommendations
- Start:
- Oregano oil
- Allimax Pro
- Oregano oil
- Continue:
- Iron
- Triple therapy probiotics
- GI support nutrients
- Stop (her self-prescribed supplements)
- Amino Acids – Designs for Health
- HCL w/ Pepsin
- Probiotics – Nature’s Way
- Melatonin
- Topical Progesterone
- DIM
- Butyrate
- Followup: 6-8 weeks
- Start:
- Subjective Assessment
- Current Symptoms:
- Improved:
- Brain fog
- Histamine Reaction
- Bloating, Gas, Heartburn – Better, but noticed slight flare after increased carbohydrates.
- Fatigue – Better, especially after working out now that she’s increased carbohydrates.
- Constipation – Better, 1 bowel movement per day.
- Same: none
- Worse: none
- Improved:
- Treatment Response:
- Herbal antimicrobials: Less food reactions, better GI symptoms, improved brain fog.
- Notes:
- Hasn’t had a histamine reaction in about 3 weeks, which is rare for her.
- Reports ability to expand diet slightly without issues
- Current Symptoms:
- Impression:
- Overall, she is moving in the right direction with gut-targeted therapies. Less food reactions is a big indicator to me that dysbiosis is likely contributing to histamine intolerance. Of importance, she hasn’t had any negative reactions to the supplements.
- Updated Treatment Recommendations
- New Treatment:
- Start:
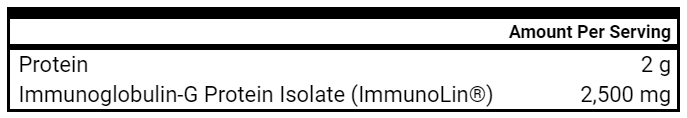
- Immunoglobulins
- Immunoglobulins
- Continue:
- Triple therapy probiotics
- GI support nutrients
- Oregano oil and Allimax
- Electrolytes
- Start:
- Followup:
- 6-8 weeks
- New Treatment:
- Updated Treatment Rationale
- Why immunoglobulins? My theory was dysbiosis was leading to increased bacterial toxins, which was “revving up” the immune system in the gut. Immunoglobulins are able to coat and bind toxins, like dipping shards of glass in wax, thus deactivating them and reducing immune reactivity.
- Subjective assessment:
- Improved: none
- Same:
- Bloating, gas and heartburn
- Worse:
- Brain fog
- Worsened when she ran out of probiotics and antimicrobial herbs.
- Histamine Reactions
- Reports 3 food reactions in the past month. These occurred when she wasn’t in her protective bubble.
- She also has been experiencing increased allostatic load due to career changes. Required use of epi-pen and Benadryl.
- Constipation
- Worse with increased allostatic load.
- Fatigue
- Brain fog
- Impression:
- Histamine intolerance seemed to have taken 2 steps forward and 1 step back, which coincided with an increased allostatic load in her life due to career changes.
- She let me know that she believes she has worse histamine intolerance when her stress levels are high. She started to get brain fog again once she stopped taking her probiotics and antimicrobials, which leads me to believe we have more work to do regarding her gut health.
- Because of how much stress affects her, and her symptoms of histamine intolerance began after her traumatic miscarriage, I believe Limbic Retraining will be very helpful for her. We will continue to work on gut health and also address her limbic system
- Updated Treatment Recommendations
- New Treatment:
- Start:
- Limbic retraining (Gupta Program)
- Continue:
- Immunoglobulins
- Triple therapy probiotics
- GI support nutrients
- Oregano oil and Allimax
- Electrolytes
- Start:
- Followup:
- 8 weeks
- Repeat calprotectin before next visit
- New Treatment:
- Subjective Assessment
- Current Symptoms:
- Improved:
- Histamine reaction
- Brain fog
- Same: none
- Worse:
- Constipation
- Fatigue
- Improved:
- Treatment Response:
- Immunoglobulins: Significant immune tolerance to food
- Notes:
- No histamine reaction or need for epi-pen in 1+ month
- “This is the longest I have not had a reaction in several years.”
- She successfully reintroduced food she previously couldn’t tolerate
- Her biggest win was she moved in with other people, which she hasn’t done in a decade.
- Her fatigue and constipation seemed to have gotten worse after increasing workload and not sleeping as well due to lack of a routine.
- Patient did not do limbic retraining due to perceived inability to make the time commitment required.
- She stopped the Oregano and Allimax antimicrobial herbs for 2 weeks, and she didn’t notice any regression
- No histamine reaction or need for epi-pen in 1+ month
- Current Symptoms:
- Lab Results
- Fecal calprotectin 10 mcg/g (previously 187 mcg/g)
- Lab Interpretation and Diagnosis
- GI inflammation appears to have reduced alongside significant symptomatic improvement.
- Impression:
- Maddison’s histamine intolerance is improving dramatically with a GI focused approach, specifically probiotics, antimicrobial herbs and immunoglobulins. I believe she no longer needs antimicrobial herbs at this point. I still feel Limbic Retraining would be useful and important for her to do based on her history of trauma and stress aggravating histamine intolerance.
- Updated Treatment Recommendations
- Diet + Lifestyle
- Limbic Retraining – When you feel ready for it
- Continue to work on expanding your diet and find a balance between symptom management and a variety of foods you can eat!
- Supplement
- Continue
- Triple therapy probiotics
- Immunoglobulins
- Stop
- Oregano and Allimax
- GI support nutrients
- Continue
- Followup: 2 months
- Diet + Lifestyle
Take Home Points
- Highlighted Clinical Rules
- Give time for healing before adding new treatments.
- Remember that lab tests only tell about 25% of the whole clinical picture. Good history taking, physical exam (when necessary), and assessment of prior treatment response supplies 75% of the information needed to make informed treatment decisions.
- Consider pushing further into therapies that have a clear positive signal as compared to adding new therapies (e.g. focusing on dysbiosis before adding in antihistamine agents).
- Addressing underlying GI imbalances is important in addressing histamine intolerance.
- Clinician Commentary
- Maddison’s case demonstrates a wonderful example of GI dysbiosis + inflammation leading to severe histamine intolerance, and how prioritizing GI first can lead to significant improvements in food/environmental reactivity. Using the patient’s response to treatment was key in my clinical decision making. For example, I let her response guide when it was best to stop the antimicrobial herbs, as well as whether or not to continue pursuing GI treatments versus antihistamine treatments. The patient and I believe limbic retraining will be a useful therapy, however she is not ready at this time. I will continue to support her and bring it up at subsequent visits.
Clinical Take Home Points
Clinical Review Purpose
- It’s common to hear about the importance of feeding the microbiome with prebiotics in order to improve one’s gut health.
- While this sounds good in theory, what does the evidence say about the clinical utility of prebiotics in improving IBS, IBS-C, constipation, or SIBO?
- Does the prebiotic type and dose matter?
- Note: we are specifically looking at prebiotics and not fiber. We acknowledge that there is an overlap here.
What Does The Evidence Suggest For IBS?
- While the totality of the evidence does NOT support the use of prebiotics for IBS, lower doses of guar gum and GOS have been shown to improve gas and bloating.
What Does The Evidence Suggest For IBS-C or Functional Constipation?
- There is a slight trend in the literature for lower dose GOS for improving functional constipation, but NOT inulin, FOS, or partially hydrolyzed guar gum. Prebiotics in general did not improve IBS-C.
What Does The Evidence Suggest For SIBO?
- There is a slight signal of benefit for prebiotics, specifically guar gum, when combined with antibiotics.
What Should I Do In Clinical Practice?
- The overall trend in the data suggests prebiotics as a whole are not useful for IBS, SIBO, or functional constipation.
- When treating IBS, SIBO, or functional constipation, we recommend starting with the therapies that have the most evidence and/or clinical validation, including:
- Diet (Paleo or Low FODMAP)
- Lifestyle (improving sleep, stress, and physical activity)
- Probiotics
- Gut healing nutrients (e.g. glutamine)
- Antimicrobials
- Elemental diet
- Immunoglobulins
- Consider trialing prebiotics like low dose GOS or guar gum as an end-phase treatment, not a first-line therapy.
Fiber/Prebiotics Overview
Before reviewing prebiotics and their effect on various GI symptoms, it’ll be helpful to have a quick refresher on the different types of fiber, prebiotics, and the difference between them.
- What is fiber (1)?
- Fiber is the part of the plant that is non-digestible (i.e. breakdown into smaller components) by human enzymes
- Fiber can be categorized into:
- Fermentable (e.g. oligosaccharides, inulin, pectin, resistant starch, etc.)
- Non-fermentable (e.g. cellulose, hemicellulose, psyllium husk)
- What are prebiotics (2)?
- A type of fiber that positively affects the host by selectively stimulating the growth of beneficial intestinal bacteria
- To further simplify this, fiber is defined by the structure of the compound, whereas prebiotics are defined by their function. As an example, cellulose is a type of fiber the human microbiome can NOT utilize, therefore it is not considered a prebiotic. However, the microbiome in cows is able to break down cellulose, thus making it a prebiotic. So while cellulose is structurally a type of fiber, since the human microbiome can’t utilize it, it doesn’t function as a prebiotic.
- The Venn diagram below is a useful illustration to demonstrate the main similarities and differences between prebiotics and fiber, as well as examples of each.
- The main types of prebiotics studied in the medical literature for IBS, SIBO and constipation include:
- Inulin
- Food sources: leeks, asparagus, onions, wheat, garlic, chicory, oats, soybeans, and Jerusalem artichokes (3)
- Fructo-oligosaccharodes (FOS)
- Food sources: onion, chicory, garlic, asparagus, banana and artichoke (4)
- Galacto-oligosaccharides (GOS)
- Food sources: legumes such as lentils, chickpeas and beans (5)
- Partially hydrolyzed guar gum
- No common food source, but commonly added to foods as a thickener
- Inulin
Are Prebiotics Clinically Useful for IBS?
- High-Level Overview
- Prebiotics in general do NOT lead to clinically meaningful improvements in global IBS symptoms.
- Supporting Research
- The best evidence (i.e. meta analysis and systematic reviews) does NOT support the use of prebiotics and irritable bowel syndrome.
- A 2019 systematic review and meta-analysis of 11 RCTs and 729 participants with IBS or functional GI disorders. Compared to placebo, prebiotics did NOT lead to improvements in:
- Abdominal pain
- Bloating
- Flatulence
- Quality of life
- The authors concluded “Prebiotics do not improve gastrointestinal symptoms or quality of life in patients with IBS or other FBDs, but they do increase bifidobacteria.”
- A 2020 systematic review and meta analysis including 3 studies on prebiotics (fructo-oligosaccharides, partially hydrolyzed guar gum) and 250 patients with IBS (IBS-D, IBS-C, IBS-M) found “there was NO significant effect of prebiotics on IBS symptoms”
- A 2019 systematic review and meta-analysis of 11 RCTs and 729 participants with IBS or functional GI disorders. Compared to placebo, prebiotics did NOT lead to improvements in:
- However, it’s important we understand these studies are drawing conclusions based on the combined data of different types of prebiotics and multiple subtypes of IBS. In fact, a majority of the studies in the 2019 meta-analysis were based on inulin. We want to make sure we look at the prebiotics individually and at different doses to ensure we get the most accurate data.
- The best evidence (i.e. meta analysis and systematic reviews) does NOT support the use of prebiotics and irritable bowel syndrome.
Does Prebiotic Type or Dose Matter for IBS?
- High-Level Overview
- While prebiotics as a whole do not improve IBS, lower doses (≤ 6 g/day) of GOS and guar gum improve some IBS symptoms, specifically gas and bloating. Inulin and FOS do not lead to any IBS symptomatic improvement.
- Supporting Research
- Prebiotic type and dose matters when treating IBS
- “Meta-analysis showed that prebiotics did not significantly impact integrative symptom scores, severity of abdominal pain, bloating, or flatulence. However, there was considerable heterogeneity in these symptom findings, which was explained in part by variations in prebiotic dose and type.”
- “For example, prebiotics at a dose of ≤6 g/d improved flatulence, but higher doses did not impact this or any other symptoms. Furthermore, Inulin significantly worsened flatulence, whereas GOS and guar gum significantly improved flatulence. This highlights the importance of considering prebiotic dose and type in both clinical nutrition practice and research (6)”
- Fructo-oligosaccharide and inulin prebiotics do NOT improve IBS symptoms
- FOS does not lead to improvements in IBS symptoms when given between doses of 5-20 grams. When comparing placebo versus FOS, 3 studies with a total of 175 patients found that there was either NO difference in symptomatic improvement, and one study found symptoms were better in the placebo group (7, 8, 9).
- 71 children with IBS were randomized to probiotics, synbiotics, or inulin (1.8 g/day). After 1 month, prebiotics did NOT lead to greater improvements in bloating, belching, abdominal fullness, defecation difficulty, or mucus in the stool (10).
- Galacto-oligosaccharides (GOS) and guar gum slightly improve gas and bloating, but no other IBS symptoms
- Guar gum improved gas and bloating at doses of 6 g/day, but no other IBS symptoms improved
- In a study of 108 IBS patients, “12 weeks of administration of 6 g/day of guar gum on the clinical symptoms of IBS patients revealed that guar gum produced a significant improvement on bloating and gasses symptoms of IBS patients compared to placebo.”
- However, guar gum did not lead to improvements in abdominal pain, IBS severity or overall quality of life (11)
- Low dose GOS improved gas and bloating, but no other IBS symptoms improved
- In a study of 44 patients with IBS, compared to placebo, both low and high dose GOS (3.5 g/day and 7 g/day) did NOT improve BM frequency, straining/urgency, abdominal pain, or quality of life.
- Low dose GOS improved flatulence and bloating, while higher dose worsened bloating (12).
- Guar gum improved gas and bloating at doses of 6 g/day, but no other IBS symptoms improved
- Prebiotic type and dose matters when treating IBS
Do Prebiotics Differentially Benefit IBS-C or Functional Constipation?
- High-Level Overview
- There is a slight trend in the literature for improving functional constipation with GOS, but NOT inulin, FOS or partially hydrolyzed guar gum. In general, prebiotics do not significantly improve IBS-C, although the number of studies included were very small.
- Supporting Research
- GOS may improve functional constipation greater than other prebiotics
- In a meta-analysis of 5 RCTs and 199 patients with functional constipation, compared to placebo, GOS led to the greatest improvement in stool frequency, ease of defecation and abdominal pain. Inulin-type prebiotics did not significantly improve constipation (13)
- 2 studies including 112 participants with functional constipation were randomized to placebo or partially hydrolyzed guar gum (5 g/day or 15g/day). NO improvement in constipation was observed between groups. However, one study did find treatment with guar gum led to fewer laxative medications needed (14, 15).
- FOS does NOT significantly improve constipation in IBS patients, however the sample sizes are very small
- 20 patients with IBS-C were randomized to placebo or FOS (5 g/day). After 1 month, FOS led to greater improvement in IBS symptom severity (-122 FOS vs -38 placebo), however these results were not statistically significant, likely due to low sample size (16).
- In this study of 7 patients with IBS-C, FOS (6 g/day) did NOT lead to greater improvements compared to placebo (17).
- GOS may improve functional constipation greater than other prebiotics
Are Prebiotics Clinically Useful For SIBO?
- High-Level Overview
- There is a slight signal of benefit for prebiotics (guar gum) and SIBO when combined with antibiotics. However, due to the lack of high quality studies (e.g. larger and placebo-controlled), it is difficult to recommend prebiotics to SIBO patients, especially when we have access to other well-researched and validated therapies for treating SIBO, including probiotics, the low FODMAP diet, and elemental dieting.
- Supporting Research
- Guar gum + rifaximin improves SIBO eradication rates but NOT symptoms
- 77 patients with SIBO based on a positive glucose breath test were randomized to either rifaximin alone (1,200 mg/day) or rifaximin + guar gum (5 g/day). After 10 days, rifaximin + guar gum led to greater eradication of SIBO (87% vs 62%), but NO difference in SIBO symptom scores. It’s important to mention this study was not placebo-controlled (18).
- 77 patients with SIBO based on a positive glucose breath test were randomized to either rifaximin alone (1,200 mg/day) or rifaximin + guar gum (5 g/day). After 10 days, rifaximin + guar gum led to greater eradication of SIBO (87% vs 62%), but NO difference in SIBO symptom scores. It’s important to mention this study was not placebo-controlled (18).
- Rifaximin followed by FOS did NOT lead to improved SIBO symptoms
- 40 patients with SIBO based on both a glucose and lactulose breath test were randomized to low dose rifaximin (400 mg/day) followed by FOS (2.5 g/day) or probiotics.
- After 6 months, both groups experienced symptomatic improvements (abdominal pain, flatulence, gas), but there was no significant difference in improvement with probiotics vs prebiotics. Unfortunately, no repeat breath testing was performed, so eradication rates cannot be compared. Also important to note is this study was not placebo-controlled. Note the low dose of rifaximin used, when normal doses are about 1,200 mg/day (19).
- Guar gum + rifaximin improves SIBO eradication rates but NOT symptoms
How This Changes Clinical Practice
Clinical Takeaways
- In general, prebiotics do NOT lead to clinically meaningful improvement for IBS, IBS-C, functional constipation or SIBO.
- However, there is a signal of benefit for using prebiotics in the following applications:
- Lower dose GOS (≤ 6 g/day) for improving functional constipation
- Guar gum and GOS for improving gas and bloating in IBS patients
- Guar gum + antimicrobials for increasing eradication rates of SIBO
- Before using prebiotics, we recommend starting with therapies that have been clinically shown to work, including:
- Diet (Paleo or low FODMAP)
- Lifestyle (improving sleep, stress and physical activity)
- Probiotics
- Gut healing nutrients (e.g. glutamine)
- Antimicrobials
- Elemental diet
- Immunoglobulins
Final Comments
- This review highlights an important principle: Mechanistic data supporting a theory doesn’t always equate to supportive outcome data. For example, this meta-analysis found that prebiotics increase bifidobacterium, a species that is low in IBS patients (20). In theory, it would make sense that if we give prebiotics to increase a species that is deficient in IBS, it should lead to better outcomes. However, this was not the case, as this meta-analysis found “Prebiotics do not improve gastrointestinal symptoms or QoL in patients with IBS.”
Is it okay to take antimicrobials with probiotics at the same time?
Listener asks:
Is it okay to take antimicrobials at the same time as probiotics?
Yes! The evidence suggests that probiotics alongside antimicrobials are more effective than antimicrobials alone. The most common objection to this is, “won’t the antimicrobials just kill the probiotics?” This is a logical thought, but the assumption here is probiotics only work if they are alive. However, this is not exactly how probiotics work, as probiotics exert their benefits in numerous ways that don’t require them to be alive. It’s important to understand 3 main points about probiotics:
- Probiotics have a variety of mechanisms in which they can improve the host’s GI tract that don’t require them to be alive. For example, various components of probiotics have been shown to:
- Improve the intestinal barrier (i.e. reducing leaky gut)
- Prevent pathogens from “sticking” to the intestinal wall
- Bolster the GI immune function
- Killed probiotics can still exert benefits on the host. For example, this systematic review and meta analysis of 40 studies and 3,913 people found that killed probiotics were similarly effective compared to live probiotics in 78% of the studies, and were actually more effective in 15% of the studies. This study of 137 patients with chronic diarrhea found killed probiotics were more effective at reducing diarrhea compared to live probiotics.
- Research suggests probiotics enhance the effectiveness of antimicrobials for various conditions, including H. Pylori and SIBO. The most relevant study to show this effect is a systematic review of 20,215 patients with H. pylori infections. Patients who took probiotics and antibiotics together had better results than patients who only took antibiotics. Another study on SIBO found that compared to antibiotics alone, antibiotics + probiotics led to a more than 2x increased effectiveness in SIBO eradication.
To summarize, probiotics make antimicrobials work more effectively, and they should be taken together. Taking them together means either at the same time for convenience, or simply taking probiotics a few hours away from antimicrobials if desired. This is a great example of why it’s so important to look at outcome data as opposed to making decisions based on speculation or theory. If you want to get more benefit from antimicrobials, use probiotics alongside them!