Iterative Care: Limbic Retraining and Supplementation for Mast Cell Activation Provide Remarkable Benefits
TREATING CLINICIAN: ROBERT ABBOTT, M.D.
Patient Summary: Ashley
- Overview Context:
- Ashley is a 35-year-old menstruating mother of 2 young children. She has a cheery demeanor, but has been experiencing severe episodes of reactivity involving a constellation of neurological and GI symptoms.
- Concerns and Goals
- The patient desires to better understand the etiology (yet determined) of these episodes, decreasing their frequency and severity.
- Initial Symptoms:
- Food Reactivity – extreme with multiple categories of foods
- Abdominal cramping, muscular spasms
- Vomiting
- Migraines
- Extreme fatigue
- Throat swelling with reflux
- Dizziness, lightheadedness, sensation of fainting, episodes of low blood pressure
- Loss of full limb function, bladder control
- Onset, Timeline, and History:
- 2015
- Started to experience mild elements of these symptoms after the birth of first child
- Episodes were most prominent after meals – could include flushing/hot flashes, nausea and at times, vomiting
- Began to follow dietary eliminations to try to identify triggers and causes
- 2015-2019
- Experienced symptoms during her second pregnancy, worsening muscle spasms
- Post-partum following her second child was quite challenging – increasing nausea
- Discovered thyroid nodules and eventually had left partial thyroidectomy and initiated medication 2019
- Felt symptoms were less pronounced for a period of 3 months following surgery
- Continued to use various dietary patterns: AIP, keto, and carnivore to try and address reactivity
- Experienced symptoms during her second pregnancy, worsening muscle spasms
- 2020
- Cholecystectomy, Nov 2020
- Experienced change in stool pattern following that eventually normalized
- Reports the need to still be mindful of fat intake
- Would utilize Benadryl multiple times daily to address reactivity
- Additionally prescribed Zanaflex that seemed to provide some benefit for decreased abdominal/muscular cramping
- Recognized symptom aggravation leading up to and during menses
- Cholecystectomy, Nov 2020
- April 2021
- Reported attempt to decrease Benadryl leading to severe symptoms, including neurologic and cardiac elements
- Reported an ER workup following episode being negative alongside previous negative findings, MRI, EEG
- Persists now with marked reactivity and a reliance on Benadryl
- Reported attempt to decrease Benadryl leading to severe symptoms, including neurologic and cardiac elements
- 2015
- Prior Diagnosis:
- Obesity
- Thyroid Nodules (removed with partial thyroidectomy)
- Medications:
- Benadryl 25 mg, 4-6x daily
- Prior Surgical History (if relevant)
- 2019 – Partial Thyroidectomy
- Nov 2020 – Cholecystectomy
- Treatment History Summary:
- Benadryl – decreases food reactivities, allows her to function
- Nature Throid – reported negative reaction
- Cholecystectomy – did not change abdominal cramping, suspects in some ways symptoms were worse after
- Moving out of previous water damaged home appeared to help
- Has implemented numerous dietary patterns, reports some benefits from removing common allergenic foods, following AIP
- Clinical Questions/Comments:
- Are the patient’s symptoms of immune and nervous system hyper-reactivity a result of environmental toxicity, previous mold exposure?
- Is her hyperreactivity severe enough that I will be limited in my ability to recommend various supplements, including gut-directed therapies?
- Is there any information (lab testing) I do not have that would be helpful to guide my treatment?
- Prognosis:
- It is somewhat difficult to discern given the nature of her hyperreactivity, but I expect over the course of 3-6 months we will see positive changes in her symptoms.
- Differential Dx
- Dietary & Lifestyle
- Dietary mismatch – restrictive dietary pattern
- Sedentarism – suboptimal movement pattern
- Limbic imbalance – symptoms of nervous and immune hyperreactivity
- Gastrointestinal
- Dysbiosis
- Histamine intolerant
- GI pathogen
- Bile Acid Diarrhea – History of Cholecystectomy
- Hormonal
- Female hormone imbalance – symptoms worse around menstruation
- Partial Thyroidectomy – no current replacement, negative reaction to NDT
- Nutritional
- Nutritional Deficiencies – very likely given dietary pattern
- Metabolic
- Insulin Resistance
- Dyslipidemia
- Obesity
- Other Considerations
- GI & physical
- Abdominal/pelvic adhesions – History of Cholecystectomy, 2 c-sections
- Hiatal Hernia – Obesity, symptoms of GERD at time
- Sleep
- Sleep disordered breathing
- Toxic
- MCAS – symptoms of histamine reactivity
- Mold exposure/illness – Hx of exposure
- Heavy metal toxicity
- GI & physical
- Dietary & Lifestyle
- Recommended Testing
- Urinary Mycotoxin Testing
- Clinical Decision Making
- Ashley has experienced significant hyperreactivity with neurologic symptoms. Given her extensive negative work-ups in the traditional medical setting, I feel her hyperreactivity is a manifestation of limbic system and immune reactivity with elements of mast cell activation in the setting of historical mycotoxin exposure and multiple stressors, including two pregnancies and two surgeries. The cholecystectomy may have further compromised her biliary tract and the capacity for the effective removal of toxins in stool.
- I would like to begin with a foundational diagnostic evaluation for urinary mycotoxins. We will have her start with some form of limbic retraining to hopefully decrease her hyperreactivity. She will also likely require some additional antihistamine and mast cell mitigation supports prior to the consideration of additional therapies, including gut directed treatment or GI binders.
- Treatment Hierarchy
- Limbic Retraining
- Urinary Mycotoxin Testing
- MCAS Supports
- Probiotics
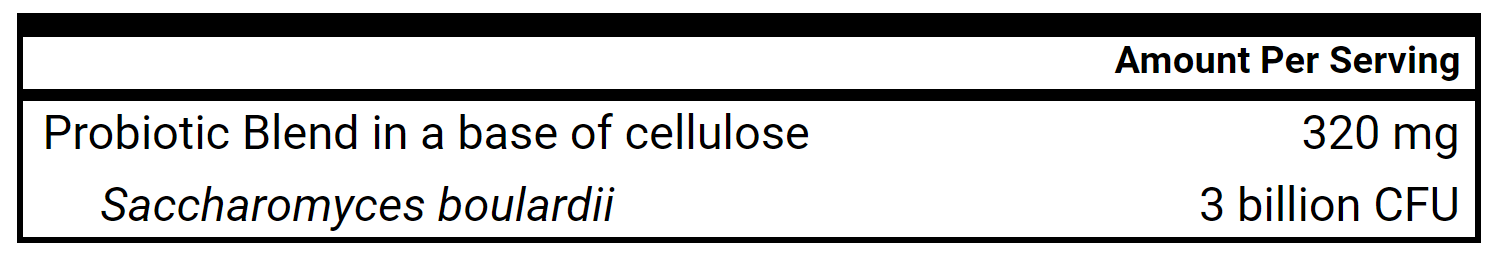
- S. boulardii
- Gut Barrier Support
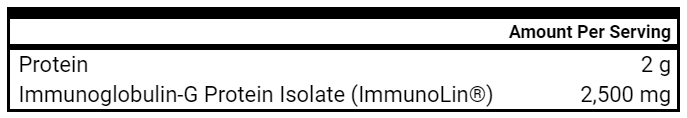
- Immunoglobulins
- GI Binders, Bile Acid Binders
- Nutritional Replacement Therapy
- Hybrid Elemental Diet
- Initial Treatment Recommendations
- Diet and Lifestyle
- Low Histamine Paleo
- Limbic Retraining Programs
- MCAS
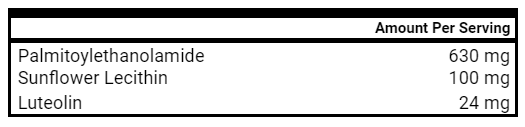
- PEA + Luteolin, 2-3 capsules 2x daily
- Flavonoids, 2-3 capsules, 2x daily
- Consider local Rx for Cromolyn with meals
- PEA + Luteolin, 2-3 capsules 2x daily
- Follow-up Plan
- 5 weeks
- Diet and Lifestyle
- Clinician Treatment Summary
- I am quite suspicious of previous mold toxicity as a driver of her symptoms and so have focused our initial testing efforts on urinary mycotoxins. While I would like to help improve the health of her gut, I am worried she will not be able to tolerate some of the GI-directed treatment and so will start first with limbic retraining and MCAS supports to see if I can calm things down enough to “access” her gut as another area for healing.
- Patient Self-Assessment
- Patient rates her health as 60-70/100
- She reports a 25% improvement since the first visit
- Her migraines and abdominal cramping/spasms have decreased
- She feels her mood has improved and she is able to see a larger picture, trajectory for healing
- She acknowledges continued food reactivity, but reports some capacity to eat more foods than previously
- She introduced the Flavonoids with positive benefits, but reports an extreme negative reaction to Cromolyn and likely negative response to PEA + Luteolin
- She began limbic retraining which has already been quite helpful, providing cognitive reframing
- Lab Results
- Urinary Mycotoxins
- Negative findings for all mycotoxins
- Urinary Mycotoxins
- Lab Interpretation and Diagnosis
- This is an interesting and somewhat unexpected finding. While all of the urinary mycotoxins were below thresholds for concern, this does not fully rule out this domain as a previous trigger and mediator for her current symptoms of hyperreactivity.
- Clinical Decision Making
- Ashley has responded very well to limbic retraining and the incorporation of Flavonoids. While she responded negatively to Cromolyn, she has rebounded really well. With the negative urinary mycotoxin testing findings and early positive responses to treatment, I will suggest continuing forward with an exploration of some gut-directed treatments with immunoglobulins and S. boulardii.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue Low Histamine Paleo
- Continue Limbic Retraining
- MCAS
- Continue flavonoids, 2-3 capsules, 2x daily
- GI
- Immunoglobulins – 0.5-1 scoop 2x daily, slow increase
- S. boulardii – 0.5-2 capsules, 1x daily, slow increase
- Immunoglobulins – 0.5-1 scoop 2x daily, slow increase
- Follow-up Plan
- 6-8 weeks
- Diet and Lifestyle
- Patient Self-Assessment
- The patient reports continued improvement since last visit, around 10%
- Overall, she feels she is 50% better than when we started working together
- No migraines since beginning treatment
- Abdominal muscle spasms and “nerve pain” continue to decrease
- Food reactions have greatly decreased overall, although some are still relatively severe
- Reported one severe episode involving some cooked potatoes with a small amount of added cheese – dairy causing significant reactivity
- Symptoms have not been as severe as previous around menstruation – she also recognizes the correlation between the quality of her diet and these symptoms
- She is requiring much less Benadryl than previous
- She introduced the S. boulardii with no clear negative reactivity
- She also introduced immunoglobulins that have clearly been helpful
- She has even been able to exercise and move more since our last session
- Clinical Decision Making
- Ashley has continued to progress with recovery from limbic reactivity and histamine reactivity despite a severe reaction (suspected to dairy) prior to our visit involving esophageal spasms. At this stage, I would like to continue our efforts with additional MCAS supports and zinc carnosine while ensuring no further intake of dairy. We also discussed the role of lower intensity cardio and resistance exercise to support her health.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue Low Histamine Paleo
- Continue Limbic Retraining
- Shared resources for incorporating cardiometabolic and resistance training into her daily routine
- Encouraged intake of some herbal teas, including Throat Coat and Chamomile
- MCAS
- Continue Neuroprotex, 2-3 capsules, 2x daily
- Add Quercetin Ascorbate Powder, goal 1 tsp daily
- GI
- Continue Immunoglobulins
- Continue S. boulardii
- Add Zinc Carnosine, goal 1 capsule, 2x daily
- Follow-up Plan
- 6-8 weeks
- Diet and Lifestyle
- Patient Self-Assessment
- The patient reports overall stagnation since the last visit
- She feels she has been in a constant mild flare since the last visit, reacting to some degree to even lower histamine foods
- With more time using the S. boulardii, she wonders if it could possibly now be aggravating
- Zinc carnosine and quercetin ascorbate appeared to aggravate nausea, although it is somewhat challenging to determine with overall baseline challenges the last 6 weeks
- Reports even some degree of reactivity to the herbal teas – chamomile and slippery elm
- Has not been able to further decrease her use of Benadryl
- Had been consuming more salmon recently which could have contributed to overall higher histamine intake as well
- Clinical Decision Making
- Ashley has been mildly flared since our last visit, with seemingly the biggest contributors being probiotics and regular fish consumption. We discussed trying to remove potential triggers for 7-10 days followed by retrials of Quercetin in capsule form, Vitamin C, L-Glutamine powder, and 3 mg of nightly melatonin. I also advised on ways to get lower histamine (flash frozen) salmon and ways to continue including certain animal proteins.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Discussed Vital Choice – flash frozen King Salmon
- MCAS
- Continue flavonoids, 2-3 capsules, 2x daily
- Add Quercetin 500 Ascorbate 1-2 capsules, 3x daily with meal
- Add Vitamin C, 1 capsule, 2x daily
- GI
- Continue Immunoglobulins
- Stop S. boulardii
- Stop and reintroduce Zinc Carnosine
- Add L-Glutamine, 1-3 tsp daily
- Melatonin 3 mg nightly (can help with lower esophageal sphincter alongside sleep)
- Follow-up Plan
- 6-8 weeks
- Diet and Lifestyle
- Patient Self-Assessment
- The patient reports maybe 5-10% further improvement since last visit, overall 50-60% better.
- She states that she had some clear negative reactions when she reintroduced zinc carnosine as well as vitamin C and L-Glutamine, describing elements of urinary burning and urgency.
- She can see more clearly that symptoms appear more prominent around ovulation, as well as menstruation
- Describes some bloating, distension, and abdominal pain
- Reiterates some previous concerns for endometriosis with negative findings
- She does positively report that she has been able to go a few stretches of time without Benadryl, which she has not been able to do for some time
- Utilized an alternative to flavonoids when it was out of stock with benefits
- Clinical Decision Making
- Ashley is still pushing through some reactions related to new supplementation and has been able to go without Benadryl on some occasions, which is remarkably encouraging. We discussed seeking to avoid any new supplementation at this time, to let things generally calm and give more time for the core diet, lifestyle, and tolerated supplements to provide benefit. While she is concerned she won’t be able to “heal her gut” given her inability to tolerate many of the GI supplements, I encouraged her by reminding her of the positive trajectory she is on that is, in and of itself, a reflection of improving gut health.
- Updated Treatment Recommendations
- MCAS
- Continue flavonoids, 2-3 capsules, 2x daily
- Continue Quercetin Ascorbate 1-2 capsules, 3x daily with meal
- GI
- Continue Immunoglobulins
- Continue Melatonin 3 mg nightly
- Follow-up Plan
- 8 weeks
- MCAS
- Patient Self-Assessment
- The patient reports her highest score for overall health 75/100 since we began working together.
- She describes 25% improvement from our last visit and overall 75% improvement.
- Less severe and frequent food reactions
- Less severe and much less frequent migraines
- Reports rare abdominal spasms/pain
- Reports that she went nearly 2 weeks without any use of Benadryl
- A sequence of increased emotional stress leading up to menstruation created a mild flare event
- Reiterates some previous concerns for endometriosis with negative findings
- Reports consuming a nourishing Thanksgiving meal without flares, and was even able to reintroduce a food she has not had in quite some time
- She reports a further realization to be focused on her Paleo lower histamine way of eating while also being mindful of certain fodmaps that appear to create reactivity
- Clinical Decision Making
- Ashley continues to make significant progress with decreasing reactivity and less need for Benadryl. Her main exacerbations of symptoms occur in the setting of increased stress, dietary indiscretion, and in relation to flux in female hormones. Given our work up to this point, I shared that we could consider exploring the use of some adaptogens, including L-Theanine and some female hormone adaptogens, that may help to mitigate some of her reactivity. I also shared that she could consider the use of DAO with meals to see if this allows her to further decrease Benadryl and expand her diet.
- Updated Treatment Recommendations
- Diet and Lifestyle
- No changes
- MCAS
- Continue Neuroprotex, 2-3 capsules, 2x daily
- Continue Quercetin 500 Ascorbate 1-2 capsules, 3x daily with meal
- Trial DAO, 1 capsule with meals
- GI
- Continue Immunoglobulins
- Continue Melatonin 3 mg nightly
- Adaptogens
- L-Theanine 100 mg, 1-2 capsules, 1-2x daily
- Estrogen Balancer and Progesterone Balancer, 20-30 drops 2x daily
- Follow-up Plan
- 8 weeks
- Diet and Lifestyle
Clinical Rule(s) and Final Clinician Comments
- Ashley’s case demonstrates the challenges we can face as clinicians caring for patients with significant neurologic and immune reactivity. Several treatments caused some degree of reactivity for Ashley, and it can be easy to get discouraged when this happens, but one must keep the big picture in mind and not lose heart!
- When patients are this reactive, I’ve found it most helpful to start with limbic retraining, and if indicated, supplementation to dampen down histamine and mast cell type responses. These therapies can often then allow you to begin gut-directed interventions that hold additional promise.
- Be patient. Sometimes in these types of cases, you have to take pauses in treatment when patients become overly reactive. Patience is key.
- When progress is stalled, avoid unnecessarily intricate and complex treatments in patients with increased reactivity. When in doubt, give more time for the body to heal and wait on introducing new elements.
Patient Summary: Paul
- Overview Context:
- Paul is a 31-year-old male with a history of recurrent diverticulitis treated with antibiotics and subsequent partial sigmoidectomy who continues with chronic abdominal pain, as well as food sensitivities and an alternating stool pattern.
- Concerns and Goals
- Paul would like to better understand the etiology of his abdominal pain and decrease the total burden of symptoms.
- Initial Symptoms:
- Abdominal Pain – Frequent and Severe
- Mostly postprandial
- Predominantly in all areas, except right lower quadrant
- Food intolerance – Frequent and Severe
- Constipation – Occasional and Mild
- Diarrhea – Occasional and Mild
- Abdominal Pain – Frequent and Severe
- Onset, Timeline, and History:
- 2020
- Paul reported 3 episodes of diverticulitis all treated with antibiotics
- At the time, his symptoms were predominantly in the left lower quadrant with accompanying severe diarrhea
- Following the third recurrence of diverticulitis, he had partial colonic (sigmoid) resection in August 2020
- January 2021
- While he noted some initial benefit from the surgery (98-99%), he eventually developed more diffuse abdominal pain, without the same previous irregular stool pattern associated with the diverticulitis
- He reported a colonoscopy and endoscopy with negative findings
- Paul engaged in an extended bone broth fast that helped resolve symptoms
- Following the fast, he was then able to eat a mixed diet with regular exercise
- August – October 2021
- He gradually began to consume more fiber that started to negatively impact motility and seemed to contribute to a return of pain starting around August 2021
- With the reemergence of abdominal pain, he pursued Clear Passage for visceral adhesive therapy with notable benefit in decreasing his abdominal pain
- He began additionally pursuing functional medicine care at this time
- His clinician suspected SIBO (empirical diagnosis) and so initiated a combination treatment
- Xifaxin for 14 days – noted some significant die off and overall health worsening during treatment, no improvement
- Candibactin AR and BR for 3 further weeks – with no additional benefit
- Alongside the combination antimicrobial treatments, he was started on Naltrexone (Low Dose) and Motegrity (Pruclaopride) intended to act as prokinetics.
- Around the end of Candibactin AR and BR treatments, he reports starting cycles of Clomid to support improved testosterone, as well as T3 for poor thyroid conversion.
- Throughout this time, he continued to experience food reactivity, bloating with early satiety that led to significant unwanted weight loss.
- He then sought to modify his diet further, finding that the semi-elemental diet seemed to cause the fewest postprandial symptoms.
- As he was still experiencing elements of pelvic pain, abdominal pain, irregular stools, and erectile dysfunction, he returned to Clear Passage where they confirmed his adhesions had been successfully addressed
- An additional Abdominal/Pelvic CT scan corroborated Clear Passage suggesting that there were no further clinical significant adhesions
- December 2021 – Present
- He began using some digestive enzymes and Betaine HCl without clear benefit
- He collected a stool sample (GI MAP) prior to our visit
- He was told from the results that it showed Candida and C. difficile and that he would need to consider Vancomycin and Fluconazole treatment
- With his reluctance and uncertainty about this treatment alongside continued pain and a restricted diet, he pursued care with us.
- 2020
- Prior Diagnosis:
- Diverticulitis, 2020
- Medications:
- Motegrity (Prucalopride) 1.5 mg – 2.0 mg
- Naltrexone 3.0 mg
- Liothyronine 12 mcg
- Clomid (Clomiphene) 25 mg every three days
- Anastrozole once weekly
- Prior Surgical History (if relevant)
- August 2020 – Partial Colectomy – portion of sigmoid colon
- Prior Testing Summary:
- November 2021 Blood Chemistry
- Grossly inappropriate and excessive testing that included:
- Beta Carotene, Vitamin A, Vitamin E, Total and Free Fractions of DHT, Total and Free Fractions PSA, Plasma and RBC Copper, RBC Zinc, MMA, IGFBP-2, Pregnenolone, IGF-1, Serum Iodine, Leptin, CoQ10, HHV-6, Ab, HSV-1 Ab, Full Thyroid Panel with reverse T3 and Thyroid Ab’s, AM Cortisol and Progesterone (amidst even more)
- Testosterone: 475
- Free Testosterone: 17.7 (Range: 8.7-25.1)
- Grossly inappropriate and excessive testing that included:
- January 2022 Urinary Mycotoxin (Self-administered)
- Equiv – Ochratoxin
- Equiv – Zearalenone
- +Trichothecene
- +Gliotoxin
- January 2022 GI MAP
- Pathogens: Positive for C. diff
- H. pylori: Negative
- Bacterial Dysbiosis: Moderate
- Fungi / Yeast: Candida spp. Elevated
- Intestinal Health:
- Elastase 567
- Calprotectin 31
- Zonulin 107.8
- November 2021 Blood Chemistry
- Differential Dx
- Dietary & Lifestyle
- Dietary mismatch – restricted diet
- Sedentarism – concern for further weight loss with additional exercise
- Poor sleep hygiene, timing or duration – goes to sleep late at night
- Gastrointestinal
- History of Partial Sigmoid Colectomy
- Excessive/Inappropriate Use of Prokinetics
- Dysbiosis
- Candida
- GI pathogen – C. difficile Carrier
- Hormonal
- Inappropriate exogenous hormone supplementation – Clomid and aromatase inhibitor
- Incorrect thyroid dx and/or unnecessary thyroid medication – T3
- Andropause male
- Nutritional
- Nutritional Deficiencies – overall restricted, inadequate dietary intake
- Electrolyte insufficient
- Metabolic
- Weight Loss
- Sarcopenia
- Other Considerations
- GI & physical
- Abdominal/pelvic adhesions – addressed with Clear Passage
- Pelvic floor disorder
- Sleep
- Need for sleep CBT?
- Infectious
- C. diff carrier
- Toxic
- Mold – + urinary mycotoxin profile
- Heavy metal toxicity?
- GI & physical
- Dietary & Lifestyle
- What went wrong?
- Most notable errors and concerns from his past treatment
- Excessive antibiotics perpetuated dysbiosis (possible reasons for Candida and C. diff appearing on his latest GI MAP
- Possibly premature surgical intervention that led to the development of adhesions, causing new symptoms and the need to pursue additional expensive, albeit helpful, medical care
- Excessive and inappropriate use of the antibiotic Rifaximin and herbal antimicrobials
- Markedly excessive blood testing (total cost likely close to $10,000 by estimates)
- Inappropriate prescription of Clomid
- Inappropriate prescription of Liothyronine (T3)
- Inappropriate suggestion of antibiotic and anti-fungal treatment based on literal GI MAP testing interpretation
- Most notable errors and concerns from his past treatment
- Clinician Comments
- Paul appears to have been significantly overtreated, overtested, and inappropriately diagnosed since his original diagnosis of diverticulitis in 2020.
- He has been “forced” to pursue additional costly treatment as a result of higher risk therapies that created new problems.
- He was recommended significantly excessive and inappropriate laboratory testing, and despite normal findings for thyroid function and testosterone, was provided multiple medications to improve things to “more optimal levels.”
- Given the nature of the recommended hormone treatments, titration and cessation is not straightforward, and will likely cause further (previously avoidable) suffering and challenge.
- The GI MAP test was inappropriately utilized, leading to the recommendation of likely further unnecessary and risky treatment.
- We have shared this case with you all to demonstrate, unfortunately, one of several examples we see in the clinic of well-intentioned, but misguided functional medicine care. Hormone replacement therapy (thyroid and sex hormone) appears to be increasing and this is leading to many unnecessary and inappropriate prescriptions. We must also be very careful in how we utilize and interpret stool testing and avoid unwarranted and risky treatments. We have spoken many times before about the dangers of over-testing – precise markers showing various nutrients and hormones can be alluring, but they rarely will actually change your clinical management. Be sure to prioritize tests that will change clinical management and with which you have a solid clinical (not just mechanistic) understanding.
Clinical Question
- Is metformin an effective therapy for Hashimoto’s Thyroiditis?
Functional Medicine “Bias”
- Metabolic health is an important contributor to chronic inflammatory disease. However, some suggest carbohydrate restriction in thyroid disease is contraindicated.
What Does The Evidence Actually Suggest?
- Metformin has been found to reduce both TPO and anti-thyroglobulin antibodies in populations of patients with Hashimoto’s Thyroiditis (HT) and subclinical hypothyroidism (SH) with insulin resistance.
What Should I Do In Clinical Practice?
- Addressing disturbances in metabolic health alongside gut, nutritional, and environmental contributors is likely to support improvements in thyroid health, including antibody levels in patients with HT
- Given the small nature of the meta-analysis examined here, and the risks, albeit small, associated with metformin use, clinicians may desire to focus their metabolic therapies first on lifestyle interventions including increasing nutrient density, lowering carbohydrate volume, increasing physical activity, and supporting weight loss (when appropriate) while also considering supplemental therapies such as berberine or medications such as metformin.
Primary Study Title
- Metformin reduces autoimmune antibody levels in patients with Hashimoto’s thyroiditis: A systematic review and meta-analysis
Intervention Details
- 3 observational studies (6 sub-observational cohorts) and 1 randomized, double-blind, placebo-controlled clinical trial
- 118 metformin treated patients
- 100/118 with subclinical hypothyroidism
- 75/118 with definitive Hashimoto’s Thyroiditis
- Treatment courses lasted between 3-6 months
- Patients were generally between age 40-50, 25-42% smokers, with borderline high blood pressure (132/87) with an overweight BMI (between 25-30 kg/m^2) and a significant degree of insulin resistance (HOMA-IR between 4-7)
- Statistically and clinically significant decrease in TPO Ab in those with HT, weighted mean difference of 177.61 IU/mL, 95% CI (43.48-311.75)
- Statistically and clinically significant decrease in TSH in those with HT, weighted mean difference of 1.25 μIU/mL, 95% CI (0.76–1.74)
- Statistically and clinically significant decrease in HOMA-IR – (measure of insulin resistance) in those with HT, weighted mean difference of 1.89, 95% CI (1.62-2.16)
Study Author’s Primary Conclusion
- “Overall, our study found for the first time that metformin can reduce autoimmune antibody levels in patients with SH and HT, especially TPOAb.”
Interesting Notes
- This was a relatively small meta-analysis of individuals with baseline TPO Ab’s generally between 1000-1500 and fairly significant insulin resistance.
- I would not consider the population studied in the meta-analysis reflective of the typical functional medicine patient. However, it does provide support, both clinical and mechanistic, to focus on improving a patient’s metabolic health as a way (access point) to address disease activity in patients with HT.
- Berberine has been found through several systematic reviews and meta-analyses to be helpful (both alone and in combination) for addressing elements of metabolic dysfunction in patients with dyslipidemia and insulin resistance, making it a viable natural alternative to metformin.
Secondary Study Title
Final Comments
- Alongside gut-based interventions, consider addressing disturbances of metabolic health in patients with autoimmune thyroiditis.
Clinical Question
- Can Vitamin D and Omega 3 fats prevent the development of symptomatic autoimmune disease?
Functional Medicine “Bias”
- Vitamin D and Omega 3’s are popular supplements that can benefit patients with chronic inflammatory disease, and may even be used to prevent the development of certain chronic diseases.
What Does The Evidence Actually Suggest?
- Vitamin D supplementation at 2,000 IU daily in older adults (~65 years old) without autoimmune disease may decrease the risk for the development of diagnosed autoimmune disease when taken over a period of five years.
- “Low” dose omega 3 supplementation (640 mg EPA, 380 mg DHA daily) in isolation DOES NOT appear to lower the incidence of autoimmune disease in an older population.
What Should I Do In Clinical Practice?
- Consider the use of Vitamin D supplementation (in concert with other fat soluble vitamins A, E, and K) in older patients at risk for chronic inflammatory or immune mediated disease
- Consider the use of Omega 3’s alongside increased fatty fish intake in older patients with additional risk factors for cardiovascular disease
Primary Study Titles
- Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial
- Effect of omega-3 fatty acids on cardiovascular outcomes: A systematic review and meta-analysis
Intervention Details
- 25,871 people, average age 67.1 years, 71% white, 51% female were followed for ~5 years
- 4555 participants were noted with autoimmune disease at baseline (18%)
- Patients were randomized to get either
- Vitamin D 2,000 IU daily
- 460 mg EPA, 380 mg DHA daily
- Vitamin D or Omega 3 placebos
- Researchers collected data at 6 months and every year thereafter via a questionnaire to patients asking about new onset autoimmune disease
- If patients reported a new diagnosis, study physicians reviewed medical records to confirm the diagnosis
Study Author’s Primary Conclusion
- “This study of more than 25 000 older adults in the US provides evidence that daily supplementation with 2000 IU/day vitamin D or a combination of vitamin D and omega 3 fatty acids for five years reduces autoimmune disease incidence, with more pronounced effects found after two years of supplementation.”
Interesting Notes and Final Comments
- There were only 123 confirmed cases of autoimmune disease in the Vitamin D treatment group, and 155 in the placebo arm. When compared statistically, the p-value for statistical significance was right at 0.05. The upper limit of the confidence interval for the hazard ratio was also 0.99
- Taken together, the 2,000 IU Vitamin D treatment is not providing a huge therapeutic effect
- Autoimmune disease incidence in older populations may likely be less than other cohorts (ex. younger women)
- It is possible Vitamin D could provide a larger protective effect in populations at higher risk for the development of autoimmune disease.
- The methodological approach used (relying on a patient report of an autoimmune diagnosis followed by medical confirmation) may have led to overall underreporting of disease.
- If this occurred equally in placebo and treatment groups, this should not have affected the statistical comparison of the groups, but it may have diminished the ability of the study to detect a more prominent therapeutic effect of the Vitamin D.
What Do You Do With Patient Provided Lab Results You Do Not Normally Run?
Listener asks:
What do you do with patient provided lab results you do not normally run?
This is a commonly encountered scenario in functional medicine with its plethora of clinical testing paradigms. A typical initial response when faced with lab results from an uncommonly performed test may be one of curious inquiry – let me see if I can figure this out! There is some danger here, however, as test results based on some discernible mechanistic/physiological principles often cannot be interpreted well alongside a patient’s clinical presentation.
For example, with certain tests that you commonly run, you will likely have observed and learned trends for abnormalities of less or no clinical significance. While flagged “high or abnormal,” you learned to ignore certain signals to discern what is of true clinical meaning. Often our ability to best use a test is dependent on our ability to know its shortcomings and common findings so that we can better observe signals from noise. Simply going off a lab’s designated normal range or your researched understanding of a physiological pathway may give you a false sense of fluency with a certain test.
In our opinion, it is best in these situations to share with the patient your lack of familiarity with the test and avoid interpreting a finding that is clinically irrelevant or even inaccurate.