Patient Summary:
Overview Context:
- Julianna is a pleasant 51-year-old post-menopausal female with lifelong food intolerances. She has been diagnosed with ulcerative colitis. While an initial steroid treatment has been helpful, she is seeking support in addressing ongoing GI symptoms and excessive food restriction.
Symptoms and Concerns
- Chief Complaints:
- Bloating
- Gas
- Joint pain – associated with dairy consumption
- Abdominal cramping – now resolving
- Migraines
- Excessive food restriction – underweight, sarcopenic
- Other Symptoms:
- Diarrhea – improving (has 1 bowel movement daily now)
- Onset, Timeline and History:
- July 2020 – Last menstrual cycle
- May 2021 – Began inappropriate HRT (pellet) and thyroid medications
- Reports symptoms primarily of constipation began at this time
- No longer taking thyroid replacement given reactions
- August 2021 – Follow up testing shows elevated testosterone; reports bloody stools beginning to develop at this time
- September 2021 – Went to ER where she received Abd/Pelvis CT showing suspected inflammatory colitis
- Started 2 antibiotics – really negative reactions (vomiting and diarrhea)
- Reports another ER visit where the physician suggested ulcerative colitis
- She was given Prednisone IV followed by an oral course
- Some abdominal cramping and diarrhea improved after prednisone
Past Medical History
- Prior Diagnosis:
- Ulcerative Colitis diagnosed via abdominal CT scan and symptoms
- Medications:
- None at this time
Prior Testing and Treatment History
- Prior Testing Summary:
- Blood Chemistry Oct 2020 (before HRT)
- Testosterone <3
- TSH: 2.4
- Free T3: 2.9
- Estradiol <5
- hs-CRP: 0.23
- WBC: 3.8, Neutrophils: 48%
- AST: 66, Albumin 5.2
- Blood Chemistry May 2021 (on HRT pellets)
- Total Testosterone: 436
- GI Effects July 2021
- Elastase: 137
- Calprotectin: 67
- Negative Blood
- Negative pathogens
- Abd CT Scan September 2021
- “Diffuse descending, colonic sigmoid wall mucosal thickening”
- Suggestive of colitis – infectious vs. inflammatory vs. ulcerative
- “Diffuse descending, colonic sigmoid wall mucosal thickening”
- Note: No thyroid tests after starting thyroid medication
- Blood Chemistry Oct 2020 (before HRT)
- Previous Diets:
- Now following more restrictive lower histamine type ancestral diet with intermittent period of fasting
- Previous Treatments:
- Thyroid medication (unwarranted, see labs above)
- HRT – pellet testosterone (now with markedly excessive testosterone)
- Oral prednisone (decreasing bloating, gas, abdominal pain)
- Flagyl (strong negative reactions – nausea and vomiting)
Initial Impression
- Clinical questions:
- Does the patient actually have UC? This onset later in life would be abnormal.
- Are part of the patient’s symptoms related to inappropriate thyroid and hormone replacement therapy?
- Do we need to repeat stool testing to be able to support her continued gut healing?
- Do we need to provide pancreatic enzymes given her low elastase levels?
- Clinical Commentary:
- The patient has unfortunately been overdosed on testosterone and previously given unnecessary thyroid medication (no longer taking). While she has not done pellet therapy recently, her testosterone levels remain high and will stay that way for some weeks.
- She has not really done many gut-based therapies, so despite the significant reactivity, we may be able to support her gut healing that will also allow for calming immune/food reactivity and dietary expansion.
- Outside of gut and nervous system based supports, she will likely also benefit from other tools including mast cell/histamine intolerance type supplementation and limbic retraining.
- Recommended Testing
- None
- Initial Treatment Recommendations
- Diet:
- Paleo diet
- Partial Elemental Diet for 1 meal daily or as desired
- Lifestyle:
- Daily meditation
- Treatment:
- GI:
- S. boulardii, soil-based probiotics, lacto-bifido probiotic blend
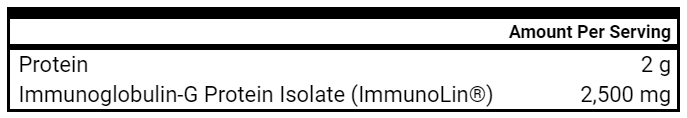
- Immunoglobulins
- L-glutamine
- S. boulardii, soil-based probiotics, lacto-bifido probiotic blend
- Hormone/NRT:
- Adrenal Herbal Formula
- L-Theanine and GABA
- Amino Acid/Magnesium/Herbal blend
- Adrenal Herbal Formula
- GI:
- Follow up: 6 weeks
- Diet:
- Clinician Summary
- We decided to pursue a more intensive period of treatment focused mainly on supportive gut based interventions and adaptogenic supports for a burdened nervous system.
- Given concerns for her underweight nature and maldigestion/malabsorption, I suggest a meal replacement with the Elemental Heal hoping this can alleviate some food fear, simplify things, and get her some needed nutrition.
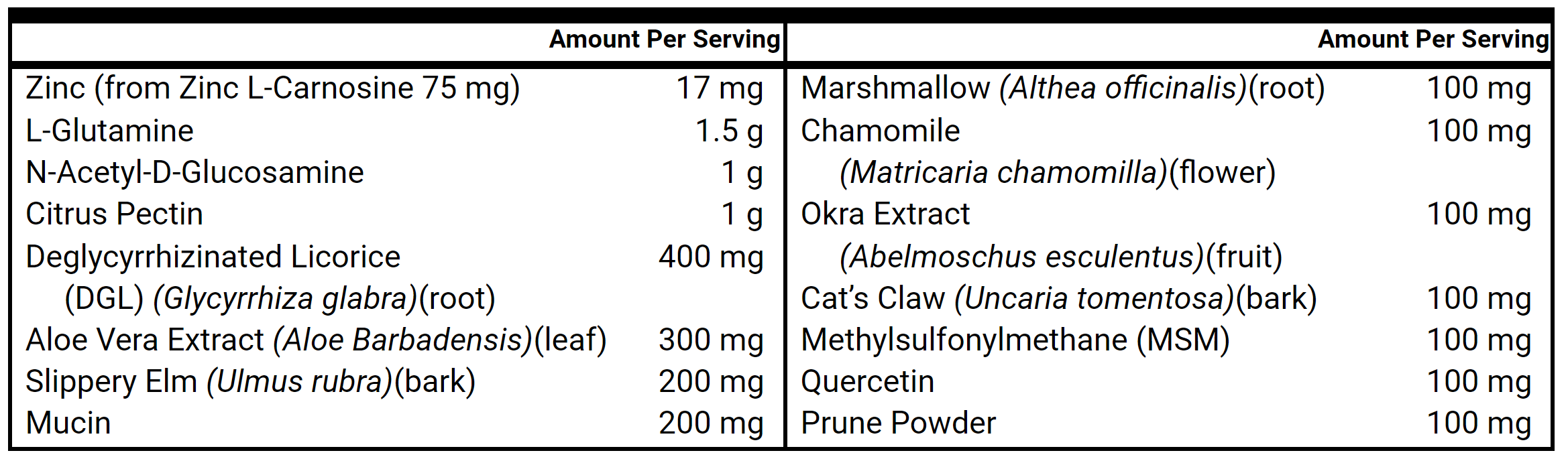
- Regarding the gut supports, I am approaching this more intensively – combining the immunoglobulins with additional L-Glutamine to go with the triple probiotics. I commonly take this approach with more reactive IBD patients or patients with more concerning colitis/bowel inflammation.
- Regarding the adaptogens, I have seen encouraging success with the use of L-Theanine alongside magnesium and other adaptogenic/herbal blends. Rather than try to force several nutritional supplements that may not be absorbed or needed, we will focus instead on nervous system support alongside the gut.
- Subjective Assessment
- Current Symptoms:
- Improved: Bloating, abdominal pain, “overall GI inflammation”
- Same: Food reactivity
- Worse: None
- Treatment Response:
- Probiotics – helpful
- L-theanine – helpful for sleep
- Adaptogenic herbs – no clear benefit
- Elemental diet – some reactivity perhaps from Stevia?
- Notes:
- She implement the probiotics but did not yet start immunoglobulins or the L-Glutamine yet
- Has not resumed HRT pellets or other hormone-based treatment
- Current Symptoms:
- Impression:
- She is encouragingly on a positive trajectory. We discuss the utility of adding the immunoglobulins and glutamine to see if this can further normalize her stools and decrease food reactivity. We will not try to reintroduce Elemental Heal at this time.
- Given her past abnormal labs (testosterone, CBC, CMP – liver enzymes), I would like to follow-up on these while simultaneously checking some markers of systemic inflammation and nutritional status.
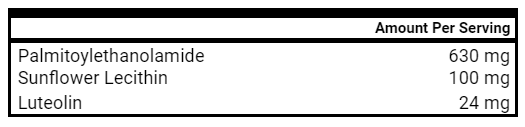
- Her GI symptoms are often aggravated by food. We discussed that while she does not have typical symptoms of histamine intolerance or allergic reactivity, that it may be worth exploring supplementation that can decrease histamine in the gut or decrease overall mast cell reactivity.
- Updated Treatment Recommendations
- New Treatment:
- GI:
- Continue triple probiotics
- Introduce Immunoglobulins, and L-glutamine.
- Hormone/NRT
- Continue theanine and melatonin as needed given apparent benefit, stop adaptogens as desired
- MCAS
- Quercetin
- DAO
- Quercetin
- GI:
- Labs:
- CBC with Diff
- CMP, GGT, Uric Acid
- CK, hs-CRP
- Vit D, B12, Folate, Homocysteine
- Followup: 6 weeks
- New Treatment:
- Subjective Assessment
- Current Symptoms:
- Improved: Bloating, abdominal pain stool pattern, Food reactivity (histamine intolerance), sleep
- Same: joint pain – in knees
- Worse: None
- Treatment Response:
- Immunoglobulins & Glutamine – strong positive response
- DAO & Quercetin – less food reactions / histamine intolerance
- Theanine & Melatonin (self prescribed) – more improvement in sleep
- Notes:
- The patient reports health now up to 95%
- 50% improvement since beginning to work together
- Bloating has continued to decrease and she feels less inflamed in her abdomen
- Her stool frequency and pattern have improved
- “I’m feeling good and more confident that I can address my food sensitivities.”
- Acknowledges some longer standing knee pain that is challenging to her
- The patient reports health now up to 95%
- Current Symptoms:
- Lab Results
- WBC: 3.7, Normal Diff
- Hgb: 14.7
- Albumin: 5.2
- AST: 45
- ALT: 13
- B12: 900
- Folate: 16.1
- Testosterone: 109.2
- Vit D: 90.5
- hs-CRP: 0.35
- Homocysteine: 8.5
- CK: 92
- Lab Interpretation and Diagnosis
- Her testosterone levels are slowly declining from the peak in 2021.
- She still maintains a high-normal albumin (suspected at least in part a reaction to testosterone) as well as AST.
- Nutritionally, she appears well. CK and hs-CRP are not elevated. Vitamin D is higher than is likely necessary.
- Updated Treatment Recommendations
- New Treatment:
- Continue previous supplements supports
- Decrease outside recommended Vitamin D use given high normal levels
- Explore introduction of fermented foods in lower volume
- Bloodwork (in 8 weeks):
- CBC with diff, CMP, GGT, Total Testosterone, Vitamin D
- Follow up: 8-10 weeks
- New Treatment:
- Subjective Assessment
- Current Symptoms:
- Maintained Improved: bloating, histamine intolerance, food intolerances.
- Same: knee pain
- Worse: NA
- Notes:
- Reports maintained improvements and is following an expanded personalized ancestral template (but still mindful of some higher FODMAPs and higher histamine foods)
- While she has some anxiety about recurrence of colitis, she continues to feel much less neurotic around food and calmer in general
- She continues to use immunoglobulins, L-Glutamine and probiotics most days alongside theanine. Does not require DAO now. She prefers to take digestive enzymes with her meals.
- Current Symptoms:
- Lab Results
- WBC: 3.9, Lymph 43%
- Albumin: 5.1
- AST: 55
- ALT: 16
- GGT: 8
- Testosterone: 37.1
- Vit D: 74.4
- Impression:
- Juliana is doing much better than when we began work in October 2021 (Now May 2022).
- Her testosterone has finally normalized and both her nervous system and immune system are less reactive.
- She has expanded her diet and has a much healthier gut. She feels confident in her way of eating. It will still be helpful to monitor her slightly elevated albumin and AST over time.
- Updated Treatment Recommendations
- New Treatment:
- Continue to modify and expand dietary regimen as desired.
- Explore discontinuation of enzymes; resume if needed.
- Maintain L-glutamine, Immunoglobulins, adaptogens and MCAS supplementation as she desires
- Follow up: 4-5 months or sooner if needed
- New Treatment:
Take Home Points
- Highlighted Clinical Rules and Commentary
- Functional Medicine is foundationally a diet and lifestyle based approach and should start with the least invasive treatments first such as diet, lifestyle, and gut health.
- Further dietary restriction may not be necessary in someone with an already restricted diet and/or fear around food. Correcting gut imbalances can often improve food sensitivities.
- Exhaust low risk, empirically informed treatments prior to the consideration of testing to guide/modify treatment recommendations.
- Remember that lab tests only tell about 25% of the whole clinical picture. Good history taking and assessment of prior treatment response supplies 75% of the information needed to make informed treatment decisions.
- Treat diet, lifestyle and gut health before supporting female hormones and thyroid imbalances.
- Our patient was likely negatively affected by previous unnecessary HRT
- Functional Medicine is foundationally a diet and lifestyle based approach and should start with the least invasive treatments first such as diet, lifestyle, and gut health.
Patient Summary:
Overview Context:
- Karen is a very pleasant 76-year-old female who is seeking guidance for her ongoing lifelong GI symptoms and histamine issues.
Symptoms and Concerns
- Chief Complaints:
- Heartburn
- Sharp pain in stomach
- Postprandial tachycardia, nausea, lightheadedness, chills, flushing, hot flashes
- Other Symptoms:
- Recently mild constipation, overall normal BM’s
- Denies itchy ears, runny nose, more traditional allergic symptoms
- Onset, Timeline and History:
- 1970s
- Suspected food poisoning
- Eventually developed reflux, abdominal pain
- Some reactivity to certain supplements
- 1990s
- Diagnosed with Hashimoto’s Thyroiditis
- Used Elimination diet with some improvement of symptoms
- 2020
- Breath test positive for SIBO
- Followed traditional Rx SIBO treatment followed by herbal antimicrobials
- Nov 2021 – Present
- Worsening GI symptoms
- Tried previous herbal antimicrobials and unable to tolerate
- Episodes of significant reactivity
- Fluoride (dental)
- Eye drops
- Reports worse on empty stomach
- 1970s
Past Medical History
- Prior Diagnosis:
- Hypothyroid/Hashimotos
- Hyperlipidemia
- Food allergies
- GERD
- Barrett Esophagus
- Kidney stone
- Medications:
- NP Thyroid 60 mg (takes with food)
- Benadryl PRN
Prior Testing and Treatment History
- Prior Testing Summary:
- April 2021 Blood Chemistry (on NP Thyroid 60 mg)
- TG Abs: 786
- TPO Abs: 214
- TSH: 5.23
- Free T4: 0.73
- Free T3: 3.1
- July 2021 Blood Chemistry
- ANA: 1:40
- RF: 15 (nl)
- SCr: 1.02
- eGFR: 54
- Hgb: 15.1
- CRP: 0.1
- ESR: 20
- TC: 320, HDL: 65, LDL: 238, Trigs: 85
- April 2021 Blood Chemistry (on NP Thyroid 60 mg)
- Previous Diets:
- Low FODMAP – helpful
- Continues to mostly remove gluten, dairy and is mindful of total carbohydrate intake
- Previous Treatments:
- Benadryl – helps when reactivity is more severe
- DAO – helpful for reactivity
- Aloe and Ginger – helpful for GI symptoms
- Herbal antimicrobials – negative reactivity – cannot tolerate
Initial Impression
- Clinical Questions:
- To what degree will the patient require treatment outside of the gut to help her reactivity?
- What kind of dietary approach is best suited for her given the reactivity and gut symptoms?
- Do I need any testing to help her?
- Prognosis:
- At this stage, I recognize it may take some time to support her given the long-standing nature of symptoms and their more reactive nature, but I am still optimistic. I am suspecting that she will likely require MCAS support, limbic retraining alongside supportive GI treatments to see more enduring and positive changes.
- Recommended Testing
- None
- Initial Treatment Recommendations
- Diet:
- Maintain existing dietary regimen or transition to Paleo low histamine
- Use whey-free Elemental Diet to replace 1 meal on most days for 2-4 weeks
- Lifestyle:
- Begin Limbic retraining
- Treatment:
- GI:
- S. boulardii
- Immunoglobulins (aiming for 1 scoop – wanting to avoid worsening constipation)
- Gut Healing Nutrients
- S. boulardii
- MCAS:
- Palmitoylethanolamide (PEA) with Luteolin
- Palmitoylethanolamide (PEA) with Luteolin
- GI:
- Follow up: 5-6 weeks.
- I also encouraged a visit with the nutritionist before our next follow-up to get more targeted support for her diet given her history.
- Diet:
- Clinician Summary
- Our primary goals are to decrease food reactivity, decrease symptoms of reflux/GERD, and allow for greater dietary expansion as time goes on.
- My primary pillar focus areas are immune reactivity (histamine focus), gut dysbiosis, limbic reactivity and recognizing her baseline autoimmune thyroid condition. I suspect that histamine intolerance may be driving both gut symptoms and some of the post-prandial reactivity.
- Her past labs do indeed show signs of autoimmunity and overall systemic inflammation as well as suboptimally high TSH (despite medication). I will keep in mind her baseline kidney function may be slightly below goal. While she may require more thyroid medication in the future, this would likely be aggravating to her symptoms currently and likely unnecessary if we can heal her gut and decrease over immune activation.
- Subjective Assessment
- Current Symptoms:
- Improved: Resolution of heartburn & abdominal pain, decreased heart racing, lightheadedness and dizziness, sleep
- Same: Constipation (mild)
- Worse: None
- Notes:
- No reactivity to supplements noted
- Reports an unexpected rapid treatment response rating a 70% improvement in 6 weeks and her health around 70-100.
- She attributes improvement to gut-based therapies and MCAS support (PEA, luteolin)
- Current Symptoms:
- Impression:
- Karen has experienced about 70% improvement since our first visit stating that heartburn, bloating, abdominal pain and sleep have all improved.
- She reports some degree of continued constipation and carb cravings and is wondering how we will seek to continue to address what she views as symptoms connected to SIBO.
- I feel that we can see some continued improvements with the current treatments and give more time to explore introducing higher histamine foods and using DAO with those meals as she desires.
- I do not think it is necessary to do a more comprehensive herbal antimicrobial regimen, but suggest a low dose oregano oil trial that may help determine if these treatments may be helpful.
- Updated Treatment Recommendations
- New Treatment:
- Continue to use a Hybrid Elemental approach while exploring introducing moderate histamine foods as tolerated
- GI:
- Continue S. boulardii and Gut Healing Nutrients
- Add Vitamin C + Bioflavonoids (this could be helpful for both stool frequency and constipation, practically it mixes well with the gut repair nutrients)
- Add low dose Oregano oil
- MCAS:
- Continue Palmitoylethanolamide (PEA) with Luteolin
- Add DAO
- Follow up: 5-6 weeks
- New Treatment:
- Subjective Assessment
- Current Symptoms:
- Improved: Constipation
- Worse: Burping and Headaches (temporary with oregano oil, now resolved)
- Treatment Response:
- Oregano oil – Burping and Headaches began after 3 weeks taking oregano oil; she ceased taking supplement and symptoms subsided
- Notes:
- Karen reports an 80% overall improvement in symptoms and an additional 5% improvement since our last visit.
- Current Symptoms:
- Impression:
- She has maintained improvements in constipation and overall decreased food reactivity. We will keep her supportive GI supplement unchanged and have her consider further dietary expansion.
- Given her positive response, I have now recommended some comprehensive labwork to follow up on her thyroid function as well as other areas of concern including her thyroid antibodies, elevated ESR, elevated lipoproteins, basic blood chemistry and nutritional markers.
- Updated Treatment Recommendations
- New Treatment:
- Expand foods as desired, using DAO as desired for higher histamine reintroductions.
- Consider adding a protein powder to the diet
- Blood Chemistry:
- CBC with Diff, CMP,
- Vitamin D, Iron Profile, Homocysteine
- Lipid Panel, Fasting Insulin
- TSH, Free T4, Free T3, TPO, TGA
- ESR, hs-CRP
- Follow up: 6 weeks or sooner if needed
- New Treatment:
Take Home Points
- Highlighted Clinical Rules
- Treat diet, lifestyle, and gut health before thyroid imbalances.
- Low thyroid symptoms are often attributed to GI imbalances.
- Give time for healing before adding new treatments.
- Consider making changes slower in patients who seem to be “sensitive” or have a history of reactivity
- At the onset of supplement utilization, provide the patient with a tentative timeline for a supplements use and update the patient as treatment progresses
- Consider pushing further into therapies that have a clear positive signal as compared to adding new therapies (e.g. doubling dose of probiotics before adding antimicrobials).
- Treat diet, lifestyle, and gut health before thyroid imbalances.
- Clinician Commentary:
- Given the postprandial tachycardia and symptoms of hyper-reactivity, it was NOT prudent to simply increase her medication despite the patient currently taking thyroid medication with a TSH between 4.5-7. This could have actually made things worse. Instead, we chose to focus on her gut health and decreasing reactivity, and then re-evaluate thyroid function AFTER these treatments.
- Our patient ended up not needing:
- Antimicrobials to improve her GI symptoms – despite a past history of SIBO
- No change in thyroid medication to feel better – her GI was most likely contributing to her symptoms
- We found a core of supportive GI supplements and histamine mitigating supports that can be maintained or tweaked as needed moving forward. Once a positive signal was obtained, we leaned into these treatments more and avoided higher risk treatments and novelty bias.
Clinical Take Home Points
Study Purpose
- Can you get the same health benefit by being a “Weekend Warrior” (exercising just on the weekends) compared to exercising more frequently?
What Does The Evidence Suggest?
- “Weekend Warriors” have nearly the same or identical benefits and health outcomes (i.e. all-cause mortality, cardiovascular mortality, cancer mortality) when compared to those who exercise more frequently.
- However, those with more risk factors (hypertension, diabetes) may need to exercise more frequently to get the most benefit.
What Should I Do In Clinical Practice?
- For patients who are extremely busy, you can encourage them to exercise vigorously 1-2x/wk to achieve similar results as more frequent exercise.
| All-cause mortality | Cardiovascular disease mortality | Cancer mortality | Notes | |
| Study 1 | 60-90% reduction | Similar reductions in Weekend Warriors vs more frequent bouts of training | ||
| Study 2 | 30% reduction | 40% reduction | 18% reduction | Weekend Warriors exercised vigorously 300 min/week |
| Study 3 | • No reduction • Those with NO risk factors had 59% reduction |
Risk factors = smoking, overweight, hypertension, dyslipidemia | ||
| Study 4 | 31% reduction |
Study 1 Details
Title: Physical Activity Patterns and Mortality:The Weekend Warrior and Activity Bouts
Methods
- 3,438 participants, 40+ years old, from NHANES cohort
- Used accelerometer to assess moderate-to-vigorous physical activity (MVPA)
- ‘Weekend Warriors’ = majority of their activity on only one or two days a week
- Followed x77 months
Results
- More weekly movement = lower mortality
- “Compared to participants with <37.5 minutes of MVPA per week, those with greater amounts of activity had a 60–69% mortality rate reduction after adjusting for relevant covariable.”
- Benefits were seen regardless of exercise frequency
- “Similar risk reductions were found when contrasting weekend warriors with those who were more frequently active.”
- “Similar risk reductions were found when contrasting weekend warriors with those who were more frequently active.”
Authors’ Conclusions
- “We examined the ‘weekend warrior’, finding that those participants who performed a majority of their MVPA on only one or two days, had similar mortality rate reduction as those who spread out their activity over more days during the week.”
Interesting Notes
- From the graphic above, the initial dip in all-cause mortality is at 75 minutes/week of exercise – this is very practical for most. After this point, there is not much more benefit seen when going from 100 to 500 minutes of exercise per week.
Study 2 Details
Methods
- Prospective study of 63,591 participants, 40+ years old
- Physical activity defined as:
- “Inactive” (no moderate- or vigorous-intensity activities)
- “Insufficiently active” (<150 min/wk in moderate-intensity and <75 min/wk in vigorous-intensity activities)
- “Weekend warrior” ( ≥150 min/wk in moderate-intensity or ≥75 min/wk in vigorous-intensity activities from 1 or 2 sessions)
- “Regularly active” (reporting ≥150 min/wk in moderate-intensity or ≥75 min/wk in vigorous-intensity activities from ≥3 sessions)
- Followed x18 years
Results
- Any amount of movement reduced all-cause mortality, cardiovascular mortality, and cancer mortality.
- Compared with the inactive participants, the hazard ratio (HR) for all-cause mortality:
- Insufficiently active: 0.66
- Weekend warrior: 0.70
- Regularly active: 0.65
- Compared with the inactive participants, the hazard ratio (HR) for cardiovascular disease mortality:
- Insufficiently active: 0.60
- Weekend warrior: 0.60
- Regularly active: 0.59
- Compared with the inactive participants, the hazard ratio (HR) for cancer mortality:
- Insufficiently active: 0.83
- Weekend warrior: 0.82
- Regularly active: 0.79
- Compared with the inactive participants, the hazard ratio (HR) for all-cause mortality:
Authors’ Conclusions
- “One of the most striking findings in the present study was that 1 or 2 sessions per week of moderate- or vigorous-intensity leisure time physical activity was sufficient to reduce all-cause, CVD, and cancer mortality risks regardless of adherence to prevailing physical activity guidelines.”
Interesting Notes
- “The mean time spent in moderate- or vigorous-intensity physical activity was approximately 300 min/wk for weekend warriors and approximately 450 min/wk in the regularly active participants”
- However, “the proportion of vigorous-intensity physical activity was higher in weekend warriors than the regularly active participants”
- This means that if you are going to be a “Weekend Warrior”, physical activity may need to be more intense.
Study 3 Details
Title: The “Weekend Warrior” and Risk of Mortality
Methods
- Prospective study of 8,421 men without chronic disease
- Classified based on activity levels:
- “Sedentary” (expending <500 kcal/week)
- “Insufficiently active” (500–999 kcal/week)
- “Weekend warriors” (≥1,000 kcal/week from sports/recreation 1–2 times/week),
- “Regularly active” (all others expending ≥1,000 kcal/week)
- Followed x9 years
Results
- Weekend warriors did NOT have a lower all-cause mortality.
- “The multivariate relative risks for mortality among…weekend warriors was 0.85 (95% CI: 0.65, 1.11)”
- However, Weekend Warriors did have lower all-cause mortality in those without risk factors (smoking, overweight, hypertension, dyslipidemia).
- “In stratified analysis, among men without major risk factors, weekend warriors had a lower risk of dying, compared with sedentary men (relative risk = 0.41, 95% CI: 0.21, 0.81). This was not seen among men with at least one major risk factor (corresponding relative risk = 1.02, 95% CI: 0.75, 1.38).”
Authors’ Conclusions
- “High-risk men may not benefit from sporadic physical activity, such as the weekend warrior pattern, because some beneficial effects of physical activity are short-lived.”
Study 4 Details
Methods
- Pooled analysis of 6 studies, 661,137 participants (21-98 years old)
- Followed x14.2 years
Results
- The maximum amount of benefit for reducing all-cause mortality is found at exercising at least 3-5x/wk. But, “Weekend Warriors” still saw similar benefits.
- “Compared with individuals reporting no leisure time physical activity, we observed a:
- 20% lower mortality risk among those performing less than the recommended minimum of 7.5 metabolic-equivalent hours per week (HR, 0.80 [95% CI, 0.78-0.82])
- A 31% lower risk at 1 to 2 times the recommended minimum (HR, 0.69 [95% CI, 0.67-0.70])
- And a 37% lower risk at 2 to 3 times the minimum (HR, 0.63 [95% CI, 0.62-0.65]).
- An upper threshold for mortality benefit occurred at 3 to 5 times the physical activity recommendation (HR, 0.61 [95% CI, 0.59-0.62]); however, compared with the recommended minimum, the additional benefit was modest (31% vs 39%).
- “Compared with individuals reporting no leisure time physical activity, we observed a:
- Cancer and cardiovascular disease benefit is also found at the highest frequency of training.
- “A similar dose-response relationship was observed for mortality due to cardiovascular disease and to cancer.”
How This Changes Clinical Practice
Clinical Takeaways
- Exercising just 1-2 days a week (“Weekend Warrior”) can lead to similar benefits in all-cause mortality compared to more frequent bouts of training. But, training should be fairly vigorous in intensity.
- However, patients with severe metabolic dysfunction may need a higher frequency of exercise/movement (up to 3-5x/wk) to get the greatest amount of benefit.