TREATING CLINICIAN: JOE MATHER, M.D.
Patient Summary: William
- Overview Context:
- William is a 41-year-old male with severe systemic symptoms that began while living in a moldy home. He has a background of working in construction and a moldy paper mill. Became ill 2 years ago, worsened after cholecystectomy. Prior to his illness he was a very active and athletic man.
- Concerns and Goals
- Patient’s main concerns are GI symptoms, fatigue, brain fog, and heart palpitations. He attributes symptoms to food triggers.
- Initial Symptoms:
- Intestinal discomfort including: nausea, bloating, cramping, stomach sensitivity, indigestion.
- Reports nausea when going several hours of fasting.
- BM every 1-2 days, consistency varies: diarrhea/mush.
- Chronic fatigue/muscle soreness:
- “I have been exercising since I was 14. I’m an MMA fighter and have fought guys 2x my size. This has never happened before… I can’t exert myself at all.“
- Chronic persistent brain fog:
- Worsens with exertion: head spins and brain fog worsens.
- Heart palpitation, blurry vision, shakiness, orthostatic dizziness/feeling faint.
- Reports experiencing heart palpitations mostly at night. Accompanied by nausea, chills, and feelings of sadness, terror, bad dreams, sense of dread.
- Intestinal discomfort including: nausea, bloating, cramping, stomach sensitivity, indigestion.
- Prior Diagnosis:
- Alkaline induced gastritis ~3 months ago.
- Bile reflux: Bile laying in stomach during scope. ~3 months ago.
- Onset, Timeline and History:
- Worked in construction. “I got an unexplained fever three times after working in a specific paper mill with mold and chemicals. Lived in a house that smelled of dampness and mildew for three years.” Symptoms began in this time period.
- After a period of many tests and doctor visits in an attempt to find the cause of his symptoms, he had his gallbladder removed. Everything worsened significantly after surgery.
- Gradually improved from nearly nonfunctional, to the current state of settled discomfort and weakness, hoping he doesn’t flare for whatever reason.
- “That house had moisture, my wife was sensitive and had histamine issues.”
- Clinical Analysis
- Even though William has worked through some foundational GI care, therapies such as probiotics and elemental dieting were done in isolation or at an inadequate dose.
- There are two main avenues to pursue in his history. First, his past endoscopy noted a remarkable amount of bile reflux. Second, he is extremely likely to have been made sick by mold given:
- Chronic fatigue worsens with exercise, brain fog, orthostasis, muscle soreness, and constellation of nighttime symptoms. Nighttime worsening flares, or early morning grogginess that slowly fades over the course of the day suggests mold exposure in a bedroom, AC system, or mattress.
- Very clear exposure at work and home. It is important that his wife developed symptoms from his house.
- Recommended Testing
- Real Time Labs urine mycotoxin test
- CMP, CBC w diff, iron panel, ferritin, Vit D
- Thyroid Panel: TSH, fT4, fT3, TPO
- Metabolic: fasting insulin, CMP, HgA1c, lipid panel
- Clinical Decision Making
- Identify and measure the burden of mycotoxins
- Help build buy-in for subsequent treatment for mold illness
- Rule out other pathologies (e.g. hypothyroidism, iron deficiency, insulin resistance)
- Initial Treatment Recommendations
- Diet and Lifestyle
- Please continue your current diet. Our goal is to slowly work to expand what you can tolerate, but continue to focus on foods that you tolerate without reaction.
- Please add ⅛ – ¼ tsp of flax meal / flax fiber to each meal and slowly increase the amount to ½ – 1 tsp with each meal. This should be done very gradually so that you do not notice any bloating or nausea.
- GI
- Elemental Diet – 2-4 day reset
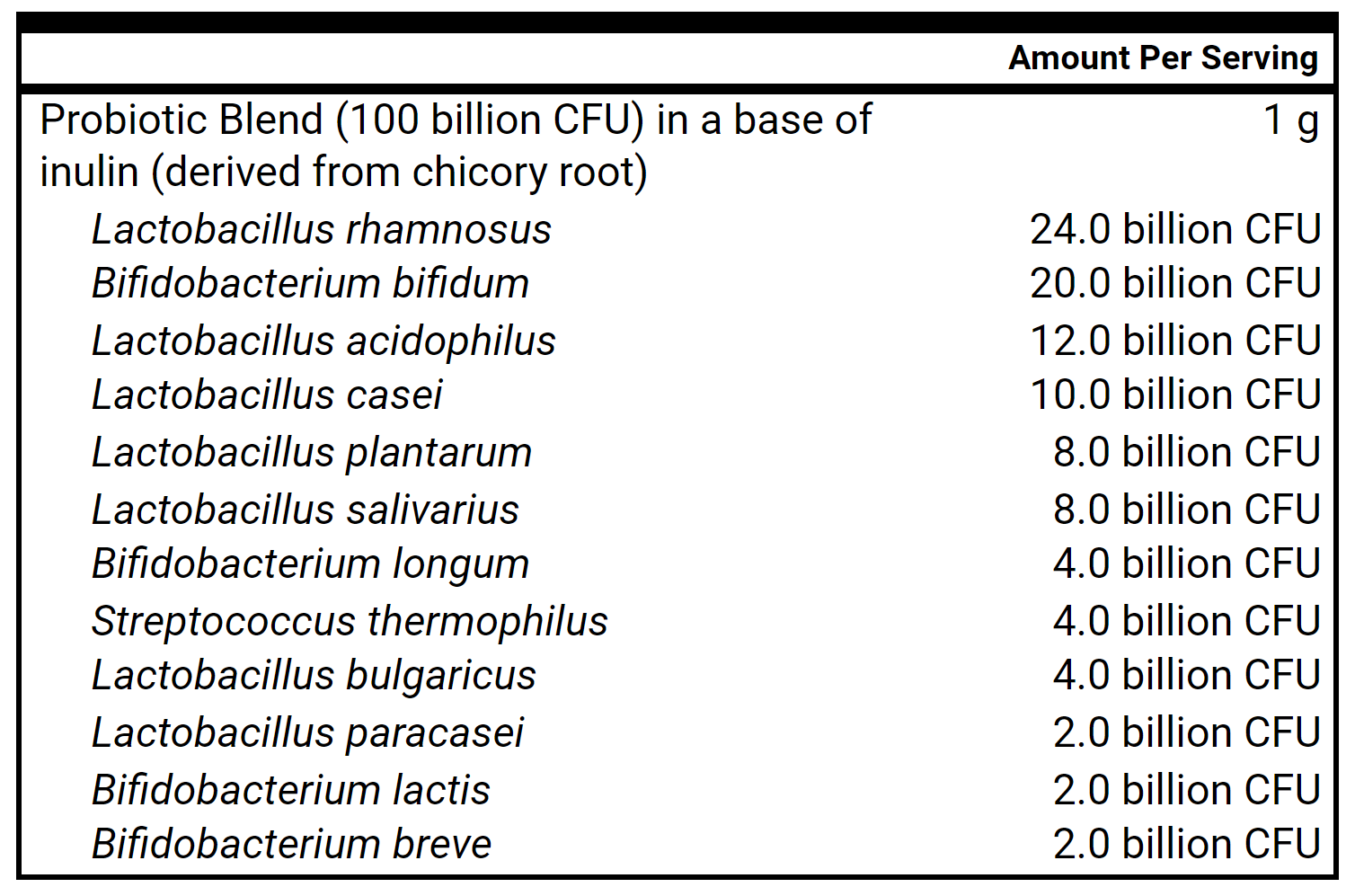
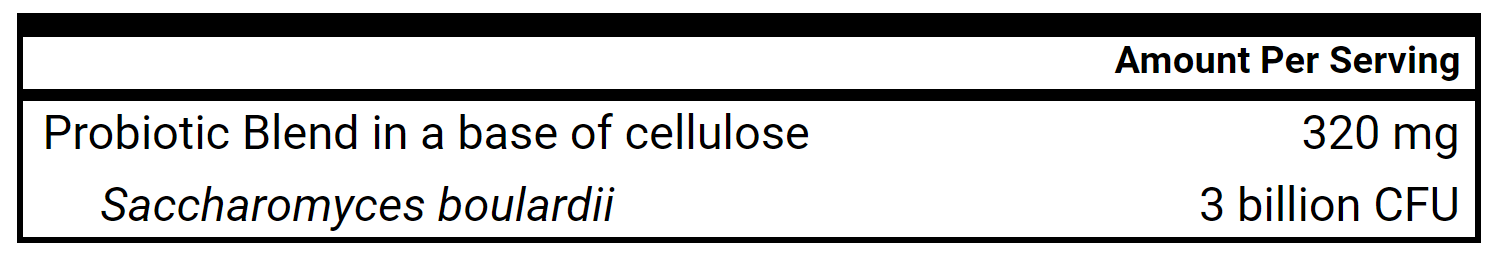
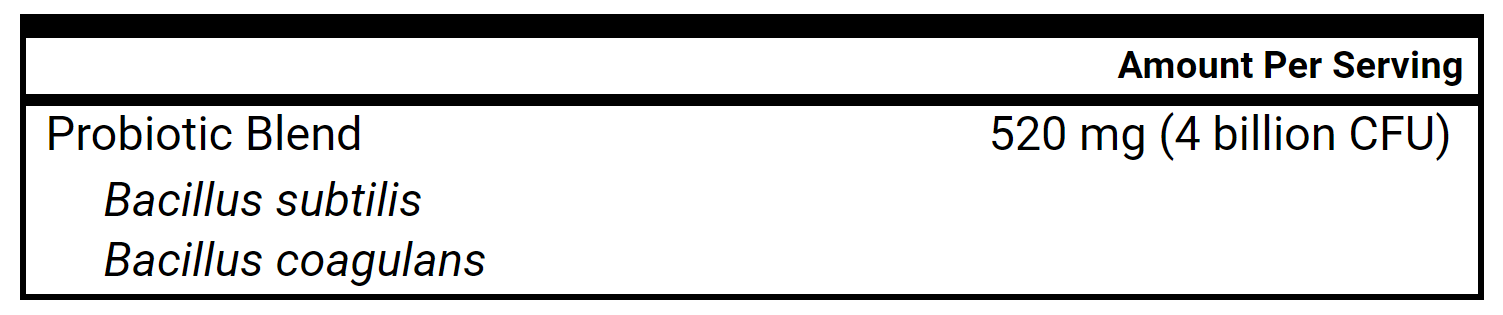
- Lacto-Biff., Soil-Based, Saccharomyces boulardii, OR All-in-one probiotic
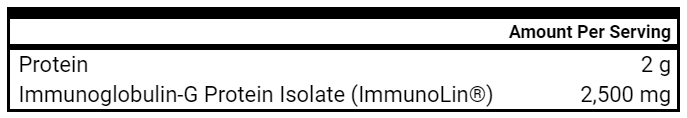
- Immunoglobulins – please increase to 2 scoops (5 grams) a day
- Elemental Diet – 2-4 day reset
- Follow-up: 4-5 weeks
- Diet and Lifestyle
- Clinician Treatment Summary
- First, we will revisit foundational GI care (probiotics, elemental diet) and use at a clinically effective dose.
- We will start flax fiber as a binder sequestrant for bile and mycotoxins.
- We can also address MCAS if still experiencing sensitivities.
- Then, consider antimicrobials.
- Patient Self Assessment
- Patient rates health as 60/100 and 10% better than the last time we met. Reports less constipation, diarrhea, bloating and better sleep.
- Brain fog, muscle fatigue/weakness, food sensitivities, sensitivity to exertion stayed the same.
- Elemental Diet – “I tried too fast.” Drank 3 shakes in a short period of time. Crashed. Went backwards for 3-4 days. Now tolerates 4 scoops for breakfast.
- Notices yellow to white coating on his tongue.
- Lab Results
- RTL: Ochratoxin 0.52, Aflatoxin 0.69, Trichothecene 0.10, Gliotoxin 0.03, Zearalenone 0.34.
- Ferritin 543, Iron sat 44% Iron 140 Hgb 16.6, Hct 49.2
- TC 253, LDL-C 185
- Fasting glucose 88, A1c 5.1, Insulin 4.2
- TSH 2.7, 3F 2.8, TPO <8
- Lab Interpretation and Diagnosis
- Labs notable for:
- Elevated trichothecene. Other mycotoxins unremarkable.
- Elevated iron with normal Hct/hemoglobin: most likely hereditary hemochromatosis, possibly worsened from an inflammatory response.
- Dyslipidemia with good glycemic control.
- Euthyroid, negative for autoimmunity.
- Labs notable for:
- Clinical Analysis
- William had a great response to adding flax to his meals. This alone markedly reduced many of his GI symptoms.
- Candida, dysbiosis, and SIBO are flagged given the new finding of oral thrush.
- As he was still experiencing severe fatigue, exercise intolerance, and food sensitivities, we will layer in:
- Limbic retraining
- Histamine support (both natural and OTC)
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue current diet + GI supports
- Start Gupta limbic retraining program
- Food Reactivity Support
- Loratadine 10mg (Claritin) OR Fexofenadine 60 mg tablets (Allegra) – 1 tablet daily, may increase to 1 tablet twice daily.
- Famotidine 20mg (Pepcid AC) OR Cimetidine 200 mg (Tagamet) – 1 tablet daily, may increase to 1 tablet twice daily.
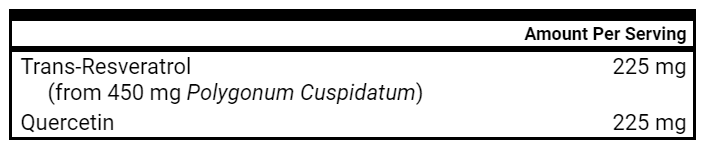
- Resveratrol – 1 capsule prior to meals, may increase to 2 prior to meals
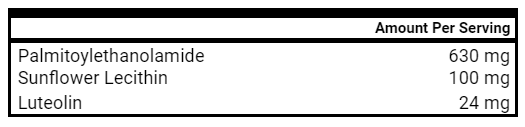
- PEA + Luteolin: Start 1 capsule in the morning, slowly increase to max of 2 capsules twice daily (especially helpful for fatigue, brain fog, depression)
- Follow-up: 4-5 weeks
- Diet and Lifestyle
- Patient Self Assessment
- Patient rates health as 65/100 and 10% better than the last time we met.
- Diarrhea and constipation, muscle soreness, fatigue and brain fog, GI discomfort all improved.
- Food sensitivities and aversion to physical activity stayed the same.
- Had some night attacks and anxiety, determined it was due to PEA + Luteolin. Went away as soon as the supplement was discontinued.
- He expressed concern about elevated iron.
- Clinical Decision Making
- GI symptoms are continuing to improve.
- He likely needs more time on limbic work.
- We will layer in other binders in addition to flax fiber.
- We will also give him specific suggestions on ways to reduce iron overload.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Revisit flax fiber recommendations
- Avoid vitamin C, as this increases iron absorption
- Binders – Add binders one at a time, aiming to add a new binder once every 3 days
- Activated Charcoal – 1 capsule daily taken with other binders
- Chlorella – 1 capsule daily taken with other binders
- Bentonite Clay – 1 capsule daily taken with other binders
- Follow-up: 5 weeks (after you’ve been on the binders 1 month)
- Diet and Lifestyle
- Patient Self Assessment
- Patient rates health as 75-80/100 and 10-15% better than the last time we met.
- Intestinal troubles, diarrhea, brain fog, night time attacks, weight all improved.
- Fatigue, muscle soreness have improved greatly. “I have not feared the stairs at work. I still have a hard time in the morning and can’t exert myself but not constantly.”
- No stomach discomfort. “I noticed only very minor discomfort if I stay within the diet and don’t overeat.”
- Food sensitivities have mostly stayed the same.
- Recommended Testing
- Repeat Real Time Lab mold testing and bloodwork
- Clinical Decision Making
- The addition of binders has led to steady improvements. We’ll work up to the upper end of the dose range of binders and layer in herbal antimicrobials.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Increase the flax upwards to max of 3 tsp each meal.
- Periodically try resuming your workouts with the goal of pushing yourself, but backing off if you experience fatigue the following day.
- Binders
- Double binders to 2 each taken once daily.
- GI
- If you are having any remaining loose stools or GI pain, then please try adding the mylanta taken with each meal.
- Then start herbal antimicrobial protocol.
- Herbal antimicrobial 1: 4 pills, 2x per day
- Herbal antimicrobial 2: 2 pills, 2x per day
- Herbal antimicrobial 1: 4 pills, 2x per day
- Follow up: 4-6 weeks
- Diet and Lifestyle
Clinical Rule(s) / Final Clinician Comments
- Clinical rule: Consider Bile Acid Malabsorption as a root cause of chronic GI Symptoms
- Commentary: This case shows the power of the right treatment given at the right time, as William responded extremely well to layering in fiber with meals early in his treatment. When we continued adding further binders, he did even better confirming our clinical hypothesis. Along with helping detoxify mold toxins, natural binder therapies can be effective in managing bile acid malabsorption symptoms.
Clinical Questions
- Is Blastocystis hominis a commensal or a pathogen?
- Does it play a role in IBS and/or IBD?
- Should it be treated?
Functional Medicine “Bias”
- Functional medicine circles are quick to view Blastocystis hominis as a pathogen and are ready to eradicate it with antimicrobial therapy.
What Does The Evidence Actually Suggest?
- The association between Blasto and IBS and IBD is modest at best.
- Results are mixed on whether eradication therapy improves IBS or IBD outcomes.
- Blasto is relatively common in the general population.
- Highly sensitive stool tests may identify Blasto in individuals where it may not be the source of symptoms.
- There is more evidence that Blasto is a commensal than a direct pathogen. It may be more of a sign of dysbiosis than a true “infection”.
What Should I Do In Clinical Practice?
- Be careful in interpreting positive Blasto results on stool tests.
- Direct eradication therapy is not recommended in the majority of cases.
- If eradication therapy is chosen, the therapeutic goal should be resolution of symptoms (not eradication of Blasto).
Blasto and IBS
- High-Level Overview
- Studies are mixed as to whether B. hominis is associated with IBS. If there is an association, it is modest at best.
- B. hominis may be more associated w/ IBS-D compared to other IBS subtypes.
- B. hominis subtype 1 may be the most problematic.
- Symptoms that result from the presence of B. hominis may be secondary to an imbalanced microbiome and/or an unhealthy host.
- Clinical response to B. hominis eradication is sometimes associated w/ microbiological eradication, but NOT always.
- We argue that Blasto is not an “infection” that needs to be eradicated in ALL individuals, as this may lead to over-treatment. However, there may be a subset of individuals who may benefit from direct antiparasitic therapy after they exhaust more foundational, empirical interventions in cases of high counts of colonization.
- Correlation between Blasto & IBS
- A meta-analysis of 29 observational studies showed a significantly higher risk of IBS (OR 1.78) in those with Blasto.
- Another meta-analysis of 17 studies involving 5,900 participants (2,500 IBS, 3,300 controls) also found an association between IBS and B. hominis (OR 2.19). The greatest association was seen w/ Blasto subtype-1 (OR 4.4). No association was found between D. fragilis and IBS.
- NO correlation between Blasto & IBS
- It’s important to note that not all data agrees. Some studies have found that Blasto was present at higher rates in healthy controls when compared to individuals with IBS. In a study of 419 individuals, presence of any kind of parasite and Blasto were both found at higher rates in healthy controls.
- A 2020 population based case control study of 483 adults in Denmark found that D. fragilis and Blastocystis were detected in a greater proportion of fecal samples from the asymptomatic background population in Denmark than from subjects with IBS symptoms.
- D. fragilis was detected in a greater proportion of fecal samples from controls than cases (35% vs. 23%)
- Blastocystis (22% of controls vs. 15% of cases)
- Greater percentage of controls carried more than 1 species of parasite (16% of controls vs. 8% of cases)
- Correlation between treatment and improved IBS
- Analysis of 2 pooled randomized, double-blind, placebo-controlled studies found that Blasto eradication w/ Nitazoxanide for those w/ Blasto and diarrhea was better at achieving clinical remission of symptoms when compared to placebo (86% treatment vs 38% placebo).
- A placebo-controlled study of 616 individuals w/ diarrhea showed that 16% had B. hominis (per microscopy) and 24% of those infected w/ B. hominis had co-infection w/ another organism (e.g Giardia, Cryptosporidium). Improvement of symptoms correlated w/ eradication of the parasite after Flagyl therapy (80% eradication rate; 88% became asymptomatic at 1 month).
- NO correlation between treatment and improved IBS
- This study of 39 patients w/ symptoms and Blasto who received Flagyl therapy found that 79% had symptom improvement after therapy. However, only 48% had eradication of Blasto. This means that many improved their symptoms WITHOUT necessarily eradicating Blasto.
Blasto and IBD
- High-Level Overview
- There are many fewer studies on IBD compared to IBS. The vast majority of the studies suggest that Blasto is NOT associated w/ IBD (both Crohn’s disease and ulcerative colitis).
- In fact, some studies suggest Blasto rates are higher in healthy controls.
- Antibiotic therapy may improve IBD outcomes but clinical improvement is NOT always associated with eradication of the organism.
- Correlation between Blasto & IBD
- The largest study to date we have on this is a case-control study of 2,334 patients w/ gastrointestinal symptoms including 335 w/ IBD, compared to 192 healthy controls. It found that Blasto was more common in those w/ IBD compared to controls, but this finding was only found in those w/ ulcerative colitis (not Crohn’s disease).
- NO correlation between Blasto & IBD
- In a study of 616 healthy individuals and 107 IBD patients, Blasto was more common in healthy controls (30% vs 4%). Another study found similar results while also noting almost a 2x higher rate in healthy controls. A third study found a 2.5x increased rate (32% vs 13%) of Blasto in healthy controls compared to those w/ UC. Finally, a fourth study found a 4x increased rate (19% vs 5%) of Blasto in healthy controls.
- Correlation between treatment and improved IBD
- In a study of 100 UC patients and 200 healthy individuals, UC patients treated with a combination of nitazoxanide with mesalazine showed better mucosal healing than in patients treated with conventional monotherapy of mesalazine. However, symptom improvement was not different between the two therapies.
- NO correlation between treatment and improved IBD
- This small retrospective study of 12 IBD patients with Blasto found that only 3 of the 8 who received Flagyl had symptom improvement.
Is Blasto a pathogen or a commensal?
- High-Level Overview
- Blasto is common in the general population- more so in developing countries.
- Overall, the majority of the research suggests that Blasto is more of a commensal than an overt pathogen.
- Most studies utilize culture and microscopy, and only a few studies have utilized quantitative PCR (qPCR) technology (e.g. GI-MAP). The qPCR studies have suggested that Blasto is NOT higher in symptomatic individuals compared to asymptomatic individuals.
- Supporting Research
- “Recent studies using DNA-based methods to assess the positive rate in different cohorts have seen prevalence rates ranging from about 50% in healthy adults in highly industrialized countries to 100% in healthy Senegalese children. There is also data suggesting that long-term carriage of Blastocystis may exist, with some individuals testing positive for the same strain over a span of 10 years.” (X)
- In a multicenter case-control study of 1,374 gastroenteritis cases and 1,026 healthy controls using PCR analysis, the presence of both D. fragilis and Blasto was highest in children under 20 years of age and lowest in the oldest age group. More GI symptoms were reported in cases without D. fragilis or Blastocystis.
- “This study suggests that the presence of these protozoans may be considered characteristic of a healthy intestinal microbiome.”
- This study used quantitative PCR (like GI-MAP) and found Blasto in 72% of 95 children without symptoms. In another study using qPCR technology, only 29.6% of the patients who tested positive for Blasto presented with symptoms. In another study, none of the 30 children w/ Blasto had any digestive symptoms. This may suggest that Blasto may be less problematic if acquired earlier in life.
- Antibiotic therapy may improve symptoms by correcting dysbiosis other than Blasto.
- This study suggests “It has been speculated that any resolution of symptoms may actually be secondary to eradication of some unrecognized pathogen rather than to specific treatment of Blastocystis.”
Should Blasto be treated?
- High-Level Overview
- Given the higher sensitivity of quantitative PCR (e.g GI-MAP) and the lack of evidence to support Blasto being overtly pathogenic, the mere presence of Blasto does not necessitate treatment in all individuals (especially if asymptomatic).
- Antimicrobial therapy may be indicated under the following conditions:
- 1) The patient exhibits symptoms.
- 2) There are higher counts of Blasto on PCR (cutoff has yet TBD but perhaps above 4.85 x 104).
- 3) You have established the use of more foundational GI therapies (triple probiotics, diet, lifestyle).
- If you do choose antimicrobial treatment, the target should be resolution of symptoms, not complete eradication of the parasite.
- This means that you may NOT need to use direct antiparasitic medications (e.g. Alinia, Flagyl) in all patients. Rather, a more broad-spectrum antimicrobial protocol (e.g. herbal combos) may be a better choice given that you can also correct for other dysbiosis (bacterial, fungal, etc).
- If you do choose medications, here are the ones most commonly used:
- Metronidazole (Flagyl)
- Nitazoxanide (Alinia)
- TMP-SMX (Bactrim)
- Paromomycin
- Antimicrobial therapy may correct other pathogens/dysbiosis, leading to resolution of symptoms.
- Remember to lay GI therapy foundations (diet, lifestyle, probiotics) before layering in antimicrobial therapy to ensure the best possible outcome.
Final Thoughts
- Blasto is not as harmful as many make it out to be.
- It is safe to hold direct eradication therapy for Blasto in the majority of cases. However, some individuals may benefit from antimicrobial therapy after using more foundational therapies (e.g. diet, probiotics).
- This potential benefit may be independent of Blasto eradication therapy, though.
Study Purpose
- Narrative review of the role of fecal calprotectin (FC) in the setting of IBD management
Main Results:
- Low FC is good at ruling out IBD.
- “In conclusion, FC is currently the most widely used fecal marker for differentiating between IBD and IBS; due to the high negative predictive value, it is highly accurate in ruling out intestinal inflammation both in primary and secondary care.”
- FC is a good marker for distinguishing IBS from IBD, even in IBD patients who are in remission.
- “Among IBD patients apparently in remission with IBS-like symptoms, FC tends to be significantly higher than in IBS, suggesting the presence of an undercurrent low-grade inflammation.”
- FC is also a good prognostic marker for monitoring disease activity and predicting relapse.
- “In those with established diagnosis of IBD, a growing number of studies suggest an increasingly recognized role of the test in monitoring disease activity and response to therapy, as well as in predicting disease relapse, including pouchitis. The main concerns are still related to the choice of the optimal cut-off, both for ruling out intestinal inflammation and for the management of IBD patients.”
- “Fecal calprotectin has emerged as one of the most useful tools for clinical management of IBD.”
- FC levels < 50 μg/g can be used to screen for IBD.
- “A cut/off value of 50 μg/g of FC has been the most commonly adopted both in literature and by commercially available ELISA kits, for adults and children over 4 years to differentiate IBD from other forms of inflammation. Moreover, Lin et al suggested 50 μg/g as a screening cut-off value for further endoscopy examination in clinical practice, with specificity of 60% and pooled sensitivity of 92%.
- FC <250 μg/g indicates IBD remission.
- “As the cut-off value increases, sensitivity becomes lower and specificity higher. A FC value of 250 μg/g was deemed appropriate for monitoring disease activity in IBD. D’Haens et al examined 126 IBD patients (87 CD and 39 UC) and proposed a FC cut-off of 250 μg/g for indicating IBD remission.”
- FC levels are higher in younger kids, and decrease with age.
- “A statistical difference was found between FC in healthy children aged 1-3 mo and those aged 3-6 mo (375.2 μg/g vs 217.9 μg/g), as well as between 1-6 mo and 6-18 mo (median: 282.7 μg/g vs 114.9 μg/g). The results clearly indicate that different cut-offs are necessary for children less than 4 years old. Oord et al proposed:
- 538 μg/g for 1-6 mo
- 214 μg/g for 6 mo-3 years
- and 75 μg/g for 3-4 years.”
- “In newborns FC concentrations may increase up to 30% when the sample is collected from a diaper, which may be explained by the water absorption into the diaper.”
- “A statistical difference was found between FC in healthy children aged 1-3 mo and those aged 3-6 mo (375.2 μg/g vs 217.9 μg/g), as well as between 1-6 mo and 6-18 mo (median: 282.7 μg/g vs 114.9 μg/g). The results clearly indicate that different cut-offs are necessary for children less than 4 years old. Oord et al proposed:
- FC levels may be more helpful in UC than in CD.
- “Both in monitoring of therapy and in prediction of relapses FC seems to be more effective in UC than in CD.”
Clinical Takeaways:
- FC levels can effectively help you distinguish between IBD and other functional GI disorders such as IBS. Levels <50-100 μg/g effectively rule out IBD.
Heat stress and fetal risk. Environmental limits for exercise and passive heat stress during pregnancy: a systematic review with best evidence synthesis
- Background: Pregnant women are advised to avoid heat stress (e.g. excessive exercise and/or heat exposure) due to the risk of teratogenicity associated with maternal hyperthermia (defined as core temperature (Tcore) ≥39.0°C).
- Aim: Evaluate the risks of various forms of exercise on Tcore elevations
- 12 studies, 347 pregnant women
- No woman exceeded a Tcore of 39.0°C.
- The highest Tcore was 38.9°C due to exercise.
- Conclusion: Pregnant women can safely engage in:
- (1) Exercise for up to 35 min at 80%-90% of their maximum heart rate in 25°C and 45% relative humidity,
- (2) Water immersion (≤33.4°C) exercise for up to 45 min; and,
- (3) Sitting in hot baths (40°C) or hot/dry saunas (70°C; 15% humidity) for up to 20 min, irrespective of pregnancy stage, without reaching a core temperature exceeding the teratogenic threshold.
Probiotics for preventing acute upper respiratory tract infections
- 14 RCTs, 3,451 participants
- Probiotics led to reduction of acute upper respiratory tract infections (URTIs)
- At least one URTI episode (OR 0.58)
- Reduced antibiotic use (OR 0.67)
- Similar duration of each URTI episode
Variability of fecal calprotectin in healthy patients without colonic inflammation or neoplasm
- Given calprotectin’s utility in distinguishing IBS from IBD, as well as its ability to help track disease remission and relapses, calprotectin has recently been proposed as a marker of colonic neoplasm and inflammation in healthy patients. This study of 14 healthy patients referred for colonoscopy was performed to assess the biological variability of fecal calprotectin in patients referred for colonoscopy.
- Prospective study of 14 participants. 8 stool samples were collected in each volunteer leading up to the colonoscopy.
- Two groups emerged from the analysis:
- Roughly a third had very low and stable FC values <50 mcg/g.
- Roughly two thirds had high variability of FC levels > 50 mcg/g.
- “In this latter group fecal calprotectin ranged from 9 to 461 (mean 70) showing considerable day-to-day variation.”
- Conclusion: Day-to-day variation of FC is considerable in patients without colonic inflammation or neoplasm. Those with very low FC levels have less variability. For this reason fecal calprotectin is unlikely to be a reliable marker in healthy patients.
In vitro binding of bile acids by okra, beets, asparagus, eggplant, turnips, green beans, carrots, and cauliflower
- “Binding bile acids and preventing their recirculation results in:
- reduced fat absorption
- excretion of cancer-causing toxic metabolites
- and cholesterol utilization to synthesize more bile acids.”
- “Assigning a bile acid binding value of 100% to cholestyramine, the relative bile acid binding on dry matter basis for the test samples was:
- okra 16%
- beets 11%
- asparagus 4%
- and 1% by eggplant, turnips, green beans, carrots and cauliflower.”
- Conclusion: Foods (especially okra and beets) can bind to bile according to in vitro studies.
Steam cooking significantly improves in vitro bile acid binding of beets, eggplant, asparagus, carrots, green beans, and cauliflower
- This is a follow-up study.
- “Steam cooking significantly improved in vitro bile acid binding of beets, eggplant, asparagus, carrots, green beans, and cauliflower compared with previously observed bile acid-binding values for these vegetables uncooked.”
- Conclusion: Steam cooking these vegetables can improve their bile-binding properties.