Thyroid and Overall Health Improved Through Gut-Based Therapies Despite Nutritional Labs NOT Improving
TREATING CLINICIAN: ROBERT ABBOTT, MD
Patient Info:
- Rebecca is a 43 y/o F, educated and well aware of Functional Medicine
- Previous Dx
- Euthyroid Hashimoto’s Thyroiditis (HT)
- Rx
- None
- Chief Complaints
- Female Hormone Symptoms: PMS, mood fluctuations around menstruation
- Fatigue
- Bloating, Belching
- Diarrhea
- Lower abdominal pain
Initial Impression:
- Rebecca is 43 y/o overweight F with a constellation of gut, female hormone, and constitutional symptoms who currently has Euthyroid HT
- Dx/Rx
- Currently taking no medications (no hormone replacement)
- Previous Testing
- April 2020 Blood Chem
- TSH: 3.32, Free T4: 1.06, TPO: 81, TGA: 2.4
- Trigs: 124, VLDL-C: 25
- Ferritin: 19, Iron Saturation: 15%
- April 2020 Blood Chem
- Onset
- Reports a period of severe stress around 7 years ago (2013)
- Noted worsening fatigue, bloating, excessive gas
- PMS and female hormone-related symptoms became more prominent
- Self-diagnosed with Euthyroid HT in 2019, onset of above symptoms
- Followed the autoimmune protocol (AIP) after the diagnosis, was successful with weight loss and some symptoms improvement, but this was not sustainable for her
- Family History
- No history of autoimmunity, hypothyroidism
- Prior Treatments
- Iron supplement with Vitamin C – given low iron levels
- PMS support supplements – minimal relief of symptoms
- Notes/DDX
- Gut Dysbiosis vs. SIBO vs. Gut Pathogen
- Maldigestion/Malabsorption
- Nutritional Deficiencies
- Dyslipidemia with mild insulin resistance (elevated trigs, VLDL-C)
- Celiac Disease?
- Liver Steatosis?
- Female Hormone Imbalance – Estrogen Dominance?
- HPA Axis Dysregulation – Burnout Syndrome
- Euthyroid HT
- Prognosis
- Expect her to do very well with an iterative and GI focused approach
- Previous Diets
- AIP diet – helpful but not sustainable
- Whole food, gluten, and dairy-free – Helpful and more sustainable
Testing:
- Tests Ordered
- CMP, Uric Acid, GGT
- Iron Profile, homocysteine, magnesium, zinc, copper, vit D
- Lipid panel, apo b, lp(a), a1c, fasting insulin
- CBC with differential, hs-CRP
- GI MAP – stool testing
- Rationale
- I would like to get a solid baseline of blood chemistry testing as the foundation of my clinical assessment
- Given her mixture of upper and lower GI symptoms in the setting of the autoimmune thyroiditis diagnosis, I discussed the utility of stool testing which she desired to pursue
Recommendations:
- Probiotic Therapy (start after GI testing)
- SBO
- S. boulardii
- SBO
- Digestive Support (start after GI testing)
- Digestive Enzymes
- Betaine HCl with Pepsin
- Digestive Enzymes
- HPA Axis and Female Hormone Support
- Adaptogens
- Ashwagandha
- Adaptogens
- Nutritional and Lifestyle
- Paleo low FODMAP
- Daily meditation
- Increase walking
- Spend time outdoors on rural property home
- Rationale
- I am suspecting dysbiosis with aspects of maldigestion. I would like for her to begin baseline probiotic therapy for a few weeks followed by digestive support. Should her GI MAP testing reveal signs of a GI pathogen or other concerning findings, we will have laid a solid foundation on which we can layer/add herbal or prescription antimicrobial therapies if needed We will focus on her implementing a Paleo lower FODMAP diet and suggest the utilization of some adaptogens to see if this improves her upper GI symptoms and energy levels respectively. I will also encourage her to test/explore the safety of her well water.
Subjective Assessment:
- Rebecca reports some improvements in her diarrhea and energy, bloating somewhat curtailed but remains challenged with some epigastric abdominal pain. She also reports some discouraging testing on her well water that showed some elevated coliform bacteria.
Lab Interpretation:
Blood Chemistry (July 2020)
- Alkaline Phosphatase: 32 (L)
- Hemoglobin: 12.3
- WBC: 4.1, Eosinophils: 2.7%, Monocytes: 13.1% (H)
- apoB: 132 (H)
- Fasting Insulin: 6.8, HOMA-IR: 1.39
- Ferritin: 20 (L), Iron Sat %: 31
- Vitamin D: 34 (L)
- Zinc: 64 (L)
- Homocysteine: 12 (H)
GI MAP (July 2020)
- No overt GI pathogens
- Normal H. pylori
- Candida spp. Elevated
- Low/moderate level B. hominis, D. fragilis
- Elevated glucuronidase, sIgA
- Elastase: 425 (nl)
- Calprotectin: 67 (nl)
Diagnosis:
- Small intestinal dysbiosis (clinical)
- Intestinal parasitism
- Candida overgrowth?
- Nutritional Deficiencies, Zinc, B Vitamins, Vitamin D, Iron
Impression:
- Rebecca has made some progress with the initial GI supports. Her GI testing combined with well water testing was concerning for potential intestinal parasitism. Her blood chemistry testing revealed multiple nutritional deficiencies. While her iron saturation has improved, her ferritin is less than normal and she has sub-optimal Vitamin D and elevated homocysteine, common findings in those with GI issues and immune challenges. I believe her elevated monocytes are connected to chronic stress in the setting of known GI and immune challenges. I feel she would be best served by an earlier pivot to a combination herbal antimicrobial and a prescription anti-parasitic.
Recommendations:
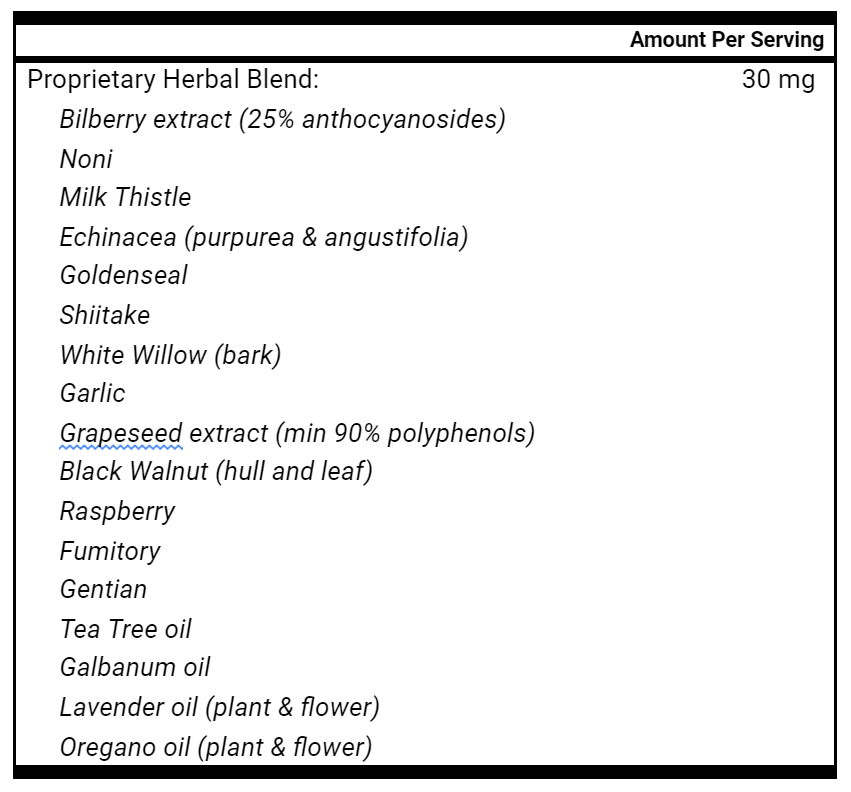
Starting
- Binder
- Liquid antimicrobials
- Transition to higher dose S. boulardii
- Order Alinia for use following herbal antimicrobials
- Continue current probiotics and digestive supports
- Continue current Paleo low FODMAP diet
Subjective Assessment:
- Was doing really well with the overall protocol and then went on vacation to the beach for 2 weeks and expanded her diet to include more wine, dairy, and grains. This seemed to exacerbate symptoms of digestive distress.
- She discontinued the Betaine HCl with pepsin and digestive enzymes given some burning when symptoms worsened
- Has been more strict with her diet since the flare, but reports continued cravings for carbohydrates
- The post-ovulatory period and menstruation still remain challenging, gets worsening mood and depression leading up to menstruation
- Has not been able to start Alinia- still waiting on mail order
- Overall would describe the trajectory as 2 steps forward, 1 step back, moving in the right direction
Impression:
- Rebecca appears to have continued her progress despite a diet-induced flare while on vacation. She no longer appears to need digestive supports but continues to do well with probiotics and herbal antimicrobials. While the flare was a challenging event – pointing to the fact that the GI tract and overall body are not quite ready for certain dietary expansions, I feel that the overall trajectory is positive and that we should continue forward with current recommendations and the plan for future Alinia as well.
Recommendations:
- Introduce Alinia upon receiving, 500 mg twice daily for 2 weeks
- Optional exploration of DIM, Calcium D Glucarate
- Continue previous supplements
- Repeat blood chemistry in 6-8 weeks prior to follow-up
- Note: Patient desires to repeat GI MAP following continued herbal antimicrobial use and Alinia. I advised that I did not feel it would be clinically necessary but obliged her request.
Subjective Assessment:
- The patient is reporting global improvement with digestive/GI health, female hormone symptoms and mood. She attributes the improvements mostly to both the herbal antimicrobials and the Alinia.
Lab Interpretation:
Blood Chemistry (Nov 2020)
- Alkaline Phosphatase: 31 (L)
- Hemoglobin: 12.3 → 11.1 (L)
- WBC: 4.1 → 3.9, Eosinophils: 2.7% → 1.3%, Monocytes: 13.1% → 10%
- TSH: 3.32 → 1.75, TPO: 81 → 37
- Ferritin: 20 → 10 (L)
- Vitamin D: 34 → 35 (L)
- Zinc: 64 → 59 (L)
- Homocysteine: 12 → 12.4 (H)
GI MAP (Nov 2020)
- No overt GI pathogens
- Still normal H. pylori
- Elevated Pseudomonas spp.
- NO Candida spp. elevation
- NO levels of B. hominis, D. fragilis
- Normalized sIgA, glucuronidase
- Low normal elastase: 425 → 210
- High steatocrit
Diagnosis:
- Mild pancreatic insufficiency
- RESOLVED Intestinal parasitism
- RESOLVED Candidal overgrowth?
- Nutritional Deficiencies, Zinc, B Vitamins, Vitamin D, Iron
Impression:
- Rebecca is showing clinical and laboratory evidence of improved gut and thyroid health. She is still somewhat nutritionally depleted, but her clinical picture has every indication of a healing gut making continued gut repair and nutritional repletion an easier task. She would likely benefit from a shorter course of reintroduced digestive enzymes WITHOUT Betaine HCl to help facilitate nutritional repletion alongside gut repair nutrients. It would be easy to get discouraged by aspects of the nutritional labs, but we do not treat labs, we treat people and we have started to turn around the biggest dysfunctions: her gut and thyroid. We will be more successful with our next phases of nutritional repletion and optimization because of these foundational improvements. The best part? SHE IS TELLING ME SHE FEELS BETTER!
Recommendations:
- Continue SBO and S. boulardii
- Add Zn and Fe supplementation (away from other supplements, with meals)
- Add ADEK supplementation
- Reintroduce digestive enzymes
- Add gut repair nutrients
This case provides a wonderful example of three clinical rules.
First, the case demonstrates again the importance of addressing the gut first for individuals with thyroid dysfunction. In this case, we identified a gut pathogen and treated the pathogen using herbal and prescription antimicrobials as part of the GI therapeutic hierarchy.
Clinical Rule 1:
Begin the sequential, GI therapeutic hierarchy for individuals with thyroid dysfunction BEFORE the immediate use of thyroid hormone replacement.
Second, the case illustrates the importance of treating the INDIVIDUAL and not treating LABS in isolation as this person’s nutritional labs were either clinically unchanged or worsened while she saw clinical improvements with her gut health.
Clinical Rule 2:
Address gut health BEFORE or DURING robust nutritional repletion.
Clinical Rule 3:
Do not treat the labs, treat the patient.
Introduction and Summary
With emerging research and continued clinical implementation, we want to provide you with KEY updates and ADDITIONS to our EXPANDED thyroid treatment algorithm for patients with thyroid dysfunction. It is our wish that the algorithm will improve your hypothyroid patient outcomes and minimize the guesswork when building diagnostic and treatment recommendations.
Intention of the Thyroid Treatment Algorithm
- Correctly identify patients WITH and WITHOUT hypothyroidism, subclinical hypothyroidism and autoimmune thyroiditis
- Better predict the need for thyroid hormone replacement medication
- Better predict the ability for patients to DISCONTINUE replacement medication
- Correctly apply an evidence informed therapeutic hierarchy prioritizing lifestyle and GI based treatments BEFORE medication (if indicated)
- Improve overall hypothyroid patient outcomes
Part 1: Screening and Clinical History
1. Does the patient have a formal diagnosis of hypothyroidism, subclinical hypothyroidism or Hashimoto’s Thyroiditis?
- If so, with what type of provider was this diagnosis made? i.e. Conventional medicine doctor or integrative medicine provider.
- Integrative providers are more likely to vector an incorrect diagnosis. To verify if a diagnosis is correct, check the lab work which made the diagnosis (from before starting medication).
2. Is there laboratory documentation of elevated TSH, and/or low Free T4 outside of CONVENTIONAL laboratory ranges?
3. Is there laboratory documentation of elevated TPO and/or elevated anti-thyroglobulin antibodies outside of CONVENTIONAL laboratory ranges?
4. What were the primary symptoms experienced by the patient at the time of diagnosis?
- Dry skin and fatigue?
- Overt gut symptoms?
5. If FEMALE, did the diagnosis occur within 1 YEAR of delivering a child?
Goals of Screening
1. Identify patient subtypes
- Overt hypothyroidism w/o laboratory evidence of autoimmunity
- Overt hypothyroidism WITH evidence of autoimmunity
- Subclinical hypothyroidism w/o laboratory evidence of autoimmunity
- Subclinical hypothyroidism WITH evidence of autoimmunity
- Euthyroid w/o laboratory evidence of autoimmunity
- Euthyroid WITH evidence of autoimmunity
- Postpartum thyroiditis
- Quantify risk associated with a degree of antibody elevation.
From these patient subtypes, we can build a clinical hierarchy with expectant treatment outcomes and begin to answer key clinical questions.
Key Clinical Questions
1. What is the likelihood of an INCORRECT hypothyroidism diagnosis?
- Diagnosis by NATURAL or functional medicine practitioner
- No laboratory evidence of HIGH TSH or LOW T4
- No laboratory evidence of HIGH TPO or TGA
- Currently not taking any thyroid hormone replacement
- Did not experience BOTH dry skin and fatigue at the time of diagnosis
- Suspected analytical interference or another potential cause of irregular/elevated TSH findings
2. What is the likelihood (IF TAKING thyroid hormone replacement medication) of the patient being able to DISCONTINUE medication in the future?
- Suspected incorrect hypothyroidism diagnosis (dx via functional ranges)
- If possible, verify diagnosis is incorrect by checking the lab work that diagnosed the hypothyroidism (from before starting medication).
- Ambiguously diagnosed cases may have a 60% chance of successful discontinuation.
- Suspected or diagnosed with subclinical hypothyroidism
- No laboratory evidence of HIGH TPO or TGA
- Thyroid medication dose is currently BELOW weight-based guidelines for post thyroidectomy (1.6 – 2.1 mcg/kg)
- Postpartum thyroiditis
3. What is the likelihood (IF REQUIRING thyroid hormone replacement medication) of the patient BENEFITING FROM combination T4/T3 or T3 medication?
- Overt hypothyroidism
- Currently using T4 only medication with continued symptom burden
- Following evidence-informed lifestyle practices
- Completion of GI specific treatment hierarchy
- Nutritional sufficiency
- Patient voiced preference for T3 or T4/T3 combination medication
Summary of Clinical History and Screening
Our ability to successfully treat individuals with thyroid dysfunction relies on the calculated and efficient screening of their clinical history including previous laboratory diagnosis and medical diagnosis. By applying a rigorous screening algorithm, you can identify patient subtypes that have likely been incorrectly diagnosed as well as patients that may be able to discontinue current medication or patients that may benefit from combination T4/T3 therapy as part of additional treatment modalities.
Part I: Screening Algorithm References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3658157/
- https://pubmed.ncbi.nlm.nih.gov/33741837/
- https://pubmed.ncbi.nlm.nih.gov/33161885/
- https://pubmed.ncbi.nlm.nih.gov/30806594/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2084120/
- https://pubmed.ncbi.nlm.nih.gov/31396154/
Part 2: Clinical Treatment – Non Medication
The intention of the clinical treatment algorithm is to properly apply low-risk and efficacious therapies in a sequential manner to increase the likelihood of improved patient outcomes and patient quality of life and to decrease the risk of patient harm.
1. Diagnostic Hierarchy
- Identify anemia or decreased oxygen-carrying capacity
- Identify or acknowledge the likelihood of a gut pathogen
- Identify or acknowledge the likelihood of small intestinal dysbiosis or SIBO
- Identify key nutritional deficiencies
- Zinc, B12, Iron, Vitamin D
- Consider screening for celiac disease and autoimmune gastritis if indicated
- Celiac: Total IgA, Transglutaminase IgA, IgG
- Autoimmune gastritis: Anti-parietal cell antibodies (APCA’s), Intrinsic factor blocking antibodies (IF-Ab’s)
2. Dietary Hierarchy
- Whole food, gluten-free
- Paleo
- Autoimmune Protocol (AIP)
- Other specialized diets – (proceed with caution)
3. GI Treatment Hierarchy
- Probiotic therapy
- Partial semi-elemental diet or full reset
- Address maldigestion/malabsorption
- Gut repair nutrients
- Immunoglobulins
- Address dysmotility
- Herbal or prescription antimicrobials
4. Supplemental Hierarchy
- Address B12 deficiency
- Note: May require B12 injections if signs of autoimmune gastritis
- Address iron deficiency
- Note: If using iron supplements AND thyroid replacement medication – please take iron with a meal at least 8 hours, preferably 12 hours away from thyroid medication
- Address zinc deficiency
- Consider utilizing selenium in autoimmune thyroiditis
- 200 mcg for 6-12 months
- Address vitamin D deficiency
- Increased importance for those with documented autoimmune thyroiditis
Part II: Clinical Treatment – Non-Medication Algorithm References
- https://pubmed.ncbi.nlm.nih.gov/30060266/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296200/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6592837/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4056127/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5405068/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/
- https://pubmed.ncbi.nlm.nih.gov/27474730/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746228/
- https://link.springer.com/article/10.1007/s12011-019-01963-5
- https://pubmed.ncbi.nlm.nih.gov/33741837/
- https://pubmed.ncbi.nlm.nih.gov/27702392/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166548/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618598/
- https://pubmed.ncbi.nlm.nih.gov/31987229/
Part III: Clinical Treatment – Medication
- Use of generic T4 only medication (Levothyroxine)
- We are seeing increasing levels of concerning manufacturing practices with generic drugs and more patients requiring LESS medication when switching to BRAND name medications.
- Taking into account patient preferences, resources, and the concerns with generic drugs, you may desire to Skip 1 and begin by utilizing brand name T4 medication
- Use of brand name T4 medication (Synthroid, Levoxyl, Tirosint)
- Ensure adherence to regular dosing schedule
- Medication WITHOUT Food
- Ensure they are NOT consuming with coffee AND creamer, for example
- Ensure NO iron supplements within 8 hours
- Use of Liquid T4 medication
- If concerned for malabsorption, unstable TSH level, or other significant GI disturbance disrupting absorption
- Note: The patient will likely require LESS medication than current non-liquid dose if taken on an empty stomach, so consider DECREASING from equivalent T4 dose when switching to Liquid T4
- Note: Some research has looked at taking liquid T4 medication WITH first meal and showed improved quality of life WITHOUT compromised thyroid hormone function
- Use of Combination T4/T3 Medication
- See Part 1: Screening and Clinical History – Key Clinical Questions #3 for further elaboration
- See Dec 2020 FFMR for more details
Bonus: Tapering and Discontinuation of Thyroid Medication
- See Part 1: Screening and Clinical History – Key Clinical Questions #2 for further elaboration of patients with a higher likelihood of successful discontinuation
- There is currently no gold standard for tapering and discontinuation
- Current Clinic Practices for Discontinuation
- Option 1: Decrease dosage by 25 mcg T4 or equivalent T4/T3 combination dose every 3-4 weeks until 25 mcg, then discontinue
- Option 2: Decrease dosage by ½ of T4 dose or equivalent T4/T3 combination dose every 3-4 weeks until 25 mcg, then discontinue
- See Rapid Fire Research: Study 1 for description of various tapering regimens examined in a meta-analysis of discontinuation studies
Part III: Clinical Treatment – Medication Algorithm References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4137817/
- https://www.nytimes.com/2019/05/13/books/review/bottle-of-lies-katherine-eban.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5997842/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6667836/
Clinical Outcomes After Discontinuation of Thyroid Hormone Replacement: A Systematic Review and Meta-Analysis
Thyroid . 2020 Dec 29. doi: 10.1089/thy.2020.0679. Online ahead of print.
- Up to ⅓ of patients may be able to effectively discontinue thyroid medication
- Individuals with subclinical hypothyroidism or incorrect hypothyroidism diagnosis are more likely to be successful with discontinuation
- “Low-quality evidence suggests that up to a third of patients remained euthyroid after thyroid hormone discontinuation, with a higher proportion of patients with an initial diagnosis of SCH (Subclinical Hypothyroidism) remaining euthyroid than patients with an initial diagnosis of OH (Overt-hypothyroidism)
- Various tapering regimens were utilized in a few of the studies included in the analysis
- “discontinuing therapy within two weeks, first halving dose at week one, and discontinuing the remaining dose at week two”
- “halving LT4 dose successively every four weeks until a dose ≤12.5 mcg/day was reached and therapy was then discontinued”
- “halving dose and eliminating the remaining dose in two months or by 25 mcg reductions until discontinuation”
The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial
Complement Ther Med . 2020 Jan;48:102234. doi: 10.1016/j.ctim.2019.102234. Epub 2019 Nov 3.
- 60 patients with euthyroid (by medication) hypothyroidism were randomized to either receive a synbiotic made from 5 strains of various Lactobacillus and Bifidobacterium bacteria plus Streptococcus thermophilus and a FOS prebiotic or placebo for 8 weeks.
- Synbiotic capsules contained seven freeze-dried probiotic strains (7 × 109 colony forming units: (CFU)
- Lactobacillus casei, 7 × 109 CFU
- Lactobacillus acidophilus, 2 × 109 CFU
- Lactobacillus rhamnosus, 1.5 × 109 CFU
- Lactobacillus bulgaricus, 2 × 108 CFU
- Bifidobacterium breve, 2 × 1010 CFU
- Bifidobacterium longum, 7 × 109 CFU
- Streptococcus thermophilus, 5 × 1010 CFU
- Fructooligosaccharide as a prebiotic
- lactose, magnesium stearate and talc as carrier substances
- Synbiotic capsules contained seven freeze-dried probiotic strains (7 × 109 colony forming units: (CFU)
- Researchers measured several thyroid function studies including thyroid antibodies, measures of quality of life as well as total thyroid dose pre and post intervention.
- Researchers found statistically significant changes in TSH, total thyroid dose, and improvements in the fatigue severity scale among synbiotic participants, but not in the controls
- Clinic Note: While we can only speculate on mechanisms for improved thyroid function with improved gut health, we suspect improved medication absorption for those taking replacement medicines and downregulation of inflammatory responses within the gut as the primary drivers based on repeated clinical observations in this patient subpopulation.